Introduction
Schwannoma originating from the sacral nerve is a
rare and slow growing tumor, which arises most commonly in the
peripheral nervous system (1).
Although several case reports (2–6) have
previously described schwannoma arising in unusual sites, the
pelvis is also a rare site for a primary schwannoma. In the current
case study, the patient was mistakenly diagnosed with benign
ovarian teratoma without characteristic symptoms. The results of
the computed tomography (CT) scan conformed to an ovarian teratoma.
A careful patient history and clinical examination are important
for identifying illnesses, particularly tumors. Further diagnostic
pathology may clarify the diagnosis. However, definitive
preoperative diagnosis of schwannomas is of great significance to
guide treatment. To the best of our knowledge, this is the first
description of a misdiagnosis of presacral schwannoma as an ovarian
teratoma, cured with surgery. Written informed consent was obtained
from the patient.
Case report
A 61-year-old female presented with low back ache of
two months and severe abdominal pain and distention, constipation
and dysuria of 2 weeks (Fig. 1).
The patient was referred to the Gynecology Department for further
investigation of a large uterine tumor and dilatation of the
bilateral ureters detected by B-scan ultrasound, indicating a left
adnexal mass. The patient had a previous history of cesarean
section. Blood test results, including the levels of the tumor
markers, carcinoembryonic antigen, α-fetoprotein (AFP) and
carbohydrate antigens 19-9 and 12-5, were within normal limits.
Screening CT showed a large mass with uneven density, 14×10×15
cm3 in size, located on the left ovary (Fig. 2A) and closely attached to the
anterior wall of the sacrum without evident bony destruction
(Fig. 2B). Enhanced CT scan
revealed several irregular indurations of the nidus, however, no
enlarged lymph nodes or distant metastases were found. Evidently,
the bladder and uterus had become flattened by compression caused
by the giant tumor. The CT demonstrated leftward hydronephrosis and
thinned renal cortex also due to compression. The leftward ureter
also appeared to be obstructed and dilated, further diagnosing a
benign teratoma.
The surgery was completed through a collaboration
between orthopedic surgeons and gynecologists. Firstly, surgery via
an anterior approach was performed, ~5 cm in length. The patient’s
uterus had become oblate and atrophic. The separation of the
ovarian ligament was continued and the intestinal tube was pushed
away with gauze. The tumor appeared grayish-white, elastic hard and
smooth and appeared to be attached to the sacrum, 25×15×10
cm3 in size. The tumor was excised completely and tissue
was extracted to perform pathological examination. The surgeon
identified that the margin of the lesions had not invaded into the
surrounding tissue and confirmed the tumor as benign. While
removing the tumor, massive and rapid hemorrhage occurred as a
result of injury to the presacral venous plexus. The surgery
duration was 7.3 h and the estimated blood loss was 10,000 ml, with
requirement of a blood transfusion of 28 units red blood cells
suspension, 39 units fresh frozen plasma, 20 units platelets and 40
units cryoprecipitate, during the surgery. The patient experienced
a challenging surgical procedure, but recovered completely
following 10 days.
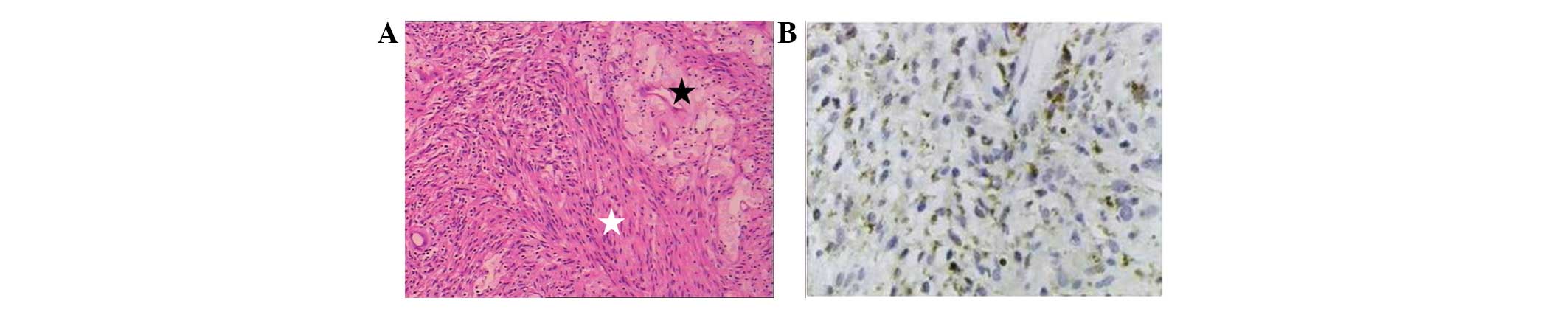
Inspection results by means of light microscopy
revealed that the tumor was a benign schwannoma. The tumor was
apparently spherical and circumscribed, with rich blood vessels. In
addition, the cut surface was light yellow with a hard texture.
Histologically, the tumor consisted of a small number of atypical
and fibroblast-like cells with breezing borders. Sections of the
cells were arranged in a scattered manner and oval vacuolated cell
nuclei were observed. There were alternating hypercellular and
hypocellular areas (Antoni A and Antoni B patterns). The
hypercellular areas presented elongated spindle cells, along with
nuclear palisading forming Verocay bodies; whereas the hypocellular
areas presented loosely arranged neoplastic cells with thick-walled
blood vessels (Fig. 3A). The tumor
cells were rarely arranged into interlaced and circinate shapes and
there was no observation of Verocay bodies. Immunohistochemical
examination revealed that the tumor cells were locally positive for
CD68, while negative for CD117, CD34 and desmin (Fig. 3B). Based on these characteristics,
the tumor was finally diagnosed as giant schwannoma originating
from sacrum. There has been no evidence of recurrence for 2 years
since the surgery.
Discussion
Schwannomas are benign neoplasms arising from the
nerve sheath. Unusual locations, including the head, neck,
peripheral nervous system, liver, pancreas, esophagus, stomach and
peritoneum, have been previously reported (7–12).
Schwannomas occurring in the pelvis are rare and account for only
1% of cases. Although the tumor arises from the peripheral nerve
sheath, it rarely elicits any clinically detectable neurological
deficits (13). Most often,
detection is late and the tumors may be painless while growing to
an extremely large size. The current case report showed that the
patient exhibited severe and painful symptoms and presented with a
giant abdominal mass with features of constipation and uroschesis.
Compression of neurovascular structures explains the ability of the
tumors to cause severe abdominal pain. However, schwannomas are
rarely large enough to obstruct the lumen and ureter.
Ovarian teratomas are an extremely common type of
abdominal tumor. Although fairly distinct in clinical and
histological presentation, preoperative diagnosis of a schwannoma
is not easy owing to a lack of distinguishing features on imaging
studies, such as B-scan ultrasound or CT, between schwannomas and
teratomas. MRI and CT are ideally suited to detect sacral pathology
and delineate the soft tissue and bony components. The majority of
benign ovarian teratomas without bony destroying present on CT scan
(14). Nyapathy et
al(15) previously reported a
giant schwannoma arising from the sigmoid, with bone window axial
CT sections of a large mass with erosions of the anterior cortex of
the sacrum. In the present study, no bony destruction was found in
the preoperative CT.
Previous studies have reported the misdiagnosis of
schwannomas as psoas abscesses (16) and ovarian dermoid cysts (17), but rarely as ovarian teratomas
occurring in the two genders and at all ages. Tumor markers,
including AFP and CA-125, have contributed to the differential
diagnosis between teratomas and schwannomas. However, the
probability of a schwannoma while negative for these markers must
be taken into consideration. It has been previously reported
(18) that 7.5% of ovarian
teratomas are positive for the expression of AFP and 22.6% for
CA125. Therefore, AFP and CA125 are not the specific criterion for
predicting ovarian teratomas. B-scan ultrasound revealing a
leftward adnexal mass is likely to be an additional major cause of
misdiagnosis. Preoperative CT also shows asymmetrical density of
the tumor. In addition, specific symptoms, such as stomach ache,
astriction and dysuria, were in accordance with the clinical
manifestation of ovarian teratomas.
On the treatment side, surgical excision has been
radically curative in a case of benign schwannoma and recurrence
has been detected in few patients following incomplete removal.
However, it must be noted that the pelvis is rich with blood
vessels that favors hemorrhage during surgery. Tang et
al(19) reported that 39.88% of
the patients accepting sacral tumor resection exhibited blood loss
of >3,000 ml. The authors results indicated that blood volume
loss is affected mainly by tumor location, volume and blood supply.
Hemorrhage is a serious intraoperative risk in cases where major
vessels are situated near the tumor and there are currently several
reports of unsuccessful tumor excision and intraoperative
mortalities (20).
In summary, the present case report described a rare
giant presacral schwannoma in the pelvic cavity, with notable
observations of its clinical manifestations of constipation,
dysuria and severe abdominal pain. Histological observations make a
definitive diagnosis, but the preoperative clinical manifestations
and details of the differential diagnosis were ignored. If
fine-needle aspiration biopsy of the tumor had been offered, the
misdiagnosis may have been avoided. The follow-up process has been
accomplished and patients have recovered. The current report
analyzed the clinical and imaging features of the tumor to
highlight possible diagnostic and management methods.
References
|
1
|
Klimo P Jr, Rao G, Schmidt RH and Schmidt
MH: Nerve sheath tumors involving the sacrum. Case report and
classification scheme. Neurosurg Focus. 15:E122003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang Y, Yu J, Qu L and Li Y:
Calcification of vestibular schwannoma: a case report and
literature review. World J Surg Oncol. 10:2072012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Huang Y and Wei W: Choroidal schwannoma
presenting as nonpigmented intraocular mass. J Clin Oncol.
30:e315–e317. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Khoo HM and Taki T: Periventricular
intraparenchymal schwannoma. Case report Neurol Med Chir (Tokyo).
52:603–607. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cugati G, Singh M, Symss NP, et al:
Primary intrasellar schwannoma. J Clin Neurosci. 19:1584–1585.
2012. View Article : Google Scholar
|
|
6
|
Sando IC, Ono S and Chung KC: Schwannoma
of the hand in an infant: case report. J Hand Surg Am.
37:2007–2011. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Akiyoshi T, Ueda Y, Yanai K, et al:
Melanotic schwannoma of the pancreas: report of a case. Surg Today.
34:550–553. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bilici S, Akpınar M, Yiğit O and Günver F:
Ancient schwannoma of the tongue: a case report. Kulak Burun Bogaz
Ihtis Derg. 21:234–236. 2011. View Article : Google Scholar
|
|
9
|
Fukuchi M, Naitoh H, Shoji H, et al:
Schwannoma of the stomach with elevated preoperative serum
carbohydrate antigen 19-9: report of a case. Surg Today.
42:788–792. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim SH, Kim NH, Kim KR, et al: Schwannoma
in head and neck: preoperative imaging study and intracapsular
enucleation for functional nerve preservation. Yonsei Med J.
51:938–942. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sasaki A, Suto T, Nitta H, et al:
Laparoscopic excision of retroperitoneal tumors: report of three
cases. Surg Today. 40:176–180. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Varaldo E, Crespi G, Ansaldo GL, et al:
Neurinoma originating from the recurrent nerve: report of a case.
Surg Today. 38:633–634. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Herregodts P, Vloeberghs M, Schmedding E,
et al: Solitary dorsal intramedullary schwannoma. Case report. J
Neurosurg. 74:816–820. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Buy JN, Ghossain MA, Moss AA, et al:
Cystic teratoma of the ovary: CT detection. Radiology. 171:697–701.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nyapathy V, Murthy UK, Chintamani J and
Sridhar DY: A case report of a giant presacral cystic schwannoma
with sigmoid megacolon. J Radiol Case Rep. 3:31–37. 2009.PubMed/NCBI
|
|
16
|
Kishi Y, Kajiwara S, Seta S, et al:
Retroperitoneal schwannoma misdiagnosed as a psoas abscess: report
of a case. Surg Today. 32:849–852. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ibraheim M, Ikomi A and Khan F: A pelvic
retroperitoneal schwannoma mimicking an ovarian dermoid cyst in
pregnancy. J Obstet Gynaecol. 25:620–621. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kawai M, Kano T, Kikkawa F, et al: Seven
tumor markers in benign and malignant germ cell tumors of the
ovary. Gynecol Oncol. 45:248–253. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tang X, Guo W, Yang R, et al: Risk factors
for blood loss during sacral tumor resection. Clin Orthop Relat
Res. 467:1599–1604. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kang CM, Kim DH, Seok JY and Lee WJ:
Laparoscopic resection of retroperitoneal benign schwannoma. J
Laparoendosc Adv Surg Tech A. 18:411–416. 2008. View Article : Google Scholar : PubMed/NCBI
|