Introduction
Myopericytoma is a rare neoplasm that commonly
arises from the skin and superficial soft tissues of distal
extremities, and is particularly rare in the visceral organs
(1). The present case of giant
myopericytoma showing kidney involvement is an extremely rare
occurrence. Myopericytoma demonstrates special morphological
features composed of myoid-appearing oval or spindle-shaped cells
with a concentric perivascular arrangement (1–3). In
addition, myopericytoma exhibits immunoreactivity for
muscle-specific and smooth muscle actin (1–4). The
current report presents a case of renal myopericytoma, and a
related literature review was performed to analyze the disease.
Written informed consent was obtained from the patient.
Case report
A 39-year-old male presented to the Department of
Urology (Second Affiliated Hospital of Anhui Medical University,
Hefei, China) with a 2-month history of a painless and palpable
mass in the region of the left abdomen, and without a history of
fever, weight loss, fatigue, urinary symptoms or hematuria. The
patient presented with normal blood pressure and stable vital
signs. Upon physical examination, no superficial lymph nodes were
found. In addition, results from an electrocardiogram, pulmonary
function test, stool analysis and other routine laboratory
examinations were all within normal limits, with the exception of
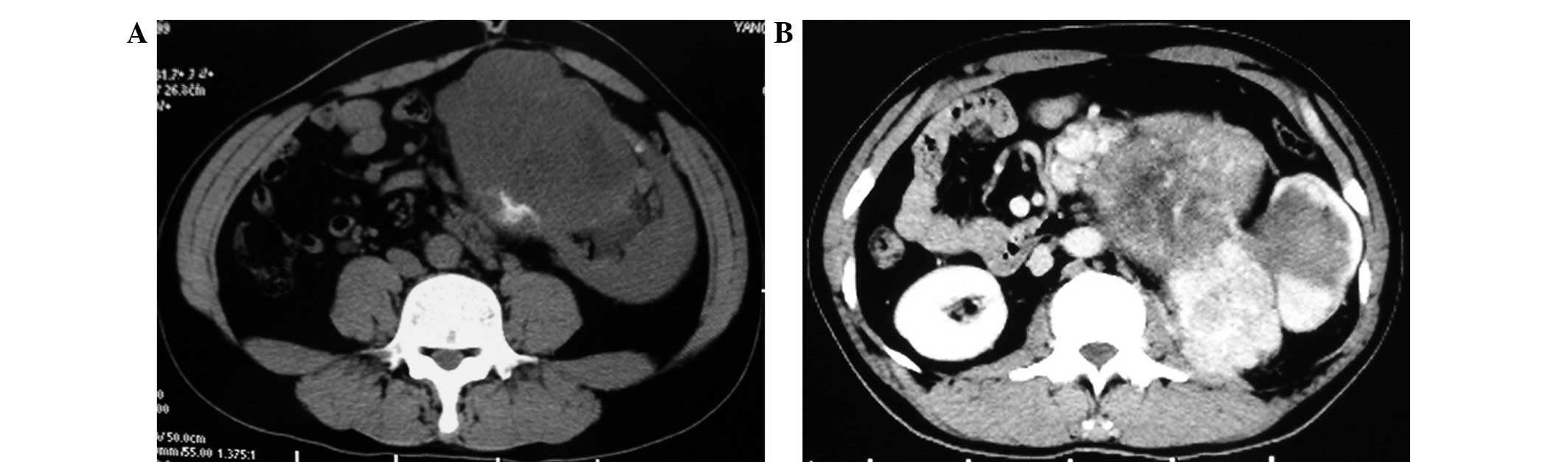
γ-glutamyltransferase (44 μmol/l). Unenhanced computed tomography
(CT) revealed a 9×10×18-cm3 mass that was heterogeneous
with a central lower density and showed a poorly defined margin
with poor calcification. No invasion was identified of the ambient
structures in the upper pole of the left kidney (Fig. 1A). Enhanced CT showed heterogeneous
attenuation with peripheral enhancement and central irregular
non-enhancement (Fig. 1B). However,
no evidence of lung metastasis was found. The patient underwent
radical nephrectomy, including lymphadenectomy, without adjuvant
therapy. The gross appearance of the resected specimen of the giant
mass showed a well-circumscribed, non-encapsulated, grayish-yellow
solid tumor with areas of necrosis in black that measured ~20×13×10
cm3 (Fig. 2A).
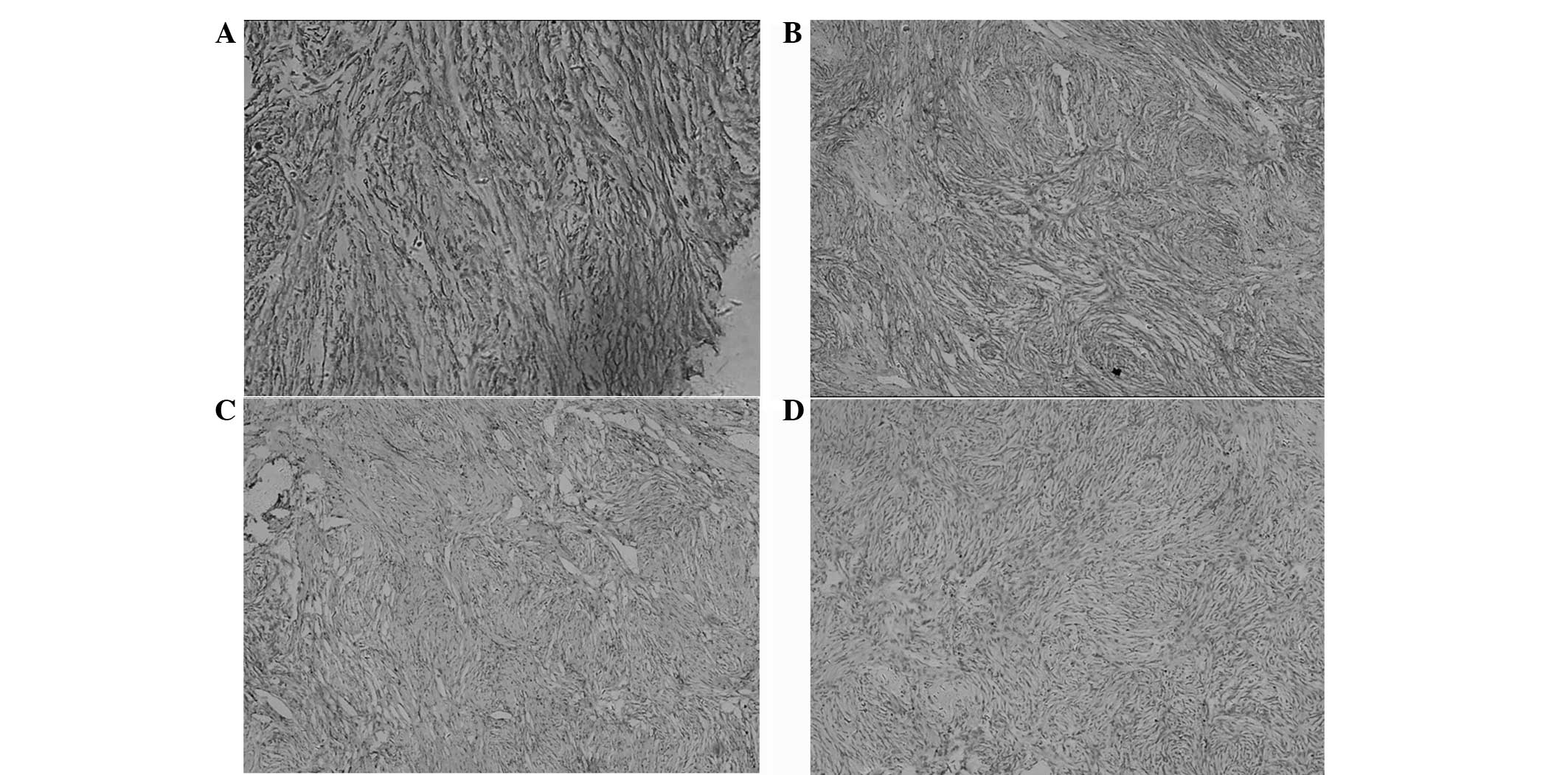
Histologically, the tumor was composed of spindle-shaped myoid
cells with a concentric arrangement of cells around numerous
variably-sized blood vessels, and the tumor cells were arranged in
nests or fascicles (Fig. 2B).
Nuclear atypia and mitotic figures were rarely found.
Immunohistochemically, the tumor cells were diffusely positive for
smooth muscle actin (Fig. 3A),
cluster of differentiation (CD)10 (Fig.
3B) and had a Ki-67 index of <1% (Fig. 3C). However, staining was negative
for CD34, desmin, S-100 protein (Fig.
3D), cytokeratin, human melanoma black (HMB)-45, B-cell
lymphoma (Bcl)-2 and CD99. A routine follow-up demonstrated no
signs of local or distant metastatic recurrence for 20 months.
Discussion
Myopericytoma is a rare neoplasm that commonly
arises from the skin and superficial soft tissues of the distal
extremities, including the trunk, head and neck regions (1–4). In
the majority of cases, myopericytoma is generally <4 cm in
diameter, and its occurrence is particularly rare in the visceral
organs. The present case of giant myopericytoma showing visceral
organ involvement is extremely rare. A thorough review of
previously published studies written in English revealed that renal
myopericytoma was first reported by Lau et al in 2010
(1). The term myopericytoma was
first proposed by Requena et al(3), and in 1998, Granter et
al(2) specified the
morphological and immunohistochemical characteristics of
myopericytoma. In 2002, the World Health Organization bagan to use
the term myopericytoma, and referred to it as a member of the
pericytic group in the Classification of Tumors of Soft Tissue and
Bone (5). Myopericytoma is
morphologically heterogeneous and typified by oval/spindle-shaped
cells with characteristic perivascular concentric growth and myoid
differentiation (1–4). Immunohistochemical analysis of the
tumor is positive for muscle-specific and smooth muscle actin,
which are characteristic of myopericytoma and useful for its
diagnosis and differential diagnosis (1–5). In
addition, the tumor cells of myopericytoma have been found to
express immunopositivity for desmin in a few cases. By contrast, in
studies including the present case, immunohistochemical staining
was negative for desmin, S-100 protein, cytokeratin and HMB-45
(1–5) Additionally, the present myopericytoma
exhibited immunopositivity for CD10. The majority of myopericytoma
cases, including the current case, are negative for CD34, a result
which differs from that of another case previously reported in the
literature (1).
Myopericytoma is generally considered a slow-growing
neoplasm. Commonly, patients with renal myopericytoma are
asymptomatic, with the tumor found incidentally by routine health
checks. For this reason, an early diagnosis of myopericytoma is
difficult for urologists. Ultrasonography, CT and MRI may highlight
evidence of renal myopericytoma. Myopericytoma has atypical imaging
features, although CT scans often show a heterogeneous density mass
with peripheral contrast enhancement, unsmoothed margins and single
or multiple slow-growing reactive lymph nodes (6).
The differential diagnosis of renal myopericytoma
includes angioleiomyoma, glomus tumors, solitary fibrous tumors and
myofibroma. Angiomyolipoma is the most common renal mesenchymal
tumor, composed of variable thick-walled blood vessels, mature
smooth muscle and mature fat. Angiomyolipoma is similar to
myopericytoma in morphological features, and expresses
immunoreactivity for HMB-45, S-100 and desmin, whereas
myopericytoma rarely expresses immunoreactivity for desmin
(7). Angiomyolipomas generally show
a well-defined, circumscribed, hypodense mass on CT. The morphology
and immunohistochemical features of myopericytoma are useful for
its differential diagnosis. Glomus tumors exhibit a perivascular
pattern of growth with cuboidal epithelioid cells, have an organoid
pattern of the glomus organ and lack the characteristic
perivascular concentric growth of myopericytoma (1,7–9). A
solitary fibrous tumor is different from myopericytoma, as it
exhibits immunoreactivity for the expression of vimentin, CD34,
Bcl-2 and CD99 (1,10). In the present case, the absence of
expression of CD34, CD99 and vimentin provided evidence for the
differential diagnosis of renal myopericytoma. Myofibroma may
exhibit a number of the characteristic microscopic features of
mature bipolar myofibromatosis, including a zonal or biphasic
architecture, fascicles of spindle cells and myoid nodules
(1,8).
Although no standard treatment for renal
myopericytoma has been established, complete surgical excision of
the lesion may be the only potentially curative treatment. The
clinical presentation and histological features of myopericytoma
are usually benign, but a fraction of malignant myopericytomas with
local recurrence or distant metastases have been reported. The size
of the tumor does not necessarily correlate with malignant
potential, but the distinction between benign and malignant
variants has been determined by criteria with malignant features,
including poor circumscription, high-mitotic activity, necrosis and
nuclear pleomorphism (8,9). In the current case, the tumor appeared
benign as the Ki-67 index was <1% and the mitotic activity was
low; however, in contrast, it was >4 cm in size. A partial
nephrectomy is performed for myopericytomas <4 cm in size, but
larger tumors (>4 cm) may be treated by radical surgery.
Chemotherapy or radiation therapy is unnecessary, although the
timing and frequency of follow-up is essential. There is little
available information with regard to targeted molecular therapies
and prognosis; therefore, in the present case, the patient was
treated with surgical exxision without adjuvant therapy.
In conclusion, renal myopericytoma is generally
considered to be a relatively rare, slow-growing and benign tumor,
with histological characteristics of the perivascular proliferation
of myoid differentiated pericytic cells, which show a slow disease
progression. Surgical excision may be the only potentially curative
treatment for renal myopericytoma. However, the few previously
reported cases may not be sufficient to allow the clinical outcome
to be fully evaluated. Longer follow-up periods may also be
necessary to definitively evaluate the clinical outcome of renal
myopericytoma.
Acknowledgements
The present study was supported by a grant from the
Anhui Provincial Natural Science Project of Higher Education (no.
ZD200907).
References
|
1
|
Lau SK, Klein R, Jiang Z, Weiss LM and Chu
PG: Myopericytoma of the kidney. Hum Pathol. 41:1500–1504. 2010.
View Article : Google Scholar
|
|
2
|
Granter SR, Badizadegan K and Fletcher CD:
Myofibromatosis in adults, glomangiopericytoma, and myopericytoma:
a spectrum of tumors showing perivascular myoid differentiation. Am
J Surg Pathol. 22:513–525. 1998. View Article : Google Scholar
|
|
3
|
Requena L, Kutzner H, Hügel H, Rütten A
and Furio V: Cutaneous adult myofibroma: a vascular neoplasm. J
Cutan Pathol. 23:445–457. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Matsuyama A, Hisaoka M and Hashimoto H:
Angioleiomyoma: a clinicopathologic and immunohistochemical
reappraisal with special reference to the correlation with
myopericytoma. Hum Pathol. 38:645–651. 2007. View Article : Google Scholar
|
|
5
|
Fletcher CDM, Unni KK and Mertens F: World
Health Organization Classification of Tumors. Tumors of Soft Tissue
and Bone. IARC Press; Lyon: 2002
|
|
6
|
Chu ZG, Yu JQ, Yang ZG, Zhu ZY and Yuan
HM: Myopericytoma involving the parotid gland as depicted on
multidetector CT. Korean J Radiol. 10:398–401. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mentzel T, Dei Tos AP, Sapi Z and Kutzner
H: Myopericytoma of skin and soft tissues: clinicopathologic and
immunohistochemical study of 54 cases. Am J Surg Pathol.
30:104–113. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Terada T: Minute myopericytoma of the
neck: a case report with literature review and differential
diagnosis. Pathol Oncol Res. 16:613–616. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McMenamin ME and Fletcher CD: Malignant
myopericytoma: expanding the spectrum of tumours with myopericytic
differentiation. Histopathology. 41:450–460. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Takizawa I, Saito T, Kitamura Y, Arai K,
Kawaguchi M, Takahashi K and Hara N: Primary solitary fibrous tumor
(SFT) in the retroperitoneum. Urol Oncol. 26:254–259. 2008.
View Article : Google Scholar : PubMed/NCBI
|