|
1
|
McCaffrey J, Lennon R and Webb NJ: The
non-immunosuppressive management of childhood nephrotic syndrome.
Pediatr Nephrol. 31:1383–1402. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhao X, Hwang DY and Kao HY: The role of
glucocorticoid receptors in podocytes and nephrotic syndrome. Nucl
Receptor Res. 5:52018. View Article : Google Scholar
|
|
3
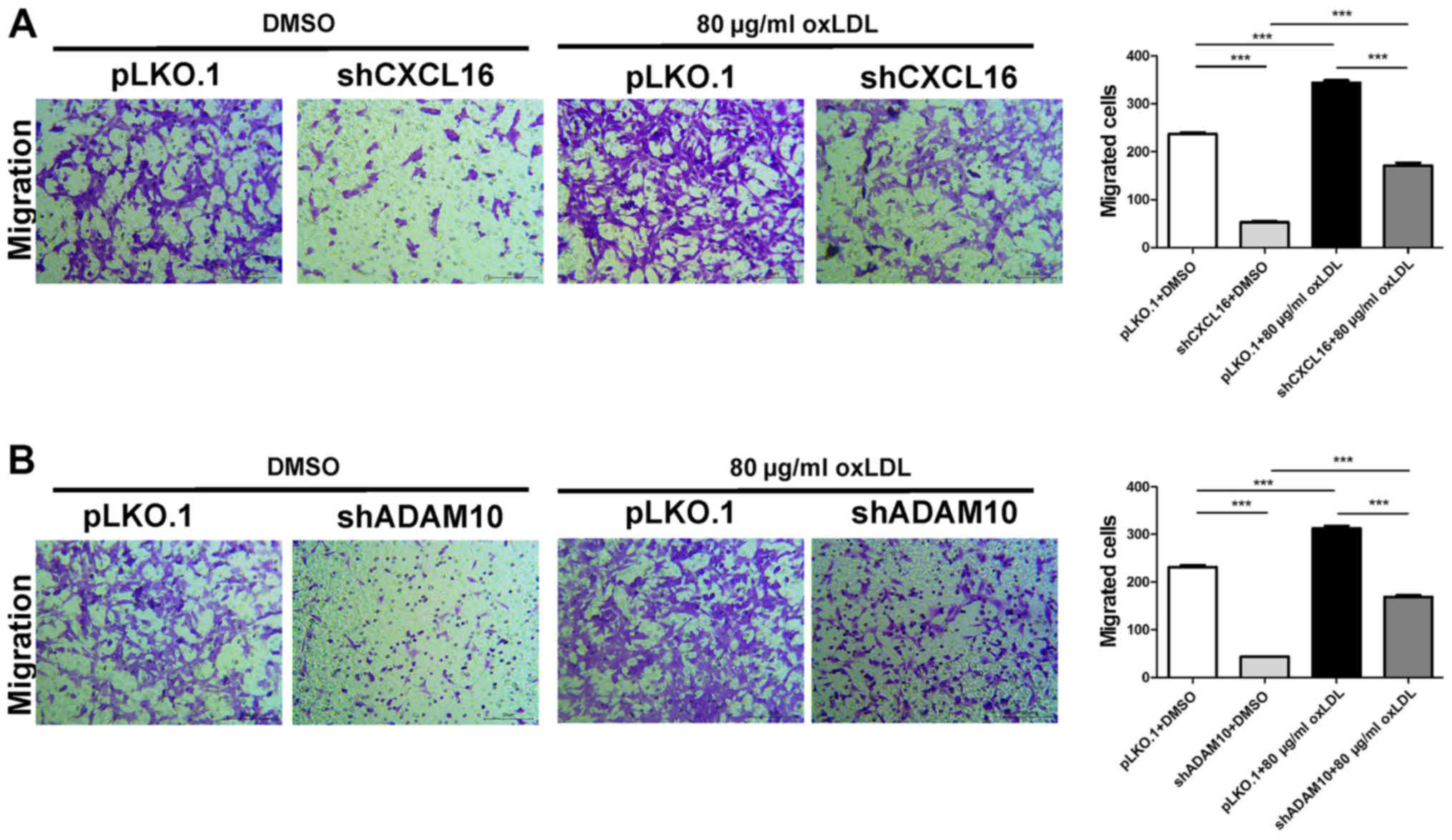
|
Ranganathan S: Pathology of
podocytopathies causing nephrotic syndrome in children. Front
Pediatr. 4:322016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fornoni A, Merscher S and Kopp JB: Lipid
biology of the podocyte - new perspectives offer new opportunities.
Nat Rev Nephrol. 10:379–388. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu M, Fan M, Zhen J, Lin J, Wang Q, Lv Z
and Wang R: FAK contributes to proteinuria in hypercholesterolaemic
rats and modulates podocyte F-actin re-organization via activating
p38 in response to ox-LDL. J Cell Mol Med. 21:552–567. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mertens A and Holvoet P: Oxidized LDL and
HDL: Antagonists in atherothrombosis. FASEB J. 15:2073–2084. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang F, Wang C, Wang H, Lu M, Li Y, Feng
H, Lin J, Yuan Z and Wang X: Ox-LDL promotes migration and adhesion
of bone marrow-derived mesenchymal stem cells via regulation of
MCP-1 expression. Mediators Inflamm. 2013:6910232013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rubina K, Talovskaya E, Cherenkov V,
Ivanov D, Stambolsky D, Storozhevykh T, Pinelis V, Shevelev A,
Parfyonova Y, Resink T, et al: LDL induces intracellular signalling
and cell migration via atypical LDL-binding protein T-cadherin. Mol
Cell Biochem. 273:33–41. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liang H, Liao M, Zhao W, Zheng X, Xu F,
Wang H and Huang J: CXCL16/ROCK1 signaling pathway exacerbates
acute kidney injury induced by ischemia-reperfusion. Biomed
Pharmacother. 98:347–356. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kato T, Hagiyama M and Ito A: Renal ADAM10
and 17: Their physiological and medical meanings. Front Cell Dev
Biol. 6:1532018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hu ZB, Chen Y, Gong YX, Gao M, Zhang Y,
Wang GH, Tang RN, Liu H, Liu BC and Ma KL: Activation of the
CXCL16/CXCR6 pathway by inflammation contributes to atherosclerosis
in patients with end-stage renal disease. Int J Med Sci.
13:858–867. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fang Y, Henderson FC Jr, Yi Q, Lei Q, Li Y
and Chen N: Chemokine CXCL16 expression suppresses migration and
invasiveness and induces apoptosis in breast cancer cells.
Mediators Inflamm. 2014:4786412014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Garcia GE, Truong LD, Li P, Zhang P,
Johnson RJ, Wilson CB and Feng L: Inhibition of CXCL16 attenuates
inflammatory and progressive phases of anti-glomerular basement
membrane antibody-associated glomerulonephritis. Am J Pathol.
170:1485–1496. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
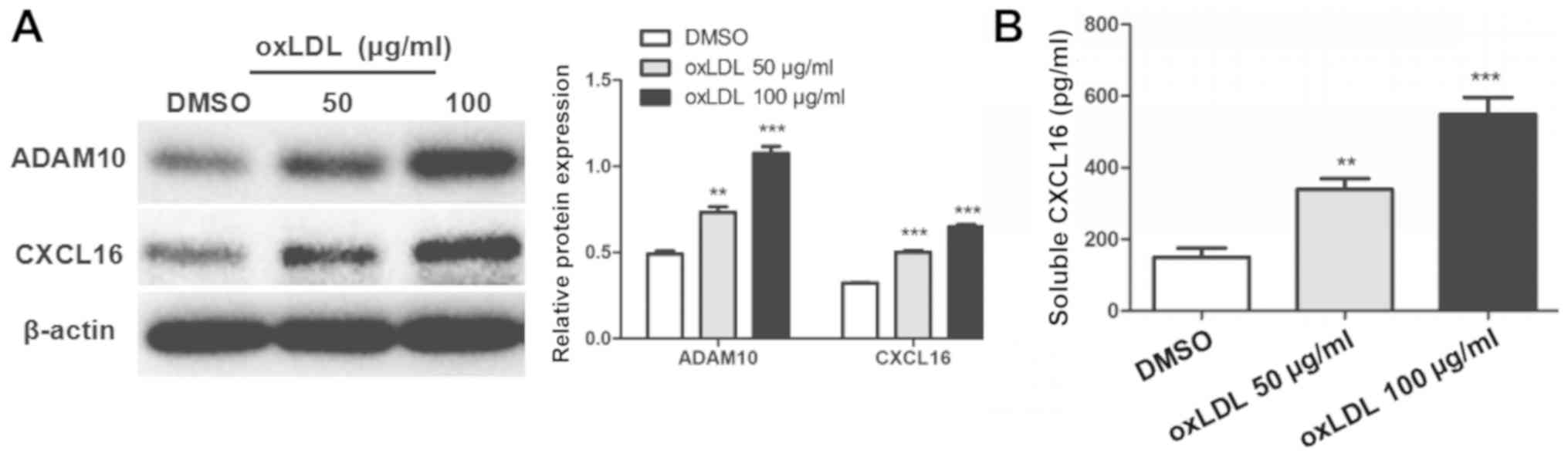
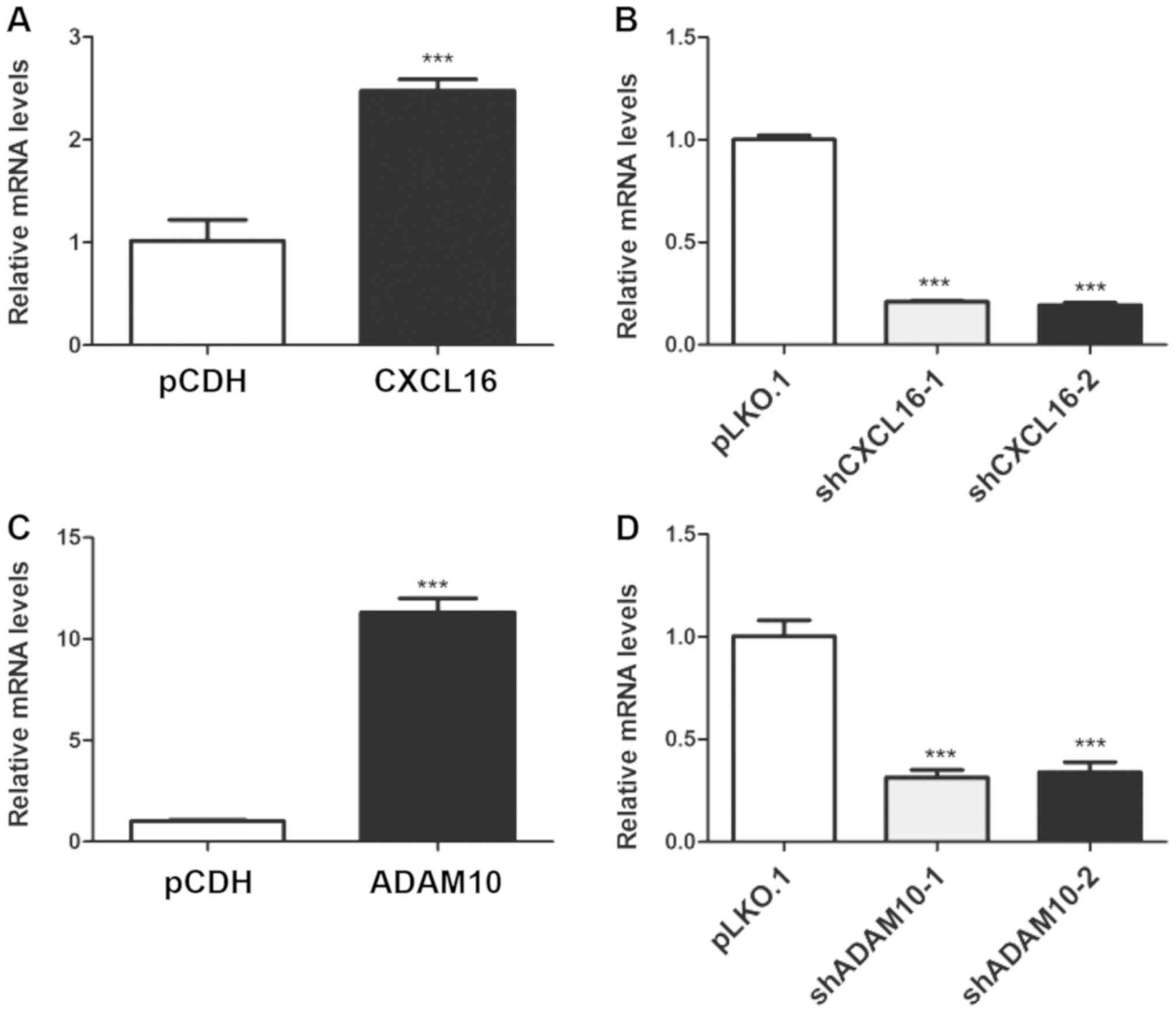
Schramme A, Abdel-Bakky MS, Gutwein P,
Obermüller N, Baer PC, Hauser IA, Ludwig A, Gauer S, Schäfer L,
Sobkowiak E, et al: Characterization of CXCL16 and ADAM10 in the
normal and transplanted kidney. Kidney Int. 74:328–338. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gutwein P, Abdel-Bakky MS, Schramme A,
Doberstein K, Kämpfer-Kolb N, Amann K, Hauser IA, Obermüller N,
Bartel C, Abdel-Aziz AA, et al: CXCL16 is expressed in podocytes
and acts as a scavenger receptor for oxidized low-density
lipoprotein. Am J Pathol. 174:2061–2072. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schramme A, Abdel-Bakky MS, Kämpfer-Kolb
N, Pfeilschifter J and Gutwein P: The role of CXCL16 and its
processing metalloproteinases ADAM10 and ADAM17 in the
proliferation and migration of human mesangial cells. Biochem
Biophys Res Commun. 370:311–316. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
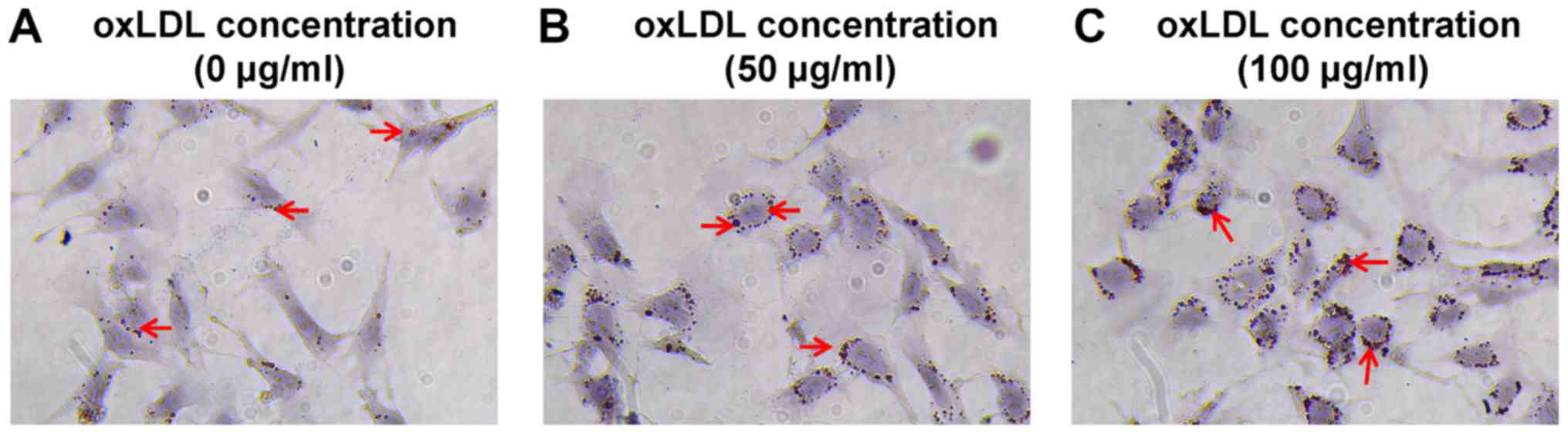
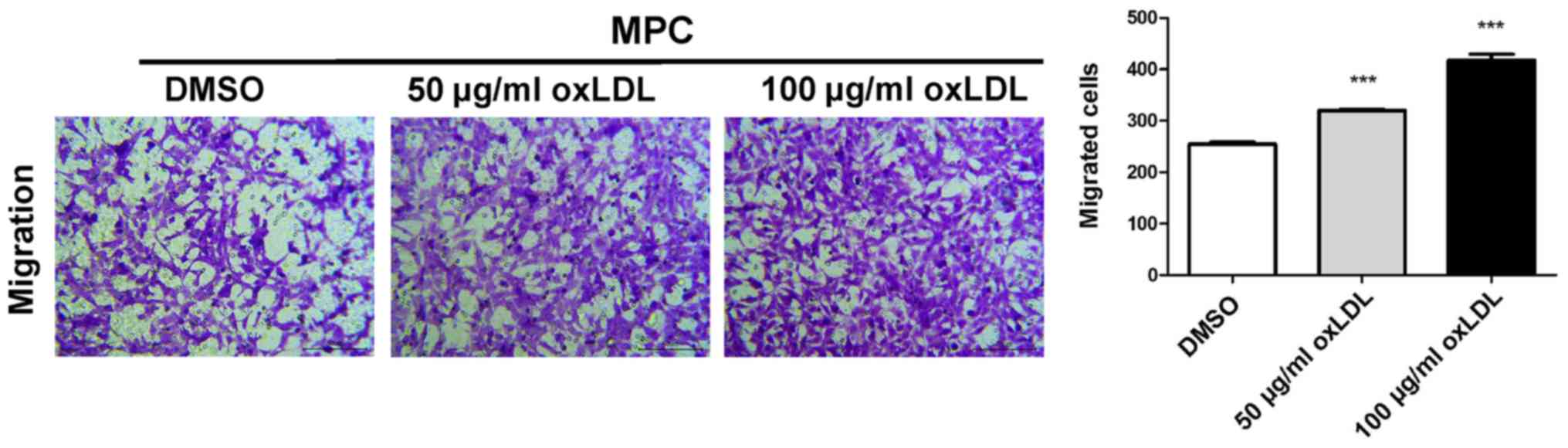
Wang L, Sun S, Zhou A, Yao X and Wang Y:
oxLDL-induced lipid accumulation in glomerular podocytes: Role of
IFN-γ, CXCL16, and ADAM10. Cell Biochem Biophys. 70:529–538. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Davin JC: The glomerular permeability
factors in idiopathic nephrotic syndrome. Pediatr Nephrol.
31:207–215. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kalluri R: Proteinuria with and without
renal glomerular podocyte effacement. J Am Soc Nephrol.
17:2383–2389. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Assady S, Wanner N, Skorecki KL and Huber
TB: New insights into podocyte biology in glomerular health and
disease. J Am Soc Nephrol. 28:1707–1715. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Reiser J and Altintas M: Podocytes.
F1000Res. 5:1142016. View Article : Google Scholar
|
|
23
|
Tan X, Chen Y, Liang X, Yu C, Lai Y, Zhang
L, Zhao X, Zhang H, Lin T, Li R, et al: Lipopolysaccharide-induced
podocyte injury is mediated by suppression of autophagy. Mol Med
Rep. 14:811–818. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Greka A and Mundel P: Cell biology and
pathology of podocytes. Annu Rev Physiol. 74:299–323. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lin T, Zhang L, Liu S, Chen Y, Zhang H,
Zhao X, Li R, Zhang Q, Liao R, Huang Z, et al: WWC1 promotes
podocyte survival via stabilizing slit diaphragm protein dendrin.
Mol Med Rep. 16:8685–8690. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Akchurin O and Reidy KJ: Genetic causes of
proteinuria and nephrotic syndrome: Impact on podocyte
pathobiology. Pediatr Nephrol. 30:221–233. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yu SM, Nissaisorakarn P, Husain I and Jim
B: Proteinuric kidney diseases: A Podocyte's slit diaphragm and
cytoskeleton approach. Front Med (Lausanne). 5:2212018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vallon V and Komers R: Pathophysiology of
the diabetic kidney. Compr Physiol. 1:1175–1232. 2011.PubMed/NCBI
|
|
29
|
Noris M and Remuzzi G: Non-muscle myosins
and the podocyte. Clin Kidney J. 5:94–101. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jin X, Wang W, Mao J, Shen H, Fu H, Wang
X, Gu W, Liu A, Yu H, Shu Q, et al: Overexpression of Myo1e in
mouse podocytes enhances cellular endocytosis, migration, and
adhesion. J Cell Biochem. 115:410–419. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kistler AD, Altintas MM and Reiser J:
Podocyte GTPases regulate kidney filter dynamics. Kidney Int.
81:1053–1055. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cechova S, Dong F, Chan F, Kelley MJ, Ruiz
P and Le TH: MYH9 E1841K mutation augments proteinuria and podocyte
injury and migration. J Am Soc Nephrol. 29:155–167. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Shao H, Wang JH, Pollak MR and Wells A:
α-actinin-4 is essential for maintaining the spreading, motility
and contractility of fibroblasts. PLoS One. 5:e139212010.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Duning K, Schurek EM, Schlüter M, Bayer M,
Reinhardt HC, Schwab A, Schaefer L, Benzing T, Schermer B, Saleem
MA, et al: KIBRA modulates directional migration of podocytes. J Am
Soc Nephrol. 19:1891–1903. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Fernández D, Horrillo A, Alquezar C,
González-Manchón C, Parrilla R and Ayuso MS: Control of cell
adhesion and migration by podocalyxin. Implication of Rac1 and
Cdc42. Biochem Biophys Res Commun. 432:302–307. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Mundel P and Reiser J: Proteinuria: An
enzymatic disease of the podocyte? Kidney Int. 77:571–580. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li Z, Zhang L, Shi W, Chen Y, Zhang H, Liu
S, Liang X, Ling T, Yu C, Huang Z, et al: Spironolactone inhibits
podocyte motility via decreasing integrin β1 and increasing
integrin β3 in podocytes under high-glucose conditions. Mol Med
Rep. 12:6849–6854. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Shao H, Travers T, Camacho CJ and Wells A:
The carboxyl tail of alpha-actinin-4 regulates its susceptibility
to m-calpain and thus functions in cell migration and spreading.
Int J Biochem Cell Biol. 45:1051–1063. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Michaud JL, Chaisson KM, Parks RJ and
Kennedy CR: FSGS-associated alpha-actinin-4 (K256E) impairs
cytoskeletal dynamics in podocytes. Kidney Int. 70:1054–1061. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Feng D, DuMontier C and Pollak MR: The
role of alpha-actinin-4 in human kidney disease. Cell Biosci.
5:442015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wang P, Zhao F, Nie X, Liu J and Yu Z:
Knockdown of NUP160 inhibits cell proliferation, induces apoptosis,
autophagy and cell migration, and alters the expression and
localization of podocyte associated molecules in mouse podocytes.
Gene. 664:12–21. 2018. View Article : Google Scholar : PubMed/NCBI
|