Introduction
Ewing's sarcoma/primitive neuroectodermal tumor
(PNET) is quite rare. Between 1973 and 2004, the incidence of the
disease in the US was 2–93 per 1,000,000 individuals (1). Ewing's sarcoma is the second most
common malignant bone tumor in children and adolescents. It affects
the pelvic bone and femur, but rarely the cervical spine. The
incidence of primary vertebral Ewing's sarcoma is 3.5% (2). It is thought to arise from neural
crest cells (3). In 1984, Jaffe
et al described a small round-cell tumor of the bone,
designated neuroectodermal tumor of bone (Ewing's sarcoma of bone)
(4). This tumor is difficult to
diagnose only by hematoxylin and eosin (H&E) staining.
In this report, all of the 4 cases were diagnosed
with dumbbell-shaped intraspinal and extraspinal Ewing's
sarcomas.
The study was approved by the research department of
Shanghai Changzheng Hospital, China, and the patients involved
provided their informed consent.
Case report
Descriptions of the 4 cases are provided in Table I. The 3 new-onset patients received
almost the same treatment (8–10 cycles of chemotherapy and local
irradiation) following surgery.
 | Table ISummary of the 4 cases. |
Table I
Summary of the 4 cases.
| Case 1 | Case 2 | Case 3 | Case 4 |
|---|
| Gender | Male | Male | Male | Male |
| Age (years) | 46 | 27 | 27 | 24 |
| Clinical
manifestations | - | - | - | Before the first
operation |
| Pain | Mild pain for 12
months | Mild pain for 2
months | Mild pain for 6
months | Mild pain for 1
month |
| Neurological
impairment | Radiculopathy | Radiculopathy | Radiculopathy | Spinal cord
compression and radiculopathy |
| Strength |
| Upper limb | Level 4–5 | Level 3 | Level 2–4 | Level 3–4 |
| Lower limb | Level 5 | Level 5 | Level 5 | Level 3–4 |
| Date of surgery | 6.16.2008 | 8.12.2010 | 9.9.2009 | 2.10.2011 |
| Surgical
approach |
Anterior-posterior |
Anterior-posterior |
Anterior-posterior | Posterolateral |
| Blood loss | 1000 ml | 1300 ml | 2000 ml | 800 ml |
| Prognosis | Died in 12
months | Still alive | Still alive | Died in 7 months |
| Metastasis | Lung metastasis | None | None | Brain metastasis |
Case 1
The patient was a 46-year-old male who experienced
neck and shoulder pain for 12 months prior to the discovery of a
mass in the neck. Physical examination revealed a mass with
tenderness. There was limitation of motion in the cervical
vertebra. The force of the left deltoid was approximately level 3
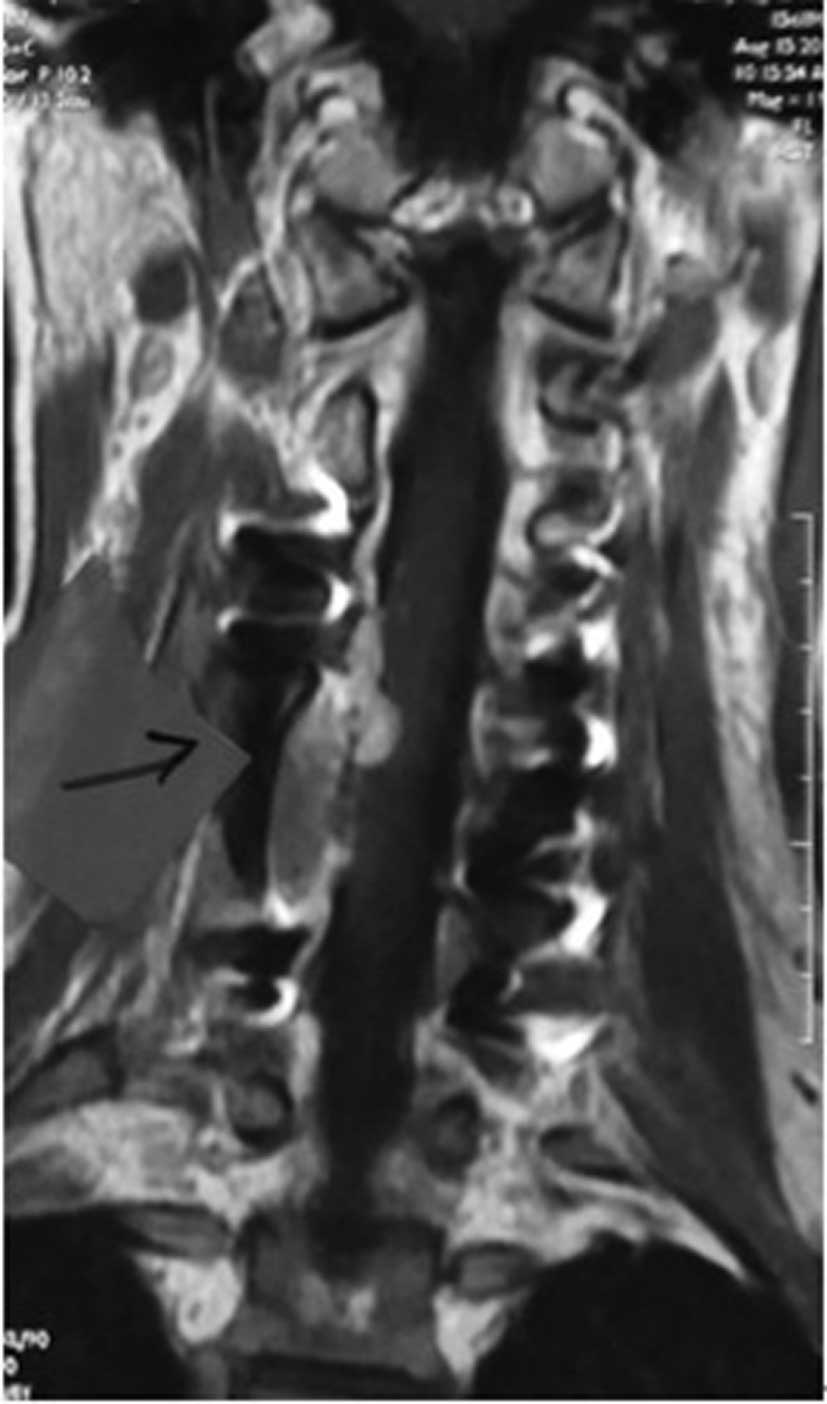
and the force of the other muscles was normal. Diagnostic imaging,
including computed tomography (CT) and magnetic resonance imaging
(MRI), revealed a dumbbell-shaped soft tissue mass beside the C3-C6
vertebra. MRI showed a collapse in the transverses of the C3 and C4
vertebra (Fig. 1). A neurogenic
tumor was suggested by imaging. After we finished preparation, the
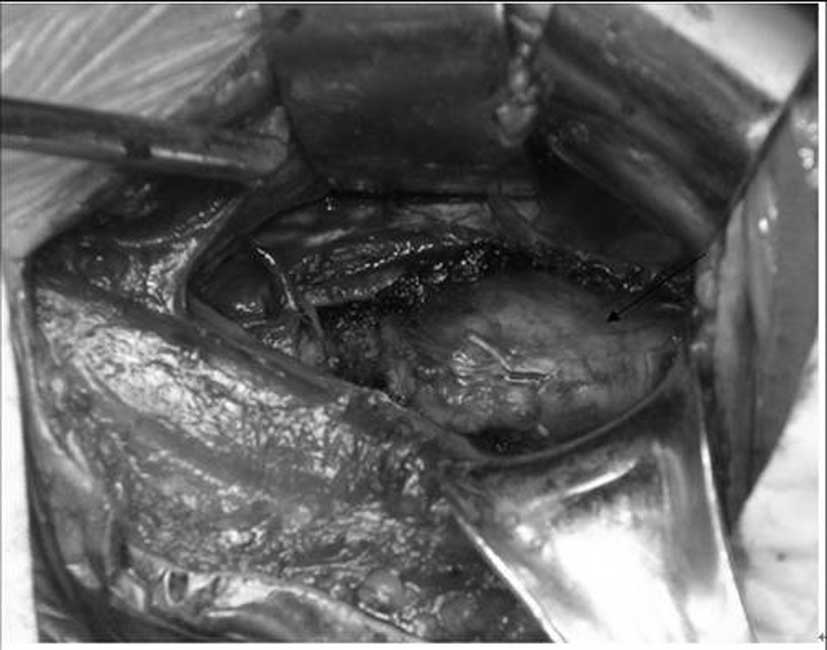
patient underwent surgery in June 2008. The procedure involved a
piecemeal resection. Anterior-posterior surgeries were performed in
this case. At first, the posterior approach was used. The tumor
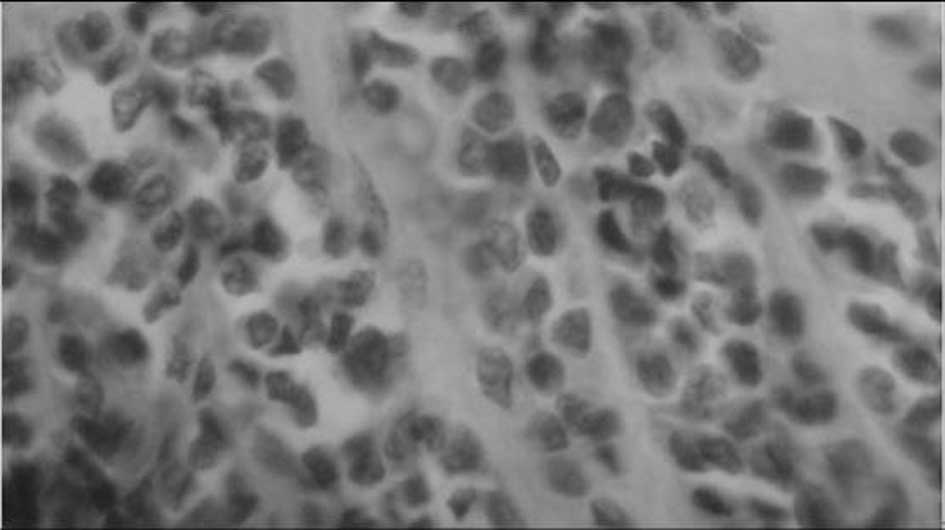
inside the spinal canal was removed. The removed tumor was sent to
be frozen in sections. Pathological investigation revealed a small
round-cell malignant tumor (Fig.
2). Cisplatin was subsequently used for intraoperative
chemotherapy. Following the posterior approach, surgery from the
anterior approach was performed (Fig.
3). The extraspinal part of the tumor was removed completely.
The nerve root and vertebral artery were protected during the
surgery. After surgery, the pathological diagnosis confirmed
Ewing's sarcoma. The patient felt that the pain had been
significantly relieved and the force of deltoid had been slightly
recovered. Although local radiotherapy and chemotherapy were used
following surgery, lung metastasis was observed. The patient
succumbed to the disease 12 months after surgery.
Case 2
The patient was a 27-year-old male with neck and
shoulder pain for 1 month prior to the discovery of a mass in the
neck. Physical examination revealed a mass with tenderness. There
was limitation of motion in the cervical vertebra. The force of the
muscles of the left upper limb was approximately level 3 and the
force of the other muscles was normal. The lower limb showed slight
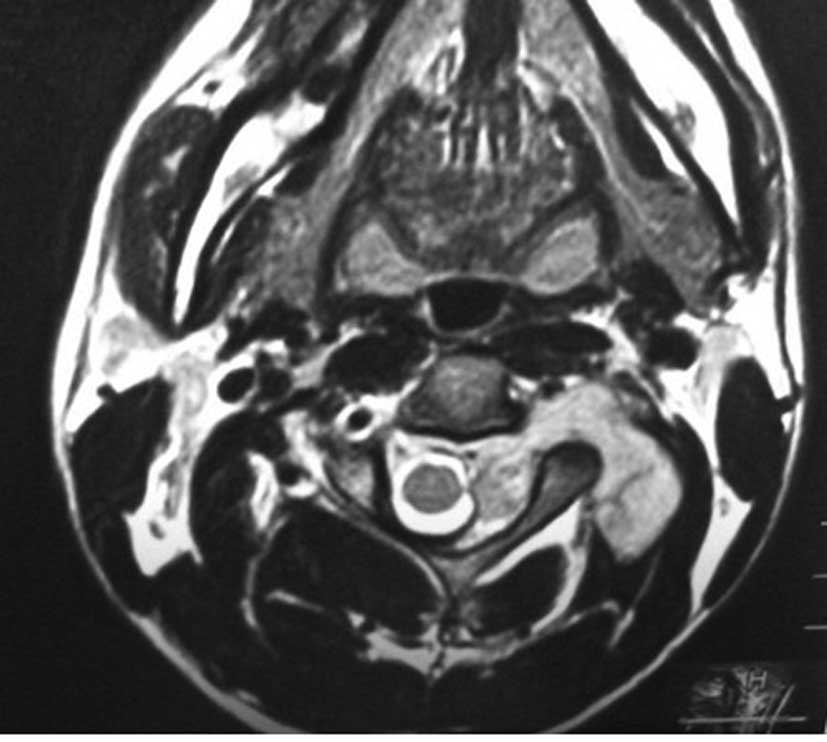
spasticity. Diagnostic imaging included CT and MRI. Imaging
revealed a dumbbell-shaped soft tissue mass on the left of the
C1-C4 vertebra. MRI showed collapse in the transverses of the C3
vertebra (Fig. 4). A neurogenic
tumor was suggested by imaging. After we finished the preparation,
the patient underwent surgery in August 2010. The surgery was a
piecemeal resection. Anterior-posterior surgery was performed in
this case. At first, the posterior approach was used. The tumor
inside the spinal canal was removed. The removed tumor was sent to
be frozen in sections. Pathological investigation revealed a
malignant neurogenic tumor. Cisplatin was used for the
intraoperative chemotherapy treatment. Following the posterior
approach, surgery from the anterior approach was performed. The
extraspinal part of the tumor was removed completely. After
surgery, the pathological diagnosis confirmed Ewing's sarcoma. The
patient felt that the pain had been significantly relieved and the
force of the muscles of the left upper limb had slightly recovered.
Local radiotherapy and chemotherapy were used following surgery. No
recurrence and metastasis have occurred thus far.
Case 3
The patient was a 27-year-old male with neck and
shoulder pain, and numbness in the left upper limb for 6 months.
Physical examination revealed that there was a limitation of motion
in the cervical vertebra. The force of the inner hand muscles of
the left limb was approximately level 2 and the force of other
muscles of the left limb was approximately level 4. Diagnostic
imaging included CT, MRI and PET-CT. The imaging revealed a
dumbbell-shaped soft tissue mass on the left of the C7 vertebra.
MRI showed collapse in the transverses of C7 vertebra (Fig. 5). PET-CT showed the FDG was mildly
absorbed. A giant cell tumor (GCT) was suggested by PET-CT. After
we finished the preparation, the patient underwent surgery in
September 2009. The surgery involved piecemeal resection.
Anterior-posterior surgery was performed in this case. At first,
the anterior approach was used. The extraspinal tumor was removed.
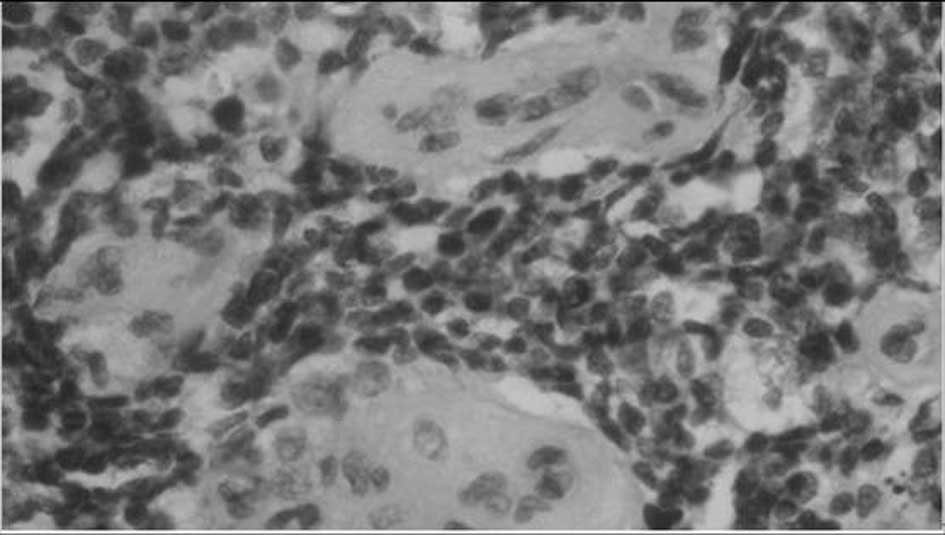
The removed tumor was sent to be frozen. Pathological investigation
revealed a small round-cell malignant tumor. Cisplatin was used as
intraoperative chemotherapy. After the anterior approach, surgery
from the posterior approach was performed. The intraspinal part of
the tumor was removed completely. The vertebral artery was
protected during the surgery; however, the C7 nerve root was not
protected. Following surgery, pathological diagnosis confirmed
Ewing's sarcoma (Fig. 6). The
patient felt that the pain had been significantly relieved and the
force of muscles of the left limb had slightly recovered. Local
radiotherapy and chemotherapy were used following surgery.
Recurrence and metastasis have not been found to date.
Case 4
The patient was a 24-year-old male with neck pain
and numbness in the left upper limb for 1 month. The patient had
received surgery in December 2009 in another hospital. A total of 7
months later, the patient complained of weakness and numbness in
the left limb. The recurrence was found by MRI (Fig. 7). Physical examination revealed that
the force of the muscles of the left limb was approximately level
3, and the force of other muscles of the right limb was
approximately level 4. Diagnostic imaging included CT and MRI. They
revealed a dumbbell-shaped soft tissue mass on the left of the C5
vertebra. MRI showed a collapse in the transverses of the C5
vertebra. After finishing the preparation, the patient underwent
surgery in July 2010. The surgery was a piecemeal resection. The
posterolateral approach was used. The tumor was located at the
ventral side of the spinal cord and was removed carefully. The
tightly adherent dura was removed together, then the dura was
repaired by soft tissue. Cisplatin was used for intraoperative
chemotherapy treatment. After the surgery, the pain had been
relieved; the force of muscles, however, had not been recovered.
Two weeks later, the patient began to receive chemotherapy.
However, recurrence of tumor appeared in the same place 6 months
following the initial removal, and the patient succumbed to brain
metastasis 7 months after the surgery.
Discussion
The incidence of dumbbell-shaped tumors in the spine
is 17.5% (118/674). The rate of dumbbell tumors in the cervical
spine is significantly higher than that of all spinal cord tumors.
Of 118 cases, 69% of tumors were found to be schwannomas (5).
Clinicopathological studies have revealed that
Ewing's sarcoma and PNET have overlapping features, supporting a
common histogenesis. Identification of a common translocation
t(11;22)(q24;q12) (6,7) that results in the formation of the
EWS-ETS fusion gene (8) in cases of
Ewing's sarcoma, PNET and Askin's tumor strongly supports the
hypothesis that these tumors are related. Therefore, all of these
lesions are now included in the same classification, the Ewing's
sarcoma family of tumors (EFTs).
The male to female ratio of Ewing's sarcoma is
1.5:1.3. Approximately 80% of patients are diagnosed with Ewing's
sarcoma when they are younger than 20 years old. A total of 50–60%
of the patients are diagnosed during their second decade (9). In the event patients are over 30 years
old, the diagnosis of Ewing's sarcoma should be made after
exclusion of the possibility of other small round-cell malignant
tumors.
Generally, Ewing's sarcoma progresses quite rapidly.
The most common clinical manifestation is pain. The 3 new-onset
patients in this study suffered mild pain, which was relieved by
using non-steroidal anti-inflammatory drugs (NSAIDS). Radiculopathy
caused by the tumor was found in all 4 cases. However, spinal cord
compression only appeared in the patient with recurrent sarcoma.
Due to the rapid progression and the dumbbell-shaped tumor, the
nerve root is affected first. Before spinal cord compression
appeared, the patients were treated for radiculopathy and the
rapidly progressing mass.
Tumor-related osteolysis and periosteal reactions
suggest a diagnosis of primary malignant tumor. Typically, Ewing's
sarcoma appears as an ill-defined, permeative, or focally
moth-eaten, destructive intramedullary lesion accompanied by a
periosteal reaction (‘onion skin’) that affects the diaphysis of
long bones (9). MRI is the most
sensitive test available for the evaluation of the soft tissue
extent of the tumor. The MRI appearance of Ewing's sarcoma is
non-specific, with TI-weighted images showing an intermediate
signal and T2-weighted images showing an intermediate-to-high
signal within the mass (10). In
the 3 new-onset patients, neurogenic tumors (schwannoma,
neurofibromatosis) and giant cell tumors (GCT) (Case 3) were
suggested by MRI.
Prior to surgery, biopsies had not been conducted
for the 3 new-onset patients as: i) Ewing's sarcoma is very
uncommon in African and Asian populations; ii) Ewing's sarcoma is
rare in the population over 20 years of age; iii) it is quite risky
to conduct a biopsy in the cervical spine, as the tumor is
surrounded by the vertebral artery, spinal cord and nerve root; iv)
neurogenic tumors (schwannoma, neurofibromatosis) or GCT were
suggested by MRI. For Ewing's sarcoma, the treatment should begin
with 2–3 cycles of neoadjuvant chemotherapy. This may help us to
achieve marginal resection. In the cervical spine, the tumor is
difficult to remove en bloc. Therefore, we propose that biopsy
should be conducted although neurogenic tumors (schwannoma,
neurofibromatosis) or GCT are suggested by imaging.
Generally, Ewing's sarcoma is sensitive to
chemotherapy and irradiation. The proportion of patients whose
primary tumors are treated with radiation alone has steadily
declined over the past 30 years. This is due to advances in
orthopedic surgery and a growing awareness of the late effects of
radiation in children, particularly second malignancies and growth
disturbances. Patients whose primary tumors are excised have a
higher survival rate, although the prognostic effects of site and
size complicate the analyses (11).
Surgical en bloc resection, where feasible, is
regarded as the best modality for local control (12). Anterior-posterior surgeries were
performed in 3 cases in this study. The posterolateral approach was
performed in 1 case, which is also recommended. Although en bloc
resection was not performed, we did our best to achieve total
resection of the tumor. In addition, cisplatin was used for the
treatment of intraoperative chemotherapy in order to lessen the
rate of recurrence and metastasis.
Ewing's sarcomas are sensitive to chemotherapy and
irradiation. In the Cooperative Ewing's Sarcoma Study (CESS)-81,
the 5-year relapse-free survival of patients with non-metastatic
Ewing's sarcoma after VACD regimen (vincristine, actinomycin-D,
cyclophosphamide and doxorubicin) was 55% (13). In the CESS-86 study, ifosfamide was
substituted for doxorubicin in the treatment of tumors with a
volume greater than 100 ml. The 10-year event-free survival was 52%
(14). In our cases, 8–10 cycles of
chemotherapy were administered after surgery. The use of
chemotherapy has greatly improved survival rates for patients with
localized Ewing's sarcoma. Hoiwever, it has much less effect on the
survival of patients with metastases at diagnosis. Radiotherapy
treatment should be used with caution since the spinal cord is
sensitive to radiation. Local irradiation is suggested.
The prognosis of Ewing's sarcoma is quite poor.
Non-metastatic disease at presentation has a 5-year disease-free
survival rate of 70%, whereas patients with metastatic disease at
presentation have a 5-year disease-free survival rate of 25%
(15). In our cases, 2 patients
were diagnosed with metastases following surgery. The new-onset
patients survived for 7 months and the other patient for 12
months.
Recently, a study showed that insulin-like growth
factor 1 receptor (IGF1R)-targeted therapies have resulted in
responses in a small number of patients with advanced metastatic
Ewing's sarcoma (16).
Ewing's sarcoma is the second most common malignant
bone tumor in children and adolescents. It affects the pelvic bone
and femur, but rarely the cervical vertebra. All of the 4 cases
were diagnosed with dumbbell-shaped intraspinal and extraspinal
Ewing's sarcomas. It is likely to be misdiagnosed as a neurogenic
tumor (schwannoma, neurofibromatosis) or GCT according to imaging.
Radiculopathy is more common than spinal cord compression in
Ewing's sarcoma. Preoperative biopsy is strongly recommended. As
soon as Ewing's sarcoma is diagnosed by pathology, the treatment
should begin with 2–3 cycles of neoadjuvant chemotherapy. The
anterior-posterior and posterolateral approach are both recommended
for exposing this tumor. Following surgery, chemotherapy is
critical to lessen the rate of recurrence and metastasis and
prolong the survival time. However, radiotherapy treatment should
be used cautiously, as the spinal cord is sensitive to radiation.
Local irradiation is suggested. The tumor is difficult to be
removed en bloc in the cervical spine. It has a high rate of
recurrence and metastasis. Therefore, the prognosis of Ewing's
sarcomas in the cervical region is poorer than that in the thoracic
and lumbosacral region.
References
|
1
|
Esiashvili N, Goodman M and Marcus R:
Changes in incidence and survival of Ewing sarcoma patients over
the past 3 decades: surveillance epidemiology and end results data.
J Pediat Hematol Oncol. 30:425–430. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Whitehouse GH and Griffiths GJ:
Roentgenological aspects of spinal involvement by primary and
metastatic Ewing's tumor. J Can Assoc Radiol. 27:290–297. 1976.
|
|
3
|
Dehner LP: Peripheral and central
primitive neuroectodermal tumors: a nosologic concept seeking a
consensus. Arch Pathol Lab Med. 110:997–1005. 1986.PubMed/NCBI
|
|
4
|
Jaffe R, Santamaria M, Yunis EJ, et al:
The neuroectodermal tumor of bone. Am J Surg Pathol. 8:885–898.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ozama H, Kokubum S, Aizawa T, Takeshi H
and Chikashi K: Spinal dumbbell tumors: an analysis of a series of
118 cases. J Neurosurg Spine. 7:587–593. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Aurias A, Rimbaut C, Buffe D, Zucker JM
and Mazabraud A: Translocation involving chromosome 22 in Ewing's
sarcoma: a cytogenetic study of four fresh tumors. Cancer Genet
Cytogenet. 12:21–25. 1984. View Article : Google Scholar
|
|
7
|
Whang-Peng J, Triche TJ, Knutsen T, Miser
J, Douglass EC and Israel MA: Chromosomal translocation in
peripheral neuroepithelioma. N Engl J Med. 311:584–585. 1984.
View Article : Google Scholar
|
|
8
|
Delattre O, Zucman J, Plougastel B, et al:
Gene fusion with an ETS DNA-binding domain caused by chromosome
translocation in human tumours. Nature. 359:162–165. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Iwamoto Y: Diagnosis and treatment of
Ewing's sarcoma. Jpn J Clin Oncol. 37:79–89. 2007. View Article : Google Scholar
|
|
10
|
Flemming DJ, Murphy MD, Nallu S and
Nicastri AD: Primary Ewing sarcoma of lumbar spine with massive
intraspinal extension. Pediatr Neurol. 38:58–60. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schuck A, Ahrens S, Paulussen M, et al:
Local therapy in localized Ewing's tumors: results of 1058 patients
treated in the CESS 81, CESS 86, and EICESS 92 trials. Int J Rad
Oncol Biol Phys. 55:168–177. 2003.
|
|
12
|
Paulussen M, Bielack S and Jurgens H:
Ewing's sarcoma of the bone: ESMO clinical recommendations for
diagnosis, treatment and follow-up. Ann Oncol. (Suppl 4): 140–142.
2009.
|
|
13
|
Jurgens H, Exner U, Gadner H, et al:
Multidisciplinary treatment of primary Ewing's sarcoma of bone. A
6-year experience of a European Cooperative Trial. Cancer.
61:23–32. 1988.
|
|
14
|
Paulussen M, Ahrens S, Dunst J, et al:
Localized Ewing's tumor of bone: final results of the cooperative
Ewing's Sarcoma Study CESS 86. J Clin Oncol. 19:1818–1829.
2001.
|
|
15
|
Caudill JS and Arndt CA: Diagnosis and
management of bone malignancy in adolescence. Adolesc Med.
18:62–78. 2009.
|
|
16
|
Rodon J, DeSantos V, Ferry RJ Jr and
Kurzrock R: Early drug development of inhibitors of the
insulin-like growth factor-I receptor pathway: lessons from the
first clinical trials. Mol Cancer Ther. 7:2575–2588. 2008.
View Article : Google Scholar : PubMed/NCBI
|