|
1
|
Boursier J, Roux M, Costentin C, Chaigneau
J, Fournier-Poizat C, Trylesinski A, Canivet CM, Michalak S, Le
Bail B, Paradis V, et al: Practical diagnosis of cirrhosis in
non-alcoholic fatty liver disease using currently available
non-invasive fibrosis tests. Nat Commun. 14:52192023. View Article : Google Scholar : PubMed/NCBI
|
|
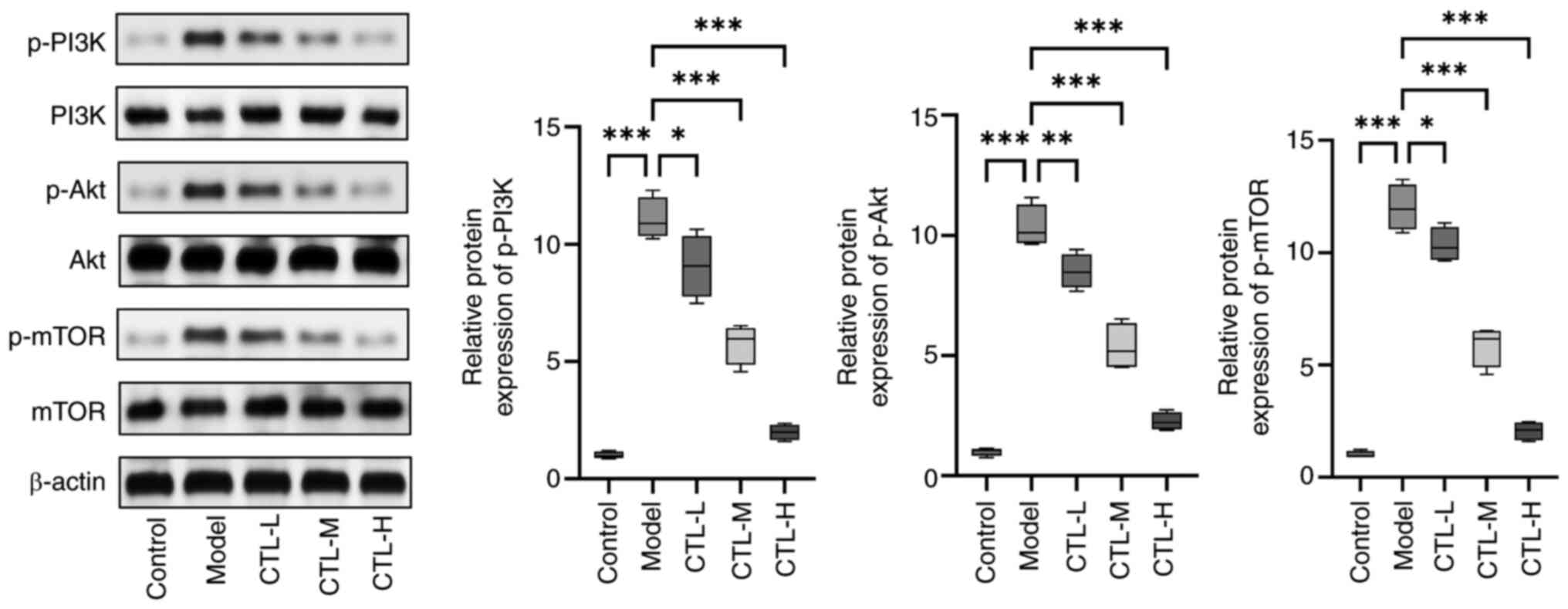
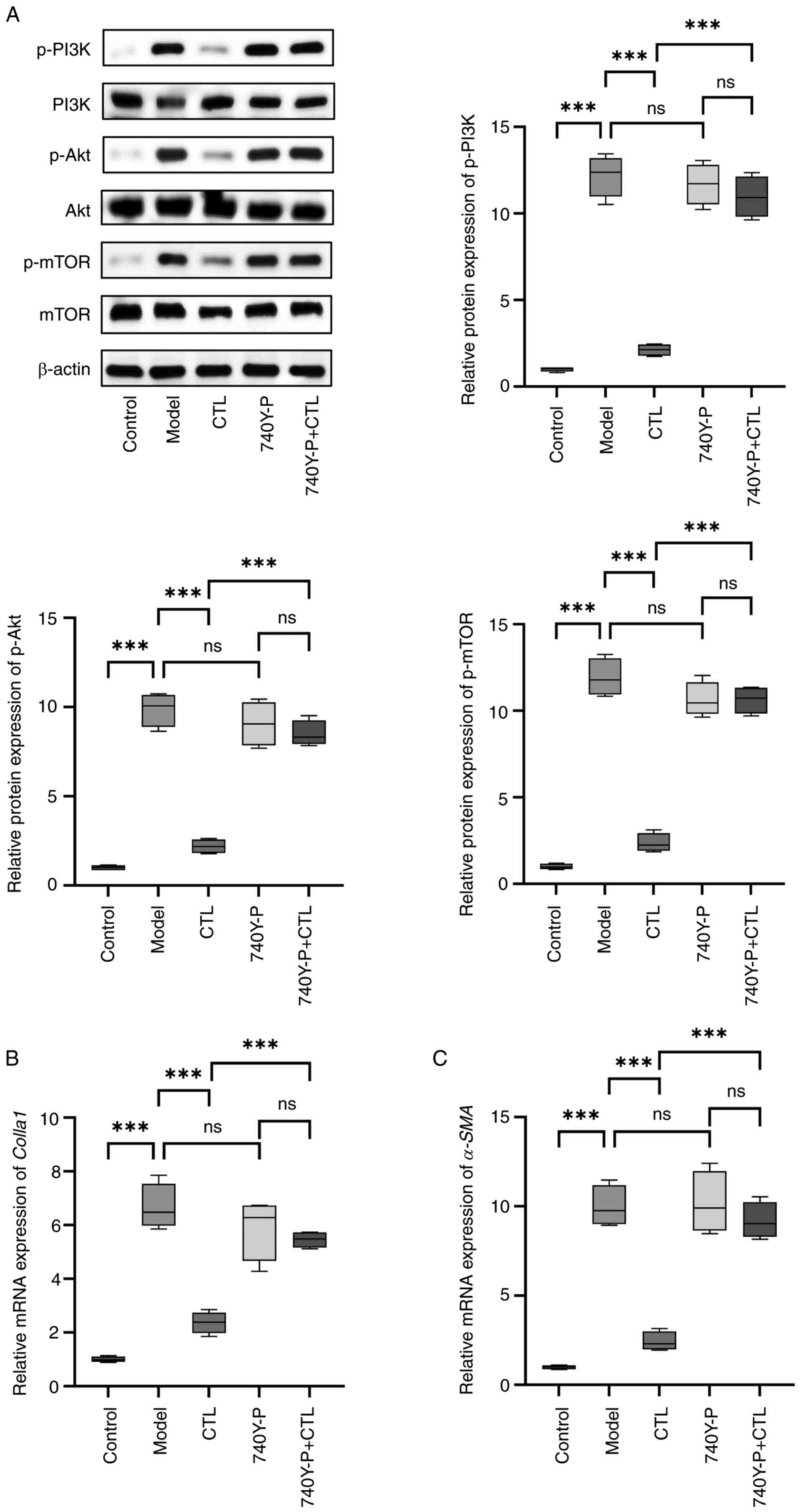
2
|
Roehlen N, Saviano A, El Saghire H,
Crouchet E, Nehme Z, Del Zompo F, Jühling F, Oudot MA, Durand SC,
Duong FHT, et al: A monoclonal antibody targeting nonjunctional
claudin-1 inhibits fibrosis in patient-derived models by modulating
cell plasticity. Sci Transl Med. 14:eabj42212022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ajmera V, Cepin S, Tesfai K, Hofflich H,
Cadman K, Lopez S, Madamba E, Bettencourt R, Richards L, Behling C,
et al: A prospective study on the prevalence of NAFLD, advanced
fibrosis, cirrhosis and hepatocellular carcinoma in people with
type 2 diabetes. J Hepatol. 78:471–478. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Luo P, Liu D, Zhang Q, Yang F, Wong YK,
Xia F, Zhang J, Chen J, Tian Y, Yang C, et al: Celastrol induces
ferroptosis in activated HSCs to ameliorate hepatic fibrosis via
targeting peroxiredoxins and HO-1. Acta Pharm Sin B. 12:2300–2314.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li Z, Wang F, Li Y, Wang X, Lu Q, Wang D,
Qi C, Li C, Li Z, Lian B, et al: Combined anti-hepatocellular
carcinoma therapy inhibit drug-resistance and metastasis via
targeting ‘substance P-hepatic stellate cells-hepatocellular
carcinoma’ axis. Biomaterials. 276:1210032021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dat NQ, Thuy LTT, Hieu VN, Hai H, Hoang
DV, Thi Thanh Hai N, Thuy TTV, Komiya T, Rombouts K, Dong MP, et
al: Hexa histidine-tagged recombinant human cytoglobin deactivates
hepatic stellate cells and inhibits liver fibrosis by scavenging
reactive oxygen species. Hepatology. 73:2527–2545. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Myojin Y, Hikita H, Sugiyama M, Sasaki Y,
Fukumoto K, Sakane S, Makino Y, Takemura N, Yamada R, Shigekawa M,
et al: Hepatic stellate cells in hepatocellular carcinoma promote
tumor growth via growth differentiation factor 15 production.
Gastroenterology. 160:1741–1754.e16. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li WX, Chen X, Yang Y, Huang HM, Li HD,
Huang C, Meng XM and Li J: Hesperitin derivative-11 suppress
hepatic stellate cell activation and proliferation by targeting
PTEN/AKT pathway. Toxicology. 381:75–86. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Parsons CJ, Takashima M and Rippe RA:
Molecular mechanisms of hepatic fibrogenesis. J Gastroenterol
Hepatol. 22 (Suppl 1):S79–S84. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shamsan E, Almezgagi M, Gamah M, Khan N,
Qasem A, Chuanchuan L and Haining F: The role of PI3k/AKT signaling
pathway in attenuating liver fibrosis: A comprehensive review.
Front Med (Lausanne). 11:13893292024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lin X, Wei Y, Li Y, Xiong Y, Fang B, Li C,
Huang Q, Huang R and Wei J: Tormentic acid ameliorates hepatic
fibrosis in vivo by inhibiting glycerophospholipids metabolism and
PI3K/Akt/mTOR and NF-κB pathways: Based on transcriptomics and
metabolomics. Front Pharmacol. 13:8019822022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Meng YX, Zhao R and Huo LJ: Interleukin-22
alleviates alcohol-associated hepatic fibrosis, inhibits autophagy,
and suppresses the PI3K/AKT/mTOR pathway in mice. Alcohol Clin Exp
Res (Hoboken). 47:448–458. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang X, Liu H, Wang Y, Wang P, Yi Y, Lin Y
and Li X: Novel protein C6ORF120 promotes liver fibrosis by
activating hepatic stellate cells through the PI3K/Akt/mTOR
pathway. J Gastroenterol Hepatol. 39:1422–1430. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang R, Song F, Li S, Wu B, Gu Y and Yuan
Y: Salvianolic acid A attenuates CCl4-induced liver
fibrosis by regulating the PI3K/AKT/mTOR, Bcl-2/Bax and
caspase-3/cleaved caspase-3 signaling pathways. Drug Des Devel
Ther. 13:1889–1900. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ji D, Zhao Q, Qin Y, Tong H, Wang Q, Yu M,
Mao C, Lu T, Qiu J and Jiang C: Germacrone improves liver fibrosis
by regulating the PI3K/AKT/mTOR signalling pathway. Cell Biol Int.
45:1866–1875. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang LL, Tian K, Tang ZH, Chen XJ, Bian
ZX, Wang YT and Lu JJ: Phytochemistry and pharmacology of
Carthamus tinctorius L. Am J Chin Med. 44:197–226. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Delshad E, Yousefi M, Sasannezhad P,
Rakhshandeh H and Ayati Z: Medical uses of Carthamus tinctorius
L. (safflower): A comprehensive review from traditional
medicine to modern medicine. Electron Physician. 10:6672–6681.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Okuyama H, Yamada K, Miyazawa D, Yasui Y
and Ohara N: Dietary lipids impacts on healthy ageing. Lipids.
42:821–825. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Suzuki K, Tsubaki S, Fujita M, Koyama N,
Takahashi M and Takazawa K: Effects of safflower seed extract on
arterial stiffness. Vasc Health Risk Manag. 6:1007–1014. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liang Y and Wang L: Carthamus
tinctorius L.: A natural neuroprotective source for
anti-Alzheimer's disease drugs. J Ethnopharmacol. 298:1156562022.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ao H, Feng W and Peng C: Hydroxysafflor
yellow A: A promising therapeutic agent for a broad spectrum of
diseases. Evid Based Complement Alternat Med. 2018:82592802018.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bai J, Wang X, Du S, Wang P, Wang Y, Quan
L and Xie Y: Study on the protective effects of danshen-honghua
herb pair (DHHP) on myocardial ischaemia/reperfusion injury (MIRI)
and potential mechanisms based on apoptosis and mitochondria. Pharm
Biol. 59:335–346. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Du SB, Zhou HH, Wang PF, Wang XP, Xue ZP,
Li J, Gao S, Li N, Bai JQ and Xie LH: Modulation effects of
danshen-honghua herb pair on gut microbiota of acute myocardial
ischemia model rat. FEMS Microbiol Lett. 369:fnac0362022.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wan H, Yang Y, Li Z, Cheng L, Ding Z, Wan
H, Yang J and Zhou H: Compatibility of ingredients of Danshen
(Radix Salviae Miltiorrhizae) and Honghua (Flos Carthami) and their
protective effects on cerebral ischemia-reperfusion injury in rats.
Exp Ther Med. 22:8492021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu Y, Zhou B and Ding X: Informatic study
of cada prescription for the treatment of liver disease. TCM
Pharmacol Clin. 39:104–110. 2023.
|
|
26
|
Meng X, Zhou B and Liu Y: Data mining of
the ‘Bashaga’ class (Qumai) prescription prescription and its
action mechanism analysis for the treatment of liver disease. Chin
Mod TCM. 25:1266–1279. 2023.
|
|
27
|
Urig Wang Y and Nao M: Progress in
experimental research on Mongolian drug therapy for liver injury.
World Sci Technol-Modern Tradit Chin Med. 22:416–422. 2020.
|
|
28
|
Yang T, Liang S and Zhou B: Progress in
the treatment of liver fibrosis. Chin Ethnic Folk Med. 28:68–71.
2019.
|
|
29
|
Chang LL, Li C, Li ZL, Wei ZL, Jia XB,
Pang ST, An YQ, Gu JF and Feng L: Carthamus tinctorius L:
Extract ameliorates cerebral ischemia-reperfusion injury in rats by
regulating matrix metalloproteinases and apoptosis. Indian J
Pharmacol. 52:108–116. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Greenfield EA: Sampling and preparation of
mouse and rat serum. Cold Spring Harb Protoc. 2017.pdb.prot100271,
2017. View Article : Google Scholar
|
|
31
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Dong Z, Li S, Si L, Ma R, Bao L and Bo A:
Identification lncRNA LOC102551149/miR-23a-5p pathway in hepatic
fibrosis. Eur J Clin Invest. 50:e132432020. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Dong Z, Li S, Wang X, Si L, Ma R, Bao L
and Bo A: lncRNA GAS5 restrains CCl4-induced hepatic
fibrosis by targeting miR-23a through the PTEN/PI3K/Akt signaling
pathway. Am J Physiol Gastrointest Liver Physiol. 316:G539–G550.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ali MH, Talha M and Hussain SAS: The role
of hepatic stellate cells and the Gas6/Axl axis in liver fibrosis
and hepatocellular carcinoma. J Clin Exp Hepatol. 14:1014002024.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Shan L, Liu Z, Ci L, Shuai C, Lv X and Li
J: Research progress on the anti-hepatic fibrosis action and
mechanism of natural products. Int Immunopharmacol. 75:1057652019.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Shan L, Wang F, Zhai D, Meng X, Liu J and
Lv X: New drugs for hepatic fibrosis. Front Pharmacol.
13:8744082022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li D, Tao L, Chen Z, Cai W and Shen W:
Treatment of peripheral facial paralysis after COVID-19 infection
with traditional chinese medicine therapies: A case report. Cureus.
16:e570472024.PubMed/NCBI
|
|
38
|
Xi S, Yue L, Shi M, Peng Y, Xu Y, Wang X,
Li Q, Kang Z, Li H and Wang Y: The effects of taoren-honghua herb
pair on pathological microvessel and angiogenesis-associated
signaling pathway in mice model of CCl4-induced chronic liver
disease. Evid Based Complement Alternat Med. 2016:29742562016.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wan S, Liu X, Sun R, Liu H, Jiang J and Wu
B: Activated hepatic stellate cell-derived Bmp-1 induces liver
fibrosis via mediating hepatocyte epithelial-mesenchymal
transition. Cell Death Dis. 15:412024. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hwang CH, Jang E and Lee JH:
Pharmacological benefits and underlying mechanisms of Salvia
miltiorrhiza against molecular pathology of various liver diseases:
A review. Am J Chin Med. 51:1675–1709. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Tuohetahuntila M, Molenaar MR, Spee B,
Brouwers JF, Wubbolts R, Houweling M, Yan C, Du H, VanderVen BC,
Vaandrager AB and Helms JB: Lysosome-mediated degradation of a
distinct pool of lipid droplets during hepatic stellate cell
activation. J Biol Chem. 292:12436–12448. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sharma A, Verma AK, Kofron M, Kudira R,
Miethke A, Wu T, Wang J and Gandhi CR: Lipopolysaccharide reverses
hepatic stellate cell activation through modulation of cMyb, small
mothers against decapentaplegic, and CCAAT/enhancer-binding protein
C/EBP transcription factors. Hepatology. 72:1800–1818. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Li R, Zhang J, Liu Q, Tang Q, Jia Q, Xiong
Y, He J and Li Y: CREKA-modified liposomes target activated hepatic
stellate cells to alleviate liver fibrosis by inhibiting collagen
synthesis and angiogenesis. Acta Biomater. 168:484–496. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yin L, Zhang Y, Shi H, Feng Y, Zhang Z and
Zhang L: Proteomic profiling of hepatic stellate cells in alcohol
liver fibrosis reveals proteins involved in collagen production.
Alcohol. 86:81–91. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Zhang M, Wu Z, Salas SS, Aguilar MM,
Trillos-Almanza MC, Buist-Homan M and Moshage H: Arginase 1
expression is increased during hepatic stellate cell activation and
facilitates collagen synthesis. J Cell Biochem. 124:808–817. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ezquerro S, Tuero C, Becerril S, Valentí
V, Moncada R, Landecho MF, Catalán V, Gómez-Ambrosi J, Mocha F,
Silva C, et al: Antagonic effect of ghrelin and LEAP-2 on hepatic
stellate cell activation and liver fibrosis in obesity-associated
nonalcoholic fatty liver disease. Eur J Endocrinol. 188:564–577.
2023.PubMed/NCBI
|
|
47
|
Jokl E, Llewellyn J, Simpson K, Adegboye
O, Pritchett J, Zeef L, Donaldson I, Athwal VS, Purssell H, Street
O, et al: Circadian disruption primes myofibroblasts for
accelerated activation as a mechanism underpinning fibrotic
progression in non-alcoholic fatty liver disease. Cells.
12:15822023. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Hussein KH, Park KM, Yu L, Kwak HH and Woo
HM: Decellularized hepatic extracellular matrix hydrogel attenuates
hepatic stellate cell activation and liver fibrosis. Mater Sci Eng
C Mater Biol Appl. 116:1111602020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Bissoondial TL, Han Y, Mullan S, Pabla AK,
Spahn K, Shi S, Zheng L, Zhou P, Jiang K, Prakash N, et al: Liver
biopsy hydroxyproline content is a diagnostic for hepatocellular
carcinoma in murine models of nonalcoholic steatohepatitis.
Diagnostics (Basel). 10:7842020. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhou L, Liang Q, Li Y, Cao Y, Li J, Yang
J, Liu J, Bi J and Liu Y: Collagenase-I decorated co-delivery
micelles potentiate extracellular matrix degradation and hepatic
stellate cell targeting for liver fibrosis therapy. Acta Biomater.
152:235–254. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lopez-Sanchez I, Dunkel Y, Roh YS, Mittal
Y, De Minicis S, Muranyi A, Singh S, Shanmugam K, Aroonsakool N,
Murray F, et al: GIV/Girdin is a central hub for profibrogenic
signalling networks during liver fibrosis. Nat Commun. 5:44512014.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Huang Y, Luo W, Chen S, Su H, Zhu W, Wei
Y, Qiu Y, Long Y, Shi Y and Wei J: Isovitexin alleviates hepatic
fibrosis by regulating miR-21-mediated PI3K/Akt signaling and
glutathione metabolic pathway: Based on transcriptomics and
metabolomics. Phytomedicine. 121:1551172023. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yu Y, Zhou S, Wang Y, Di S, Wang Y, Huang
X and Chen Y: Leonurine alleviates acetaminophen-induced acute
liver injury by regulating the PI3K/AKT signaling pathway in mice.
Int Immunopharmacol. 120:1103752023. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Zhou M, Zhao X, Liao L, Deng Y, Liu M,
Wang J, Xue X and Li Y: Forsythiaside A regulates activation of
hepatic stellate cells by inhibiting NOX4-dependent ROS. Oxid Med
Cell Longev. 2022:99383922022.PubMed/NCBI
|
|
55
|
Xiong Y, Lu H and Xu H: Galangin reverses
hepatic fibrosis by inducing HSCs apoptosis via the PI3K/Akt,
Bax/Bcl-2, and Wnt/β-catenin pathway in LX-2 cells. Biol Pharm
Bull. 43:1634–1642. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Jin J, Yang H, Hu L, Wang Y, Wu W, Hu C,
Wu K, Wu Z, Cheng W and Huang Y: Inonotsuoxide B suppresses hepatic
stellate cell activation and proliferation via the PI3K/AKT and
ERK1/2 pathway. Exp Ther Med. 23:4172022. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lu QY, Ma JQ, Duan YY, Sun Y, Yu S, Li B
and Zhang GM: Carthamin yellow protects the heart against
ischemia/reperfusion injury with reduced reactive oxygen species
release and inflammatory response. J Cardiovasc Pharmacol.
74:228–234. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Feng X, Du M, Li S, Zhang Y, Ding J, Wang
J, Wang Y and Liu P: Hydroxysafflor yellow A regulates
lymphangiogenesis and inflammation via the inhibition of PI3K on
regulating AKT/mTOR and NF-κB pathway in macrophages to reduce
atherosclerosis in ApoE-/- mice. Phytomedicine. 112:1546842023.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tu H, Ma D, Luo Y, Tang S, Li Y, Chen G,
Wang L, Hou Z, Shen C, Lu H, et al: Quercetin alleviates chronic
renal failure by targeting the PI3k/Akt pathway. Bioengineered.
12:6538–6558. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Fangma Y, Zhou H, Shao C, Yu L, Yang J,
Wan H and He Y: Hydroxysafflor yellow A and anhydrosafflor yellow B
protect against cerebral ischemia/reperfusion injury by attenuating
oxidative stress and apoptosis via the silent information regulator
1 signaling pathway. Front Pharmacol. 12:7398642021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Yang J, Pi C and Wang G: Inhibition of
PI3K/Akt/mTOR pathway by apigenin induces apoptosis and autophagy
in hepatocellular carcinoma cells. Biomed Pharmacother.
103:699–707. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ha SE, Kim SM, Vetrivel P, Kim HH, Bhosale
PB, Heo JD, Lee HJ and Kim GS: Inhibition of cell proliferation and
metastasis by scutellarein regulating PI3K/Akt/NF-κB signaling
through PTEN activation in hepatocellular carcinoma. Int J Mol Sci.
22:88412021. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Shuang R, QirigeerWurihan, Bai M,
Laxinamujila and Han X: Toxicity of Carthamus tinctorius L.
Water Extract. World Trad Chin Med. 18:979–982. 2023.(In
Chinese).
|