Introduction
Squamous cell carcinoma (SCC) of the skin, which
develops from the keratinocytes of the epidermis, is the second
most common skin malignancy and accounts for 20% of all skin
cancers (1). The incidence of SCC
continues to increase (2) and
represents a major public health concern due to the associated
significant health costs and marked disfigurement following
surgical excision. Patients with primary SCC have a good prognosis,
however, the long-term prognosis is relatively poor for those with
metastatic disease, which has a 10-year survival rate of <20%
(2). Clinically, the diagnosis of SCC
is confirmed by skin biopsy. At present, treatment modalities
include radiotherapy, brachytherapy, electrodesiccaation,
cryotherapy and photodynamic therapy, however, surgical excision
and Mohs micrographic surgery (MMS) are considered the gold
standard treatments for high-risk SCC (3). Despite this, due to the high cost and
complicated surgical process, at present MMS is not widely used.
The omental flap, a classical reconstructive flap widely used for
the treatment of ulcers and defects of the breast, may provide a
vascularized recipient bed for skin grafts and thus, may adapt well
to an ischemic environment, such as the lower limb (4). In this study, the case of a male patient
with a large SCC in the lower part of the right leg, who underwent
extensive resection with reconstruction using an omental
transposition flap, is presented.
Case report
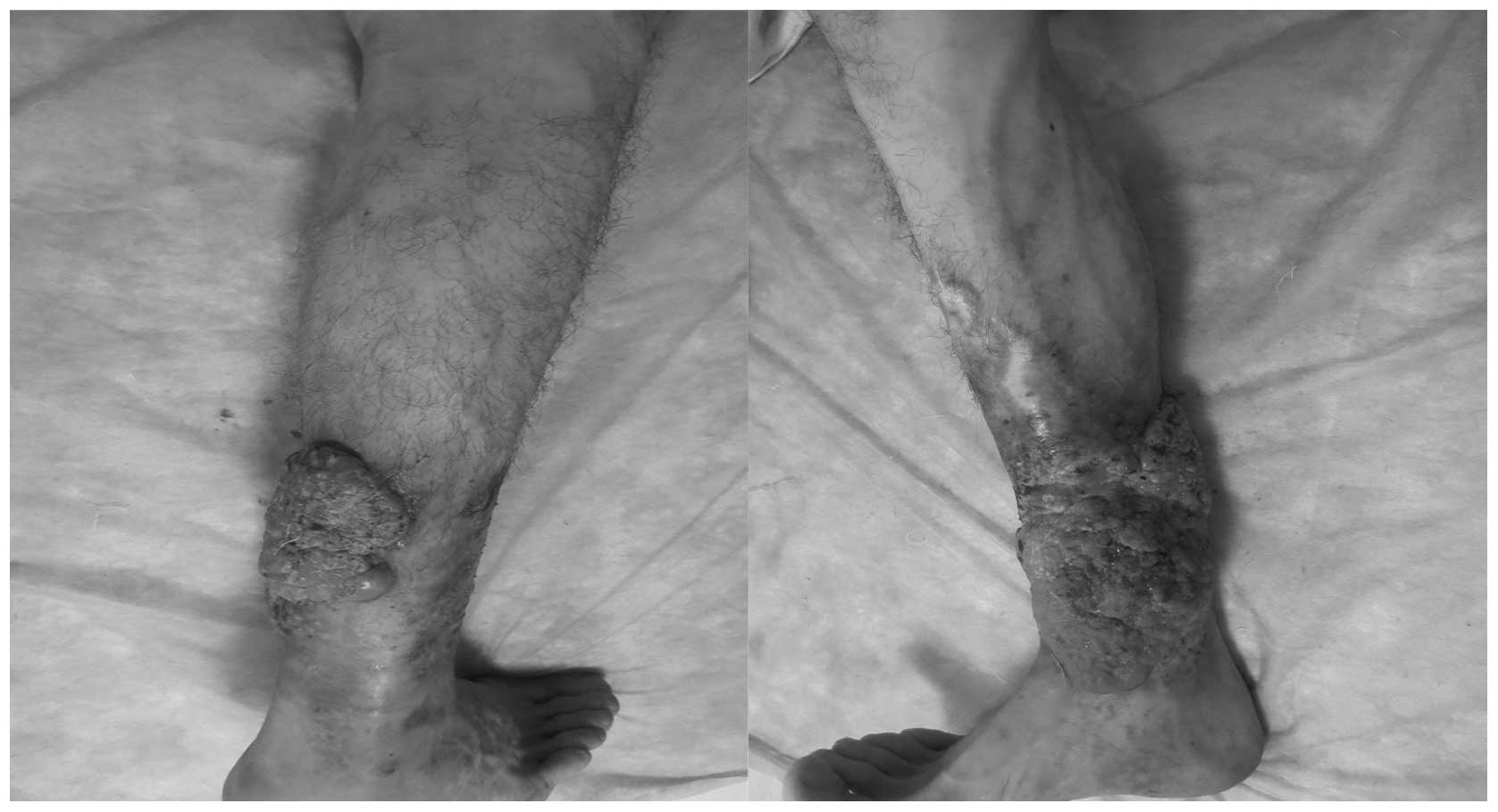
A 49-year-old male presented to Hunan Cancer
Hospital and The Affiliated Cancer Hospital of Xiangya School of
Medicine (Changsha, China) with a ulcerated skin lesion in the
lower part of the right leg, for which amputation was suggested by
doctors at other hospitals. The physical examination on admission
revealed the presence of a ∼25×20-cm2 cutaneous
cauliflower-shaped ulcerated lesion, with a specific odor and
exudate, occupying one-third of the lower part of the leg (Fig. 1), with lymphadenopathy of the
ipsilateral inguinal region. The preoperative pathological
examination established the diagnosis of highly differentiated SCC
and the bacteriological examination revealed infection by
levofloxacin-sensitive Pseudomonas aeruginosa.
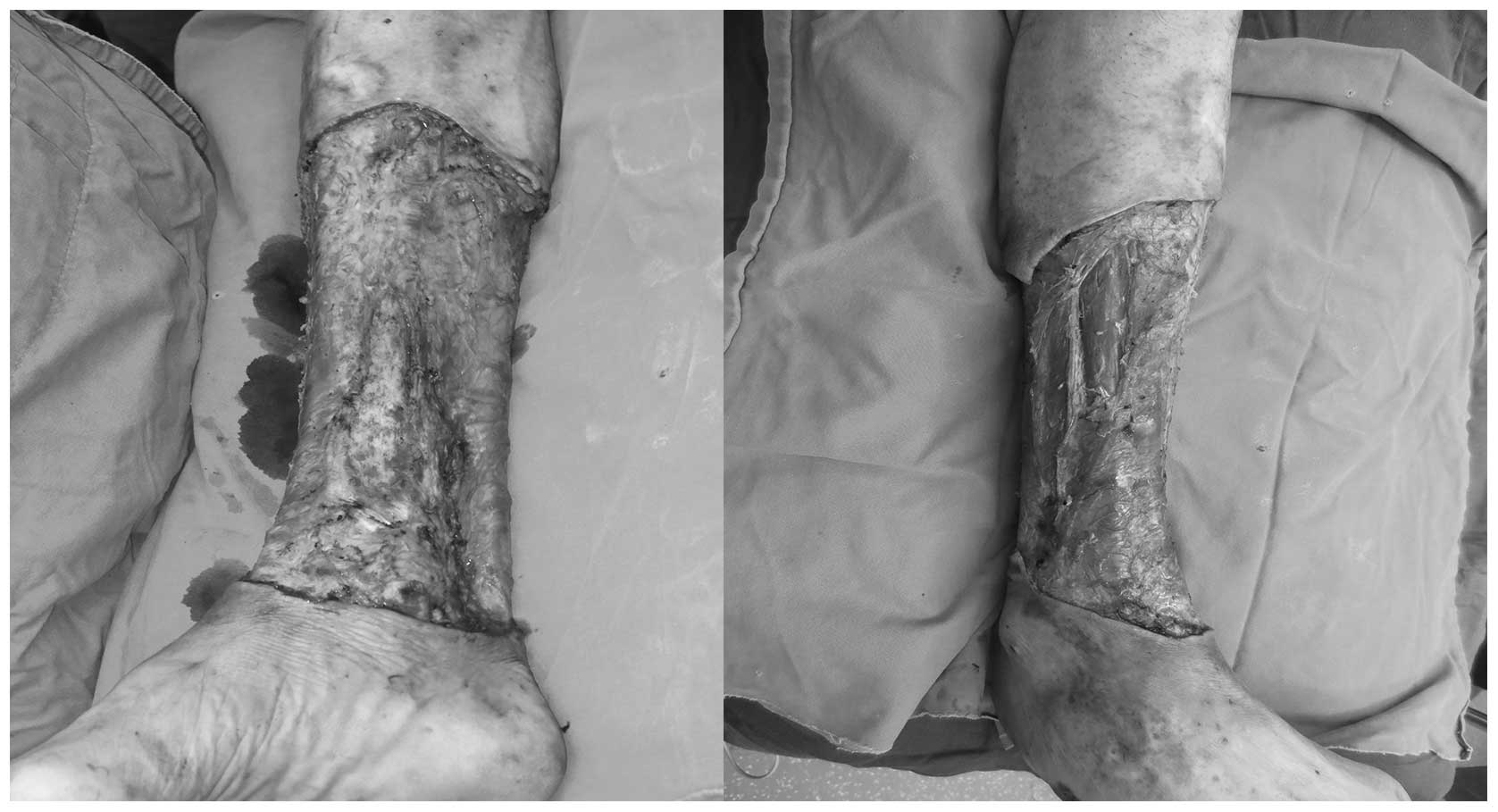
Prior to surgery, potassium permanganate was used to
soak the limb and the dressing was changed daily. The infection was
effectively controlled following administration of antibiotics with
high sensitivity. Thereafter, the patient underwent extensive
resection of the original lesion (Fig.
2), with additional biopsy of the ipsilateral inguinal lymph
nodes, which did not identify lymph node metastasis.
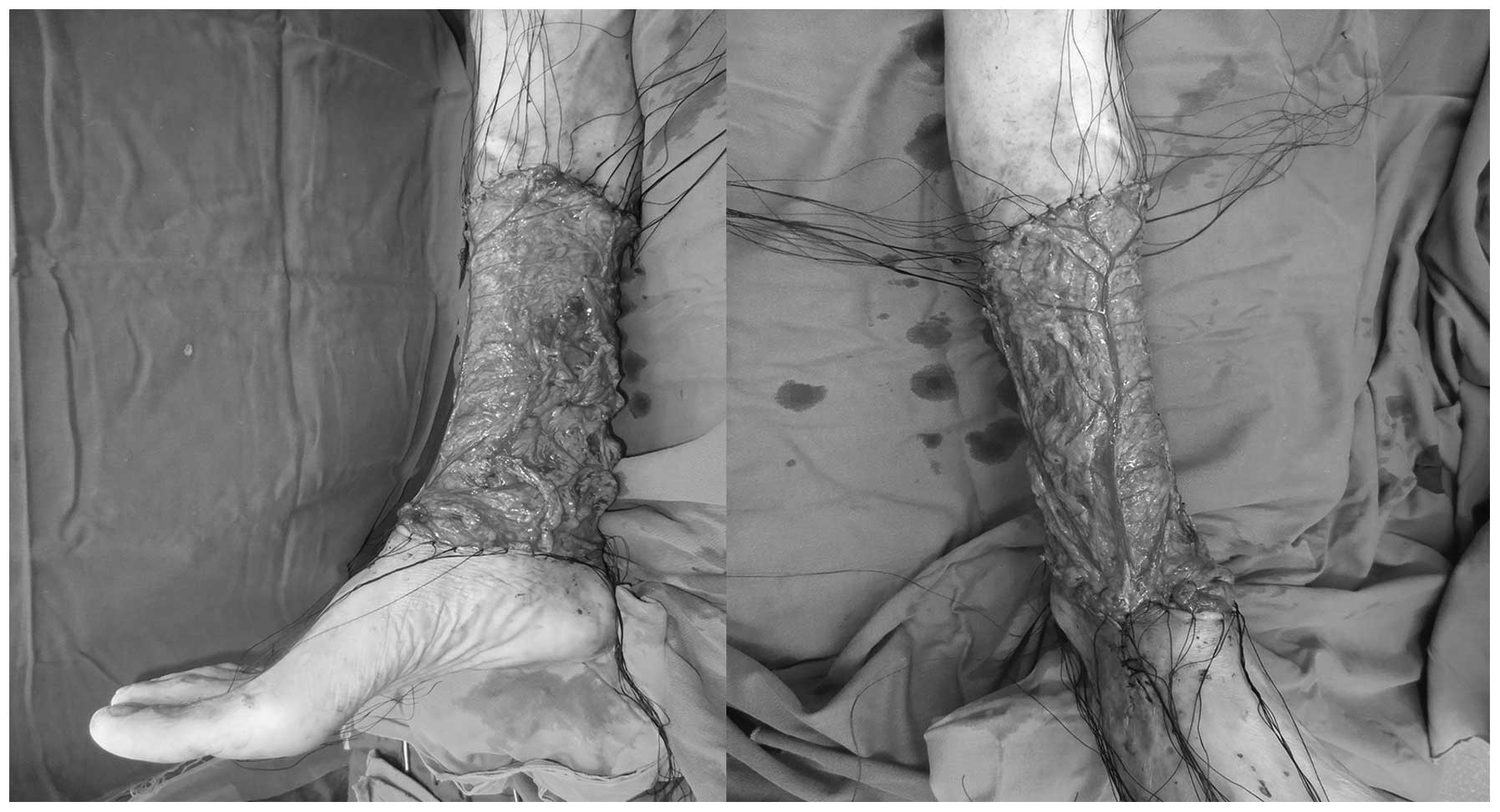
The autologous reconstructive options for the
present case were preoperatively discussed in a multidisciplinary
team setting involving general and plastic surgeons. It was decided
to repair the defect using a free omental flap with a vascular
pedicle, as this satisfied the reconstructive requirements, namely
covering the defect with healthy, well-vascularized tissue and a
reliable flap, while avoiding the long operative time and high cost
that are associated with Mohs micrographic surgery (MMS) (5).
The patient was placed in the supine position.
Following an upper midline incision, the omentum was carefully
mobilized and excised along with the right gastroepiploic pedicle,
subsequent to which it was transposed to the debrided leg defect
(Fig. 3). The dorsal artery was used
as a recipient vessel for the right gastroepiploic artery and
anastomosis was performed in an end-to-end manner. The secured
omentum was covered with a secondary skin graft that was harvested
from the thigh of the patient 10 days after the first
operation.
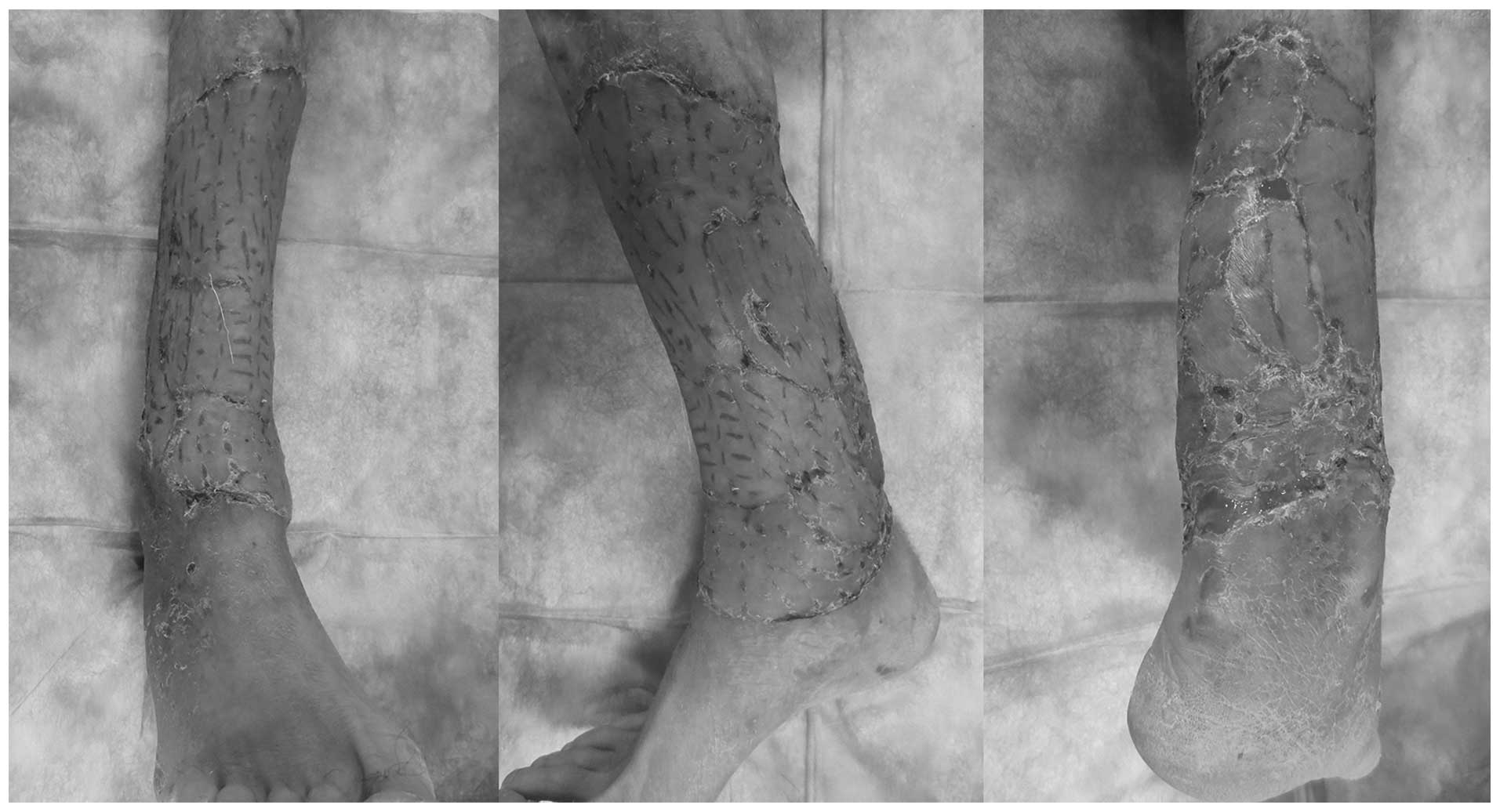
Postoperatively, the patient was prescribed a 2-day
course of cefoperazone/tazobactam. Due to persistent wound
discharge, the antibiotic therapy was continued for 5 days; by day
5, the wound discharge had significantly increased. The drainage
from the incision was collected for bacteriological examination and
the patient was administered antibiotics (ceftazidime and
levofloxacin) with high sensitivity and specificity following
secondary skin grafting. The skin graft exhibited favorable
survival (Fig. 4) and the patient was
discharged on the 15th postoperative day. No complications were
reported. At the 24-month follow-up examination, there were no
signs of disease recurrence and no reported pain or ulceration.
Written informed consent was obtained from the patient.
Discussion
The biological behavior of SCC is determined by
several variables (6) and its
treatment should be selected based on the lesion size, anatomical
location, invasion depth, degree of cellular differentiation and
history of previous treatment (7).
However, surgery with a predefined excision margin is considered
the optimal treatment option for the majority of cutaneous SCC
cases. In addition, MMS is recommended for SCCs that are associated
with a higher risk or located at anatomical sites requiring maximal
tissue conservation for the preservation of function and cosmesis
(8). However, MMS is associated with
a high cost and long operative duration and no randomized
controlled trials have yet been performed to directly compare the
two surgical procedures (3).
In the present case, considering the large area
occupied by the tumor and the fact that the lesion was located at a
region where the likelihood of postoperative skin necrosis and
infection is high, the patient was recommended to undergo
amputation at other hospitals prior to presenting to our
institution. However, amputation markedly affects the quality of
life of the patients; therefore, the patient and his family
declined this surgical approach.
The omental flap was first described by Kiricta in
1963 (9) and is a classical
reconstructive alternative for ulcers of the axilla and breast
(10). The omental flap is a highly
vascularized tissue that is resistant to infection and adapts well
to an ischemic environment (11).
Thus, the use of the greater omental flap is considered as a
back-up option in complicated cases. At present, the free omental
flap is commonly used for improving subcutaneous contour and wound
coverage, as it provides a vascularized recipient bed for skin
grafts.
Considering the absence of lymph node metastasis and
the wish of the patient to avoid amputation, the tumor was resected
and the defect reconstructed using the free omental transposition
flap with secondary skin grafting to achieve satisfactory defect
coverage with an adequate volume of well-vascularized tissue. The
immunological and angiogenic properties of omental flaps are
particularly useful for promoting the healing of defects. As
opposed to free fat grafts, which quickly lose volume following
transplantation, the vascularized omental flap maintains its
volume.
In the present case, the patient did not experience
any complications other than early recipient site infection, which
was successfully treated with antibiotics. The treatment of SCC
aims to completely remove or destroy the tumor and to minimize
functional and cosmetic impairment. Thus, limb-salvage surgery with
omental transplantation is a potential alternative for such
patients in developing countries, where the patients may require a
more cost-effective precedure and physicians may lack the special
training required for MMS. Furthermore, Chren et al
(12) reported that regional
recurrence was similar between the two treatment modalities.
The application of omental transplantation in the
present case achieved a satisfactory limb contour and also yielded
cosmetic and functional outcomes that completely met the
requirements of the patient. No local recurrence or metastasis has
been reported in the present case; however, further prospective
studies are required to determine the specific indications for this
technique. In conclusion, omental transplantation may be a viable
option for limb-salvage surgery and the reconstruction of defects
following resection of large SCCs in regions susceptible to
ischemia.
References
|
1
|
McGuire JF, Ge NN and Dyson S: Nonmelanoma
skin cancer of the head and neck I: histopathology and clinical
behavior. Am J Otolaryngol. 30:121–133. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Alam M and Ratner D: Cutaneous
squamous-cell carcinoma. N Engl J Med. 344:975–983. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lansbury L, Bath-Hextall F, Perkins W,
Stanton W and Leonardi-Bee J: Interventions for non-metastatic
squamous cell carcinoma of the skin: systematic review and pooled
analysis of observational studies. BMJ. 347:f61532013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hartmann CE, Ko LW, Ion L and Jemec B: A
difficult case: omental transposition flap reconstruction of a
large radionecrotic axillary ulcer in a patient with extensive
previous abdominal surgery. J Plast Reconstr Aesthet Surg.
66:e66–e68. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Belkin D and Carucci JA: Mohs surgery for
squamous cell carcinoma. Dermatologic clinics. 29:161–174. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Barksdale SK, O'Connor N and Barnhill R:
Prognostic factors for cutaneous squamous cell and basal cell
carcinoma. Determinants of risk of recurrence, metastasis and
development of subsequent skin cancers. Surg Oncol Clin N Am.
6:625–638. 1997.PubMed/NCBI
|
|
7
|
Goldman GD: Squamous cell cancer: a
practical approach. Semin Cutan Med Surg. 17:80–95. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stasko T, Brown MD, Carucci JA, et al:
International Transplant-Skin Cancer Collaborative; European Skin
Care in Organ Transplant Patients Network: Guidelines for the
management of squamous cell carcinoma in organ transplant
recipients. Dermatol Surg. 30:642–650. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kiricuta I: The use of the great omentum
in the surgery of breast cancer. Presse Med. 71:15–17. 1963.[(In
French)]. PubMed/NCBI
|
|
10
|
Katz MH: Nonmelanoma skin cancer. Md Med
J. 46:239–242. 1997.PubMed/NCBI
|
|
11
|
Panje WR, Pitcock JK and Vargish T: Free
omental flap reconstruction of complicated head and neck wounds.
Otolaryngol Head Neck Surg. 100:588–593. 1989.PubMed/NCBI
|
|
12
|
Chren MM, Linos E, Torres JS, Stuart SE,
Parvataneni R and Boscardin WJ: Tumor recurrence 5 years after
treatment of cutaneous basal cell carcinoma and squamous cell
carcinoma. J Invest Dermatol. 133:1188–1196. 2013. View Article : Google Scholar : PubMed/NCBI
|