Introduction
The incidence of a pure primary ovarian squamous
cell carcinoma (SCC) is extremely rare when not associated with
pre-existing ovarian lesions, such as dermoid cysts, Brenner tumors
or endometriosis (whose presence is normally indicative of ovarian
SCC) (1). To date, only 30 cases of
pure primary ovarian SCC have been reported worldwide. Due to the
rarity of pure primary ovarian SCC, the clinical features of the
disease have not been established and effective treatments are yet
to be identified. Subsequent to optimal tumor devulking, patients
with early-stage pure primary ovarian SCC may remain disease-free.
However, those patients with advanced-stage disease may experience
a poorer outcome, despite treatment with postoperative chemotherapy
and/or radiotherapy. The present case study describes a patient
with pure primary ovarian SCC, and presents a review of the
literature. Written informed consent was obtained from the
patient’s family.
Case report
A 46-year-old female (gravida 3, para 2) was
referred to the Department of Pulmonary Medicine (Dong-A
University, College of Medicine, Busan, Republic of Korea) with a
history of progressive coughing that had been apparent for three
months. Upon chest computed tomography (CT), performed at a local
clinic on February 11, 2012, a diagnosis of lung cancer was
suspected. The patient was immediately hospitalized and underwent
bronchoscopy. A transbronchial lung biopsy revealed an SCC of
unknown primary site.
To locate the primary site of the metastatic lung
cancer, an abdominal CT and positron emission tomography-CT scan
was performed. The results of the scans revealed a left-sided
pelvic mass, a left hydronephrosis and multiple regions of lymph
node metastasis in the pelvic, abdominal, mediastinal and
supraclavicular areas.
The patient was referred to the Department of
Obstetrics and Gynecology (Dong-A University, College of Medicine)
for gynecological treatment. Abdominal exploration was performed on
February 24, 2012, which revealed that the solid mass arose from
the left adnexal area, was densely adhered to the sigmoid colon and
external iliac vessel, and was encapsulating the left ureter. A
total abdominal hysterectomy, bilateral salpingo-oophorectomy,
adhesiolysis between the tumor and sigmoid colon, segmental
resection of the sigmoid colon and reanastomosis were performed.
Following segmental resection, the patient underwent an end-to-end
anastomosis of the left ureter.
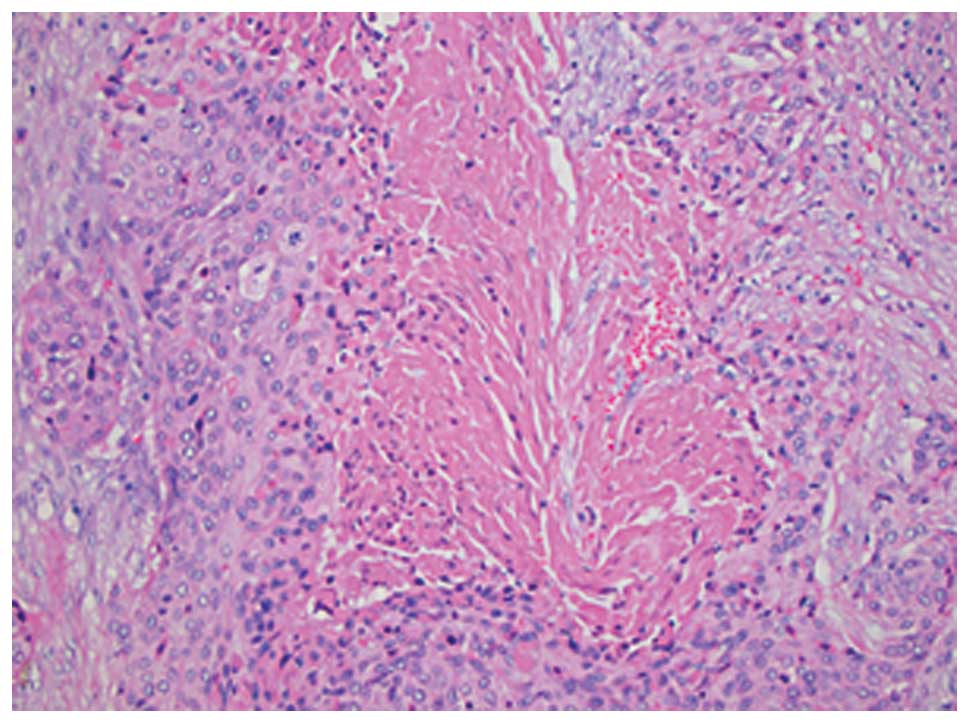
Histopathological analysis confirmed a pure SCC
arising from the left ovary. The pathological results were notable
for the absence of any associated dermoid cyst or features
suggestive of endometriosis, (Fig.
1). The patient was subsequently diagnosed with stage IVB pure
primary ovarian SCC with lung metastases according to the
International Federation of Gynecology and Obstetrics staging
system (2). Following surgery, the
patient was administered a six-course adjuvant chemotherapy
regimen, consisting of paclitaxel (175 mg/m2) and
carboplatin (5 mg/ml/min) at three-week intervals. Despite the
initiation of first-line adjuvant chemotherapy, clinical and
radiographical evidence identified tumor progression and
aggravation of the lung metastasis. Therefore, a second-line
three-course chemotherapy regimen, consisting of topotecan (1
mg/m2) and cisplatin (50 mg/m2) at three-week
intervals, and a third-line three-course regimen, consisting of
etoposide and ifosfamide at three-week intervals, was administered.
Despite this, treatment was unsuccessful and the patient succumbed
to the disease on February 12, 2013, following cardiopulmonary
arrest.
Discussion
Primary ovarian SCC is rare, with the majority of
cases preceded by dermoid cysts. Alternatively, cases of primary
ovarian SCC may be associated with Brenner tumors and endometriosis
(3). Ovarian SCCs that are reported
to arise within a dermoid cyst appear to be incidental histological
findings (4). In total, ~2% of
cases of primary ovarian SCC originate from the malignant
transformation of a dermoid cyst (5). A previous study of metastatic ovarian
tumors revealed that a total of 2.5% are of the squamous cell type,
with the majority of cases of metastatic SCC originating by direct
extension from the cervix (6).
Furthermore, of the reported cases of pure ovarian SCC, the most
significant association identified was with cervical dysplasia
(7,8). However, this association was not
identified in the present case study, as revealed by a negative
pre-operative pap smear and by post-operative pathological
analysis. The incidence of pure primary ovarian SCC is extremely
low, with thirty cases described by previous studies (Table I) (1,3,7–21).
Previous studies revealed that stage and grade of tumors correlate
with overall survival in pure primary ovarian SCC patients. Thus,
patients with early-stage pure primary ovarian SCC may remain
disease-free after optimal debulking. However, those patients with
advanced-stage disease may experience a poorer outcome, despite
treatment with post-operative chemotherapy and/or radiotherapy
(7). Due to the rare nature of pure
primary ovarian SCC, effective adjuvant chemotherapy or
radiotherapy regimens have not yet been established. In the present
case study, the patient was unresponsive to the chemotherapy
regimen administered following surgical debulking. In the twelfth
month subsequent to surgery, the patient succumbed to the
rapidly-progressive disease. The chemotherapy regimens administered
in the present study, or the doses used, may be unsuitable for this
ovarian malignant cell type. Therefore, to identify effective
therapies for the treatment of pure primary ovarian SCC, further
clinical investigations are required.
 | Table IClinicopathological features of pure
primary squamous cell carcinoma reported in the literature. |
Table I
Clinicopathological features of pure
primary squamous cell carcinoma reported in the literature.
| First author/s
(ref.) | Year | Case | Age, years | FIGO stage | Grade | Treatment | Follow-up,
months |
|---|
| Genadry et al
(11) | 1979 | 1 | 41 | CIS | 1 | TAH, BSO | NR |
| McGrady et al
(12) | 1993 | 2 | 53 | CIS | 1 | TAH, BSO | Alive |
| Sworn et al
(13) | 1995 | 3 | 39 | CIS | 3 | TAH, BSO | Alive, 60 |
| Yetman and Dudzinski
(8) | 1989 | 4 | 33 | I | 2 | TAH, BSO | Alive, 15.6 |
| Black and Benitez
(14) | 1964 | 5 | 35 | I | 1 | TAH, BSO | NR |
| Shingleton et
al (15) | 1974 | 6 | 54 | I | 1 | RO, RT | DOD, 6 |
| Mai et al
(16) | 1996 | 7 | 40 | I | 2 | TAH, BSO | NR |
| Macko and Johnson
(17) | 1983 | 8 | 90 | I | 2 | UO | Alive, 30 |
| Chen (18) | 1988 | 9 | 49 | I | 1 | TAH, BSO, RT | Alive, 12 |
| Balat et al
(19) | 2001 | 10 | 40 | IB | NR | TAH, BSO, PLND,
appendectomy, right nephrectomy, chemotherapy | DOD, 24 |
| Kashimura et
al (9) | 1989 | 11 | 61 | II | NR | TAH, BSO, RT,
chemotherapy | DOD, 9 |
| | 12 | 42 | III | NR | LSO, RT | DOD, 8 |
| | 13 | 50 | I | NR | TAH, BSO, RT | Alive, 14.4 |
| Pins et al
(7) | 1996 | 14 | 73 | IIA | 3 | TAH, BSO, RT | DOD, 49 |
| | 15 | 61 | IIB | 3 | TAH, BSO, RT,
chemotherapy | Alive, 60 |
| | 16 | 55 | IIB | 3 | TAH, BSO, TD,
chemotherapy | Alive, 30 |
| | 17 | 38 | IIC | 3 | TAH, BSO,
chemotherapy | DOD, 8 |
| | 18 | 64 | IB | 2 | RSO, LO | AWD, 60 |
| | 19 | 55 | IIIB | 3 | TAH, BSO,
chemotherapy | DOD, 2 |
| | 20 | 52 | IIIC | 3 | Ovarian, omental
biopsy | NR |
| | 21 | 46 | IIIC | 3 | Ovarian, omental
biopsy | NR |
| | 22 | 27 | IIIC | 3 | TAH, BSO,
chemotherapy | DOD, 1 |
| | 23 | 70 | IIIC | 3 | TAH, BSO,
chemotherapy | DOD, 5 |
| | 24 | 73 | IV | 3 | LSO, RT | DOD, 1 |
| Ben-Baruch et
al (3) | 1988 | 25 | 65 | III | 2 | TAH, BSO, iliectomy,
TD, chemotherapy | DOD, 6 |
| Amjad and Pal
(20) | 2008 | 26 | 31 | IIIC | 1 | TAH, BSO, TO, bowel
resection, chemotherapy | AWD, 1 |
| Radhi and Awad
(10) | 1990 | 27 | 64 | IV | 2 | TD | DOD, 9 days |
| Chien et al
(21) | 2005 | 28 | 63 | IV | 3 | TAH, BSO, PLND, TO,
TD | DOD, 7 |
| Park et al
(1) | 2010 | 29 | 76 | IIC | 1 | TAH, BSO, PLND,
PALND, TO, appendectomy, chemotherapy | Alive, 42 |
| | 30 | 48 | IV | 2 | TAH, BSO, PLND,
PALND, TO, appendectomy, chemotherapy | Alive, 6 |
| Present case | 2014 | 31 | 46 | IVB | 2 | TAH, BSO, TD, bowel
resection | DOD, 12 |
References
|
1
|
Park JY, Song JS, Choi G, Kim JH and Nam
JH: Pure primary squamous cell carcinoma of the ovary: a report of
two cases and review of the literature. Int J Gynecol Pathol.
29:328–334. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mutch DG and Prat J: 2014 FIGO staging for
ovarian, fallopian tube and peritoneal cancer. Gynecol Oncol.
133:401–404. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ben-Baruch G, Menashe Y, Herczeg E and
Menczer J: Pure primary ovarian squamous cell carcinoma. Gynecol
Oncol. 29:257–262. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dos Santos L, Mok E, Iasonos A, et al:
Squamous cell carcinoma arising in mature cystic teratoma of the
ovary: a case series and review of the literature. Gynecol Oncol.
105:321–324. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Peterson WF: Malignant degeneration of
benign cystic teratomas of the ovary; a collective review of the
literature. Obstet Gynecol Surv. 12:793–830. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Webb MJ, Decker DG and Mussey E: Cancer
metastatic to the ovary: factors influencing survival. Obstet
Gynecol. 45:391–396. 1975.PubMed/NCBI
|
|
7
|
Pins MR, Young RH, Daly WJ and Scully RE:
Primary squamous cell carcinoma of the ovary. Report of 37 cases.
Am J Surg Pathol. 20:823–833. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yetman TJ and Dudzinski MR: Primary
squamous carcinoma of the ovary: a case report and review of the
literature. Gynecol Oncol. 34:240–243. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kashimura M, Shinohara M, Hirakawa T,
Kamura T and Matsukuma K: Clinicopathologic study of squamous cell
carcinoma of the ovary. Gynecol Oncol. 34:75–79. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Radhi JM and Awad SM: Bilateral squamous
cell carcinoma of the ovary. Case report. Br J Obstet Gynaecol.
97:855–856. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Genadry R, Parmley T and Woodruff JD:
Secondary malignancies in benign cystic teratomas. Gynecol Oncol.
8:246–251. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McGrady BJ, Sloan JM, Lamki H and Fox H:
Bilateral ovarian cysts with squamous intraepithelial neoplasia.
Int J Gynecol Pathol. 12:350–354. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sworn MJ, Jones H, Letchworth AT,
Herrington CS and McGee JO: Squamous intraepithelial neoplasia in
an ovarian cyst, cervical intraepithelial neoplasia, and human
papillomavirus. Hum Pathol. 26:344–347. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Black WC and Benitez RE: Nonteratomatous
squamous-cell carcinoma in situ of the ovary. Obstet Gynecol.
24:865–868. 1964.PubMed/NCBI
|
|
15
|
Shingleton HM, Middleton FF and Gore H:
Squamous cell carcinoma in the ovary. Am J Obstet Gynecol.
120:556–560. 1974.PubMed/NCBI
|
|
16
|
Mai KT, Yazdi HM, Bertrand MA, LeSaux N
and Cathcart LL: Bilateral primary ovarian squamous cell carcinoma
associated with human papilloma virus infection and vulvar and
cervical intraepithelial neoplasia. A case report with review of
the literature. Am J Surg Pathol. 20:767–772. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Macko MB and Johnson LA: Primary squamous
ovarian carcinoma. A case report and review of the literature.
Cancer. 52:1117–1119. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen KT: Squamous cell carcinoma of the
ovary. Arch Pathol Lab Med. 112:114–115. 1988.PubMed/NCBI
|
|
19
|
Balat O, Aydin A, Camci C, Kutlar I and
Büyükberber S: Bilateral primary squamous cell carcinoma of the
ovary: a case report of isolated metastasis to the lateral pelvic
wall. Eur J Gynaecol Oncol. 22:445–446. 2001.
|
|
20
|
Amjad AI and Pal I: De novo primary
squamous cell carcinoma of the ovary: a case of a rare malignancy
with an aggressive clinical course. J Pak Med Assoc. 58:272–274.
2008.PubMed/NCBI
|
|
21
|
Chien SC, Sheu BC, Chang WC, Wu MZ and
Huang SC: Pure primary squamous cell carcinoma of the ovary: a case
report and review of the literature. Acta Obstet Gynecol Scand.
84:706–708. 2005. View Article : Google Scholar : PubMed/NCBI
|