Introduction
Traumatic brain injury (TBI) is a prevalent disease
in modern society. The fatality and disability rates of TBI are the
highest among traumas of human organs (1). The incidence of TBI in USA is ~2%,
and 500,000 new TBI cases are recorded annually, including 10%
severe TBI, which leads to ~20,000 mortality and 30,000 disability
cases, resulting in significant direct and indirect economic losses
(2). With the rapid development of
the global economy and modern transportation, TBI has become an
important human health issue (1).
Therefore, research groups are attempting to alleviate TBI-induced
neurological impairment, and improve the effectiveness of the
treatment of TBI (3). TBI and the
resulting pathological condition are major factors endangering
human health. Sequelae of TBI include post-TBI learning and memory
skill impairment, which influence the quality of life of patients
(4).
TBI-induced neural death is the most prevalent cause
of death in patients. Inhibition of post-injury cell death and
preservation of neurons is the research focus of TBI (5). Inhibition of the cell death pathway
and fundamental reduction of neuronal death is a potential
treatment approach (6). Cell death
can be classified into two categories, cell apoptosis and cell
necrosis. Apoptosis is programmed cell death regulated by gene
expression, while necrosis represents an unregulated and
irreversible passive cell death (7).
Numerous biologically active natural products
isolated from Chinese medical herbs frequently demonstrate
physiological functions. An appropriate structural modification of
these herbs may lead to the development of novel drugs with high
activity and specificity (8). Drug
research and development in China should focus on carrying out
innovative drug research based on biologically active natural
products native to China (9). Many
biologically active natural products extracted from Chinese herbal
medicine, including berberine, have been extensively applied in
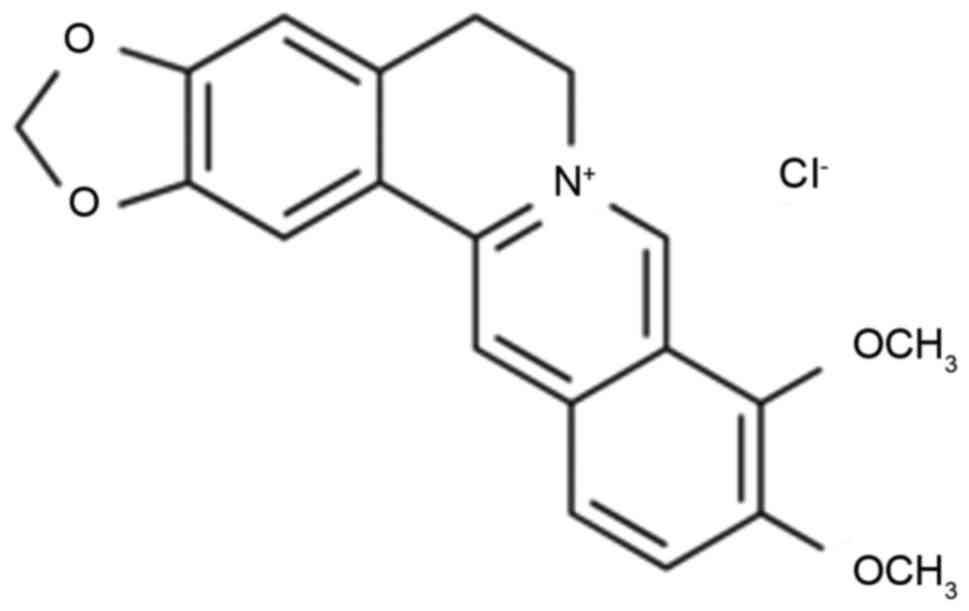
medical practice. Berberine (Fig.
1) is an isoquinoline alkaloid derived from Coptis
chinensis, a plant species native to China (9). Berberine and its derivatives
demonstrate multiple pharmacological effects on tumor treatment,
diabetes, cardiovascular disease, hyperlipidemia, inflammation,
bacterial and viral infection, cerebral ischemic injury, mental
disease, Alzheimer's disease and osteoporosis (10). The aim of the present study was to
determine the neuroprotective effect of berberine on learning and
memory skills in severe TBI, and to explore the underlying
molecular mechanism.
Materials and methods
Animals and treatment groups
Male C57BL/6J mice (6–7 weeks old; weight, 20–22 g)
were obtained from the National Laboratory Animal Center of Gansu
Medical College (Lanzhou, China). All animals were randomly
allocated into one of three groups: i) Control; ii) TBI model; and
iii) berberine agonist treatment. Mice were anesthetized with an
intraperitoneal injection (I.I) of sodium pentobarbital (65 mg/kg;
Sigma-Aldrich; Merck KGaA, Darmstadt, Germany), and 5 mm craniotomy
was performed at the right parietal cortex. Controlled cortical
impact was induced using a pneumatic piston with a 2.5 mm rounded
metal tip. The bone flap was replaced and sealed, and the scalp was
sterilized with iodophor (Sangon Biotech Co., Ltd., Shanghai,
China) and sutured. Temperature of the heated cage was maintained
at 37.0±0.5°C using a heated pad. Following injury, mice were
administered 10 mg/kg/day berberine (Sigma-Aldrich; Merck KGaA) via
intraperitoneal injection for 4 weeks. The present study was
approved by the Ethics Committee of Gansu Provincial Hospital
(Gansu, China).
Morris water maze test
Following treatment with berberine agonist, mice
were subjected to a Morris water maze test (Gansu Medical College,
Gansu, China; 1×0.5×0.4 m; 23±2°C). Mice learned how to navigate
the maze for 4 days, and then the probe trial was removed. The time
it took for mice to pass through the maze and find a platform was
recorded and called the escape latency.
Measurement of inflammation and
oxidation
Peripheral blood was collected following treatment
with berberine agonist and centrifuged at 2,000 × g for 10 min at
4°C. ELISA for glutathione peroxidase 1 (GSH-PX; S0055),
glutathione synthetase (GSH; S0053), superoxide dismutase (SOD;
S0109), malondialdehyde (MDA; S0131), tumor necrosis factor-α
(TNF-α; PT512) and interleukin (IL)-6 (PI326) levels was performed
using commercially available kits (Beyotime Institute of
Biotechnology). Choline acetyltransferase (ChAT) and
acetylcholinesterase (AchE) levels were performed using
commercially available kits (A079-1 and A024 respectively; Nanjing
Jiancheng Biology Engineering Institute, Nanjing, China).
Western blotting
Protein homogenates were prepared from hippocampal
tissues using a radioimmunoprecipitation assay (RIPA; Beyotime
Institute of Biotechnology), and centrifuged at 12,000 × g for 10
min at 4°C. Protein content was measured using a bicinchoninic acid
assay. Proteins (50 µg/per lane) were separated by 8–10% SDS-PAGE
and transferred to a polyvinylidene difluoride membrane. The
membrane was blocked using 5% skimmed milk in TBS with Tween-20 and
incubated with matrix metalloproteinase (MMP)-3 (sc-374029; 1:300),
MMP-9 (sc-10737; 1:300), caspase-3 (sc-98785; 1:500), sirtuin 1
(Sirt1; sc-15404; 1:500), phosphorylated (p)-p38 (sc-101759; 1:500)
and GAPDH (sc-25778; 1:500; all Santa Cruz Biotechnology, Inc.,
Dallas, TX, USA) primary antibodies at 4°C overnight. Following
washing with TBST for 15 min, membranes were incubated with a
horseradish peroxidase-linked anti-rabbit or anti-mouse secondary
antibody (sc-2004 or sc-2020; 1:2,000; Santa Cruz Biotechnology,
Inc.) for 2 h at 37°C and detected using Pierce enhanced
chemifluorescent western blotting substrate (cat. no. 321109;
Thermo Fisher Scientific, Inc., Waltham, MA, USA).
Statistical analysis
Data are presented as the mean ± standard deviation
using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA). One-way or
two-way analysis of variance followed by Bonferroni's post hoc test
was used for multiple group comparisons. P<0.05 was considered
to indicate a statistically significant difference.
Results
Protective effect of berberine agonist
evidenced by Morris water maze test
Berberine (Fig. 1)
is an isoquinoline alkaloid derived from Coptis chinensis, a
plant species native to China (9).
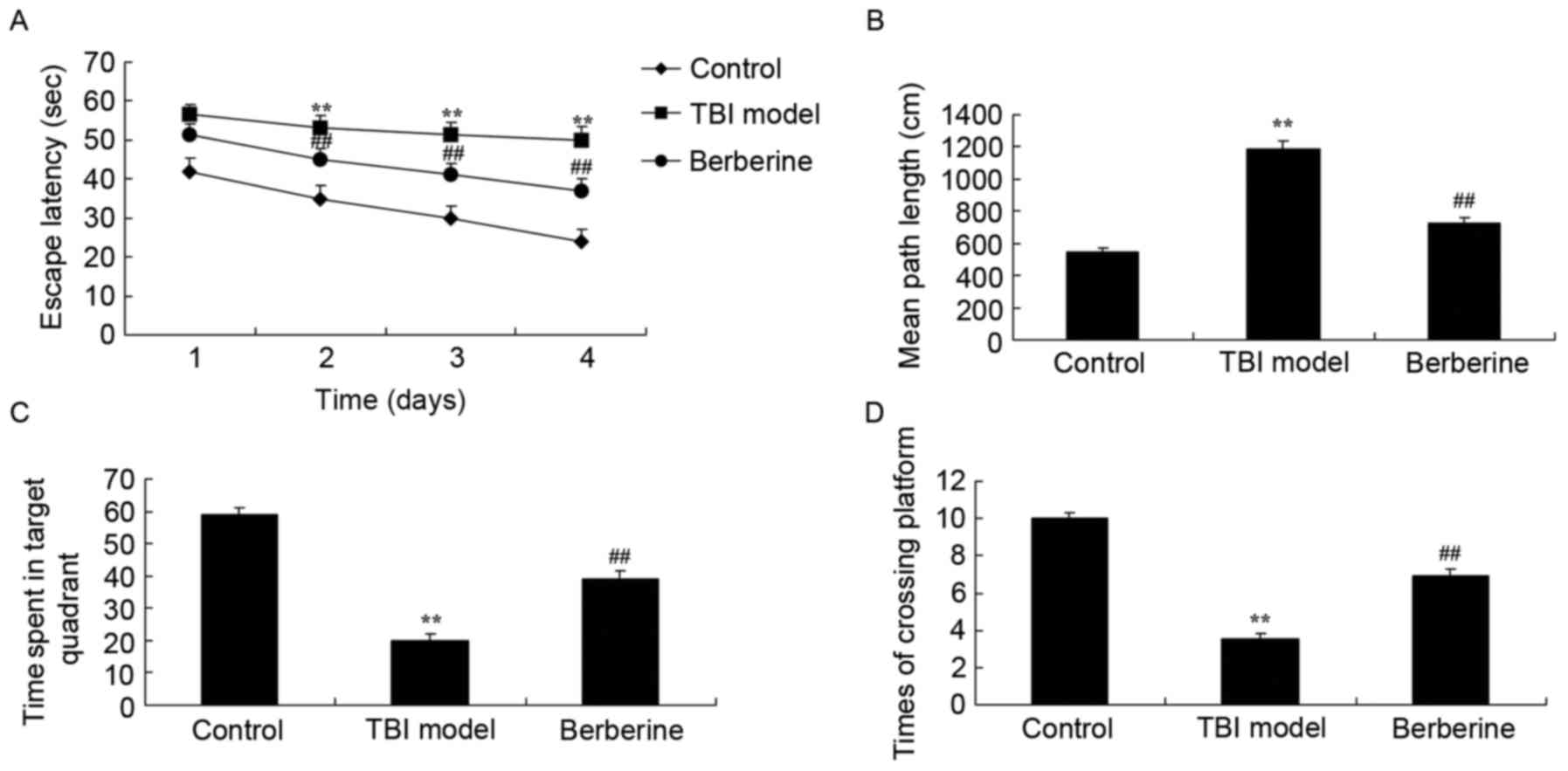
To investigate whether the protective effect of berberine agonist
rescues learning and memory skills in severe TBI, TBI mice were
treated with berberine agonist. As presented in Fig. 2A and B, a significant increase in
escape latency and a longer mean path length were observed in the
TBI model group compared with the control group. The time spent in
the target quadrant and the number of times mice crossed the
platform was decreased in the TBI model group compared with the
control group (Fig. 2C and D).
However, the treatment with berberine agonist significantly
reversed the changes compared with the TBI mice (Fig. 2).
Protective effect of berberine agonist
on choline acetyltransferase (ChAT) and acetylcholinesterase (AchE)
activity
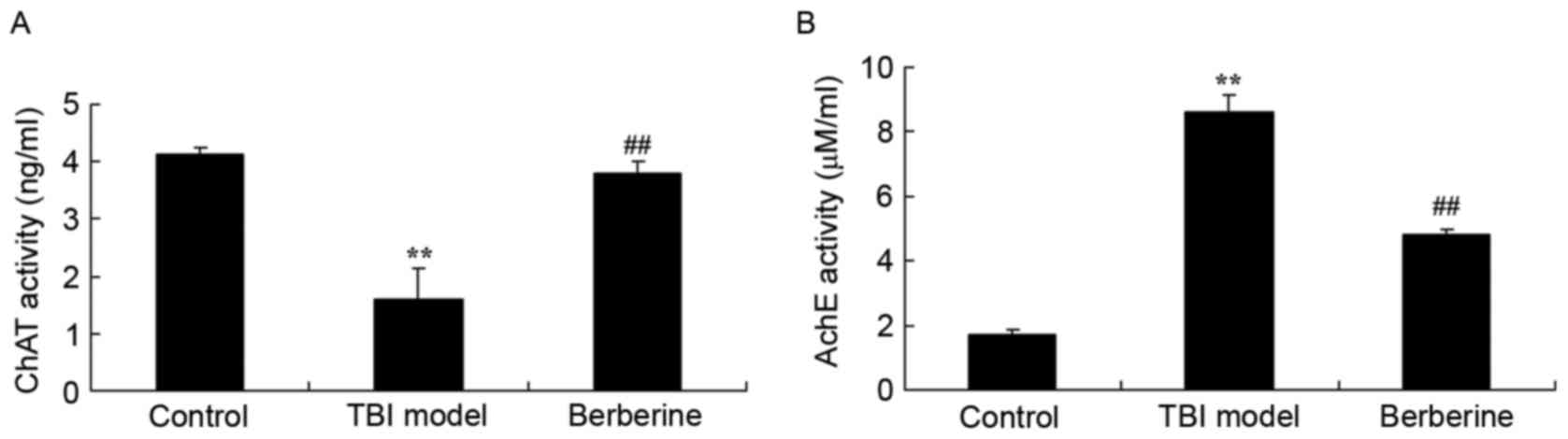
Compared with the control group, TBI inhibited ChAT
activity and induced AchE activity in untreated TBI mice (Fig. 3). Berberine significantly promoted
ChAT activity and inhibited AchE activities in treated TBI mice,
compared with the TBI model group (Fig. 3).
Protective effect of berberine agonist
on MMP-3 and −9 protein expression
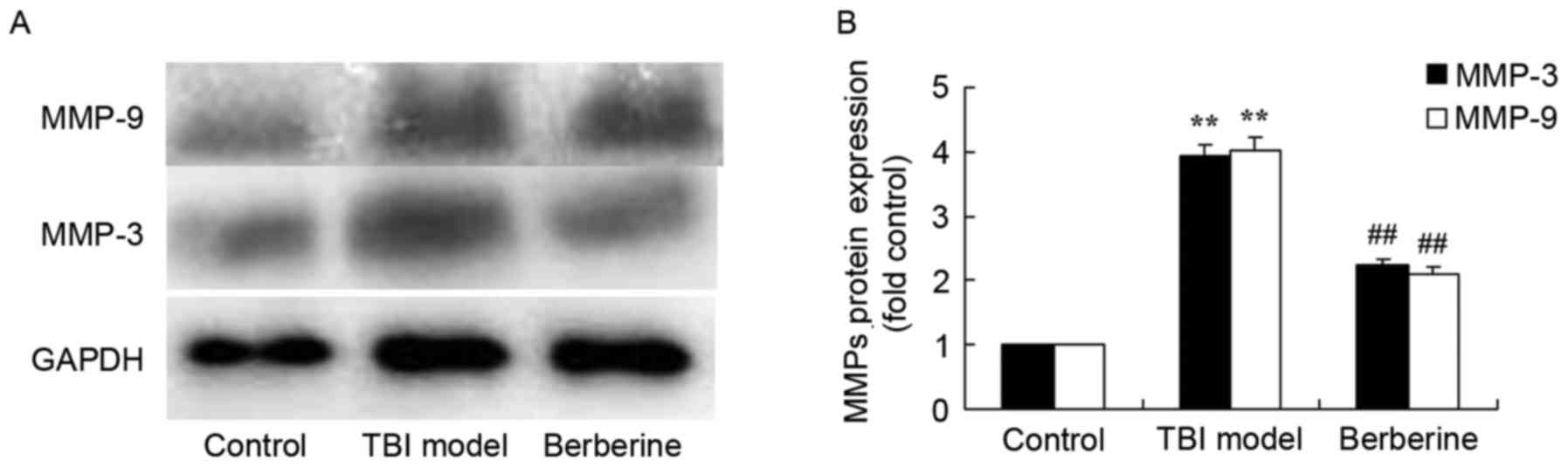
Following treatment with berberine agonist, protein
expression of MMP-3 and −9 in the TBI model group was increased
compared with the control group (Fig.
4). The increase of MMP-3/9 protein expressions in TBI mice was
significantly suppressed by berberine agonist treatment (Fig. 4).
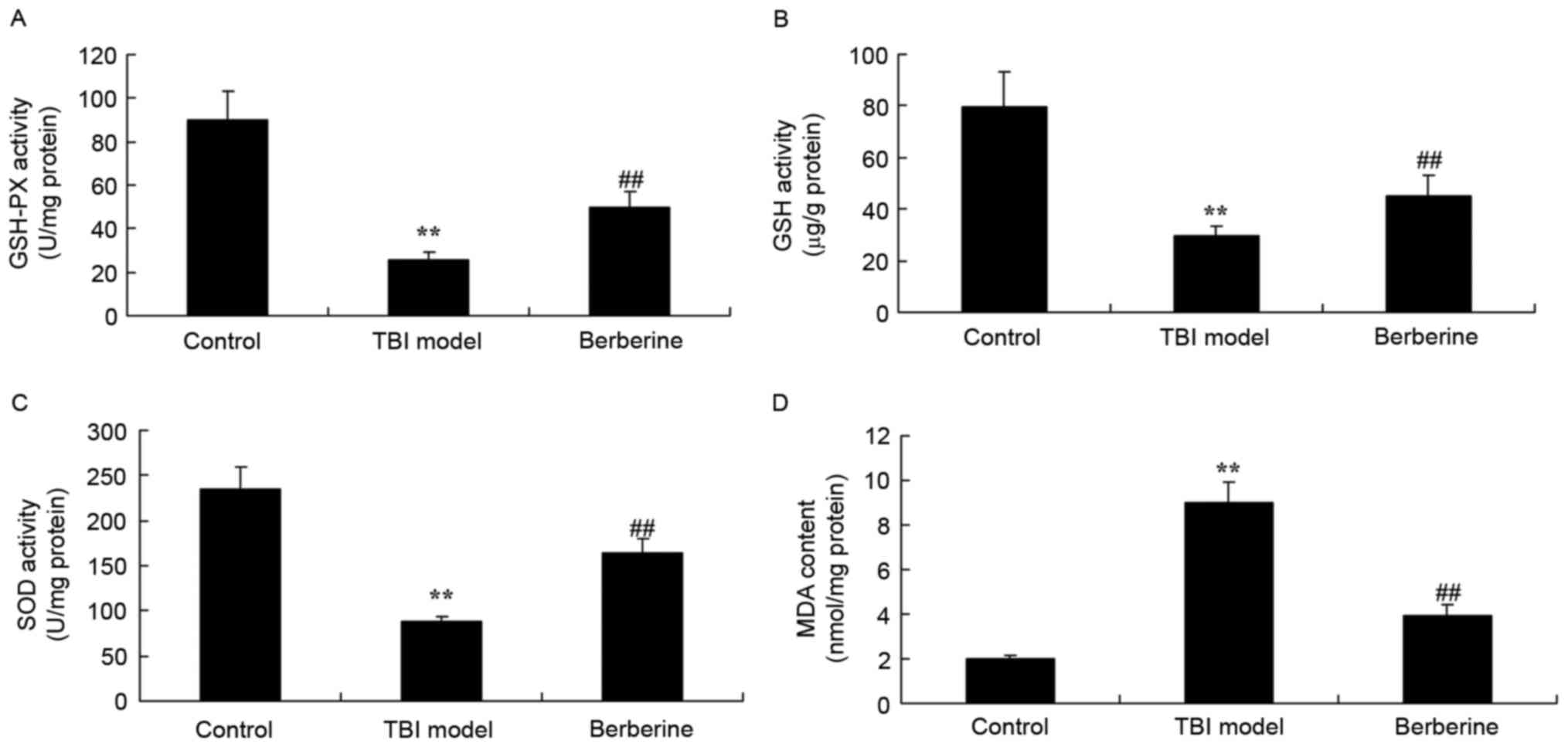
Protective effect of berberine agonist
on oxidative responses in mice
The effect of berberine agonist on TBI, GSH-PX, GSH
and SOD activity, and MDA content was measured. GSH-PX, GSH and SOD
activity was significantly inhibited and MDA level was
significantly increased in the TBI model group compared with the
control group (Fig. 5). Treatment
with berberine agonist significantly increased GSH-PX, GSH and SOD
activity and reduced the MDA level compared with the TBI mice
(Fig. 5).
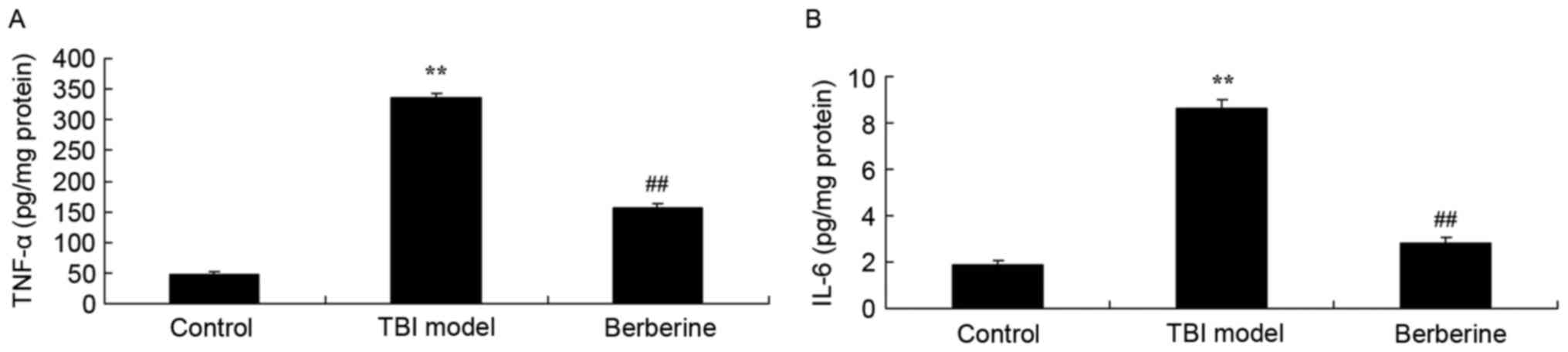
Protective effect of berberine on
inflammation in mice
To determine whether berberine agonist had an effect
on inflammation in TBI, TNF-α and IL-6 levels were measured. As
presented in Fig. 6, the abundance
of TNF-α and IL-6 increased in the TBI group compared with the
control group. Berberine agonist significantly attenuated TNF-α and
IL-6 levels compared with untreated TBI mice (Fig. 6).
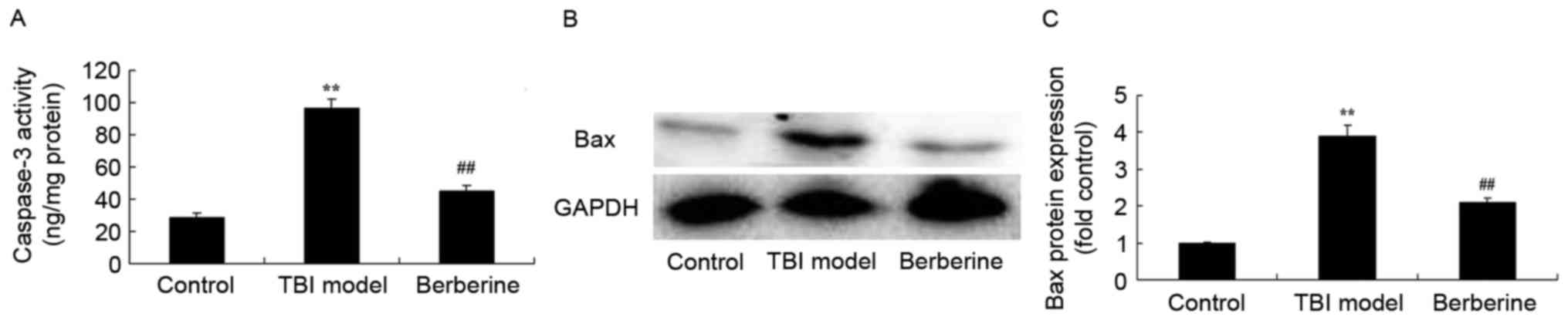
Protective effect of berberine agonist
on apoptosis levels in TBI
To explore the neuroprotective potential of
berberine agonist in the treatment of TBI, the anti-apoptotic
effects were explored. TBI induced a significant increase of
caspase-3 activity and apoptosis regulator BAX (Bax) protein
expression, compared with the control group (Fig. 7). Treatment with berberine agonist
significantly suppressed caspase-3 activity and Bax protein
expression in the treated TBI group compared with the untreated
mice with TBI (Fig. 7).
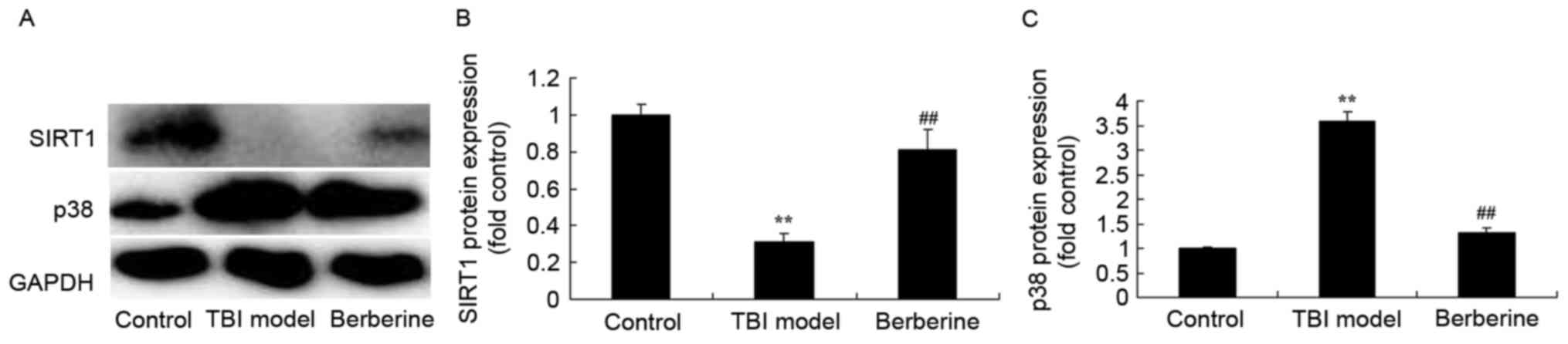
Protective effect of berberine agonist
on Sirt1 protein expression in TBI
To determine the effect of berberine agonist on
Sirt1/FoxO3α protein expression, Sirt1 and p38 mitogen-activated
protein kinase (MAPK) protein expression were measured. The Sirt1
protein expression in the TBI group was lower compared with the
control group, and p38 MAPK protein expression in the TBI group was
higher than in the control group (Fig.
8). Treatment with berberine agonist significantly induced
Sirt1 protein expression and suppressed p38 MAPK protein expression
in the treated TBI group compared with the untreated TBI group
(Fig. 8).
Discussion
TBI is a common trauma, with second highest
morbidity and highest fatality and disability rates among systemic
traumas, making it a prevalent issue in modern society (11). Severe (s)TBI demonstrates high
fatality and disability rates, and poor prognosis (12). At present, sTBI is not curable, and
the treatment for sTBI remains a challenge for neurosurgeons
(13). The results of the present
study demonstrated that the neuroprotective effect of berberine
agonist rescues learning and memory in severe TBI.
TBI can be divided into primary and secondary injury
stages. The primary injury occurs immediately after injury, is
irreversible, and drug interventions are frequently ineffective.
The secondary injury induces changes in the intracerebral
environment, aggravates the primary disease, and is characterized
by long duration and poor prognosis (14). Traditional craniotomy and drug
therapy save lives of numerous patients suffering from sTBI, but
pathological processes such as secondary cerebral neuron apoptosis
and necrosis induced by all kinds of neuron damage factors
(including glutamic acid, calcium overload, radical and
inflammatory mediators) during the primary injury and perioperative
period, cannot be inhibited (15).
Efficient reduction of secondary cerebral injury is key to
improving the prognosis for TBI patients (15). The mechanism of TBI is complex and
involves excessive post-traumatic release of excitatory amino
acids, inflammatory response, imbalance of the activity ion
channels, hydrocephalus, oxygen radical production and neural death
acting simultaneously to trigger a chain reactions, which
eventually lead to death of neurons (6,16).
In the present study, the protective effect of berberine agonist
significantly attenuated inflammation, oxidation and apoptosis
levels in severe TBI mice. Yang et al (8) previously demonstrated that berberine
exerts an anti-inflammatory role in ocular Behcet's disease.
Post-TBI neural death can be divided into a primary
and secondary death. The primary death is referred to as a direct
cell death induced by cell membrane disintegration, and the
secondary or delayed cell death occurs around and away from the
injury sites, and is caused by trauma-induced physiological or
biochemical changes in cells (16). Research on the central nervous
system cell death remains challenging, as characteristics of dead
neurons are different from that of other dead tissue cells even at
an ultrastructure level (17). The
results of the present study demonstrated the protective effect
that Jin et al (10)
previously reported, in which Berberine enhances autophagy and
mitigates high glucose-induced apoptosis of mouse podocytes through
anti-apoptosis effects.
Multiple cells in brain tissue can produce MMPs,
including glial cells, microglia, capillary endothelial cells,
macrophages and neutrophils (18).
MMPs share a common molecular structure of a signal peptide,
propeptide and a catalytic domain from the N- to C-terminal,
respectively (10). A predominant
function of MMPs is degradation of extracellular matrices, and main
components of the basement membrane of blood vessel, including
gelatin, type IV and V collagens, cohesin, elastin and fibronectin
(10,19). An MMP molecule can directly degrade
a certain type or several types of extracellular matrices, or exert
its function through the activation of other types of MMPs,
initiating a cascade effect (20).
MMPs serve important roles in the normal embryonic development and
tissue modeling, and in the genesis and development of some
diseases including membranous nephropathy, polycystic kidney,
atherosclerosis, multiple connective tissue diseases, arthritis and
tumor metastasis (21). In the
present study, berberine agonist significantly suppressed MMP-3 and
−9 proteins in severe TBI mice. Ma et al (10) suggested that berberine inhibits
Chlamydophila pneumoniae infection-induced vascular smooth
muscle cell migration by downregulating the expression levels of
MMP-3 and −9.
Choline acetyltransferase (ChAT) is the generating
enzyme of intracerebral neurotransmitter acetylcholine (ACh)
involved in learning and memory skills. ChAT abundance in
memory-associated cerebral regions is positively correlated with
learning and memory abilities (22). ChAT is a marker for cholinergic
neurons frequently used to estimate the amount of ACh released by
neurons (23). ChAT is synthesized
in cholinergic neuron cell bodies and distributed almost parallel
to Ach (24). Zhang et al
(25) demonstrated that berberine
attenuates brain injury in an aluminum-induced rat model of
neurodegenerative disease.
In conclusion, the present study demonstrated that
the neuroprotective effect of berberine agonist rescues learning
and memory skills in severe TBI, through anti-inflammation,
anti-oxidation and anti-apoptotic effects. This is, to the best of
our knowledge, the first report indicating that berberine agonist
may have a neuroprotective effect on learning and memory through
regulation of Sirt1/p38 MAPK expression.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JW and YZ contributed to the study concept and
design, JW wrote the paper, JW and YZ performed the experiments and
JW and YZ revised the article and approved the final version for
publication.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Gansu Provincial Hospital (Gansu, China).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
References
|
1
|
Wade SL, Kurowski BG, Kirkwood MW, Zhang
N, Cassedy A, Brown TM, Nielsen B, Stancin T and Taylor HG: Online
problem-solving therapy after traumatic brain injury: A randomized
controlled trial. Pediatrics. 135:e487–e495. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hammond FM, Alexander DN, Cutler AJ,
D'Amico S, Doody RS, Sauve W, Zorowitz RD, Davis CS, Shin P, Ledon
F, et al: PRISM II: An open-label study to assess effectiveness of
dextromethorphan/quinidine for pseudobulbar affect in patients with
dementia, stroke or traumatic brain injury. BMC Neurol. 16:892016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang X, Ji J, Fen L and Wang A: Effects of
dexmedetomidine on cerebral blood flow in critically ill patients
with or without traumatic brain injury: A prospective controlled
trial. Brain Inj. 27:1617–1622. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Saxena MK, Taylor C, Billot L, Bompoint S,
Gowardman J, Roberts JA, Lipman J and Myburgh J: The effect of
paracetamol on core body temperature in acute traumatic brain
injury: A randomised, controlled clinical trial. PLoS One.
10:e01447402015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Du G, Zhao Z, Chen Y, Li Z, Tian Y, Liu Z,
Liu B and Song J: Quercetin attenuates neuronal autophagy and
apoptosis in rat traumatic brain injury model via activation of
PI3K/Akt signaling pathway. Neurol Res. Oct 3–2016.(Epub ahead of
print). View Article : Google Scholar :
|
|
6
|
Chuang CH, Hsu YC, Wang CC, Hu C and Kuo
JR: Cerebral blood flow and apoptosis-associated factor with
electroacupuncture in a traumatic brain injury rat model. Acupunct
Med. 31:395–403. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hu ZG, Wang HD, Qiao L, Yan W, Tan QF and
Yin HX: The protective effect of the ketogenic diet on traumatic
brain injury-induced cell death in juvenile rats. Brain Inj.
23:459–465. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang Y, Wang Q, Xie M, Liu P, Qi X, Liu X
and Li Z: Berberine exerts an anti-inflammatory role in ocular
Behcet's disease. Mol Med Rep. 15:97–102. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Habtemariam S: Berberine and inflammatory
bowel disease: A concise review. Pharmacol Res. 113:592–599. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ma L and Zhang L, Wang B, Wei J, Liu J and
Zhang L: Berberine inhibits Chlamydia pneumoniae infection-induced
vascular smooth muscle cell migration through downregulating MMP3
and MMP9 via PI3K. Eur J Pharmacol. 755:102–109. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
NICE-SUGAR Study Investigators for the
Australian and New Zealand Intensive Care Society Clinical Trials
Group and the Canadian Critical Care Trials Group, . Finfer S,
Chittock D, Li Y, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P,
Hebert P, et al: Intensive versus conventional glucose control in
critically ill patients with traumatic brain injury: Long-term
follow-up of a subgroup of patients from the NICE-SUGAR study.
Intensive Care Med. 41:1037–1047. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Matuseviciene G, Borg J, Stålnacke BM,
Ulfarsson T and de Boussard C: Early intervention for patients at
risk for persisting disability after mild traumatic brain injury: A
randomized, controlled study. Brain Inj. 27:318–324. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nägeli M, Fasshauer M, Sommerfeld J,
Fendel A, Brandi G and Stover JF: Prolonged continuous intravenous
infusion of the dipeptide L-alanine-L-glutamine significantly
increases plasma glutamine and alanine without elevating brain
glutamate in patients with severe traumatic brain injury. Crit
Care. 18:R1392014. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu S, Zhang L, Wu Q, Wu Q and Wang T:
Chemokine CCL2 induces apoptosis in cortex following traumatic
brain injury. J Mol Neurosci. 51:1021–1029. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ge X, Huang S, Gao H, Han Z, Chen F, Zhang
S, Wang Z, Kang C, Jiang R, Yue S, et al: miR-21-5p alleviates
leakage of injured brain microvascular endothelial barrier in vitro
through suppressing inflammation and apoptosis. Brain Res.
1650:31–40. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bentz K, Molcanyi M, Schneider A, Riess P,
Maegele M, Bosche B, Hampl JA, Hescheler J, Patz S and Schäfer U:
Extract derived from rat brains in the acute phase following
traumatic brain injury impairs survival of undifferentiated stem
cells and induces rapid differentiation of surviving cells. Cell
Physiol Biochem. 26:821–830. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu SJ, Zou Y, Belegu V, Lv LY, Lin N,
Wang TY, McDonald JW, Zhou X, Xia QJ and Wang TH: Co-grafting of
neural stem cells with olfactory en sheathing cells promotes
neuronal restoration in traumatic brain injury with an
anti-inflammatory mechanism. J Neuroinflammation. 11:662014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Reinhard SM, Razak K and Ethell IM: A
delicate balance: Role of MMP-9 in brain development and
pathophysiology of neurodevelopmental disorders. Front Cell
Neurosci. 9:2802015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Grossetete M, Phelps J, Arko L, Yonas H
and Rosenberg GA: Elevation of matrix metalloproteinases 3 and 9 in
cerebrospinal fluid and blood in patients with severe traumatic
brain injury. Neurosurgery. 65:702–708. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wiggins-Dohlvik K, Merriman M, Shaji CA,
Alluri H, Grimsley M, Davis ML, Smith RW and Tharakan B: Tumor
necrosis factor-α disruption of brain endothelial cell barrier is
mediated through matrix metalloproteinase-9. Am J Surg.
208:954–960. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang Y, Fan X, Tang T, Fan R, Zhang C,
Huang Z, Peng W, Gan P, Xiong X, Huang W and Huang X: Rhein and
rhubarb similarly protect the blood-brain barrier after
experimental traumatic brain injury via gp91phox subunit of NADPH
oxidase/ROS/ERK/MMP-9 signaling pathway. Sci Rep. 6:370982016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dixon CE, Flinn P, Bao J, Venya R and
Hayes RL: Nerve growth factor attenuates cholinergic deficits
following traumatic brain injury in rats. Exp Neurol. 146:479–490.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cha Y, Lee SH, Jang SK, Guo H, Ban YH,
Park D, Jang GY, Yeon S, Lee JY, Choi EK, et al: A silk peptide
fraction restores cognitive function in AF64A-induced Alzheimer
disease model rats by increasing expression of choline
acetyltransferase gene. Toxicol Appl Pharmacol. 314:48–54. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pineda RG, Neil J, Dierker D, Smyser CD,
Wallendorf M, Kidokoro H, Reynolds LC, Walker S, Rogers C, Mathur
AM, et al: Alterations in brain structure and neurodevelopmental
outcome in preterm infants hospitalized in different neonatal
intensive care unit environments. J Pediatr. 164(52–60): e22014.
View Article : Google Scholar
|
|
25
|
Zhang J, Yang JQ, He BC, Zhou QX, Yu HR,
Tang Y and Liu BZ: Berberine and total base from rhizoma Coptis
chinensis attenuate brain injury in an aluminum-induced rat
model of neurodegenerative disease. Saudi Med J. 30:760–766.
2009.PubMed/NCBI
|