Introduction
Although double cancers in the upper aerodigestive
tract mucosa are not uncommon (1–6),
collision tumors that are composed of a papillary thyroid carcinoma
and a laryngeal squamous cell carcinoma are rare. The term
‘collision tumor’ refers to the coexistence of two histologically
distinct malignant tumors within the same mass. The present study
describes the case of a 55-year-old male who presented with a
collision tumor in the neck. Written informed consent was obtained
from the patient.
Case report
A 55-year-old male presented with a two-year history
of a rapidly expanding, painless mass in the right side of the
neck, a two-month history of progressive hoarseness and a one-month
history of dyspnea. The patient had a 20-year history of smoking
cigarettes and ingesting alcohol. The patient denied any loss of
weight or appetite, a history of exposure to radiation or any
family history of thyroid cancer. A physical examination revealed a
firm, immovable 3.0×3.0×2.0-cm mass in the right side of the neck
near the sternocleidomastoid muscle and a firm, fixed 1.0×1.0-cm
mass in the right thyroid gland. An electronic laryngoscopy
revealed a paralyzed right true vocal cord and right arytenoid,
with a large submucosal mass located in the right false vocal cord
and right arytenoids (Fig. 1). A
computed tomography (CT) scan (Fig.
2) revealed a mass in the right parapharyngeal space,
infiltrating into the right lobe of the thyroid gland, and enlarged
lymph nodes in the right side of the neck. During surgery, a frozen
pathological analysis demonstrated that the large submucosal mass
in the right arytenoid was a laryngeal squamous cell carcinoma. The
patient underwent en bloc near-total thyroidectomy combined with a
total laryngectomy, as well as paratracheal lymph node and
bilateral selective neck dissections (levels II–IV). The
pharyngoesophageal segment was reconstructed primarily. A
tracheoesophageal puncture was performed at the time of tumor
resection. The patient was discharged on post-operative day 14.
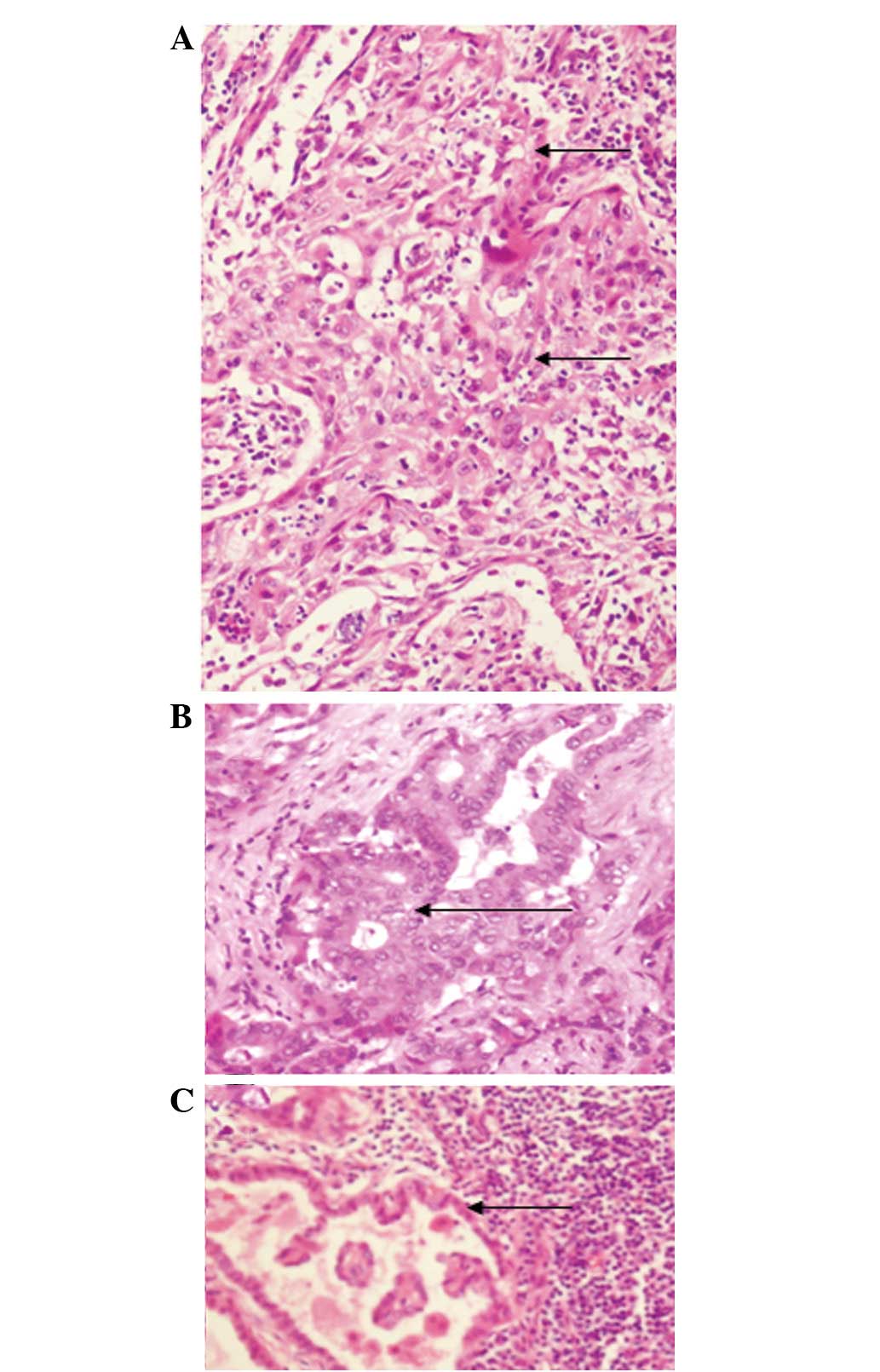
The resected laryngeal specimen revealed a large
exophytic mass involving the entire right hemilarynx in continuity
with the thyroid lesion. The final pathological analysis revealed a
laryngeal squamous cell carcinoma (Fig.
3A) with infiltration of the full-thickness wall of the larynx,
invasion and penetration of the thyroid cartilage and invasion of
the thyroid gland. The right lobe of the thyroid gland contained a
papillary thyroid carcinoma (Fig.
3B) with invasion and penetration of the thyroid cartilage, as
far as the deep tissue of the larynx. Sectioning of multiple
cervical lymph nodes revealed metastases from the thyroid papillary
carcinoma (Fig. 3C). The final
diagnosis was a collision tumor originating from a papillary
thyroid carcinoma and a laryngeal squamous cell carcinoma.
The patient was recommended to start radiotherapy at
one month post-surgery, but refused. One year after the surgery,
the patient presented with a one-month history of a rapidly
expanding painless mass in the right side of the neck. A physical
examination revealed a firm, fixed 7.0×6.0-cm mass on the right of
the tracheostomy. A CT scan (Fig.
4A) revealed a space containing a lesion on the right side of
the neck that was suspected to be lymph nodes with metastatic
disease. The neoplasm was removed and the pathological analysis
revealed lymph nodes with metastatic papillary carcinoma (Fig. 4B). Immunohistochemistry demonstrated
that the lesion was positive for cytokeratin 7, transglutaminase
and thyroid transcription factor-1 and negative for galectin-3. One
month after the second surgery, the patient was administered
131I radiation therapy for 3 days. One year after
radiation therapy, the patient presented with a mass on the right
side of the next and refused further therapy. Following this point
the patient was lost to follow-up.
Discussion
In multiple primary cancers, each tumor is malignant
and is of an independent pathological type, with none of the
lesions being metastatic (6).
Multiple primary cancers may be double (i.e. two primary cancers)
or triple (i.e. three primary cancers) cancers. Collision
carcinomas are a special type of multiple primary carcinoma, which
are difficult to diagnose prior to a surgical resection due to a
lack of characteristic clinical features. In the patient of the
present study, the mass presented as submucosal lesions. Since the
mucosa covering the lesion remained intact, a biopsy was not
performed prior to the surgery. The initial findings indicated a
thyroid gland tumor that was invaded by a laryngeal tumor, or a
laryngeal tumor that was invaded by a thyroid tumor. Since the
frozen pathology revealed only a squamous cell carcinoma, the
possibility of a collision tumor was not considered. The final
pathological findings following the surgery were of a laryngeal
squamous cell carcinoma and a papillary thyroid carcinoma that had
invaded each other.
Collision tumors may be located anywhere in the
body. A collision tumor of the breast has been described (8), as has an intracranial collision
metastasis (9). Similar to the
present case, a collision tumor of a papillary thyroid carcinoma
and a laryngeal squamous cell carcinoma has been previously
reported (7). In that patient,
however, the metastatic lymph nodes were derived from a primary
thyroid papillary carcinoma or a laryngeal squamous cell carcinoma,
with one lymph node showing metastases from the two. In the present
patient, the metastatic lymph nodes were all derived from the
primary thyroid papillary carcinoma. The earlier study patient
underwent a total thyroidectomy, total laryngectomy and bilateral
selective neck dissections (levels II–IV), whereas the present
patient underwent a subtotal thyroidectomy, total laryngectomy and
bilateral selective neck dissections (levels II–IV). During the
surgery, the tumor in the thyroid was considered to be derived from
the larynx. Therefore, a section of the thyroid gland was preserved
to ensure its continued function. The earlier study patient
underwent post-operative adjuvant radiotherapy and treatment with
131I treatment, whereas the patient of the present study
refused the two treatment modalities, perhaps for economic reasons.
One year later, however, the present patient presented with
cervical lymph nodes with a metastatic papillary thyroid carcinoma
and underwent post-operative 131I treatment.
Due to the rarity of collision tumors of the head
and neck, it is difficult to determine their etiology. Two
hypotheses have been suggested (5).
The first suggests that the two primary tumors developed in the
same location by chance, perhaps due to radiation. The second
hypothesis suggests that the presence of the first tumor alters the
microenvironment, allowing the second, adjacent tumor to develop.
The present patient and the earlier study patient were diagnosed
with a collision tumor of a papillary thyroid carcinoma and a
laryngeal squamous cell carcinoma (7), and the tumors were extremely large.
Had these patients felt uncomfortable and gone to a hospital
sooner, they may not have developed collision tumors.
The therapy for multiple primary cancers should
consist of a combination of the treatments that are normally used
for each focus. Since few patients with these tumors undergo a
pre-operative histological diagnosis, there may be differences in
the post-operative patient management. A collision carcinoma is a
special type of multiple primary carcinoma. Thus, en bloc resection
of the two inter-infiltrating tumors should be performed. The
present patient underwent an en bloc near-total thyroidectomy
combined with a total laryngectomy, along with paratracheal lymph
node dissections and bilateral selective neck dissections at levels
II–IV. Although post-operative adjuvant radiation therapy for the
laryngeal carcinoma and 131I treatment for the papillary
thyroid carcinoma was suggested, the patient refused further
treatment. The subsequent history of the patient demonstrated that
this adjuvant therapy was crucial.
Although the present patient did not exhibit any
pre-operative characteristics that indicated a collision tumor
rather than a laryngeal carcinoma and a thyroid carcinoma, the
results indicate that patients with large tumors invading other
structures should be assessed by intraoperative frozen pathology to
establish a diagnosis. Although the rarity of these patients limits
the therapeutic options, the results of the present study indicate
that a resection should be followed by radiation therapy for
laryngeal carcinoma and 131I treatment for the papillary
thyroid carcinoma.
In conclusion, as collision tumors of the head and
neck are rare, it is very difficult to obtain a pre-operative
diagnosis. The therapy for a collision tumor should consist of a
combination of the treatments that are normally used for each
focus.
Acknowledgements
The authors would like to thank Medjaden Bioscience
Limited for assisting in the preparation of this manuscript.
References
|
1
|
Esposito ED, Bevilacqua L and Guadagno MT:
Multiple primary malignant neoplasm in patients with laryngeal
carcinoma. J Surg Oncol. 74:83–86. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang CP, Lee YC, Yang TL, Lou PJ and Ko
JY: Application of unsedated transnasal esophagogastroduodenoscopy
in the diagnosis of hypopharyngeal cancer. Head Neck. 31:153–157.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang CP, Lee YC, Lou PJ, Yang TL, Chen TC,
Huang CC and Ko JY: Unsedated transnasal esophagogastroduodenoscopy
for the evaluation of dysphagia following treatment for previous
primary head neck cancer. Oral Oncol. 45:615–620. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lin ZM, Chang YL, Lee CY, Wang CP and
Hsiao TY: Simultaneous typical carcinoid tumour of the larynx and
occult papillary thyroid carcinoma. J Laryngol Otol. 122:93–96.
2008.PubMed/NCBI
|
|
5
|
Brandwein-Gensler M, Urken M and Wang B:
Collision tumor of the thyroid: a case report of metastatic
liposarcoma plus papillary thyroid carcinoma. Head Neck.
26:637–641. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Warren S and Gates O: Multiple primary
malignant tumors: a survey of the literature and a statistical
study. Am J Cancer. 16:1358–1414. 1932.
|
|
7
|
Jacobson AS, Wenig BM and Urken ML:
Collision tumor of the thyroid and larynx: a patient with papillary
thyroid carcinoma colliding with laryngeal squamous cell carcinoma.
Thyroid. 18:1325–1328. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cheung KJ, Tam W, Chuang E and Osborne MP:
Concurrent invasive ductal carcinoma and chronic lymphocytic
leukemia manifesting as a collision tumor in breast. Breast J.
13:413–417. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Palka KT, Lebow RL, Weaver KD and Kressin
MK: Intracranial collision metastases of small-cell lung cancer and
malignant melanoma. J Clin Oncol. 26:2042–2046. 2008. View Article : Google Scholar : PubMed/NCBI
|