Introduction
Lung cancer is the malignant tumor with the highest
fatality rate in the world. Meanwhile, non-small cell lung cancer
(NSCLC) is the most common pathological type of lung cancer,
accounting for >70% of all lung cancer cases (1). The increasingly improved therapeutic
means such as traditional surgery has greatly improved the
prognosis and quality of life of lung cancer patients (1). However, intensive understanding of
the molecular mechanism of lung cancer pathogenesis is lacking at
present (2). Therefore, the
existing early diagnosis target and anticancer therapy have limited
effect on lung cancer patients (2). It is reported that >50% NSCLC
patients visiting for the first time have progressed into stage III
or have metastases (2). As a
result, they have been deprived of the opportunity of surgical
treatment. Platinum-based combined chemotherapy regimen is
considered as one of the most effective methods for treating
advanced NSCLC (3). However, tumor
is a highly heterogeneous disease. It is associated with remarkably
different sensitivity to platinum-based chemotherapeutics, even in
lung cancer patients with same clinical stage or same pathological
type (4).
As is suggested in research, the
phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K)/AKT signaling
pathway is abnormally activated in NSCLC (5). This has played an important role in
tumor cell proliferation, apoptosis, survival and drug resistance
(6). Cisplatin is the most common
first-line chemotherapeutic in clinic (7). However, tumor resistance to cisplatin
becomes increasingly common as treatment progresses, which has
severely restricted its clinical effects (7). Cisplatin resistance is a complex
process involving multiple mechanisms. Of them, continuous
activation of the PI3K/AKT pathway or its components is one of the
vital factors (6).
Chinese herbal medicine has been applied in treating
disease for thousands of years in traditional medicine (8). For instance, Jinhuang powder and
ichthammol ointment have the effects of softening hardness to
dissipate stagnation, clearing heat and removing toxicity (8). Therefore, they have been used to
treat non-suppurative acute mastitis and sebaceous cyst (9). In recent years, some scholars have
studied the effects of Yishenguchong decoction, which is
constituted by 11 kinds of Chinese herbs, on treating breast cancer
(10). Cucurbitacin is a
tetracyclic triterpenoid, which is abundant in cucurbitaceous plant
(11). Data have indicated that
cucurbitacin has anti-inflammatory, anti-bacterial and immunity
boosting effects (10). Moreover,
cucurbitacin is mainly employed in traditional medicine to assist
in treating hepatitis or primary liver cancer. It has favorable
therapeutic effects and moderate property (9). Cucurbitacin I is one of the
Cucurbitacin family members with the richest content (12). At the same time, it is also one of
the most extensively studied Cucurbitacin family members in terms
of anticancer effects (8).
Research in vivo and in vitro has suggested that
Cucurbitacin I can inhibit cellular growth of multiple malignant
tumors, such as liver cancer, gastric cancer, breast cancer and
neuroblastoma (12). In addition,
it can suppress their proliferation and apoptosis in the meantime
of improving sensitivity of tumor cells to chemotherapeutics
(12). In this study, we aimed to
identify potential anticancer effects of Cucurbitacin I regulators
cell growth of human NSCLC and to explore their mechanism.
Materials and methods
Cell culture
A549 lung adenocarcinoma were grown in complete DMEM
containing 10% FBS (both Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) at 37°C and 5% CO2.
Cell proliferation assay and toxicity
assay
Cell was treated with 0 (DMSO), 50, 100 and 200 nM
of Cucurbitacin I for 24, 48, and 72 h, for 48 h, and stained with
MTT assay for 4 h at 37°C. DMSO assay was used to dissolve for 20
min at 37°C. Absorbance was measured using an MRX II microplate
reader (Dynex, Chantilly, VA, USA) at 490 nm.
We used LDH activity to explain cell cytotoxicity of
Cucurbitacin I on NSCLC using LDH Release Assay kit (C0016;
Beyotime Institute of Biotechnology, Haimen, China). Absorbance was
measured using an MRX II microplate reader (Dynex) at 405 nm.
Flow cytometry analysis
After treatment with Cucurbitacin I for 48 h, cells
washed with PBS three times. Cells were stained with all 5 µl of
Annexin V-FITC and PI (Sigma-Aldrich Co., St Louis, MO, USA) for 15
min at darkness. The apoptosis rate was analyzed by flow cytometry
(BD FACSCanto II; BD Biosciences, San Diego, CA, USA).
Western blot analysis and caspase-3/9
activity
Protein samples from cells were prepared in RIPA
buffer (Beyotime Institute of Biotechnology) and protein
concentrations were measured using the BCA protein assay kit
(Beyotime Institute of Biotechnology). The equal amounts (40 µg) of
protein were separated on 8–12% SDS gel and transferred onto PVDF
membranes. Membranes were probed with the primary antibodies: PI3K
(1:500), p-AKT (1:500), p-p70S6K (1:500) and GAPDH (1:500; all
Santa Cruz, CA, USA) at 4°C overnight. After incubating with
HRP-conjugated secondary antibodies goat anti-rabbit IgG, protein
bands were detected using an enhanced chemiluminescence detection
kit (ThermoFisher Scientific, Inc.). Equal amounts protein also was
used to measure caspsae-3/9 activity using caspsae-3/9 activity
kits (Beyotime Institute of Biotechnology).
Statistical analysis
Data were presented as the mean ± standard error.
Statistical differences were analyzed using the one-way analysis of
variance (ANOVA) with the Tukey's test. P<0.05 was considered to
indicate a statistically significant difference.
Results
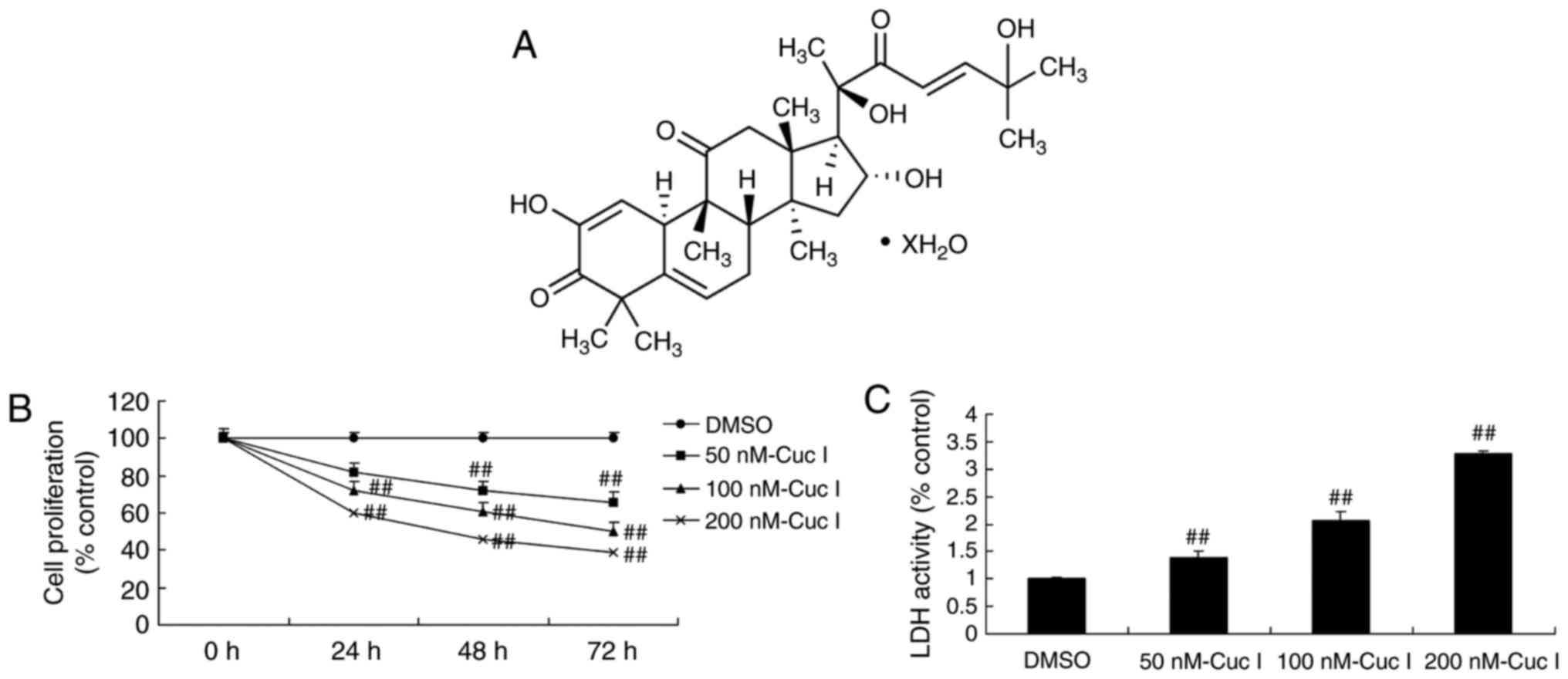
Cucurbitacin I attenuated cell
proliferation of NSCLC
To investigate whether the anticancer of
Cucurbitacin I on NSCLC, A549 cell was treated with Cucurbitacin I,
cell proliferation and LDH activity were measured. The structural
formula of Cucurbitacin I was showed at Fig. 1A. As showed in Fig. 1B, C, Cucurbitacin I attenuated cell
proliferation and increased LDH activity in A549 cell, compared
with control group.
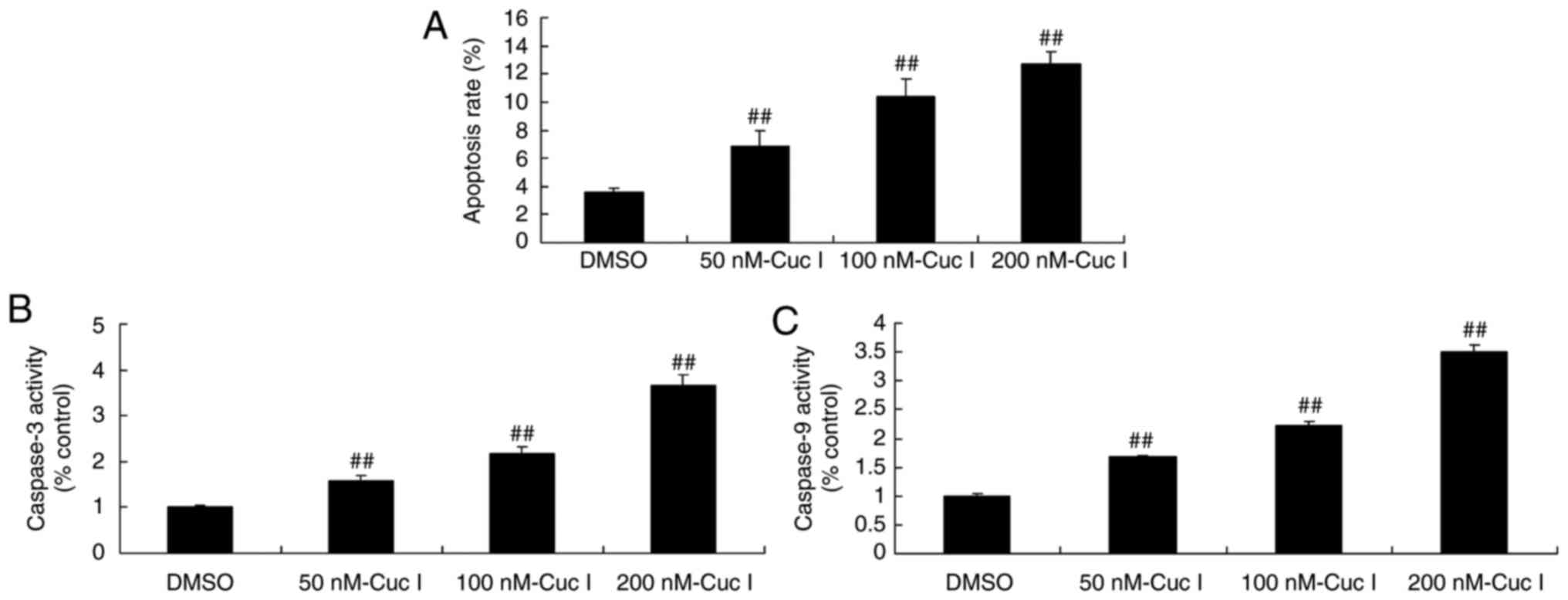
Cucurbitacin I induced apoptosis of
NSCLC
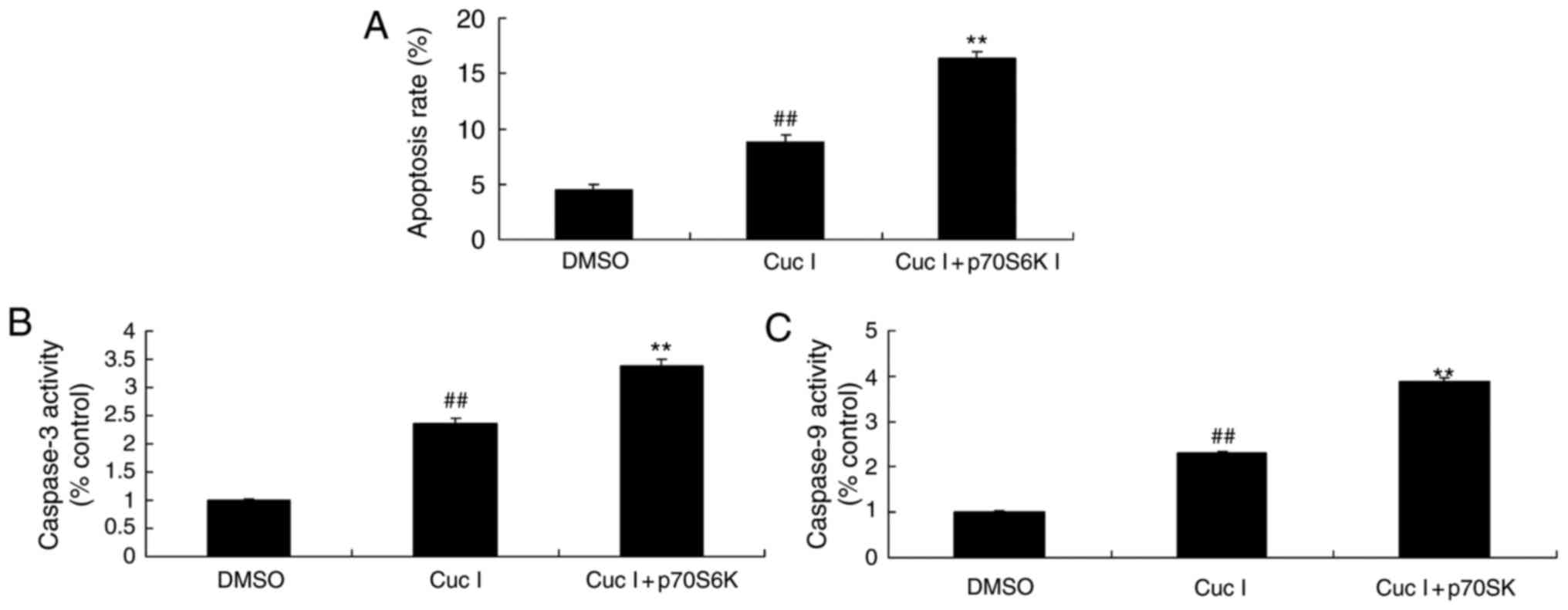
Next, Cucurbitacin I induced apoptosis, and promoted
capase-3/9 activity in A549 cell, compared with control group
(Fig. 2).
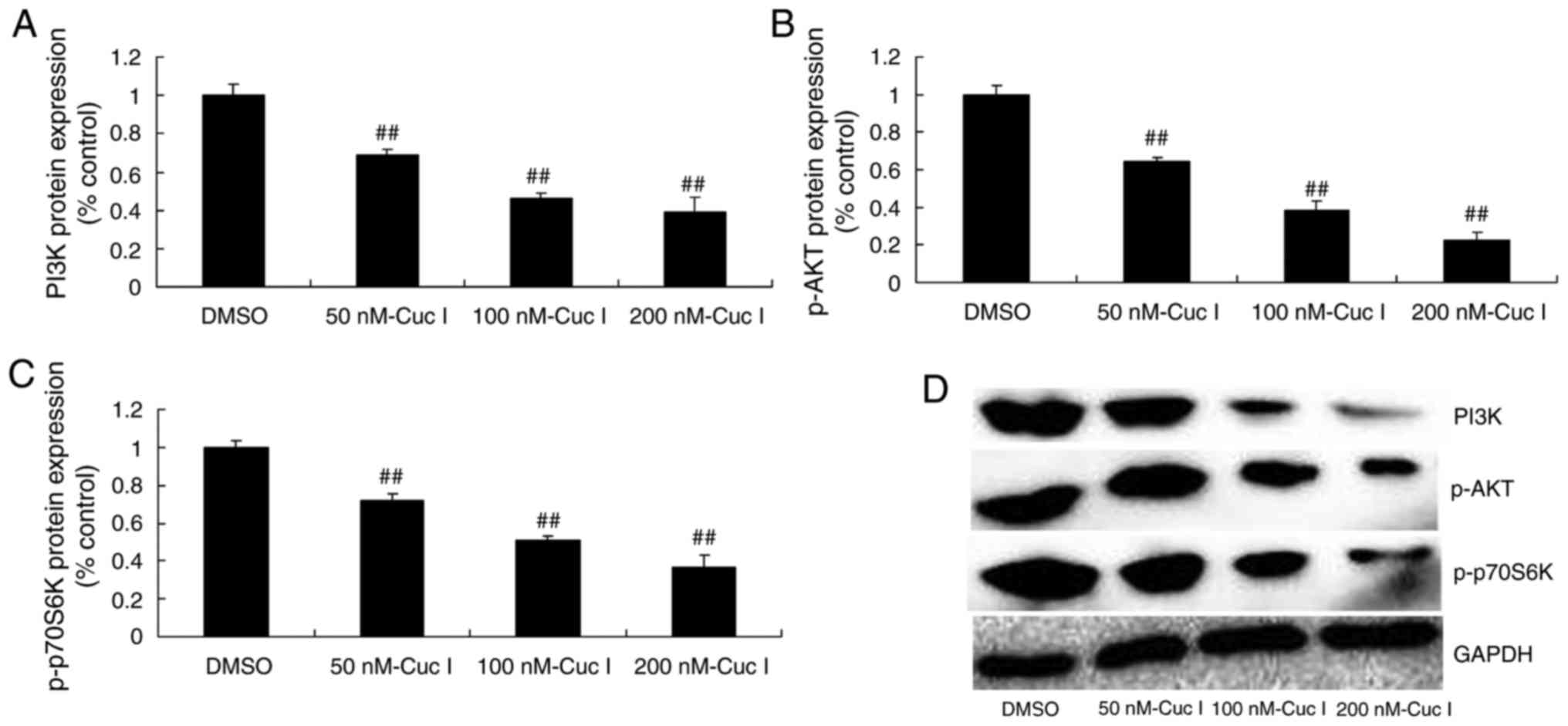
Cucurbitacin I suppressed
PI3K/AKT/p70S6K pathway of NSCLC
To identify the PI3K/AKT/p70S6K pathway mediator
involved in the anticancer effects of Cucurbitacin I on NSCLC, we
examined the changes of PI3K/AKT/p70S6K pathway. Cucurbitacin I
suppressed PI3K, p-AKT and p-p70S6K protein expression, compared
with control group (Fig. 3).
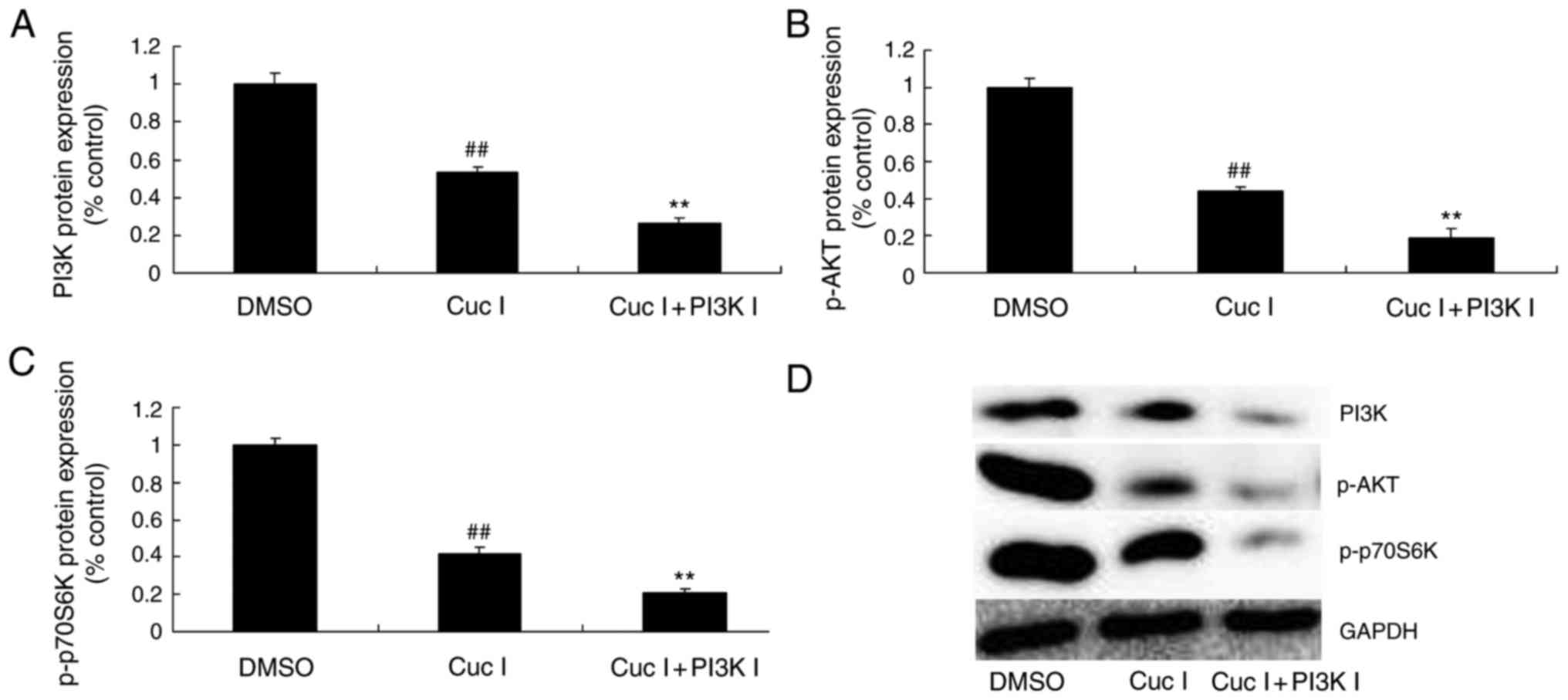
Suppression of PI3K increased the
anticancer effects of Cucurbitacin I on PI3K/AKT/p70S6K pathway of
NSCLC
To validate the downregulation of PI3K/AKT/p70S6K
pathway by PI3K inhibitor (LY294002; 100 nM) affects the anticancer
effects of Cucurbitacin I on NSCLC. PI3K inhibitor suppressed PI3K,
p-AKT and p-p70S6K protein expression, compared with control group.
Taken together, PI3K/AKT/p70S6K pathway maybe mediates the
anticancer effects of Cucurbitacin I on NSCLC (Fig. 4).
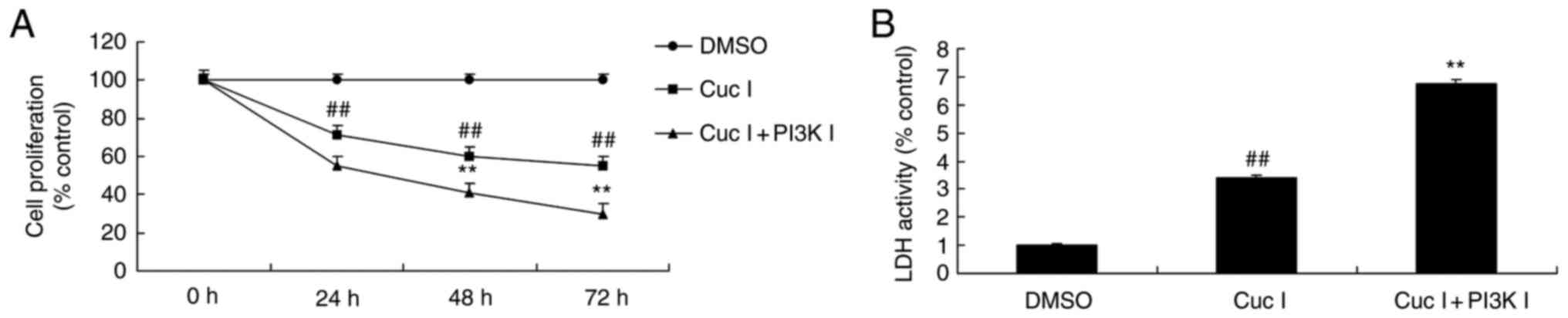
Suppression of PI3K increased the
anticancer effects of Cucurbitacin I on cell proliferation of
NSCLC
Fig. 5 showed that
the suppression of PI3K increased the anticancer effects of
Cucurbitacin I on the inhibition of cell proliferation and the
activation of LDH activity of NSCLC, compared with only
Cucurbitacin I treatment group (Fig.
5).
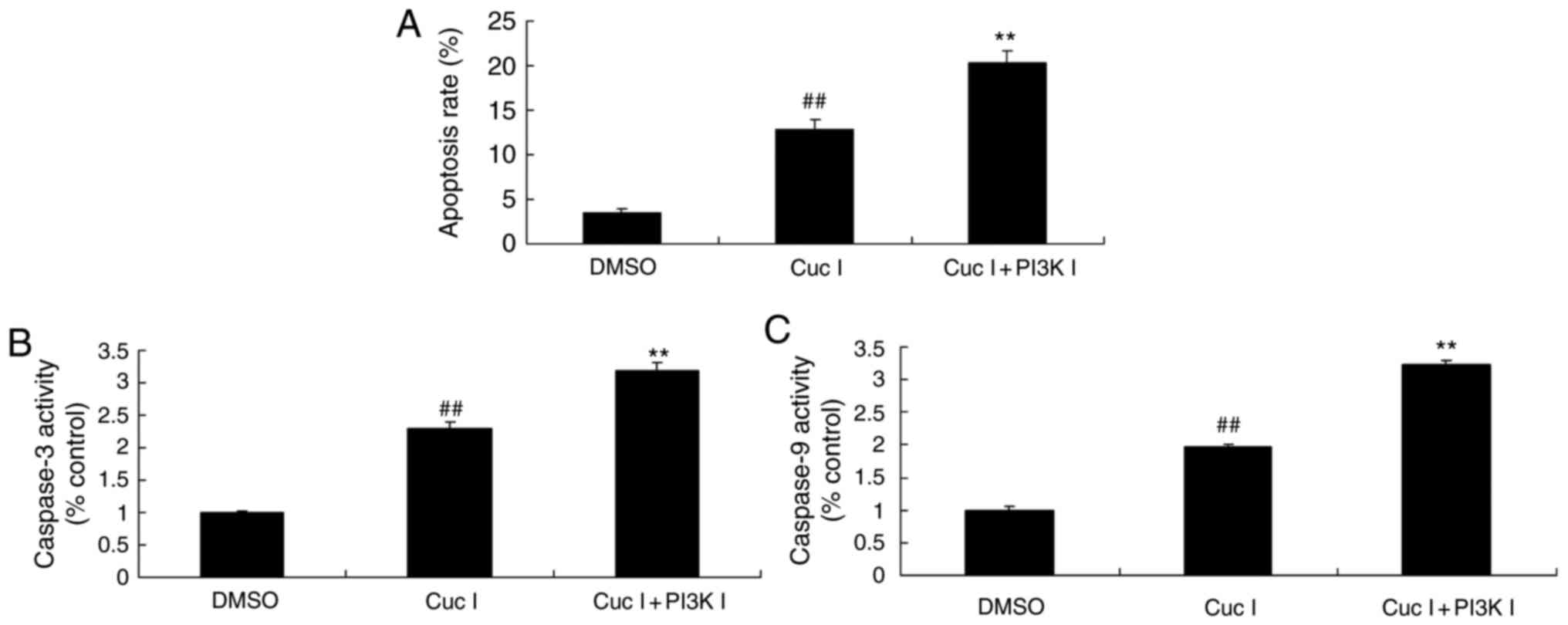
Suppression of PI3K increased the
anticancer effects of Cucurbitacin I on apoptosis of NSCLC
Meanwhile, the suppression of PI3K increased the
anticancer effects of Cucurbitacin I on the promotion of apoptosis
and caspase-3/9 activity of NSCLC, compared with only Cucurbitacin
I treatment group (Fig. 6).
Overall, these data suggest that Cucurbitacin I induced apoptotic
in NSCLC involve inhibition of PI3K/AKT/p70S6K pathway.
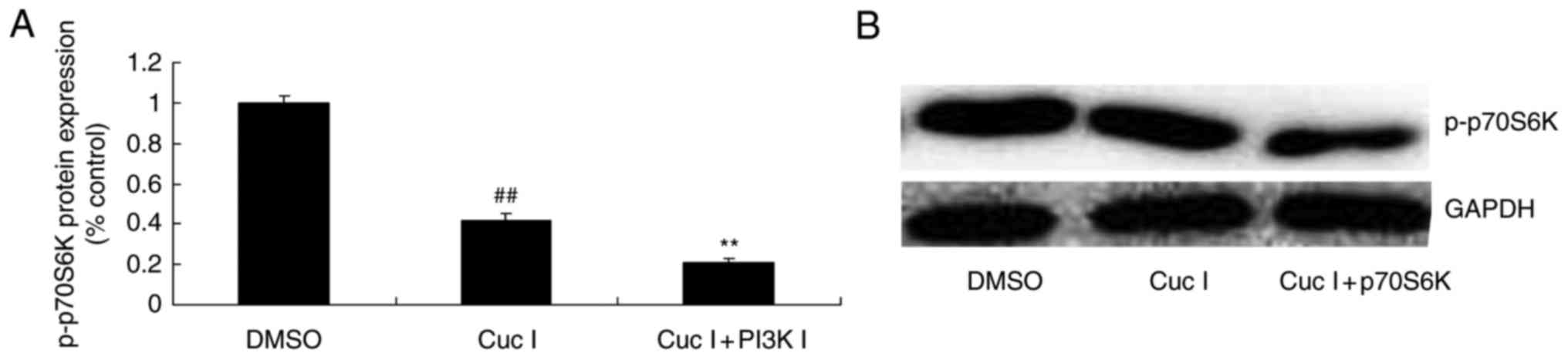
Suppression of p70S6K reduced the
anticancer effects of Cucurbitacin I on PI3K/AKT/p70S6K pathway of
NSCLC
We next explored whether p70S6K is involved in the
anticancer effects of Cucurbitacin I on cell proliferation of
NSCLC. As showed in Fig. 7, p70S6K
inhibitor (LY-2584702 hydrochloride, 2 nM) suppressed the protein
expression of p-p70S6K in NSCLC by Cucurbitacin I, compared with
only Cucurbitacin I treatment group (Fig. 7).
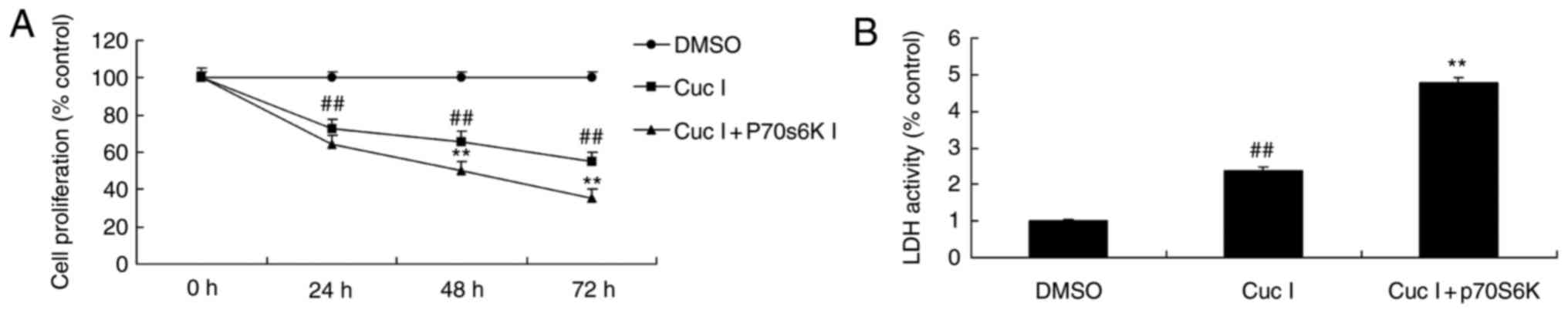
Suppression of p70S6K reduced the
anticancer effects of Cucurbitacin I on cell proliferation of
NSCLC
The suppression of p70S6K increased the anticancer
effects of Cucurbitacin I on the inhibition of cell proliferation
and the activation of LDH activity of NSCLC, compared with only
Cucurbitacin I treatment group (Fig.
8).
Suppression of p70S6K reduced the
anticancer effects of Cucurbitacin I on apoptosis of NSCLC
Moreover, the suppression of p70S6K increased the
anticancer effects of Cucurbitacin I on the promotion of apoptosis
and caspase-3/9 activity of NSCLC, compared with only Cucurbitacin
I treatment group (Fig. 9).
Discussion
Lung cancer is a severe disease affecting human
life. The world has witnessed over 1.1 million of patients dying of
lung cancer, including 80% NSCLC patients (4). Surgical resection remains the
preferred method for treating NSCLC at present (13). However, most patients have
developed into moderate and advanced stage at diagnosis, which has
deprived them of the optimal surgical timing. Therefore, they can
only extend their life through chemotherapy or radiotherapy
(13). In addition, most patients
undergoing surgery requires adjuvant chemotherapy (14). Consequently, chemotherapy is an
indispensable means for treating tumor and delaying patients' life
span (15). The current study
indicated Cucurbitacin I markedly attenuated cell proliferation in
NSCLC. However, we only used A549 cell, which is a limitation of
our study. So, further studies will be conducted with more CSCLC
cell lines in order to confirm the study's results.
Genotype difference of NSCLC is suggested to be
partly correlated with body sensitivity to platinum-based
chemotherapeutics (16).
Platinum-based chemotherapeutics, such as cisplatin and
carboplatin, are one of the most extensively used anticancer
chemotherapeutics with the most definite efficacy (17). Moreover, they show strong
cytotoxicity (16). Platinum-based
drugs will bind with intranuclear DNA after entering the cell
nucleus. They can lead to irreversible DNA damage through forming
the platinum-DNA complex (18).
Meanwhile, they can also induce cell apoptosis and thus exert their
anticancer effects (16). The
intracellular DNA damage repair mechanism allows cells to recruit
DNA damage repair-related factors to repair the DNA damage induced
by platinum-based chemotherapeutics (18). Therefore, expression and function
of regulatory factors during DNA repair process are considered to
play a determining role in tumor sensitivity to platinum-based
chemotherapeutics (17). The
results of the present study indicated that Cucurbitacin I markedly
induced apoptosis in NSCLC. Ishdorj et al demonstrates that
Cucurbitacin-I activates of apoptosis and cell cycle arrest,
leading to increased VEGF expression in B leukemic cells (11).
Exon point mutation of gene PI3K is found in
multiple human tumor cells, such as colorectal cancer, breast
cancer, brain cancer, liver cancer, gastric cancer, ovarian cancer
and lung cancer. About 3% NSCLC patients have PI3K mutation in
tumor cells (19). The PI3K/Akt
signal transduction pathway plays a vital role in growth
factor-mediated cell survival (20). Research has indicated that,
dysfunction of the PI3K/Akt/mTOR pathway may play a crucial role in
lung cancer formation (19). As
has been reported, several cell proliferation signals produced by
the binding of transmembrane receptor with ligand can activate the
transduction of PI3K/Akt/mTOR signal (20). This is closely associated with the
proliferation and survival of NSCLC (7). Furthermore, out showed that
Cucurbitacin I suppressed PI3K and p-AKT protein expression in
NSCLC. Johnson et al indicate that Cucurbitacin I blocks
cerebrospinal fluid through Akt signal (21).
In recent years, the role of PI3K/Akt/m TOR
signaling pathway in human tumor has attracted extensive attention
(22). Activation of PI3K/Akt/m
TOR signaling pathway is quite common in the genesis of human tumor
(5). Such pathway can promote
cancer genesis through multiple mechanisms, including gene
mutation, decreased expression of tumor suppressor gene PTEN, PI3K
mutation or amplification, Akt mutation or amplification, and
activation of oncogene receptor (23). Moreover, activation of all pathway
components is a factor indicating poor prognosis for numerous
tumors, which can induce treatment resistance (20). Inhibiting such pathway can reverse
the resistance, and improve the chemotherapy and radiotherapy
effects both in vivo and in vitro (23). Consequently, it is necessary to
intensively study the precise mechanism of that pathway (22). Our study showed that PI3K inhibitor
increased anticancer effects of Cucurbitacin I on NSCLC. Premkumar
et al reported that Cucurbitacin I induces defects in cell
cycle progression and promotes ABT-737 cell death of cell death
through PI3K/Akt (24).
P70s6k is one of the direct substrates of p-mTOR
protein, which can be phosphorylated by p-mTOR protein (25). The phosphorylated p70s6k can
further phosphorylate the 40S ribosomal subunit of protein S6, so
as to enhance mRNAs translation (26). In this way, the ribosome,
initiation factor and elongation factor can be produced, thus
promoting tumor cell diffusion (26). Research has suggested that p70s6k
protein is closely associated with tumors such as digestive system
neoplasms, ovarian cancer, breast cancer, hemangiomas and parotid
adenocarcinoma. P-mTOR/p70s6k signaling pathway can regulate
expression of downstream genes, thus affecting protein synthesis,
cell proliferation and apoptosis (27). Moreover, it is closely related to
the genesis, growth, metastasis and resistance of malignant tumor.
Thus, it has become a hotspot of current tumor research (25). We found that Cucurbitacin I
suppressed p-p70S6K pathway in NSCLC. Yuan et al showed that
Cucurbitacin I induces protective autophagy through p70S6K pathway
in glioblastoma in vitro and in vivo (12).
In conclusion, the present study demonstrated that
anticancer effects of Cucurbitacin I inhibited cell growth of human
NSCLC through PI3K/AKT/p70S6K pathway. Therefore, Cucurbitacin I
may present a novel therapeutic treatment for NSCLC.
References
|
1
|
Yang JC, Ahn MJ, Kim DW, Ramalingam SS,
Sequist LV, Su WC, Kim SW, Kim JH, Planchard D, Felip E, et al:
Osimertinib in pretreated T790M-positive advanced non-small-cell
lung cancer: AURA study phase II extension component. J Clin Oncol.
35:1288–1296. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Crawford J, Swanson P, Schwarzenberger P,
Sandler A, Prager D, Zhang K, Freeman DJ, Johnson CW, Krishnan K
and Johnson D: A phase 2 randomized trial of paclitaxel and
carboplatin with or without panitumumab for first-line treatment of
advanced non-small-cell lung cancer. J Thorac Oncol. 8:1510–1518.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kubota K, Ichinose Y, Scagliotti G, Spigel
D, Kim JH, Shinkai T, Takeda K, Kim SW, Hsia TC, Li RK, et al:
Phase III study (MONET1) of motesanib plus carboplatin/paclitaxel
in patients with advanced nonsquamous nonsmall-cell lung cancer
(NSCLC): Asian subgroup analysis. Ann Oncol. 25:529–536. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liang J, Bi N, Wu S, Chen M, Lv C, Zhao L,
Shi A, Jiang W, Xu Y, Zhou Z, et al: Etoposide and cisplatin versus
paclitaxel and carboplatin with concurrent thoracic radiotherapy in
unresectable stage III non-small cell lung cancer: A multicenter
randomized phase III trial. Ann Oncol. 28:777–783. 2017.PubMed/NCBI
|
|
5
|
Wang B, Jiang H, Wang L, Chen X, Wu K,
Zhang S, Ma S and Xia B: Increased MIR31HG lncRNA expression
increases gefitinib resistance in non-small cell lung cancer cell
lines through the EGFR/PI3K/AKT signaling pathway. Oncol Lett.
13:3494–3500. 2017.PubMed/NCBI
|
|
6
|
Chao W, Deng JS, Li PY, Liang YC and Huang
GJ: 3,4-Dihydroxybenzalactone suppresses human non-small cell lung
carcinoma cells metastasis via suppression of epithelial to
mesenchymal transition, ROS-Mediated PI3K/AKT/MAPK/MMP and NFκB
signaling pathways. Molecules. 22:pii: E5372017. View Article : Google Scholar
|
|
7
|
Pérez-Ramírez C, Cañadas-Garre M, Molina
MÁ, Faus-Dáder MJ and Calleja-Hernández MÁ: PTEN and PI3K/AKT in
non-small-cell lung cancer. Pharmacogenomics. 16:1843–1862. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu Y, Chen H, Li R, Wang X, Li H, Xin J,
Liu Z, Wu S, Jiang W and Zhu L: Cucurbitacin-I induces hypertrophy
in H9c2 cardiomyoblasts through activation of autophagy via
MEK/ERK1/2 signaling pathway. Toxicol Lett. 264:87–98. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Song J, Liu H, Li Z, Yang C and Wang C:
Cucurbitacin I inhibits cell migration and invasion and enhances
chemosensitivity in colon cancer. Oncol Rep. 33:1867–1871. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Qi J, Xia G, Huang CR, Wang JX and Zhang
J: JSI-124 (Cucurbitacin I) inhibits tumor angiogenesis of human
breast cancer through reduction of STAT3 phosphorylation. Am J Chin
Med. 43:337–347. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ishdorj G, Johnston JB and Gibson SB:
Cucurbitacin-I (JSI-124) activates the JNK/c-Jun signaling pathway
independent of apoptosis and cell cycle arrest in B leukemic cells.
BMC Cancer. 11:2682011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yuan G, Yan SF, Xue H, Zhang P, Sun JT and
Li G: Cucurbitacin I induces protective autophagy in glioblastoma
in vitro and in vivo. J Biol Chem. 289:10607–10619. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sharma N, Pennell N, Nickolich M, Halmos
B, Ma P, Mekhail T, Fu P and Dowlati A: Phase II trial of sorafenib
in conjunction with chemotherapy and as maintenance therapy in
extensive-stage small cell lung cancer. Invest New Drugs.
32:362–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Heigener DF, Pereira JR, Felip E, Mazal J,
Manzyuk L, Tan EH, Merimsky O, Sarholz B, Esser R and Gatzemeier U:
Weekly and every 2 weeks cetuximab maintenance therapy after
platinum-based chemotherapy plus cetuximab as first-line treatment
for non-small cell lung cancer: Randomized non-comparative phase
IIIb NEXT trial. Target Oncol. 10:255–265. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Larkins E, Scepura B, Blumenthal GM,
Bloomquist E, Tang S, Biable M, Kluetz P, Keegan P and Pazdur R:
U.S. Food and drug administration approval summary: ramucirumab for
the treatment of metastatic non-small cell lung cancer following
disease progression on or after platinum-based chemotherapy.
Oncologist. 20:1320–1325. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li L, Zhu T, Gao YF, Zheng W, Wang CJ,
Xiao L, Huang MS, Yin JY, Zhou HH and Liu ZQ: Targeting DNA damage
response in the radio(Chemo)therapy of non-small cell lung cancer.
Int J Mol Sci. 17:pii: E8392016. View Article : Google Scholar
|
|
17
|
Shen H, Wang L, Zhang J, Dong W, Zhang T,
Ni Y, Cao H, Wang K, Li Y, Wang Y and Du J: ARRB1 enhances the
chemosensitivity of lung cancer through the mediation of DNA damage
response. Oncol Rep. 37:761–767. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu D, Wu C, Jiao Y, Hou L, Lu D, Zheng H,
Chen C, Qian J, Fei K and Su B: WEE1 kinase polymorphism as a
predictive biomarker for efficacy of platinum-gemcitabine doublet
chemotherapy in advanced non-small cell lung cancer patients. Sci
Rep. 5:111142015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chou PY, Huang GJ, Pan CH, Chien YC, Chen
YY, Wu CH, Sheu MJ and Cheng HC: Trilinolein inhibits proliferation
of human non-small cell lung carcinoma A549 through the modulation
of PI3K/Akt pathway. Am J Chin Med. 39:803–815. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sun Z, Wang Z, Liu X and Wang D: New
development of inhibitors targeting the PI3K/AKT/mTOR pathway in
personalized treatment of non-small-cell lung cancer. Anticancer
Drugs. 26:1–14. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Johnson MD, O'Connell MJ and Walter K:
Cucurbitacin I blocks cerebrospinal fluid and platelet derived
growth factor-BB stimulation of leptomeningeal and meningioma DNA
synthesis. BMC Complement Altern Med. 13:3032013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fumarola C, Bonelli MA, Petronini PG and
Alfieri RR: Targeting PI3K/AKT/mTOR pathway in non small cell lung
cancer. Biochem Pharmacol. 90:197–207. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Park C, Hong SH, Kim GY and Choi YH:
So-Cheong-Ryong-Tang induces apoptosis through activation of the
intrinsic and extrinsic apoptosis pathways, and inhibition of the
PI3K/Akt signaling pathway in non-small-cell lung cancer A549
cells. BMC Complement Altern Med. 15:1132015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Premkumar DR, Jane EP and Pollack IF:
Cucurbitacin-I inhibits Aurora kinase A, Aurora kinase B and
survivin, induces defects in cell cycle progression and promotes
ABT-737-induced cell death in a caspase-independent manner in
malignant human glioma cells. Cancer Biol Ther. 16:233–243. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
In JK, Kim JK, Oh JS and Seo DW:
5-Caffeoylquinic acid inhibits invasion of non-small cell lung
cancer cells through the inactivation of p70S6K and Akt activity:
Involvement of p53 in differential regulation of signaling
pathways. Int J Oncol. 48:1907–1912. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dhar R and Basu A: Constitutive activation
of p70 S6 kinase is associated with intrinsic resistance to
cisplatin. Int J Oncol. 32:1133–1137. 2008.PubMed/NCBI
|
|
27
|
Dong S, Zhang XC, Cheng H, Zhu JQ, Chen
ZH, Zhang YF, Xie Z and Wu YL: Everolimus synergizes with gefitinib
in non-small-cell lung cancer cell lines resistant to epidermal
growth factor receptor tyrosine kinase inhibitors. Cancer Chemother
Pharmacol. 70:707–716. 2012. View Article : Google Scholar : PubMed/NCBI
|