Introduction
Giant cell tumors of the bone (GCTB) are
intramedullary bone tumors with benign and locally aggressive
pathological and clinical characteristics (1,2). GCTBs
account for 5% of primary skeletal tumors and 21% of benign bone
tumors (3,4). Although categorized as a benign bone
tumor, GCTBs have been reported to have recurrence rates of 8–62%
(5,6) and metastatic rates of 1.5–7% (7,8). GCTBs
may have a higher prevalence in females than males, as certain
studies have reported a female-to-male ratio of 1.3–1.5:1.0
(9,10). The usual primary sites for GCTBs
include the distal femur, proximal tibia and distal radius
(11,12). Diagnostically, X-ray and computed
tomography (CT) scans may show eccentric lytic lesions with
cortical extension. Pain, swelling and occasional pathological
fractures are the usual manifestations of GCTB (13). There have been few studies on the
primary lesions of GCTs of the spine, sacrum and small bones
(14), and even fewer reporting the
metastasis of these lesions to the lung. The present case study
reports two cases of thoracic and sacral spinal GCTB lesions with
pulmonary metastasis. Written informed consent was obtained from
the patients.
Case report
Case one
A 45-year-old male presented to a local hospital
with pain in the left buttock that had persisted for 2 years. The
pain was particularly bad when the patient was tired, however, the
patient did not initially seek medical attention, as the pain was
bearable. As the pain gradually worsened over the two-year period,
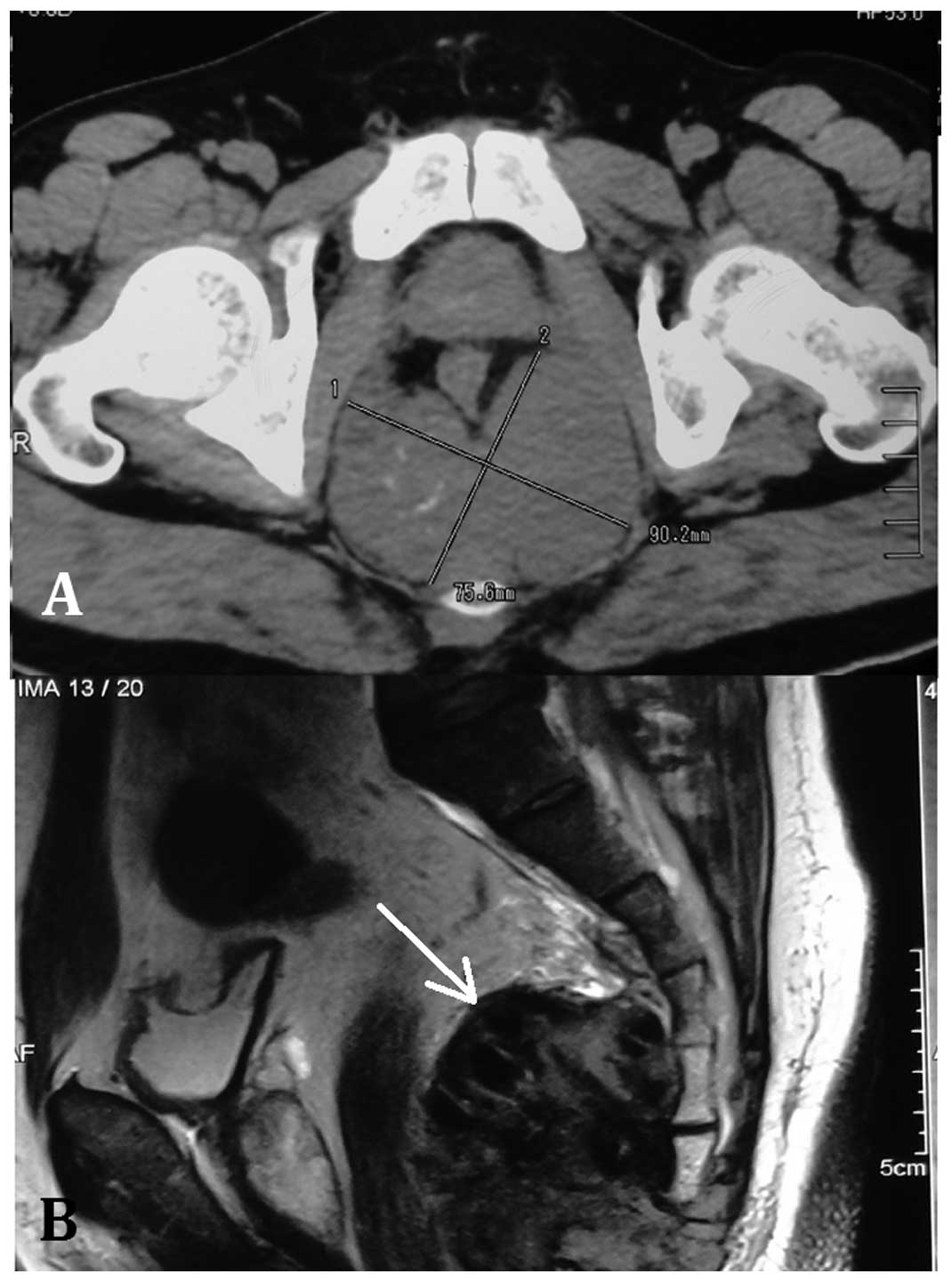
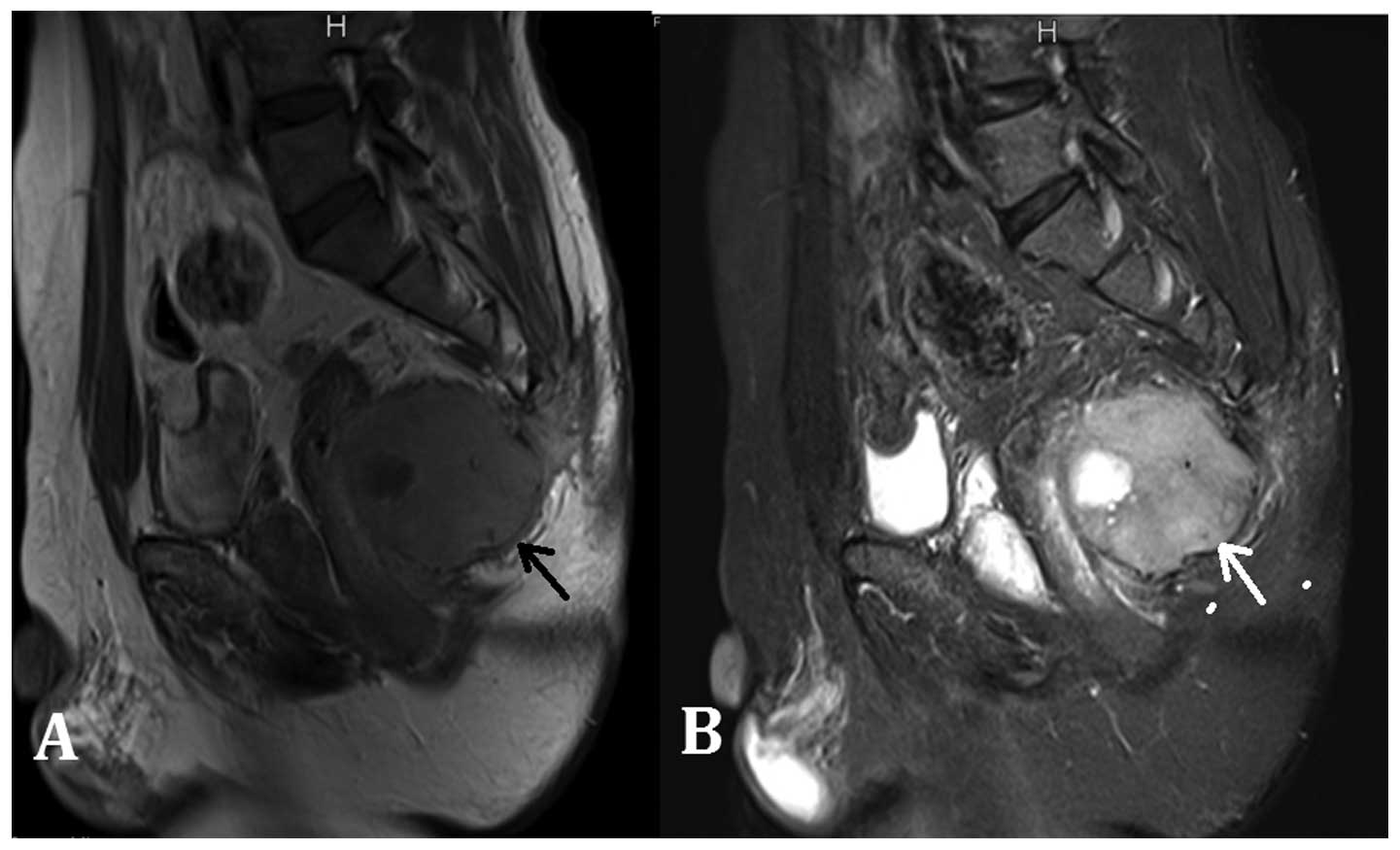
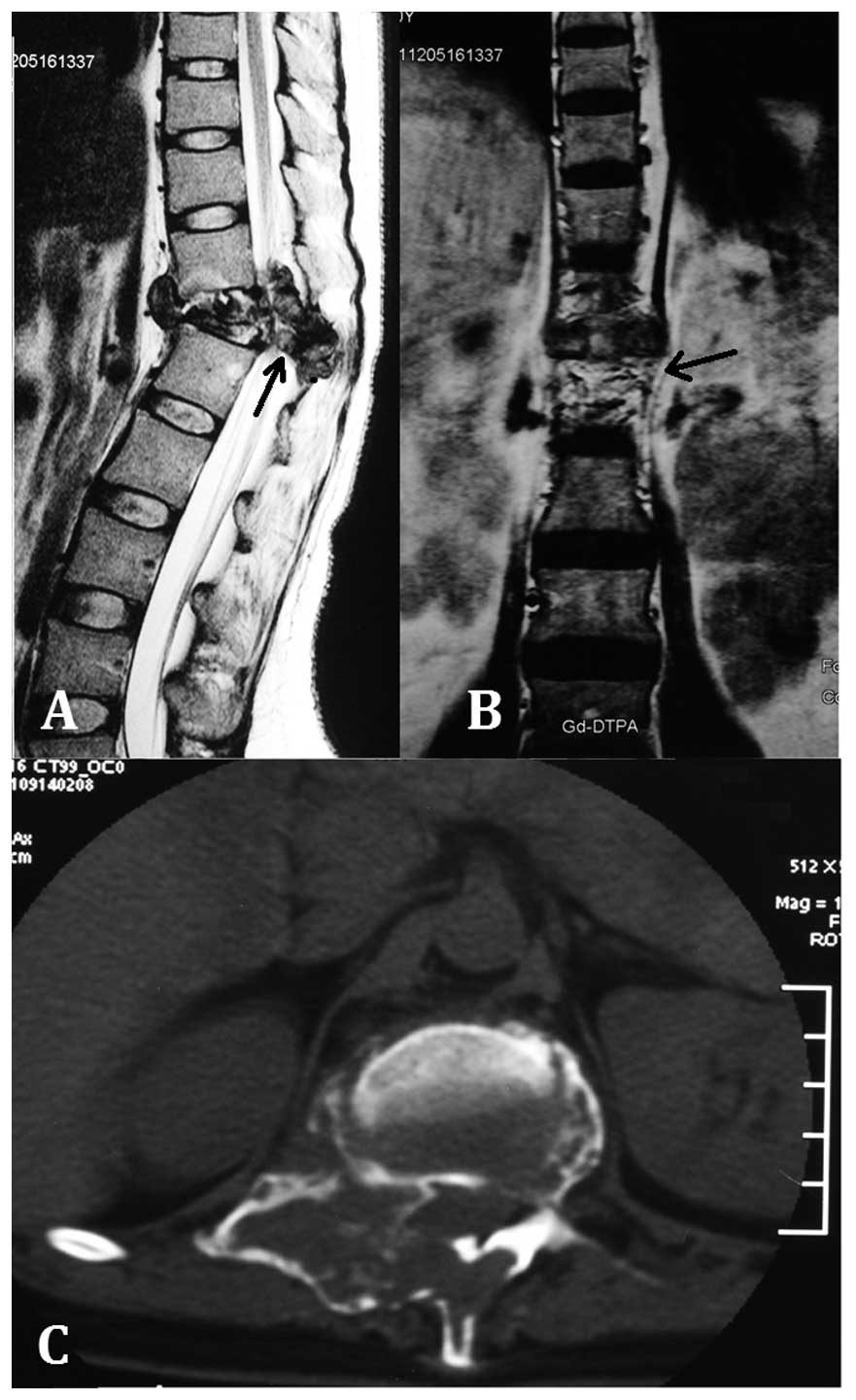
the patient finally attended a clinic at a local hospital. Magnetic
resonance imaging showed an irregularly-shaped mass, 7.5×9.1×9.3 cm
in size (Fig. 1). Surgeons in the
hospital carried out resection of the tumor and sacrum at the level
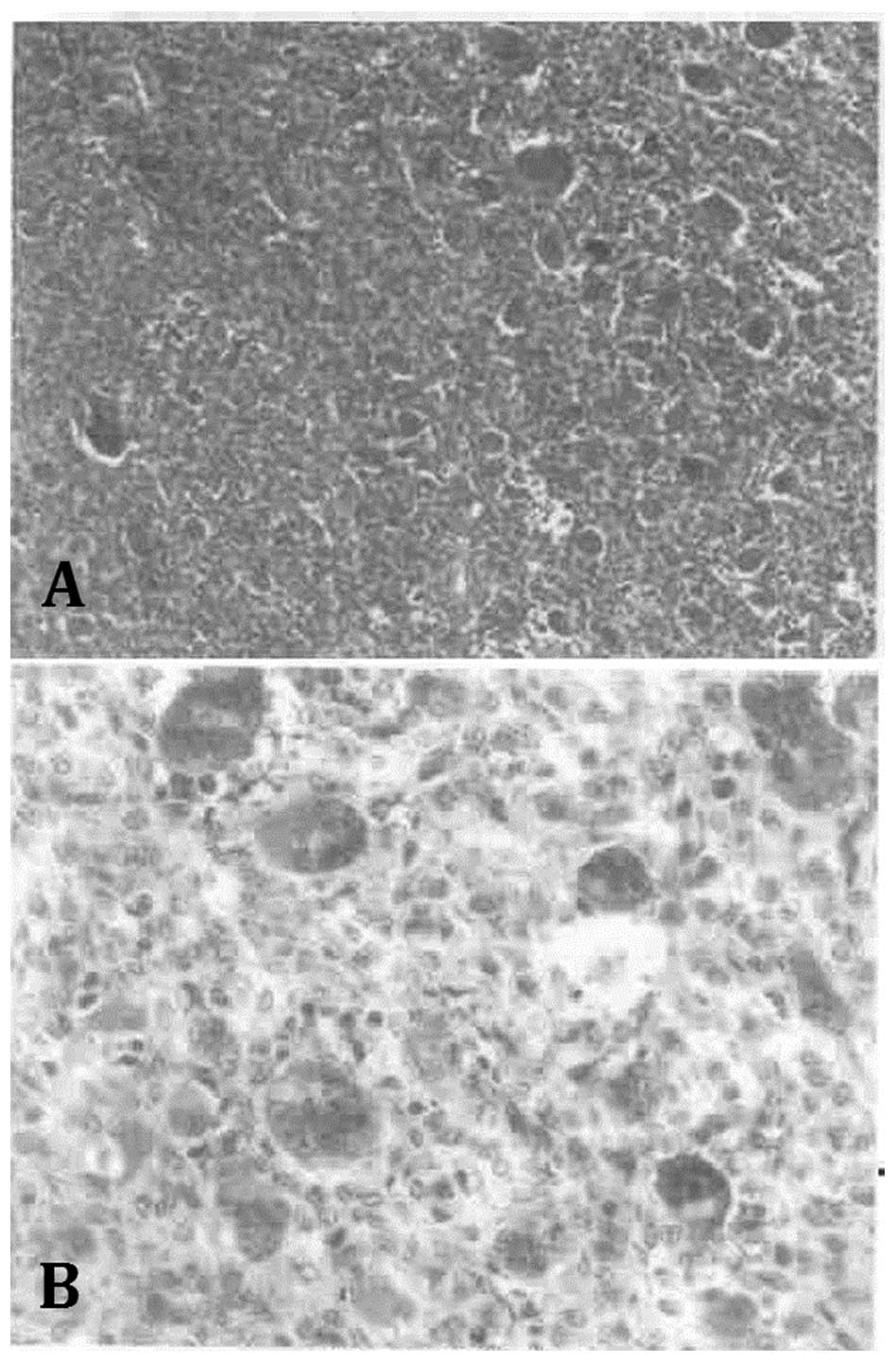
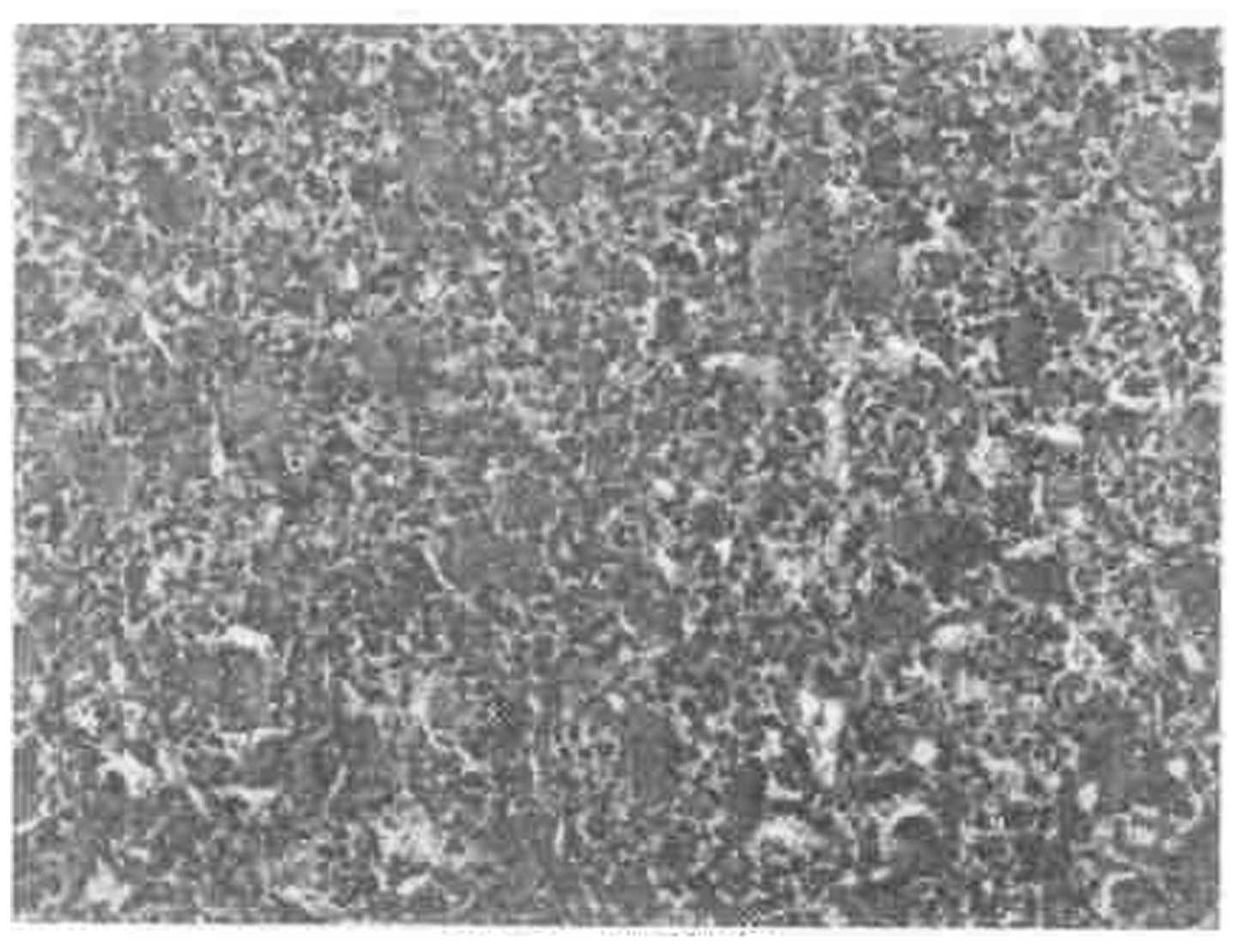
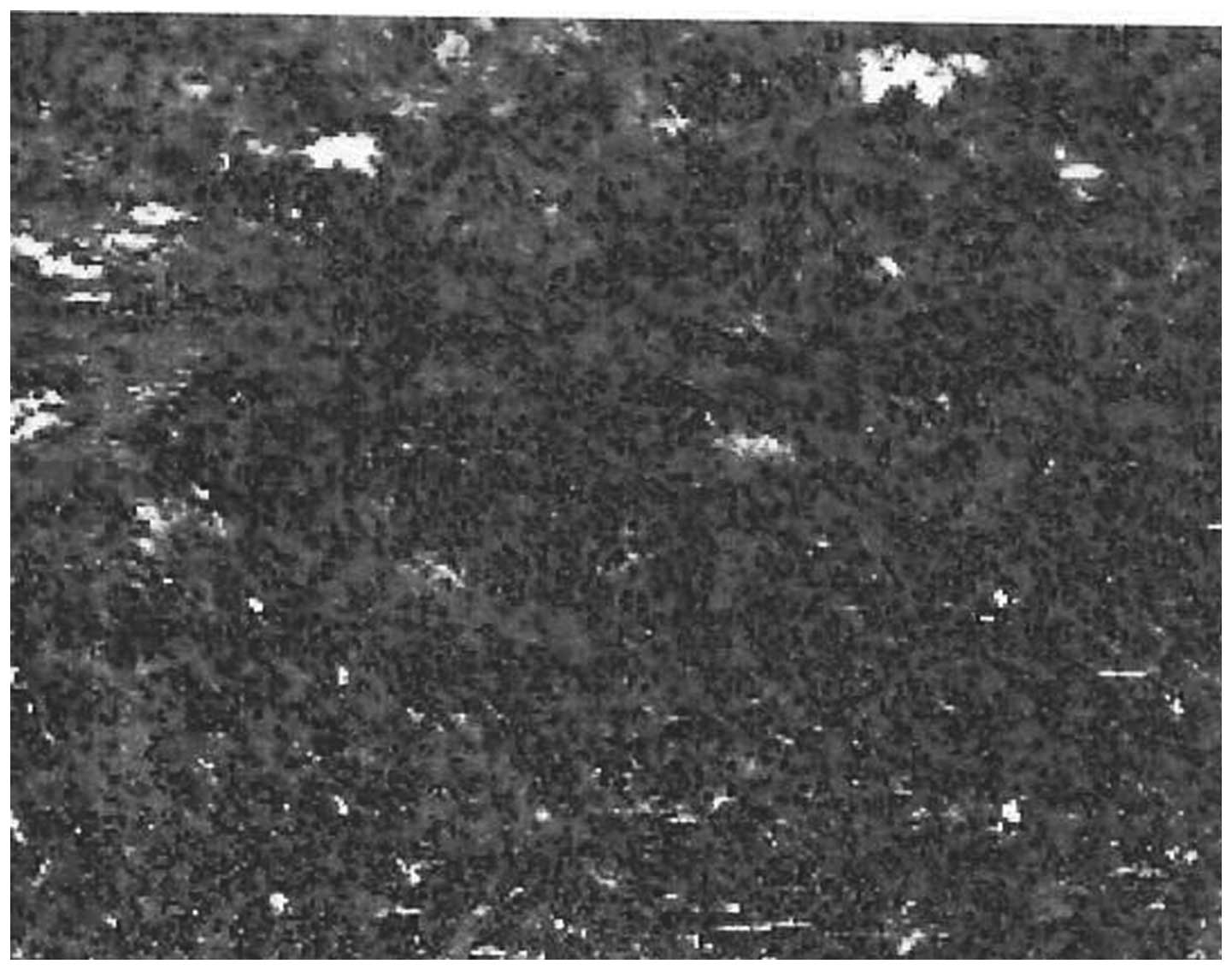
of the 4th sacral vertebra. Immunohistochemical staining for the
pre-operative fine-needle biopsy and the post-operative resection
showed the lesion to be AE1/AE3(−), cluster of differentiation
68(+), p53(+) and S-100(+), with a Ki-67 of 20%. The
histopathological examinations of the lesion established the
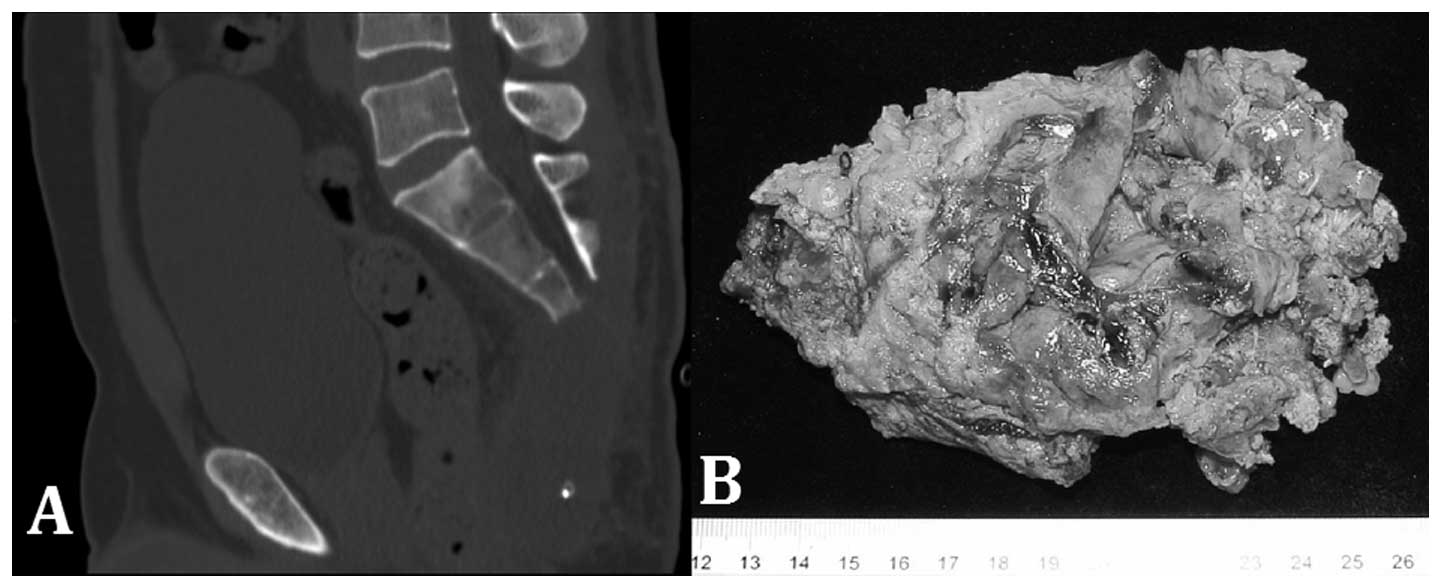
diagnosis of a GCTB (Fig. 2).
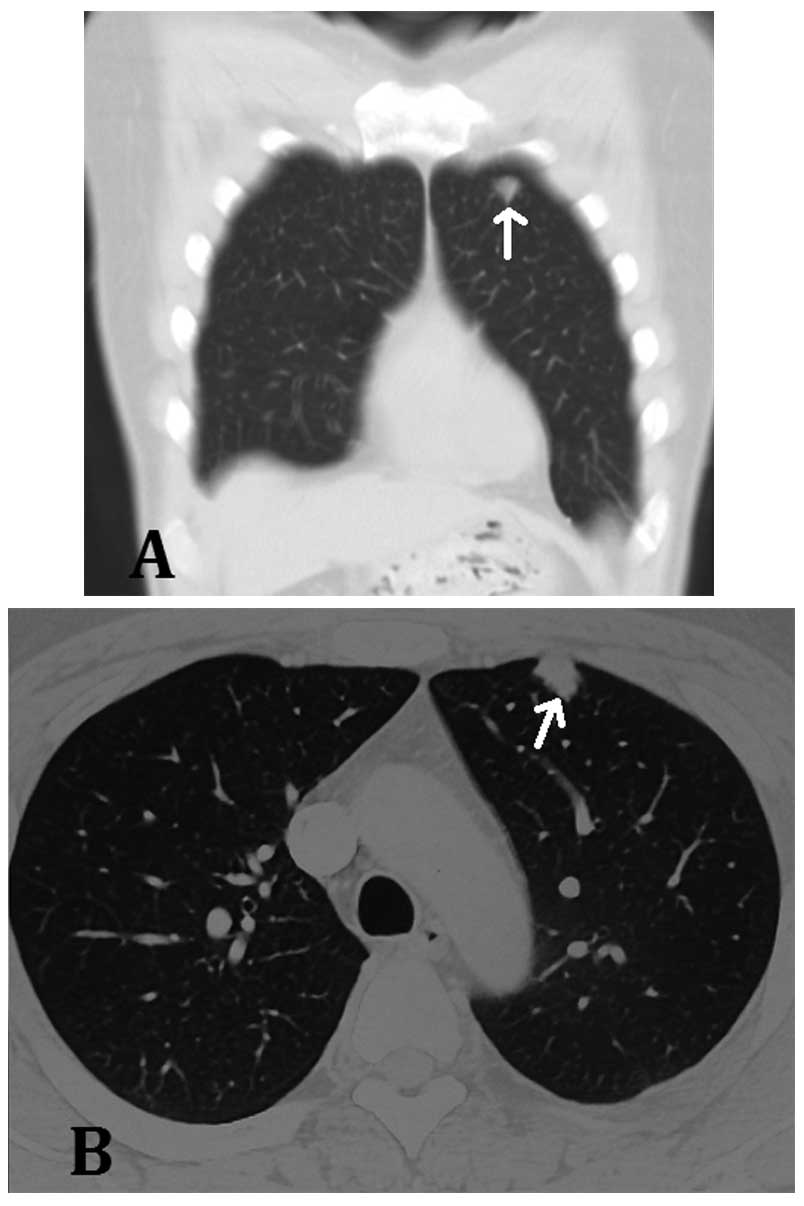
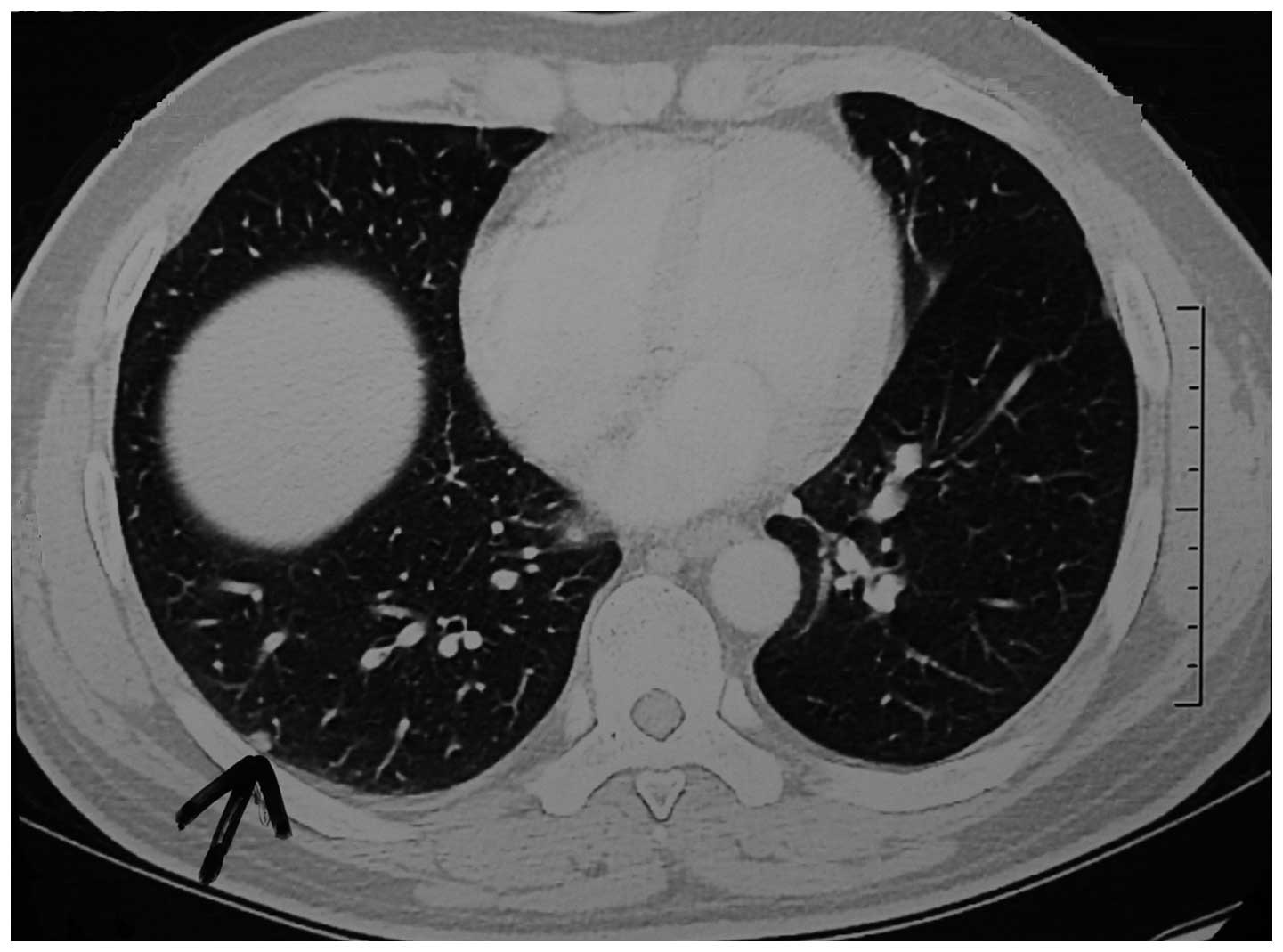
At the follow-up examination four months after the
first surgery, a chest CT scan revealed a nodule with clear borders
in the anterior upper left lobe of the lung (Fig. 3). Subsequent to a fine-needle
biopsy, the 7.5×2.5×2.5-cm pulmonary lobe, which contained the
2.0×1.0×0.6-cm mass, was resected. The fine-needle and incisional
biopsies each supported the diagnosis of a GCTB that had
metastasized to the lung (Fig.
4).
Nine months after the first surgery, a follow-up
magnetic resonance imaging (MRI) scan showed a recurrent mass at
the site of the original GCTB lesion (Fig. 5). The patient was transferred to the
Department of Orthopedic Oncology Surgery, Beijing Ji Shui Tan
Hospital (Beijing, China) and a surgical resection of the lesion
was performed and the sacral body was excised at the level of the
3rd sacral vertebra (Fig. 6).
Histopathological analysis after the surgery confirmed that it was
a recurrent lesion from the original GCTB (Fig. 7).
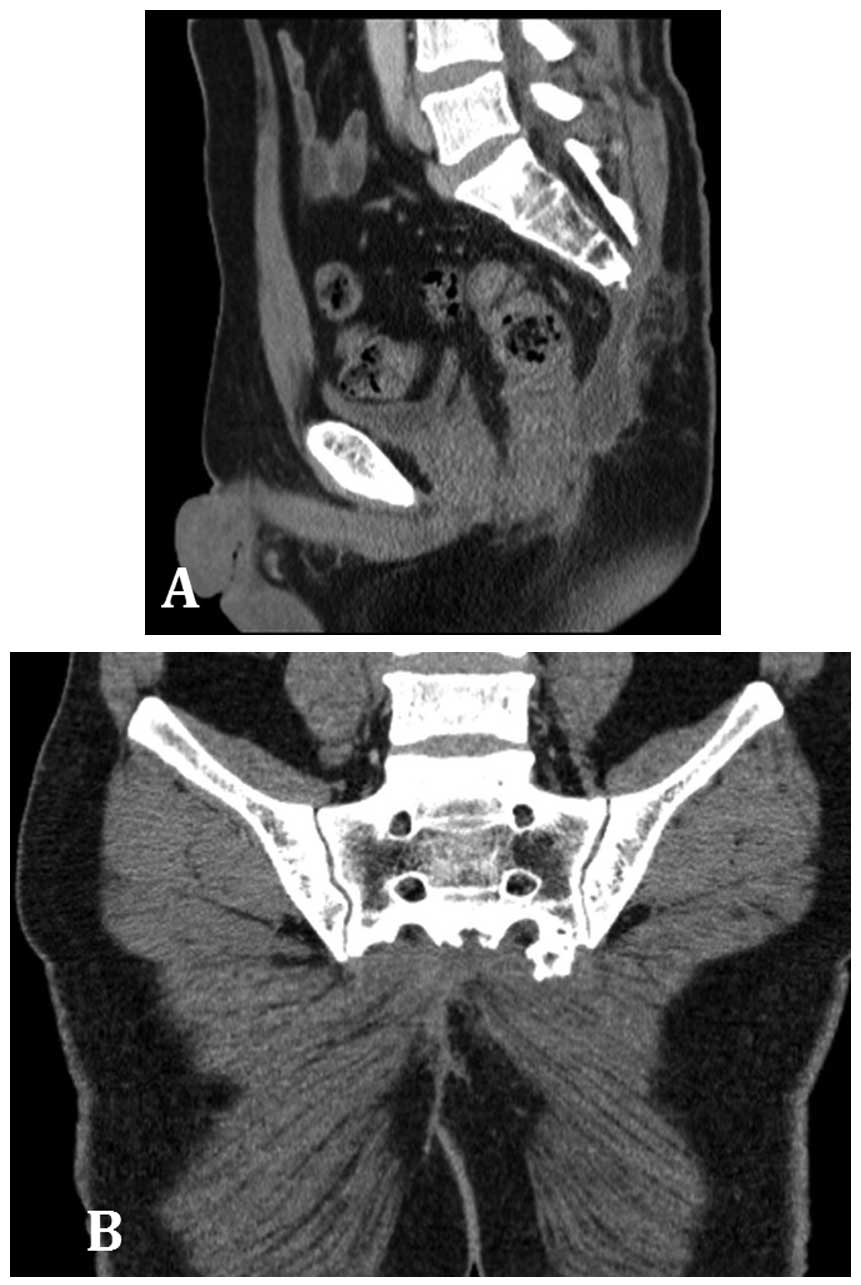
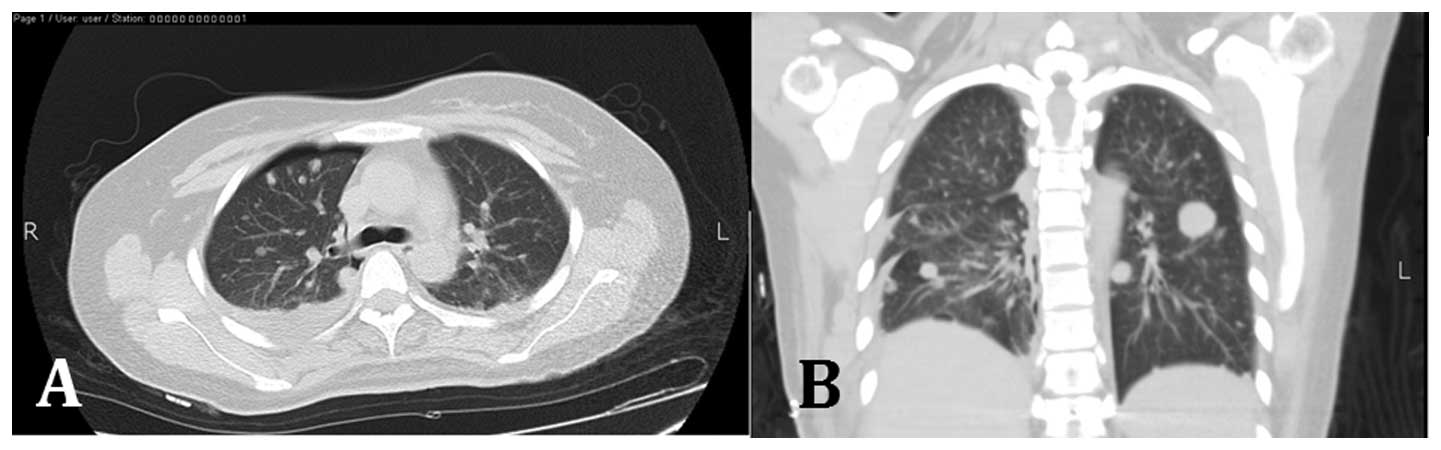
A chest CT scan performed at a follow-up examination
21 months after the first surgery, showed numerous metastatic
nodules in diffuse and random distributions in each lung (Fig. 8). The patient refused to undergo any
further surgical treatment or chemotherapy. The last follow-up took
place 33 months after the first surgery, during which a CT scan
found no local recurrence, and the patient complained of no pain at
the site of the original lesion (Fig.
9). A chest CT scan showed several newly developed nodules, the
largest being 7 mm in diameter (Fig.
10). However, the patient reported no chest pain or trouble in
breathing.
Case two
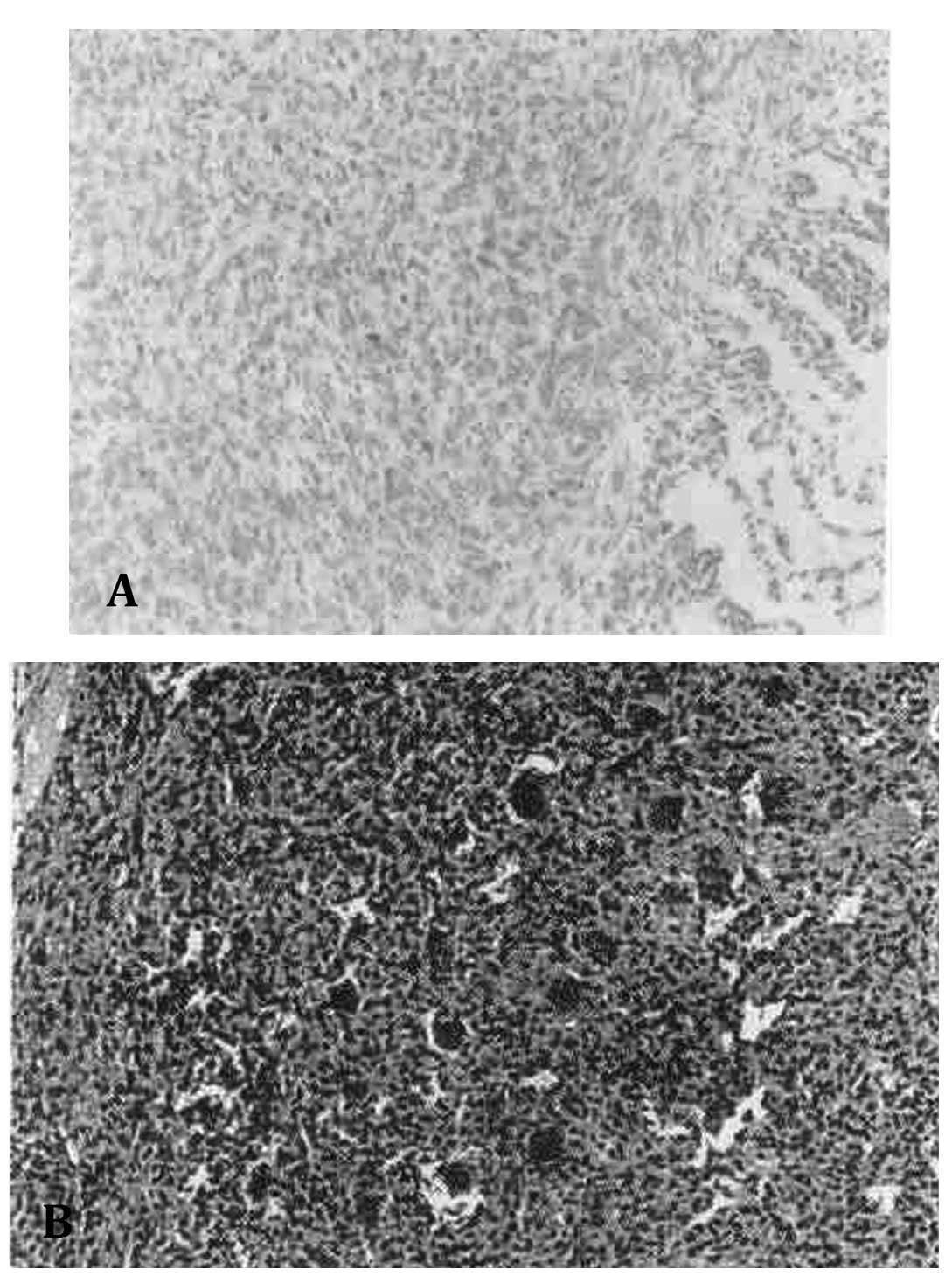
A 30-year-old female presented to a local hospital
due to back pain that had persisted for one year. MRI revealed a
3.2×3.8×3.3-cm lesion in the twelfth thoracic vertebral body, with
evident compression of the adjacent spinal canal and foramen. A
3.0×3.4×5.6-cm mass was also present in the spinal canal and
posterior column of the T12 vertebra (Fig. 11). A fine-needle biopsy was
performed and the tumor was diagnosed as a GCTB (Fig. 12).
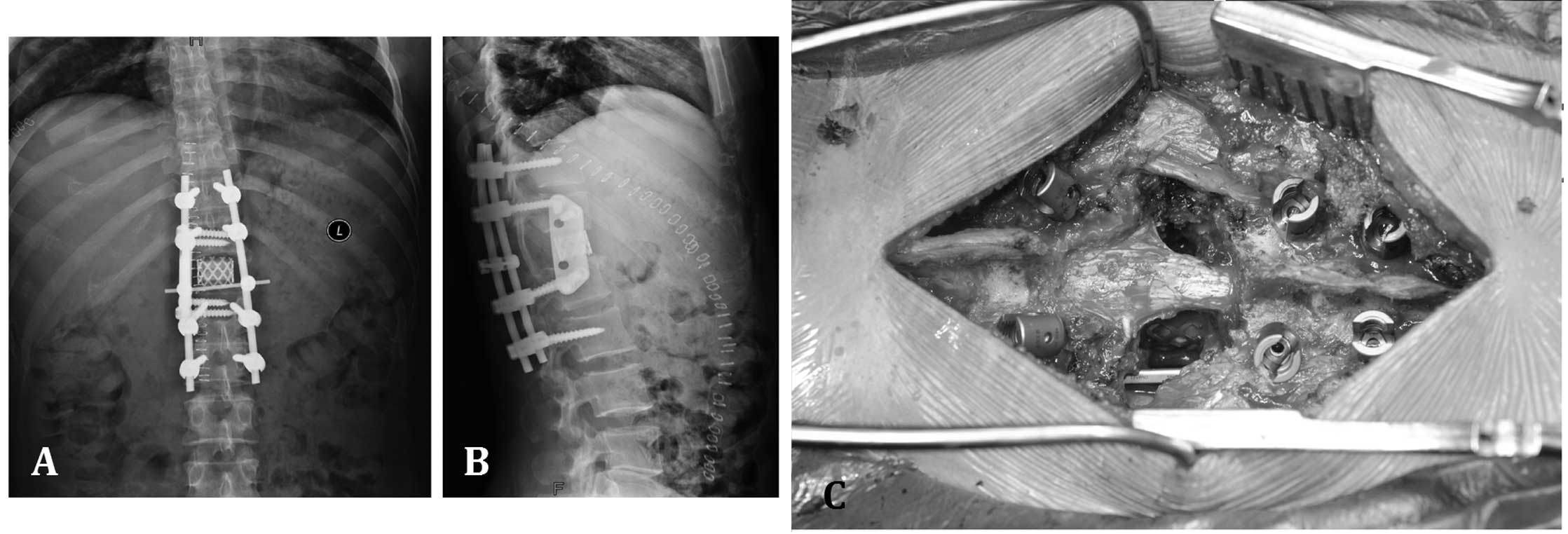
The patient was transferred to the Department of
Orthopedic Oncology Surgery, Beijing Ji Shui Tan Hospital and
computer-guided surgery was subsequently performed to resect the
primary tumor (Fig. 13). The spine
was stabilized by vertical and horizontal rods fixed by eight
pedicle screws fixed into the 10th and 11th thoracic vertebrae, and
the 1st and 2nd lumbar vertebrae. The vertebral body of the 12th
thoracic vertebra was removed and replaced by a mesh cage filled
with bone cement. A titanium palate with four screws was fixed
laterally on the 11th thoracic and 1st lumbar vertebrae to provide
reinforcement (Fig. 14). Due to
the possibility of pulmonary metastasis, a chest CT scan was
ordered, which showed multiple nodules of varying sizes in each
lung (Fig. 15). Subsequent to a
recovery period, the patient was advised to seek further surgical
resection in a more specialized hospital or receive resection of
the pulmonary metastasis. The patient was subsequently lost to
follow-up.
Discussion
Giant cell tumors of the bone within the vertebrae
are rare, accounting for just 2.7–6.5% of all GCTB (15). According to the literature, the
sacrum may be the most common site for this lesion, followed by the
thoracic, cervical and lumbar segments (16). Patients with vertebral GCTB usually
demonstrate clinical manifestations such as pain with radicular
distribution, weakness and sensory deficits. A variety of imaging
modalities, including magnetic resonance imaging, CT scans,
radionuclide imaging and positron emission tomography, are useful
tools for the diagnosis for the diagnosis of GCT of the spine.
Fine-needle aspiration biopsy can be used to aid the differential
diagnosis and confirm the final diagnosis.
The ideal treatment for GCTB consists of an en-bloc
excision at the early stages of the development of the lesion
(17). However, due to the
complicated anatomical structure of the spine and adjuvant spinal
tissues, the surgical treatment of tumors of the spine is extremely
challenging. In case one of the present study, the local hospital
that the patient attended did not have much experience with rare
sacral GCTB, and therefore failed to obtain an en-bloc resection.
This was probably the most significant cause of the recurrent
lesion and lung metastases not long after the first surgical
treatment. In our center, the majority of patients are treated by
senior surgeons who perform GCTB resection with the assistance of
computer navigation, which predominantly achieves en-bloc resection
of the tumor. In case one, following the resection of the recurrent
lesion in our center, there was no further recurrence at the
original site of the tumor and the metastatic lesions in the lungs
were relatively stable with no symptoms. In case two, although the
patient was lost to follow-up after the first surgery, it is not
likely that there will be further recurrence or metastasis.
Although radiotherapy is recommended in cases of
unresectable GCTB (18), it is not
suitable for vertebral lesions, as it may cause spinal cord
myelitis and malignant transformation of the tumor (19,20).
Chemotherapy is also not highly recommended for the treatment of
GCTB due to its toxic effects and the normally benign nature of
GCTB (21). Thus, there is no
standard chemical therapy protocol for the lesion. However,
denosumab, a novel drug that inhibits the function of the cytokine
receptor activator of nuclear factor-κB ligand (RANKL) may be an
effective alternative based on the fact that GCTs overexpress RANKL
and its receptor (22). Although
the two patients in the present study refused to receive
chemotherapy, certain other patients with GCTB that metastasized to
the lung received a chemotherapy regime consisting of Adriamycin,
ifosfamide and mitoxantrone, resulting in more growth of the
metastatic tumor in the lung compared with the tumors of those who
did not receive chemotherapy (23).
However, randomized controlled trials should be carried out to
evaluate the pros and cons of chemotherapy for GCTB with pulmonary
metastasis.
Acknowledgements
The present study was funded by the National Natural
Science Foundation Project of China (grant no. 61372179).
References
|
1
|
Gong L, Liu W, Sun X, et al: Histological
and clinical characteristics of malignant giant cell tumor of bone.
Virchows Arch. 460:327–334. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Enneking WF: Musculoskeletal Tumor
Surgery. Churchill Livingstone, Inc; New York (NY): 1983
|
|
3
|
Kivioja AH, Blomqvist C, Hietaniemi K, et
al: Cement is recommended in intralesional surgery of giant cell
tumors: a Scandinavian Sarcoma Group study of 294 patients followed
for a median time of 5 years. Acta Orthop. 79:86–93. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lackman RD, Hosalkar HS, Ogilvie CM, et
al: Intralesional curettage for grades II and III giant cell tumors
of bone. Clin Orthop Relat Res. 438:123–127. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Balke M, Schremper L, Gebert C, et al:
Giant cell tumor of bone: treatment and outcome of 214 cases. J
Cancer Res Clin Oncol. 134:969–978. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Arbeitsgemeinschaft Knochentumoren. Becker
WT, Dohle J, Bernd L, Braun A, et al: Local recurrence of giant
cell tumor of bone after intralesional treatment with and without
adjuvant therapy. J Bone Joint Surg Am. 90:1060–1067. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Prosser GH, Baloch KG, Tillman RM, Carter
SR and Grimer RJ: Does curettage without adjuvant therapy provide
low recurrence rates in giant-cell tumors of bone? Clin Orthop
Relat Res. 211–218. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vult von Steyern F, Bauer HC, Trovik C, et
al: Scandinavian Sarcoma Group: Treatment of local recurrences of
giant cell tumour in long bones after curettage and cementing. A
Scandinavian Sarcoma Group study. J Bone Joint Surg Br. 88:531–535.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Harness NG and Mankin HJ: Giant-cell tumor
of the distal forearm. J Hand Surg Am. 29:188–193. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Moon JC, Kim SR, Chung MJ and Lee YC:
Multiple pulmonary metastases from giant cell tumor of a hand. Am J
Med Sci. 343:171–173. 2012. View Article : Google Scholar
|
|
11
|
Osaka S, Sugita H, Osaka E, et al:
Clinical and immunohistochemical characteristics of benign giant
cell tumour of bone with pulmonary metastases: case series. J
Orthop Surg (Hong Kong). 12:55–62. 2004.
|
|
12
|
Xiuchun Yu, Ming Xu, Songfeng Xu and Qing
Su: Clinical outcomes of giant cell tumor of bone treated with bone
cement filling and internal fixation, and oral bisphosphonates.
Oncol Lett. 5:447–451. 2013.
|
|
13
|
Ropars M, Kaila R, Cannon SR and Briggs
TW: Primary giant cell tumours of the digital bones of the hand. J
Hand Surg Eur Vol. 32:160–164. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Averill RM, Smith RJ and Campbell CJ:
Giant-cell tumors of the bones of the hand. J Hand Surg Am.
5:39–50. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shimada Y, Hongo M, Miyakoshi N, et al:
Giant cell tumor of fifth lumbar vertebrae: two case reports and
review of the literature. Spine J. 7:499–505. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bidwell JK, Young JW and Khalluff E: Giant
cell tumor of the spine: computed tomography appearance and review
of the literature. J Comput Tomogr. 11:307–311. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Niu X, Zhang Q, Hao L, et al: Giant cell
tumor of the extremity: retrospective analysis of 621 Chinese
patients from one institution. J Bone Joint Surg Am. 94:461–467.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bhatia S, Miszczyk L, Roelandts M, et al:
Radiotherapy for marginally resected, unresectable or recurrent
giant cell tumor of the bone: a rare cancer network study. Rare
Tumors. 3:e482011. View Article : Google Scholar
|
|
19
|
Khan DC, Malhotra S, Stevens RE, et al:
Radiotherapy for the treatment of giant cell tumor of the spine: a
report of six cases and review of the literature. Cancer Invest.
17:110–113. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen ZX, Gu DZ, Yu ZH, et al: Radiation
therapy of giant cell tumor of bone: analysis of 35 patients. Int J
Radiat Oncol Biol Phys. 12:329–334. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cheng YY, Huang L, Lee KM, et al:
Bisphosphonates induce apoptosis of stromal tumor cells in giant
cell tumor of bone. Calcif Tissue Int. 75:71–77. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thomas D, Henshaw R, Skubitz K, et al:
Denosumab in patients with giant-cell tumour of bone: an
open-label, phase 2 study. Lancet Oncol. 11:275–280. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Klenke FM, Wenger DE, Inwards CY, Rose PS
and Sim FH: Recurrent giant cell tumor of long bones: analysis of
surgical management. Clin Orthop Relat Res. 469:1181–1187. 2011.
View Article : Google Scholar :
|