Introduction
The jugular foramen is the point of communication
between the posterior fossa and the upper cervical vertebrae region
(1), and tumors developed within this
aperture lead to caudal cranial nerve lesions. The clinical
presentation of jugular foramen tumors is variable, depending on
the extent of involvement of the various cranial nerves (including
nerves IX, X, XI and XII) (2). Glomus
jugulare, paraganglioma and schwannoma are the most commonly
diagnosed tumors in the jugular foramen (3). The occurrence of a primary meningioma
within the jugular foramen is rare (4), particularly the occurrence of papillary
meningioma (PM) within the jugular foramen. In 2004, Tabuse et
al (5) reported the first case of
jugular foramen PM (5).
Meningioma accounts for 24–30% of primary
intracranial tumors diagnosed in the USA (6). The majority of meningiomas are benign,
slow-growing tumors with a good prognosis. However, PM is an
aggressive histological variant of meningioma, accounting for
1.0–2.5% of all the intracranial meningiomas diagnosed (7). According to the 2007 revision of the
World Health Organization (WHO) tumor classification system
(6), PM is pathologically identified
as Grade III in cases where a perivascular or pseudopapillary
pattern is present in the meningioma (8). The present study reported the case of an
adult male patient who presented with paralysis of the cranial
nerve XII and was diagnosed with a meningioma in the jugular
foreman. The aim of the current study was to present the management
of this rare entity and briefly provide its clinical, radiological
and pathological characteristics, as well as to describe the
surgical treatment strategy used and the outcome four years after
surgery. This study was approved by the Ethics Committee of The
First Hospital of Jilin University (Changchun, China) and written
informed consent was obtained from the patient.
Case report
A 21 year-old male presented at the First Hospital
of Jilin University (Changchun, China) in March 2010 with symptoms
of headache and dizziness that had persisted for six months. A
neurological examination revealed left hypoglossal nerve palsy and
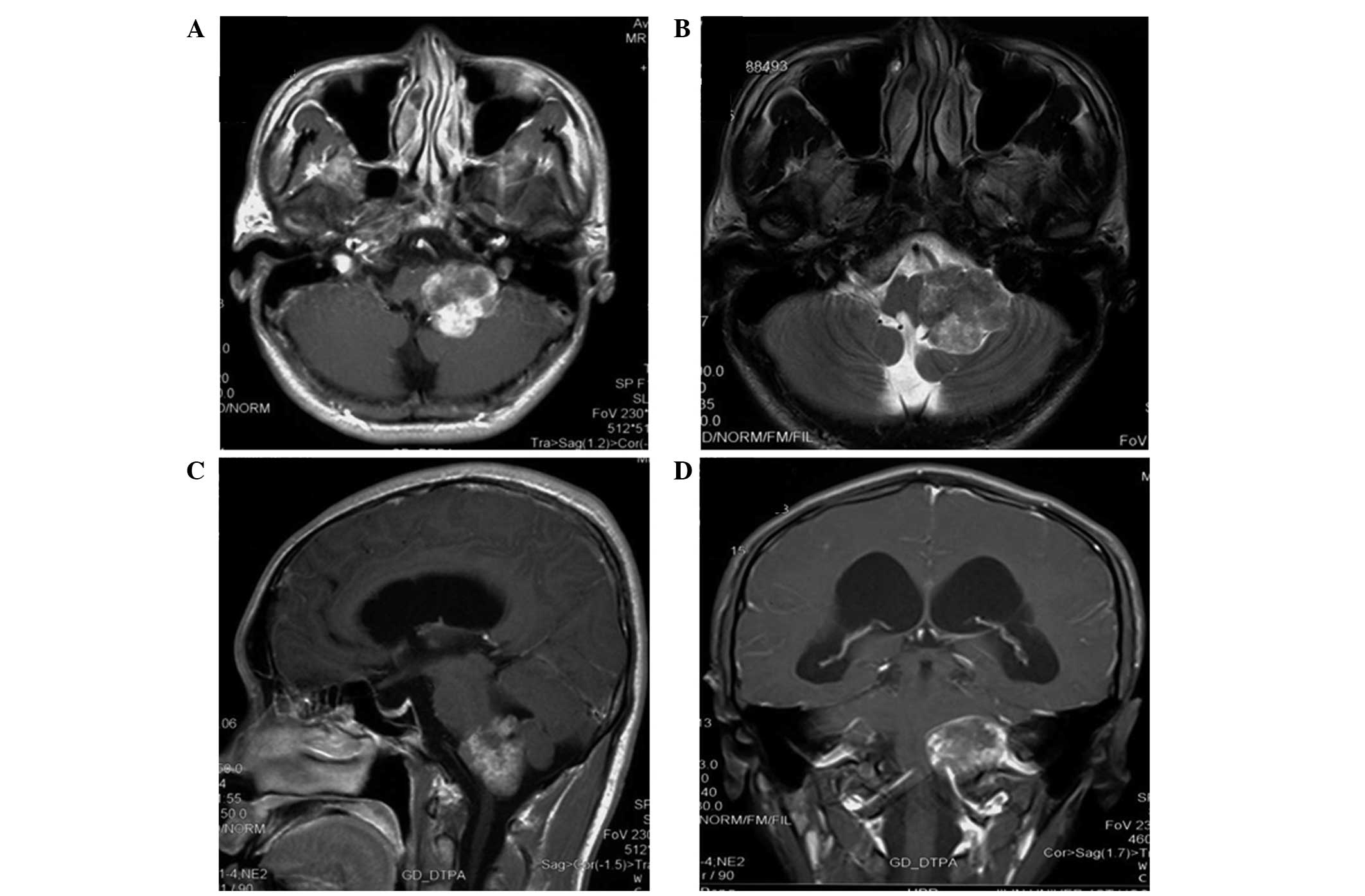
a left cerebellar sign (left-hand weakness). Computed tomography
(CT) scans of the brain revealed a high-density mass in the left
jugular foramen area, which was compressing inward onto the
brainstem and the fourth brain ventricle. In addition, the
bilateral and third brain ventricles were enlarged (Fig. 1A). A bone CT scan demonstrated
expansion of the left jugular foramen and destruction of the
adjacent bone (Fig. 1B). Furthermore,
magnetic resonance imaging (MRI) scans of the brain identified a
round, irregular signal (3.0×2.5×1.0 cm) in the left jugular
foramen and verified the compression and enlargement patterns
observed in the CT scans (Fig. 2A and
B). Subsequent MRI scans using gadopentetate dimeglumine as a
contrast agent demonstrated an enhanced irregular lesion (Fig. 2C and D).
The patient underwent a craniotomy for symptomatic
improvement. Subsequently, complete surgical resection of the tumor
was performed using a left far-lateral approach (9). During surgery, the tumor was identified
to be attached to the dorsal part of the left petrous bone. The
tumor-adjacent bone was evidently destroyed, and regions with the
greatest extensive destruction were removed. Clear boundaries
existed between the tumor and normal brain tissue, and the
resection was conducted along these boundaries. The dural
attachment was identified and coagulated; however, cranial nerves V
and VII–XI were found to be intact.
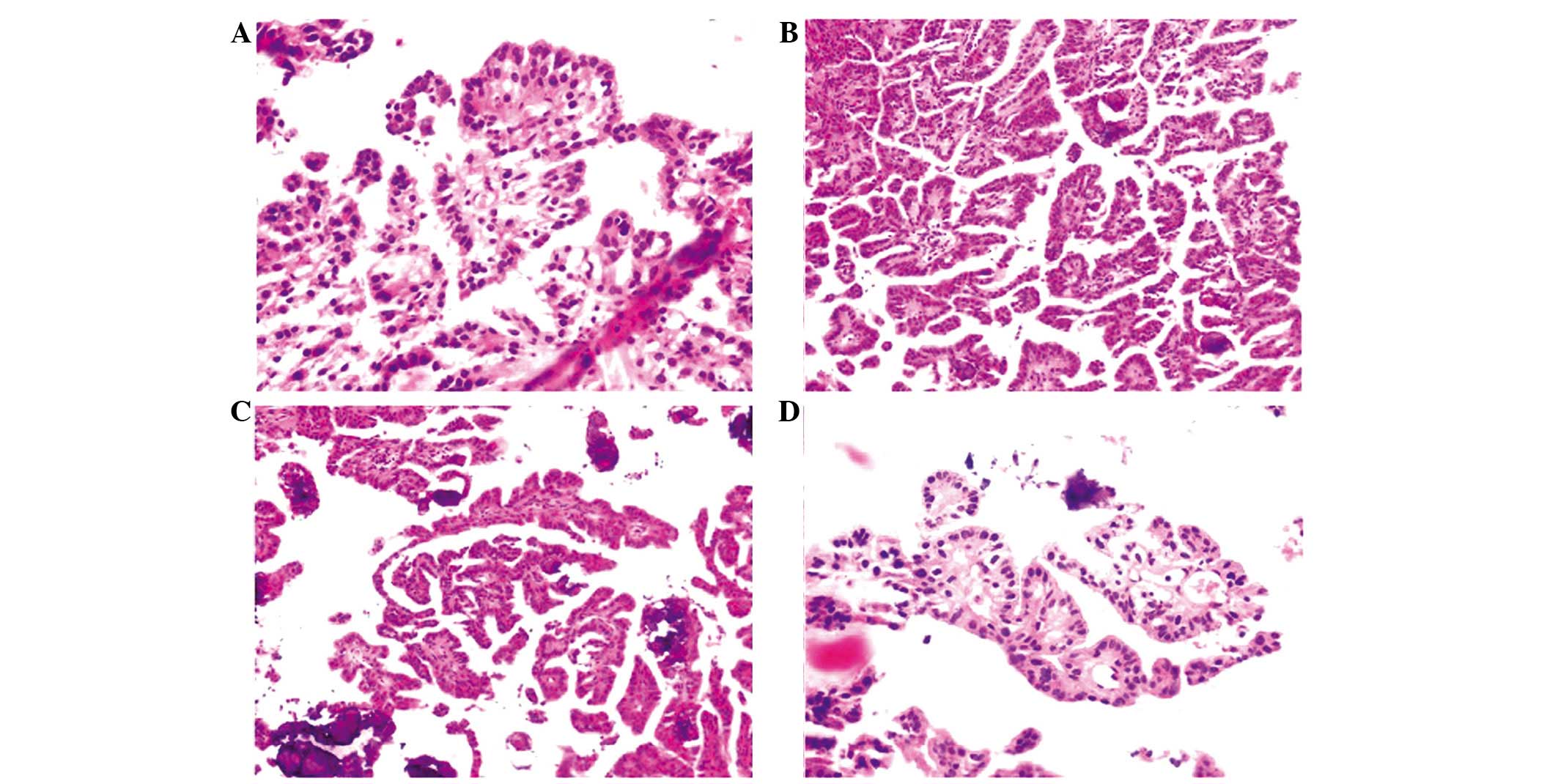
The resected tumor was grey in color and 3.0×2.5×1.0
cm in size, and appeared to be solid and gritty. Microscopically,
the tumor consisted of a monolayer of cells, which were arranged in
a perivascular pseudorosette pattern surrounded by fibrous vessels
with rich papillary growth. The papillary area was characterized by
mitotic cells, regions of focal necrosis and eosinophilic cells
with foamy nucleoli. Immunohistochemical staining (Fig. 3) revealed that the tumor cells were
positive for galectin-3 and the epithelial membrane antigen. By
contrast, immunostaining was negative for the primary adenoma
(thyroid transcription factor-1 and cytokeratin 7), astrocyte
(glial fibrillary acidic protein), thyroid cancer (thyroglobulin),
meningioma (progestogen) and neuroendocrine tumor (synaptophysin)
markers. However, immunostaining for the mesenchymal cell marker,
vimentin, was inconclusive. These pathological findings identified
the tumor to be a Grade III PM, according to the WHO
classification.
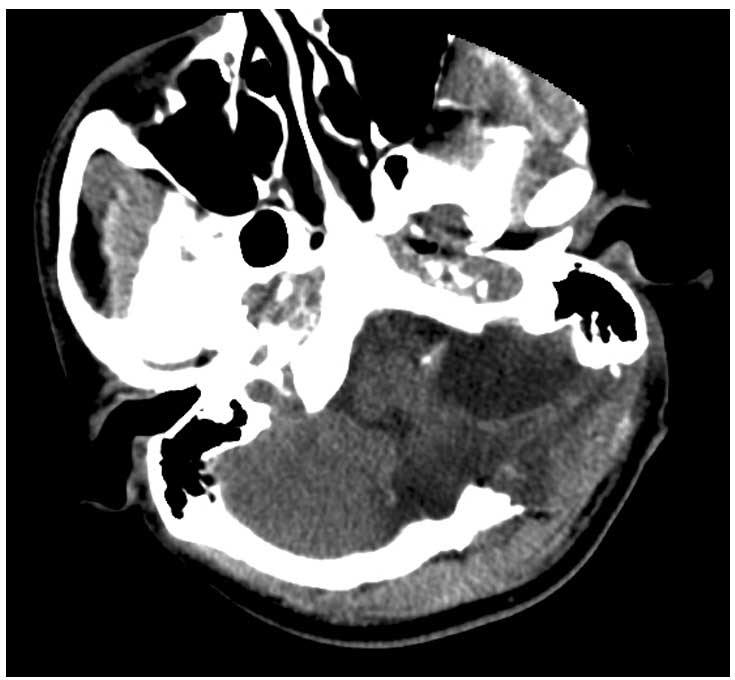
The resection surgery was uneventful and no
secondary symptoms emerged. CT scanning one day after surgery
confirmed that the tumor had been completely resected. This was
evidenced by the replacement of the high-density mass in the left
jugular foramen area, which was present in the preoperative CT
scan, with a hypo-density signal in the postoperative scan
(Fig. 4). However, the patient
continued to experience persistent headaches and dizziness, which
were completely resolved 10 days after surgery. Within the
four-year follow-up period following surgery, the cerebellar
impairment and cranial nerve XII palsy were improved. However, the
patient refused all recommendations for MRI examinations and
further treatment due to personal reasons. A physical follow-up
examination was performed in May 2012 and a telephone follow-up
examination was conducted in February 2014, which revealed that the
patient was well with no tumor recurrence.
Discussion
The present study reported a case of PM, which is a
rare meningioma type, that was located within the jugular foramen.
Complete tumor excision was performed without causing further
neurological deficits. After four years of follow-up, no evidence
of transformation or recurrence was identified.
Meningioma is a common intracranial neoplasm,
accounting for 24–30% of primary intracranial tumors occurring in
the USA (6). However, meningioma or
PM arising from the jugular foramen are uncommon (8). Thus, only a limited number of PM cases
in the jugular foramen have been reported in the literature. For
instance, Wang et al (10)
performed a large clinicopathologic study investigating 30 PM
cases; however, no cases presented PM in the jugular foramen. To
the best of our knowledge, the first case of jugular foramen PM was
reported by Tabuse et al (5)
in 2004.
Although PM is rare, it is a well-recognized
histological variant of meningioma. The first reported case of PM
was presented by Cushing and Eisenhardt in 1962 (11). A study reviewing 123 primary PMs
revealed that PM tumor types were not gender-specific, but tended
to occur in young adult patients with an average age of 35 years
(12). In addition, 25% of the tumors
assessed occurred in patients within the first two decades of their
life, with a slightly increased incidence in females (female to
male ratio, 3:2). Furthermore, Ludwin et al (13) identified that a relatively large
proportion of PM cases in their study (8/17 patients) occurred in
children, while Pasquier et al (14) reported seven cases of PM that occurred
in patients between the ages of 21 and 69 years. In the population
of the latter study, five of the tumors were supratentorial, one
was located in the left temporal bone and one was located in the
thoracic spinal canal (14). Thus,
the supratentorial region was suggested to be a common location of
PM. This observation was also confirmed by a further study by Wang
et al (15), which reported 17
PM cases.
Regarding the clinical behavior of PM, the study by
Ludwin et al (13) indicated
that these tumors frequently display an aggressive clinical
behavior, which is marked by a high rate of local recurrence and/or
development of distant metastases. Jiang et al (16) reported a case of intraparenchymal PM
of the brainstem. In addition, other studies have identified
correlations between the clinical behavior of PM and certain
clinical features. For instance, in a study of eight PM cases
(17), two patients exhibited
long-term survival without recurrence, two patients succumbed to
the disease shortly after surgery, and four patients presented one
or more recurrences and eventual PM-associated mortality. Those
authors identified a correlation between ‘more malignant’
histological aspects and ‘more aggressive’ clinical behavior
(17). Pasquier et al
(14) also reached a similar
conclusion, reporting that certain histological features (including
necrosis, high mitotic index and rich peripapillary reticulin
network) and tumor evolutionary events (such as high rate of local
recurrence or development of distant metastases) were correlated
and may represent a histological link between syncytial,
fibroblastic and hemangiopericytic meningiomas.
PM is generally associated with a high mortality
rate. Wang et al (15)
reported that the 3-year mortality rate for PM was 50% after gross
total resection and 63.6% for other cases. A previous study
concluded that the majority of PM cases reported in the literature
are aggressive variants of meningioma, with frequent local
recurrence, dissemination in the cerebral spinal fluid and
metastases to remote sites (18). In
addition, local recurrence of PM has been reported in 56.5% of
cases, which is significantly higher compared with the 10–20%
recurrence rate reported for conventional meningiomas (19). Furthermore, the aggressive behavior of
PM associated with morbidity and mortality warrants a timely
recognition of the diagnosis (20).
A genetic study has also been conducted in PM
patients, by Weber et al (21), in which a comparative genomic
hybridization screening for genomic imbalances was performed in
benign, atypical and anaplastic sporadic meningiomas. The authors
identified that accumulation of genomic aberrations occurred in
parallel with increasing malignancy grade. Thus, genetic profiles
of meningiomas were proposed corresponding to tumors with varying
degrees of malignancy.
Considering the frequent malignant behavior of PM,
radical surgical intervention is the routine treatment strategy.
However, surgical manipulation of the jugular foramen region is
challenging (22). Although the
treatment of choice for meningiomas is complete resection, this may
not be feasible for jugular foramen PM. The principal aim of
surgical treatment is to improve survival, while a secondary
objective is to return the function of caudal cranial nerves
(23). Therefore, the development of
a PM management strategy that is noninvasive/nonsurgical is
crucial. A previous study has evaluated the efficacy of
radiotherapy or chemotherapy, but reported inconclusive findings
(5). Due to the rarity of PMs, no
clear consensus exists regarding the appropriate management of the
disease. However, the combination of aggressive surgical resection
and postoperative radiotherapy has emerged as a standard treatment
strategy for PM (16,23). For patients with asymptomatic
recurrence or high-risk surgical cases, stereotactic radiosurgery
may be a useful alternative. Mattozo et al (24) analyzed the efficacy of a stereotactic
radiation treatment strategy in patients with recurrent nonbenign
meningiomas. The results indicated that stereotactic radiation
treatment provided effective local control of ‘aggressive’ Grade I
and II meningiomas; however, Grade III lesions maintained a poor
outcome. (24). Therefore, it is
critical to perform careful and long-term follow-up of patients due
to the malignant and aggressive behavior of this rare tumor.
However, in the current study, no further MRI scans were performed
following the decision of the patient, who did not present any
physical complaints during the postoperative follow-up period.
In conclusion, the present study reported a case of
jugular foramen PM in a young adult who presented with persistent
headaches and dizziness. The definitive diagnosis of PM relied on
histopathological findings. PM is a rare disease, particularly in
the jugular foramen area. Therefore, careful clinical care and
follow-up should be provided to manage this rare meningioma
considering its malignant and aggressive behavior.
References
|
1
|
Roche PH, Mercier P, Sameshima T and
Fournier HD: Surgical anatomy of the jugular foramen. Adv Tech
Stand Neurosurg. 33:233–263. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Samii M, Babu RP, Tatagiba M and Sepehrnia
A: Surgical treatment of jugular foramen schwannomas. J Neurosurg.
82:924–932. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gilbert ME, Shelton C, McDonald A, et al:
Meningioma of the jugular foramen: glomus jugulare mimic and
surgical challenge. Laryngoscope. 114:25–32. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ramina R, Neto MC, Fernandes YB, Aguiar
PH, de Meneses MS and Torres LF: Meningiomas of the jugular
foramen. Neurosurg Rev. 29:55–60. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tabuse M, Uchida K, Ueda R, Ikeda E and
Kawase T: Jugular foramen papillary meningioma: a case report.
Brain Tumor Pathol. 21:143–147. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Louis DN, Ohgaki H, Wiestler OD, et al:
The 2007 WHO classification of tumours of the central nervous
system. Acta Neuropathol. 14:97–109. 2007. View Article : Google Scholar
|
|
7
|
Enam SA, Abdulrauf S, Mehta B, Malik GM
and Mahmood A: Metastasis in meningioma. Acta Neurochir (Wien).
138:1172–1177. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Buccoliero AM, Caldarella A, Taddei A, et
al: Atypical, aplastic and unusual meningiomas. Morphology and
incidence in 300 consecutive cases. Pathologica. 95:83–87. 2003.(In
Italian). PubMed/NCBI
|
|
9
|
Flores BC, Boudreaux BP, Klinger DR,
Mickey BE and Barnett SL: The far-lateral approach for foramen
magnum meningiomas. Neurosurg Focus. 35:E122013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang XQ, Chen H, Zhao L, et al:
Intracranial papillary meningioma: a clinicopathologic study of 30
cases at a single institution. Neurosurgery. 73:777–790. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cushing H and Eisenhardt L: Meningiomas:
their classification, regional behaviour, life history, and
surgical end results. New York: Hafner Publishing Co. 199–207.
1962.
|
|
12
|
Shuangshoti S: Primary papillary
meningioma of the optic nerve sheath: a case of unique location and
benign pathology. Surg Neurol. 39:200–203. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ludwin SK, Rubinstein LJ and Russell DS:
Papillary meningioma: a malignant variant of meningioma. Cancer.
36:1363–1373. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pasquier B, Gasnier F, Pasquier D, Keddari
E, Morens A and Couderc P: Papillary meningioma. Clinicopathologic
study of seven cases and review of the literature. Cancer.
58:299–305. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang DJ, Zheng MZ, Gong Y, et al:
Papillary meningioma: clinical and histopathological observations.
Int J Clin Exp Pathol. 6:878–888. 2013.PubMed/NCBI
|
|
16
|
Jiang XB, Ke C, Han ZA, et al:
Intraparenchymal papillary meningioma of brainstem: case report and
literature review. World J Surg Oncol. 10:102012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Brignolio F and Favero M: Considerations
on the malignancy of papillary meningioma. Clinico-pathological
study of eight cases. Zentralbl Neurochir. 45:79–84.
1984.PubMed/NCBI
|
|
18
|
Meinsma-vdTuin M, Molenaar WM and Mooij
JJ: Spinal papillary meningioma: a case report and review of the
literature. Acta Neurochir (Wien). 142:703–708. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Thomas C and Leonetti JP: Papillary
(malignant) meningioma of the foramen magnum presenting as a
posterior neck mass. Skull Base Surg. 4:164–168. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jairajpuri Z, Jain I and Singh A:
Papillary meningioma: a rare malignant variant. Indian J Pathol
Microbiol. 54:410–411. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Weber RG, Boström J, Wolter M, et al:
Analysis of genomic alterations in benign, atypical, and anaplastic
meningiomas: toward a genetic model of meningioma progression. Proc
Natl Acad Sci USA. 94:14719–14724. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tekkök IH, Ozcan OE, Turan E and Onol B:
Jugular foramen meningioma. Report of a case and review of the
literature. J Neurosurg Sci. 41:283–292. 1997.PubMed/NCBI
|
|
23
|
Hanft S, Canoll P and Bruce JN: A review
of malignant meningiomas: diagnosis, characteristics, and
treatment. J Neurooncol. 99:433–443. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mattozo CA, De Salles AA, Klement IA, et
al: Stereotactic radiation treatment for recurrent nonbenign
meningiomas. J Neurosurg. 106:846–854. 2007. View Article : Google Scholar : PubMed/NCBI
|