|
1
|
Ouyang G, Liu Q, Wu Y, Liu Z, Lu W, Li S,
Pan G and Chen X: The global, regional, and national burden of
gallbladder and biliary tract cancer and its attributable risk
factors in 195 countries and territories, 1990 to 2017: A
systematic analysis for the Global Burden of Disease Study 2017.
Cancer. 127:2238–2250. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Baiu I and Visser B: Gallbladder cancer.
JAMA. 320:12942018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang X, Kong Z, Xu X, Yun X, Chao J, Ding
D, Li T, Gao Y, Guan N, Zhu C and Qin X: ARRB1 drives gallbladder
cancer progression by facilitating TAK1/MAPK signaling activation.
J Cancer. 12:1926–1935. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sharma A, Sharma KL, Gupta A, Yadav A and
Kumar A: Gallbladder cancer epidemiology, pathogenesis and
molecular genetics: Recent update. World J Gastroenterol.
23:3978–3998. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu YP, Jin YP, Wu XS, Yang Y, Li YS, Li
HF, Xiang SS, Song XL, Jiang L, Zhang YJ, et al: LncRNA-HGBC
stabilized by HuR promotes gallbladder cancer progression by
regulating miR-502-3p/SET/AKT axis. Mol Cancer. 18:1672019.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim M, Kim H, Han Y, Sohn H, Kang JS, Kwon
W and Jang JY: Prognostic value of carcinoembryonic antigen (CEA)
and carbohydrate antigen 19-9 (CA 19-9) in gallbladder cancer; 65
IU/ml of CA 19-9 is the new cut-off value for prognosis. Cancers
(Basel). 13:10892021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li M, Liu F, Zhang F, Zhou W, Jiang X,
Yang Y, Qu K, Wang Y, Ma Q, Wang T, et al: Genomic ERBB2/ERBB3
mutations promote PD-L1-mediated immune escape in gallbladder
cancer: A whole-exome sequencing analysis. Gut. 68:1024–1033. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen X, Wu X, Wu H, Gu Y, Shao Y, Shao Q,
Zhu F, Li X, Qian X, Hu J, et al: Camrelizumab plus gemcitabine and
oxaliplatin (GEMOX) in patients with advanced biliary tract cancer:
A single-arm, open-label, phase II trial. J Immunother Cancer.
8:e0012402020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Giguère V, Yang N, Segui P and Evans RM:
Identification of a new class of steroid hormone receptors. Nature.
331:91–94. 1988. View
Article : Google Scholar
|
|
10
|
Deblois G and Giguère V: Functional and
physiological genomics of estrogen-related receptors (ERRs) in
health and disease. Biochim Biophys Acta. 1812:1032–1040. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim SY, Yang CS, Lee HM, Kim JK, Kim YS,
Kim YR, Kim JS, Kim TS, Yuk JM, Dufour CR, et al: ESRRA
(estrogen-related receptor α) is a key coordinator of
transcriptional and post-translational activation of autophagy to
promote innate host defense. Autophagy. 14:152–168. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Deblois G, Hall JA, Perry MC, Laganière J,
Ghahremani M, Park M, Hallett M and Giguère V: Genome-wide
identification of direct target genes implicates estrogen-related
receptor alpha as a determinant of breast cancer heterogeneity.
Cancer Res. 69:6149–6157. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Luo C, Widlund HR and Puigserver P: PGC-1
coactivators: Shepherding the mitochondrial biogenesis of tumors.
Trends Cancer. 2:619–631. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huss JM, Kopp RP and Kelly DP: Peroxisome
proliferator-activated receptor coactivator-1alpha (PGC-1alpha)
coactivates the cardiac-enriched nuclear receptors estrogen-related
receptor-alpha and -gamma. Identification of novel leucine-rich
interaction motif within PGC-1alpha. J Biol Chem. 277:40265–40274.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang Y, Li S, Li B, Li Y, Xia K, Aman S,
Yang Y, Ahmad B, Zhao B and Wu H: FBXL10 promotes ERRα protein
stability and proliferation of breast cancer cells by enhancing the
mono-ubiquitylation of ERRα. Cancer Lett. 502:108–119. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gaillard S, Grasfeder LL, Haeffele CL,
Lobenhofer EK, Chu TM, Wolfinger R, Kazmin D, Koves TR, Muoio DM,
Chang CY, et al: Receptor-selective coactivators as tools to define
the biology of specific receptor-coactivator pairs. Mol Cell.
24:797–803. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
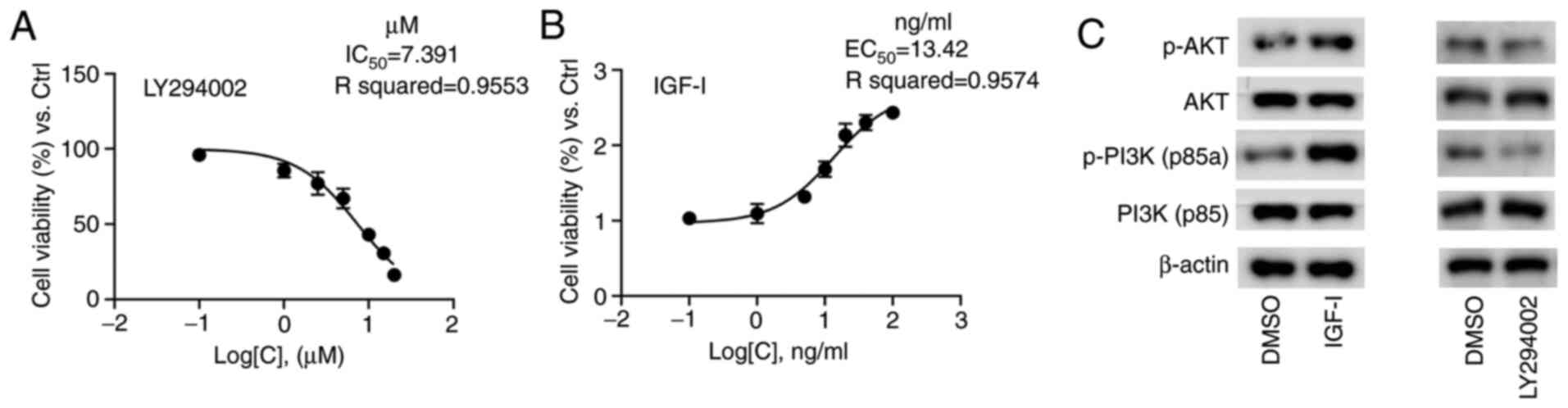
Mayer IA and Arteaga CL: The PI3K/AKT
pathway as a target for cancer treatment. Annu Rev Med. 67:11–28.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang F, Xie HY, Yang LF, Zhang L, Zhang
FL, Liu HY, Li DQ and Shao ZM: Stabilization of MORC2 by estrogen
and antiestrogens through GPER1-PRKACA-CMA pathway contributes to
estrogen-induced proliferation and endocrine resistance of breast
cancer cells. Autophagy. 16:1061–1076. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xia P, Gütl D, Zheden V and Heisenberg CP:
Lateral inhibition in cell specification mediated by mechanical
signals modulating TAZ activity. Cell. 176:1379–1392.e14. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lu Y, Tao F, Zhou MT and Tang KF: The
signaling pathways that mediate the anti-cancer effects of caloric
restriction. Pharmacol Res. 141:512–520. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Girnita L, Worrall C, Takahashi S,
Seregard S and Girnita A: Something old, something new and
something borrowed: Emerging paradigm of insulin-like growth factor
type 1 receptor (IGF-1R) signaling regulation. Cell Mol Life Sci.
71:2403–2427. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
LeRoith D, Werner H, Beitner-Johnson D and
Roberts CT Jr: Molecular and cellular aspects of the insulin-like
growth factor I receptor. Endocr Rev. 16:143–163. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Myers MG Jr, Backer JM, Sun XJ, Shoelson
S, Hu P, Schlessinger J, Yoakim M, Schaffhausen B and White MF:
IRS-1 activates phosphatidylinositol 3′-kinase by associating with
src homology 2 domains of p85. Proc Natl Acad Sci USA.
89:10350–10354. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vanhaesebroeck B and Alessi DR: The
PI3K-PDK1 connection: More than just a road to PKB. Biochem J.
346:561–576. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang L, Yang M, Guo X, Yang Z, Liu S, Ji Y
and Jin H: Estrogen-related receptor-α promotes gallbladder cancer
development by enhancing the transcription of Nectin-4. Cancer Sci.
111:1514–1527. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang Y, Liu S, Wang L, Wu Y, Hao J, Wang
Z, Lu W, Wang XA, Zhang F, Cao Y, et al: A novel PI3K/AKT signaling
axis mediates Nectin-4-induced gallbladder cancer cell
proliferation, metastasis and tumor growth. Cancer Lett.
375:179–189. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chang CY, Kazmin D, Jasper JS, Kunder R,
Zuercher WJ and McDonnell DP: The metabolic regulator ERRα, a
downstream target of HER2/IGF-1R, as a therapeutic target in breast
cancer. Cancer Cell. 20:500–510. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Theodoris CV, Zhou P, Liu L, Zhang Y,
Nishino T, Huang Y, Kostina A, Ranade SS, Gifford CA, Uspenskiy V,
et al: Network-based screen in iPSC-derived cells reveals
therapeutic candidate for heart valve disease. Science.
371:eabd07242021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ramaswamy A, Ostwal V, Sharma A, Bhargava
P, Srinivas S, Goel M, Patkar S, Mandavkar S, Jadhav P, Parulekar
M, et al: Efficacy of capecitabine plus irinotecan vs irinotecan
monotherapy as second-line treatment in patients with advanced
gallbladder cancer: A multicenter phase 2 randomized clinical trial
(GB-SELECT). JAMA Oncol. 7:436–439. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nepal C, Zhu B, O'Rourke CJ, Bhatt DK, Lee
D, Song L, Wang D, Van Dyke A, Choo-Wosoba H, Liu Z, et al:
Integrative molecular characterization of gallbladder cancer
reveals microenvironment-associated subtypes. J Hepatol.
74:1132–1144. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ranhotra HS: Estrogen-related receptor
alpha and cancer: Axis of evil. J Recept Signal Transduct Res.
35:505–508. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mercurio L, Albanesi C and Madonna S:
Recent updates on the involvement of PI3K/AKT/mTOR molecular
cascade in the pathogenesis of hyperproliferative skin disorders.
Front Med (Lausanne). 8:6656472021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Song M, Bode AM, Dong Z and Lee MH: AKT as
a therapeutic target for cancer. Cancer Res. 79:1019–1031. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Villena JA: New insights into PGC-1
coactivators: Redefining their role in the regulation of
mitochondrial function and beyond. FEBS J. 282:647–672. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lin J, Handschin C and Spiegelman BM:
Metabolic control through the PGC-1 family of transcription
coactivators. Cell Metab. 1:361–370. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Patten IS and Arany Z: PGC-1 coactivators
in the cardiovascular system. Trends Endocrinol Metab. 23:90–97.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li S, Liu C, Li N, Hao T, Han T, Hill DE,
Vidal M and Lin JD: Genome-wide coactivation analysis of PGC-1alpha
identifies BAF60a as a regulator of hepatic lipid metabolism. Cell
Metab. 8:105–117. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Vernier M and Giguère V: Aging, senescence
and mitochondria: The PGC-1/ERR axis. J Mol Endocrinol. 66:R1–R14.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Chambers JM and Wingert RA: PGC-1α in
disease: Recent renal insights into a versatile metabolic
regulator. Cells. 9:22342020. View Article : Google Scholar : PubMed/NCBI
|