Introduction
The term ‘hemangioendothelioma’ (HE) has been used
to describe a heterogenous group of vascular neoplasms, which are
intermediate between benign and malignant tumors (1). Cases of HE often progress to rare
metastasis and infrequent mortality, primarily arising in the soft
tissues of the extremities and organs, including anterior
mediastina and liver in adults (2).
HEs are primarily surgically excised. HEs from soft tissues often
exhibit a good prognosis, while HEs from internal organs often
exhibit a relatively poor prognosis, as patients often succumb
during surgery due to complications due to progress of the disease
itself (3).
As an important peripheral immune organ, the spleen
is rarely reported as the origin of HE tumors. To the best of our
knowledge, few cases of HE have been reported to have arisen from
the spleen in adults, and only one pediatric patient with splenic
HE has been described (4). The
current report presents the second pediatric patient to be
diagnosed with splenic HE. Furthermore a literature review is
conducted to summarize the clinical treatment and outcomes of
splenic HE.
Case report
A 9-year-old female patient presented to the
Department of Hepatobiliary Surgery, Shandong Cancer Hospital
(Jinan, China) due to 20-day intermittent abdominal pain. No
abnormalities were observed during the physical examination with
the exception of an enlarged spleen (degree II) (5). Laboratory tests were normal with the
exception of a slight increase in the serum levels of cancer
antigen 125 (45.4 U/ml, normal range ≤35 U/ml) and white blood
cells (11.5×109 per liter, normal range
4–10×109 per liter). Computed tomography (CT) scanning
revealed two tumor masses in the lower lobe of the splenic
parenchyma, with the larger one measuring 5.6 × 5.9 × 6.3 cm
(Fig. 1). The images are
characterized by a round, or round-like low density area with clear
boundary to the normal tissues, as revealed by the plain scanning,
and circular, radiative enhancement at the margin.
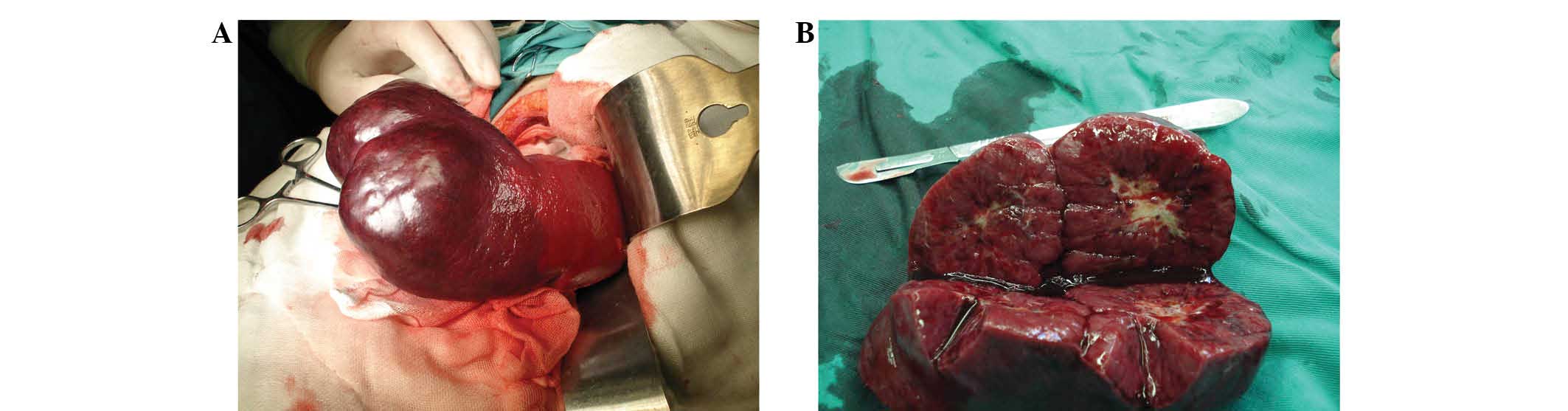
Initially a laparotomy was performed, and a rapid
diagnosis of the carcinoma was conducted, which revealed borderline
carcinoma with slight cellular heteromorphism. Due to this, a
partial splenectomy was performed. Written informed consent was
obtained from the patient’s parents. Following the surgery, a mass
was cut from the lower spleen lobe. The excised section showed a
well-circumscribed mass that was separate from the surrounding
splenic parenchyma. Upon further observation, two tumor masses,
growing in an exogenous pattern, were observed at the lower spleen
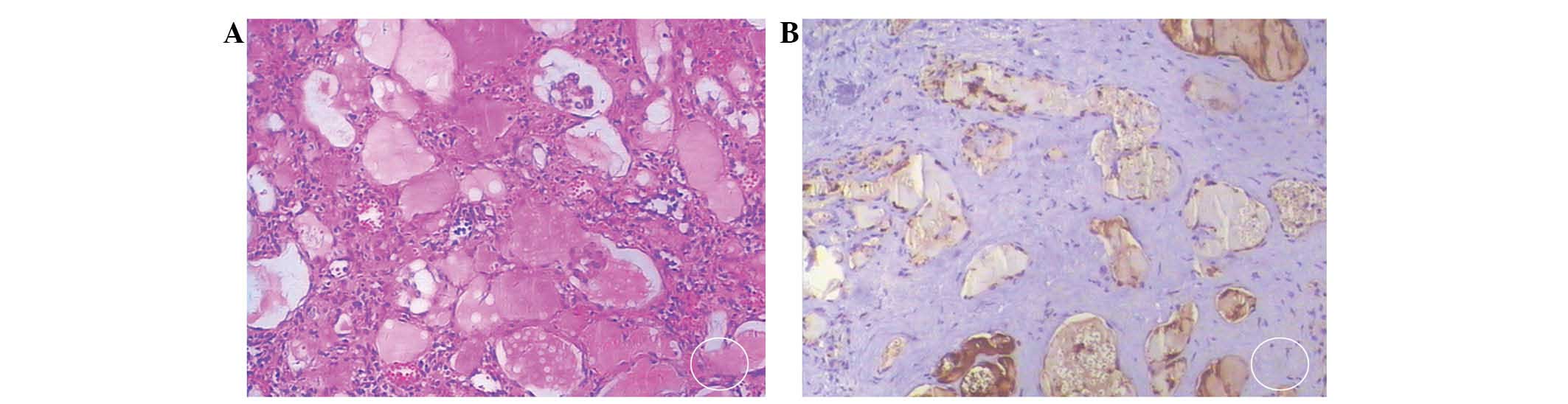
pole, measuring 6.0 × 6.0 × 5.5 cm and 5.0 × 5.0 × 4.0 cm (Fig. 2). Pathological examination indicated
that the tumor masses primarily consisted of capillaries and
well-differentiated great vessels (Fig.
3). In addition, a large volume of liquid was contained within
the great vessels, together with dispersed hyperplasia of the
vascular endothelial cells (VECs), which invaded the lumen. In the
immunohistochemical analysis, the tumor cells were positive for
CD31+, CD34+, FVIII+, Ki-67+<1%, pan CK+ and TG−. To prevent the
development of malignant carcinoma, the patient attended a check-up
every three months. To date, no recurrence or deterioration has
been reported in the 15 months following the surgery.
Discussion
The diagnosis of splenic HE remains challenging as
no specific clinical manifestations are evident in the early stages
of development (6). With the
progressive growth of the tumor, the patient may experience left
upper abdominal pain, splenic swelling and an abdominal mass. In
severe cases, a series of symptoms may be induced, including
gastric distention, nausea, vomiting, dyspnea, shoulder pain and
constipation (7–9). CT imaging is an important technique
used in the diagnosis of splenic HE, which is characterized by
early-stage radiative enhancement at the margin and by delayed
enhancement filling the center. However, the final diagnosis of
splenic HE relies on pathological examination.
To the best of our knowledge, no studies have been
published that summarize the treatment efficiency of splenic HE
cases following the initial report (9). In the current study, a literature
review of splenic HE was conducted following a search of PubMed
using the key words ‘hemangioendothelioma’ and ‘spleen’ or ‘splenic
hemangioendothelioma’. A total of six cases of splenic HE were
reported prior to February 2014 (Table
I).
 | Table IClinical features of six cases of
splenic hemangioendothelioma. |
Table I
Clinical features of six cases of
splenic hemangioendothelioma.
| Case | Gender/age,
years | Symptoms | Treatment | Follow-up | Reference |
|---|
| 1 | M/45 | Enlarged spleen and
brain metastasis | Resection of tumor
mass | Five weeks
post-onset, succumbed to the disease | 4 |
| 2 | M/3 | Well-circumscribed
mass in splenic parenchyma | Partial
splenectomy | Five years,
survived | 5 |
| 3 | M/9 | HE of liver and
spleen | Splenectomy and liver
biopsy | Two days, mortality
due to consumptive coagulopathy | 3 |
| 4 | F/36 | Kaposiform HE | Splenectomy | Six months, no
recurrence or metastasis | 6 |
| 5 | F/67 | Composite HE arising
from the spleen | Splenectomy and
chemotherapy | Not available | 7 |
| 6 | F/28 | Splenic littoral cell
HE, hepatic metastasis | Splenectomy | Not available | 8 |
The therapeutic strategies for splenic HE have been
limited as cases are rare. In adults, the most effective therapy is
considered to be complete splenectomy (7–11).
However, this incurs increased postoperative risks, including the
possibility of post-splenectomy infection, which may occur if an
infant underwent a full splenectomy. Furthermore, as the immune
system of infants is not fully developed, as it is in adults, a
complete splenectomy may exert negative effects on the immune
system. In the current report, the tumor mass was distanced from
the splenic hilum, and no adhesion to the surrounding tissues was
observed, therefore, a partial splenectomy was performed.
To our best knowledge, only one case of pediatric
splenic HE had been reported prior to the current case report
(4). The patient, a 9-year-old male
with HE of the liver and spleen, received a partial splenectomy,
however, he succumbed to consumptive coagulopathy. The current case
report presents the case of a 9-year-old female patient with
splenic HE, who underwent a partial splenectomy. The patient showed
no recurrence or complications during the 15-month follow up. This
report, together with the literature review of previous cases,
provides clinical guideline for clinicians with regard to the
management of splenic HE. The limitation of this case report is
that the exact type of HE was not determined. However, the effect
of this on the treatment and prognosis of the patient is
minimal.
References
|
1
|
Nayler SJ, Rubin BP, Calonje E, et al:
Composite hemangioendothelioma: a complex, low-grade vascular
lesion mimicking angiosarcoma. Am J Surg Pathol. 24:352–361. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mentzel T, Beham A, Calonje E, et al:
Epithelioid hemangioendothelioma of skin and soft tissues:
clinicopathologic and immunohistochemical study of 30 cases. Am J
Surg Pathol. 21:363–374. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Requena L and Kutzner H:
Hemangioendothelioma. Semin Diagn Pathol. 30:29–44. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Goyal A, Babu SN, Kim V, et al:
Hemangioendothelioma of liver and spleen: trauma-induced
consumptive coagulopathy. J Pediatr Surg. 37:E292002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Leblond RF, Brown DD and DeGowin RL: The
abdomen, perineum, anus and rectosigmoid. DeGowin’s Diagnostic
Examination. 9th edition. McGraw-Hill Medical; New York, NY: pp.
3572008
|
|
6
|
Tjandra JJ, Clunie GJ, Kaye AH and SMith
J: Benign and malignant diseases of the hepatobiliary system.
Textbook of Surgery. 3rd edition. Wiley-Blackwell; Oxford: pp.
1192006
|
|
7
|
Suster S: Epithelioid and spindle-cell
hemangioendothelioma of the spleen. Report of a distinctive splenic
vascular neoplasm of childhood. Am J Surg Pathol. 16:785–792. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yoda Y and Ohashi M: A case of composite
hemangioendothelioma arising from the spleen. Jpn J Clin Oncol.
42:7702012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nurick S and Mair WG: Brain metastases
from haemangioendothelioma of the spleen. Report of a case. Acta
Neuropathol. 14:345–349. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yu L and Yang SJ: Kaposiform
hemangioendothelioma of the spleen in an adult: an initial case
report. Pathol Oncol Res. 17:969–972. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
He P, Yan XD, Wang JR, et al: Splenic
littoral cell hemangioendothelioma: Report of a case with hepatic
metastases and review of the literature. J Clin Ultrasound.
42:308–312. 2014. View Article : Google Scholar : PubMed/NCBI
|