Introduction
Adenomatoid tumors are benign masses usually located
within the genital tract organs of males and females (1). The majority involve the epididymis,
but sites may also include the testicular tunica, spermatic cord
and, in rare cases, the testicular parenchyma (2–4).
Extragenital sites of involvement include the heart, lymph nodes,
adrenal glands, intestinal mesentery, omentum and retroperitoneum
(5). The majority present as small,
firm, asymptomatic intrascrotal masses which can be mistaken for a
large variety of diseases, including benign lesions and
intratesticular malignancies. In numerous cases, diagnosis of
adenomatoid tumors results from incidental pathological findings
following orchidectomy. Therefore, it is imperative that urologists
be aware of the features of this rare lesion to avoid erroneous
diagnosis and unnecessary extensive surgical excision. The patients
provided their written informed consent.
Case reports
Between 2006 and 2013, two patients with a one-year
history of an asymptomatic mass in the scrotum (Table I) were admitted to Peking University
Shenzhen Hospital (Shenzhen, China).
 | Table IPhysical characteristics and clinical
and radiological features of the patients. |
Table I
Physical characteristics and clinical
and radiological features of the patients.
| No. | Age, years | Chief complaint | Date of
presentation | AFP | β-HCG | Ultrasonography | CT |
|---|
| 1 | 40 | Asymptomatic mass in
scrotum | 2006 | Normal | Normal | Well-defined
heterogeneous nodule | No metastasis |
| 2 | 39 | Asymptomatic mass in
scrotum | 2013 | Normal | Normal | Hypoechoic
homogeneous mass | Not performed |
Case 1
A 40-year-old patient presented with a palpable and
painless swelling with a gradual increase in testicular size over
one year. The patient had no history of local trauma or surgery to
the scrotum. Local examination revealed a firm and painless mass of
1×1 cm fixed to the testis in the left side of the scrotum. The
overlying skin appeared normal and the inguinal lymph nodes were
not palpable. Serum levels of α-fetoprotein (AFP) and β-human
chorionic gonadotrphin (β-HCG) were within normal range.
Ultrasonography revealed a well-defined, heterogeneous, round
nodule with no capsule at the lower pole of the testis. Computed
tomography scan of the pelvis revealed no significant
intra-abdominal lymphadenopathy.
Under suspicion of malignancy, radical orchidectomy
was prescribed. During the surgery, paratesticular nodular masses
were identified between the tunica vaginalis and the head of the
epididymis, firm in consistency with no evidence of invasion which
is indicates that there is a high possibility of a benign
lesion.
Case two
A 39-year-old male presented with a palpable mass in
the right side of the scrotum. There was no history suggestive of
urinary infection, genito-urinary tuberculosis or
epididymo-orchitis. On local examination, a mass was identified in
the right testis which was 2×1.5 cm in size, firm in consistency
and well-marginated with smooth swelling. The overlying skin and
surrounding adenexa appeared normal. Serum levels of AFP and β-HCG
were within normal limits. Scrotal ultrasound revealed a solid mass
in the epididymal body of the right scrotum that was hypoechoic
compared with the testicular parenchyma.
Management
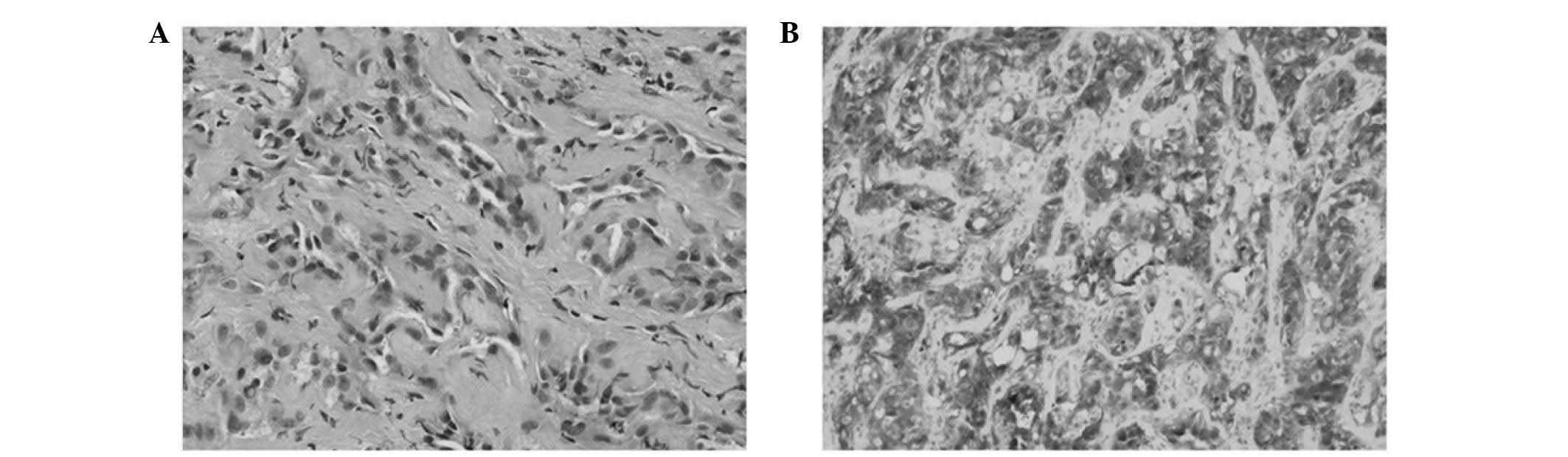
Limited local excisions were performed in the two
cases and the morphological and immunohistochemical features are
presented in Table II and Fig. 1. At the time of writing, follow-ups
have revealed no recurrence.
 | Table IIMorphological and pathological
features of the masses. |
Table II
Morphological and pathological
features of the masses.
| No. | Size, cm | Density | Location | Microscopic
features |
Immunohistochemistry |
|---|
| 1 | 1×1 | Firm | Tunica vaginalis | Channels lined by
flattened cells with cytoplasmic vacuolation, myxoid change | CK+,
D2–40+, CR+, CD68− |
| 2 | 2×1.5 | Firm | Epididiymis | Tubules of cuboidal
cells with cytoplasmic vacuolation, bland nuclei, fibrous
stroma | WT1+,
calretinin+, D2–40+, CK5/6− |
Discussion
Adenomatoid tumors are relatively uncommon benign
tumors of mesothelial origin frequently located within the genital
tract organs (6). In the female
genital tract, adenomatoid tumors may be located in the uterus,
fallopian tubes and ovarian hilus, and the epididymis, spermatic
cord, prostate and ejaculatory duct in the male (1). Adenomatoid tumors account for ~30% of
all paratesticular tumors and are are therefore the most common
type of paratesticular tissues (7).
In contrast to testicular neoplasms, which are 95% malignant,
paratesticular tumors are more frequently benign and may be cured
by local excision (7). However, it
is not always easy to differentiate between the two masses.
Adenomatoid tumors present either as an incidental
finding or a slow growing scrotal mass, most often in patients
between 30 and 50 years of age. Enlargement is usually painless and
the scrotal skin and surrounding adenexa remain normal. The
majority of adenomatoid tumors are present asymptomatically for
several years and are uniformly benign. Rarely, patients have
presented with testicular pain. In the majority of cases,
adenomatoid tumors present as painless, firm, intrascrotal masses
of <2 cm diameter.
The ultrasound features of adenomatoid tumors may
vary but usually include a well-defined, homogeneous, round nodule
with variable echogenicity ranging from hypoechoic to hyperechoic.
On magnetic resonance imaging, such masses are slightly hypointense
compared with the testicular parenchyma on T2-weighted images and,
on post-contrast images, exhibit similar enhancement to the testis
(8).
Microscopically, they contain a number of
histological patterns: adenoid or tubular glandular, angiomatoid,
solid, cystic or transitional (9),
which may pose a range of diagnostic problems, particularly for
differentiating adenomatoid tumors from other paratesticular tumors
(10). An understanding of the
pathological features of paratesticular tumors is crucial for
accurate diagnosis (Table III)
(9,10).
 | Table IIIMorphological and immunohistochemical
features of paratesticular tumors. |
Table III
Morphological and immunohistochemical
features of paratesticular tumors.
| Lesion | Microscopic
features |
Immunohistochemistry |
|---|
| Adenomatoid
tumor | Cords and tubules of
cuboidal to columnar cells with vacuolated cytoplasm and fibrous
stroma | WT1+,
D2–40+, calretinin+, CK5+,
vimentin+ |
| Fibrous
pseudotumor | Dense fibrous tissue
with interspersed fibroblasts and mixed inflammatory cells | Not clear |
| Cystadenoma | Epithelial-like tumor
cells with a sertoliform growth pattern and cystic dilatations | Inhibin+,
S-100+, CD99+ |
| Leiomyomas | Interlacing and
whorling bundles of smooth muscle cells |
Desmin+ |
| Serous borderline
tumor | Cystic with numerous
intracystic, blunt papillae lined by stratified epithelial cells
having minimal to mild cytologic atypia | ER+,
PR+, CD15+, MOC-31+,
calretinin− |
| Mesothelioma | Epithelioid cells
arising from the tunica vaginalis with papillary, tubulopapillary
or solid architectural patterns |
Calretinin+, WT1+,
D2–40+, CK7+, CK5/6+ |
An asymptomatic mass in the scrotum is a nonspecific
symptom that can be caused by benign lesions and malignances.
Ultrasound has become a first-line imaging technique, used to
assess acute and nonacute conditions of the scrotum, and in many
cases it is the only modality required (8). When ultrasound confirms that the mass
is extratesticular (particularly if located in the epididymis),
circumscribed and homogeneous with no evidence of invasion to
adjacent tissue, in addition to typical clinical features and
normal levels of serum tumor makers, a diagnosis of paratesticular
mass can be made, as in case two.
In many cases, the similar imaging studies and
clinical signs make it hard to distinguish adenomatoid tumors from
malignant intratesticular tumors, leading to unnecessary extensive
surgical excision of the whole testis (11). The present study is the first
reported case to avoid extensive surgical excision based on
intra-operative evaluation when this dilemma was encountered.
In summary, adenomatoid tumors in the testis are
rare disorders that may pose difficulty for diagnosis, particularly
when occurring in unusual locations where the aim is to preserve
endogenous testicular function. This report presents two cases of
adenomatoid tumors of the testis with the symptom of asymptomatic
mass in the scrotum. Local excisions were performed based on
thorough analysis of the clinical features, tumor makers,
radiological images and intra-operative findings. A complete
understanding of the pathological features of paratesticular tumors
is critical in making accurate diagnoses.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant no. 81101922), the Medical
Scientific Research Foundation of Guangdong Province of China
(grant nos. A2012584 and A2013606) and the Science and Technology
Development Fund Project of Shenzhen (grant no.
JCYJ20130402114702124).
References
|
1
|
Schwartz EJ and Longacre TA: Adenomatoid
tumors of the female and male genital tracts express WT1. Int J
Gynecol Pathol. 23:123–128. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Alexiev BA, Xu LF, Heath JE, et al:
Adenomatoid tumor of the testis with intratesticular growth: a case
report and review of the literature. Int J Surg Pathol. 19:838–842.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Monappa V, Rao AC, Krishnanand G, et al:
Adenomatoid tumor of tunica albuginea mimicking seminoma on fine
needle aspiration cytology: a case report. Acta Cytol. 53:349–352.
2009. View Article : Google Scholar
|
|
4
|
Di Pierro GB, Sciarra A, Innocenzi M and
Cristini C: Rare case of multiple adenomatoid tumors arising from
tunica vaginalis of testis and epididymis. Actas Urol Esp.
34:560–561. 2010.(In Spanish).
|
|
5
|
Makkar M, Dayal P, Gupta C and Mahajan N:
Adenomatoid tumor of testis: A rare cytological diagnosis. J Cytol.
30:65–67. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Alam K, Maheshwari V, Vashney M, et al:
Adenomatoid tumour of testis. BMJ Case Rep. 2011.2011:
|
|
7
|
Goel A, Jain A and Dalela D: Can radical
orchiectomy be avoided for paratesticular adenomatoid tumor? Indian
J Urol. 27:556–557. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aganovic L and Cassidy F: Imaging of the
scrotum. Radiol Clin North Am. 50:1145–1165. 2012. View Article : Google Scholar
|
|
9
|
Amin MB: Selected other problematic
testicular and paratesticular lesions: rete testis neoplasms and
pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol.
18(Suppl 2): S131–S145. 2005. View Article : Google Scholar
|
|
10
|
Rubenstein RA, Dogra VS, Seftel AD and
Resnick MI: Benign intrascrotal lesions. J Urol. 171:1765–1772.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pacheco AJ, Torres JL, de la Guardia FV,
Arrabal Polo MA and Gómez AZ: Intraparenchymatous adenomatoid tumor
dependent on the rete testis: A case report and review of
literature. Indian J Urol. 25:126–128. 2009. View Article : Google Scholar : PubMed/NCBI
|