Introduction
Breast angiosarcoma (BA) is a rare malignant
endothelial tumour (1,2). This tumour may be distinguished into
primary and secondary forms; the overall yearly incidences are
reported in the literature as 0.002–0.05% and 0.01–0.02%,
respectively (1). The aetiology of
primary BA, typically occurring in women <40 years of age,
remains unknown (2). These neoplasms
present as a growing, palpable mass that arises in the
non-irradiated breast parenchyma, with rare skin involvement
(3). Secondary BA may occur more
frequently after the fourth decade of life, particularly in
patients who have already been treated with radiation therapy
following breast-conserving surgery (2–5). It
presents as painless, multifocal skin changes that may be neglected
or misdiagnosed, or as a breast lump (3). Postoperative chronic lymphoedema is also
indicated as a potential causal factor for the development of
angiosarcoma in the breast and in the upper extremities, where it
is known as Stewart-Treves syndrome (2). BA generally arises 3–12 years after the
initial surgical and radiation therapies (6). Recurrences are rare >2 years after
surgery, and their predominant characteristics are clinical and
imaging heterogeneity (1,5).
The current study presents an unusual case of
non-metastatic late recurrent BA in an elderly woman with atypical
clinical features, including a long time interval between the first
and second occurrences of angiosarcoma, and a 25-month disease-free
survival period.
Case report
An 83-year-old female, exhibiting a superficial,
palpable painless lump in the left breast that had appeared ~1
month prior, was admitted to the General Surgery Unit of the
University Hospital of Messina (Messina, Italy) in January 2013.
Her history included hypertension, gastritis and
osteoarthritis.
In 2002, the patient had undergone a left
superoexternal quadrantectomy with synchronous ipsilateral axillary
lymph node dissection for an invasive ductal carcinoma. The lymph
nodes did not appear to be involved despite the presence of
palpable nodes in the axilla, and the patient also developed slight
postoperative lymphoedema. She was then assigned to receive
adjuvant radiotherapy in association with a 5-year hormone-therapy
schedule, consisting of tamoxifen (20 mg/day). Whole breast
irradiation was performed at a dose of 50 Gy in 25 fractions (200
cGy/fraction), plus a boost of 10 Gy (200 cGy/fraction) on the
breast bed, between May and June of 2002.
In 2008, the patient underwent a Madden mastectomy
for a secondary angiosarcoma (7). The
anatomopathological examination of the latter indicated a
cutaneous, well-differentiated angiosarcoma of 15 mm in its largest
diameter, with moderately atypical spindle cells delimiting thin
vascular spaces; the tissue also exhibited frequent mitoses, a
moderate (30%) MIB-1 labelling index (LI), and an intense
immunoreaction to endothelial markers, including cluster of
differentiation (CD)31 and CD34. No adjuvant treatment was
performed following the last surgical procedure, in accordance with
the recommendation of the International Society of Geriatric
Oncology (8).
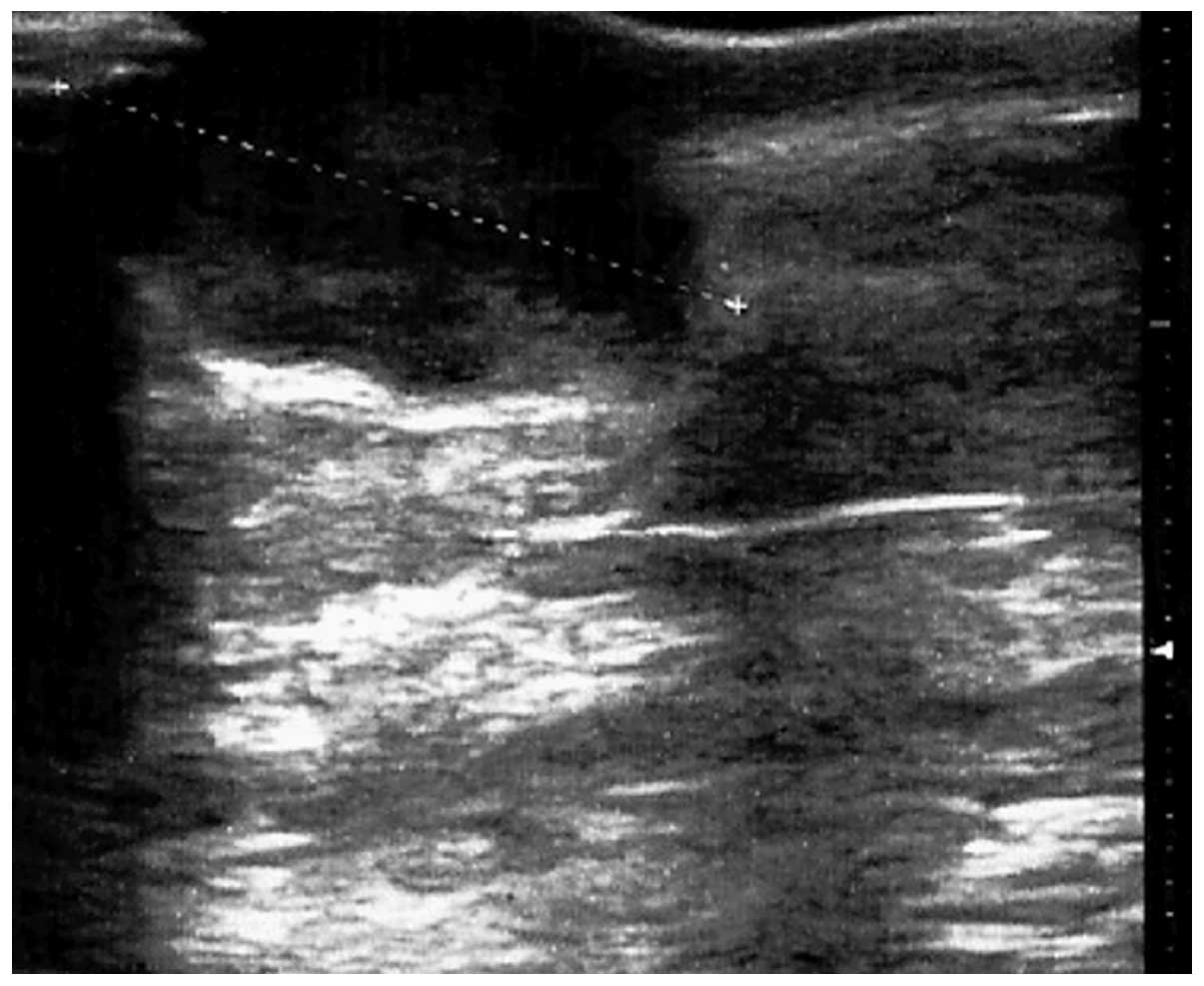
When assessed in January 2013, the patient presented
a cutaneous mass in the upper-inner quadrant of the breast, ~25 mm
in diameter, surrounded by a hyperaemic area, with no other
systemic symptoms or abnormal clinical findings (Fig. 1). An ultrasound scan (Esaote MyLab™
25; Esaote SpA, Genoa, Italy) of the breast confirmed a
circumscribed hypo-anechoic oval nodule (~22 mm in diameter)
located in the left upper-inner breast quadrant, with an irregular
vascular pattern observed on colour Doppler, and a posterior
acoustic increase (Fig. 2). A
previous practitioner had considered this finding to be suggestive
of an abscess, despite the history of neoplasia in the patient.
Following fine-needle aspiration cytology, performed by means of a
25-gauge needle, a mesenchymal neoplasm was suspected; however,
these findings were inconclusive and did not allow the confirmation
of a diagnosis. Routine laboratory investigations yielded normal
results, with the exception of an elevated C-reactive protein level
of 1.9 mg/dl (normal range, 0–0.5 mg/dl). Standard thorax
radiography did not reveal any parenchymal lesions or pleural
effusions. Values for the tumour markers carcinoembryonic antigen,
carbohydrate antigen (CA)15-3 and CA125 were in the normal
ranges.
Based on these findings, the patient was subjected
to a superomedial second-look excision. The tumour was highly
vascularised, and the estimated blood loss was ~50 ml. An
aspirative drain was placed locally. Grossly, the surgical specimen
measured 55×28×25 mm and appeared as a cutaneous, greyish, nodular
lesion (25 mm in its greatest diameter).
Histological examination of the specimen was
conducted as follows. Formalin-fixed and paraffin-embedded
specimens were cut into 4 µm-thick serial sections and mounted on
silane-coated glass slides. Following de-waxing in xylene and
re-hydration in graded ethanol, antigen retrieval was performed by
heating slides in 0.01 M citrate buffer (pH 6.0) in a microwave
oven for 3 × 5 min. For the immunohistochemical study, sections
were incubated in a moist chamber with 0.1%
H2O2 in methanol to block intrinsic
peroxidase activity, and then with normal sheep serum to prevent
nonspecific adherence of serum proteins. Subsequently, the slides
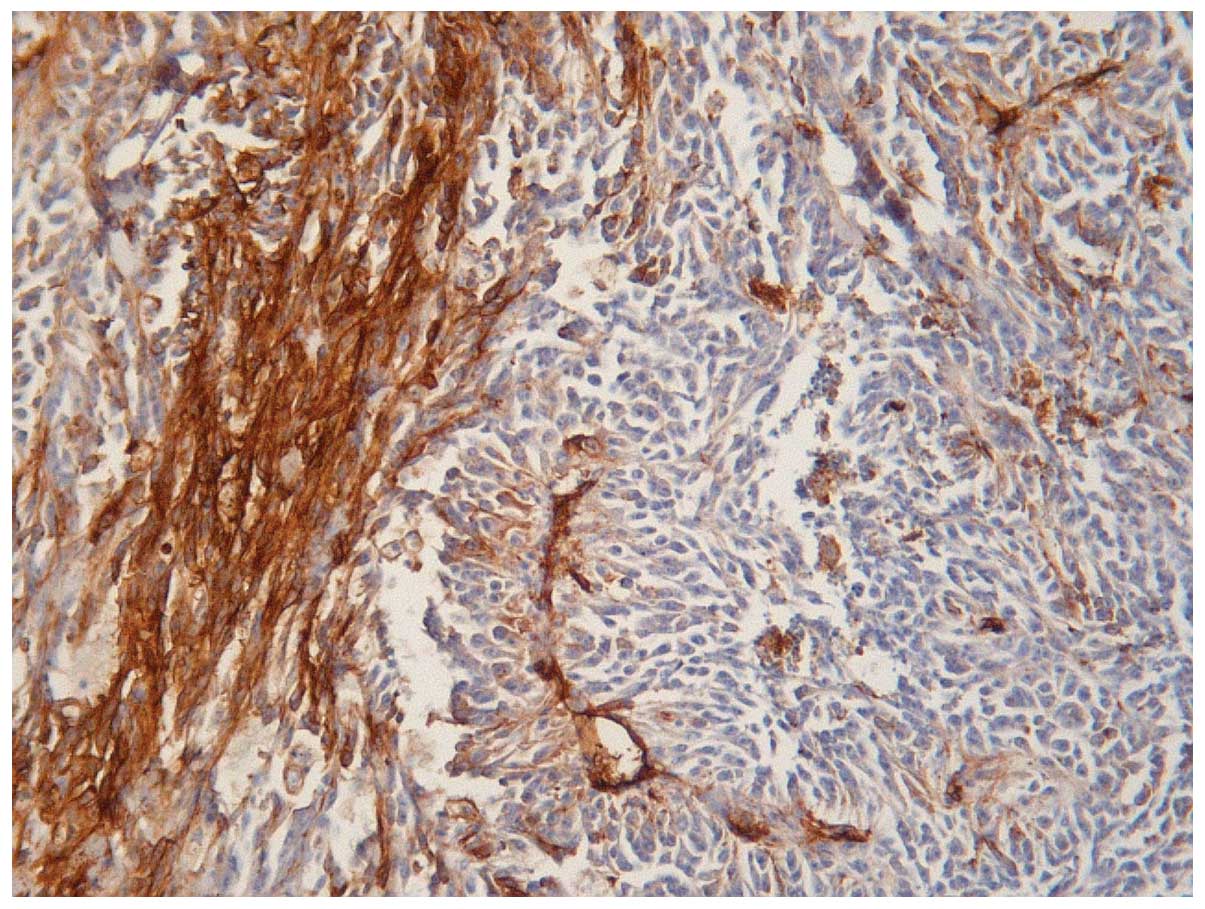
were incubated with the following primary antibodies: Mouse
monoclonal anti-human vimentin (#GA630; Clone V9; Dako, Glostrup,
Denmark; dilution, 1:100), CD34 (#GA632; Clone QBEnd 10; Dako;
1:50), CD31 (#GA610; Clone JC70A; Dako; 1:50) and Ki-67 (#GA626;
Clone MIB-1; Dako; 1:75). The slides were then incubated with sheep
anti-mouse IgG antiserum (#ab6808; Abcam, Cambridge, UK; 1:25) and
mouse anti-horseradish peroxidase-antiperoxidase complexes (LSAB 2
System-HRP; #K0672; Dako; 1:25) for 30 min each at room
temperature. For the demonstration of peroxidase activity the
sections were incubated in darkness for 10 min with
3–3′-diaminobenzidine tetra hydrochloride (Sigma-Aldrich, St.
Louis, MO, USA). Nuclear counterstaining was conducted with Mayer's
haemalum. Negative controls included omission of the primary
antiserum and replacement of the primary antiserum with
phosphate-buffered saline solution (pH 7.4) or normal horse serum;
in each of these conditions, no staining was evident. Histological
sections of capillary haemangiomas/haemangioblastomas were utilized
as positive controls for CD34 and CD31.
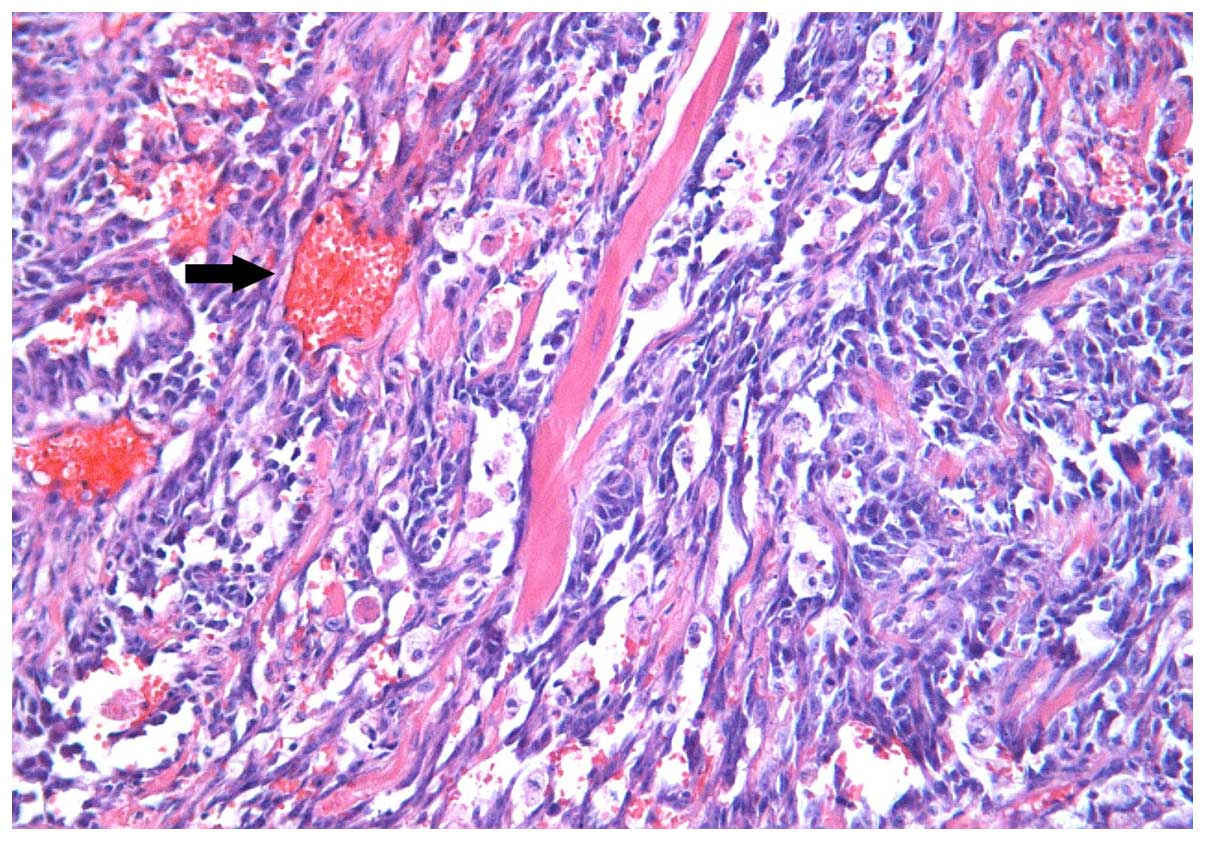
The microscopic appearance following
hematoxylin-eosin routine staining was consistent with recurrent
BA. The tumour exhibited a pseudo-papillary architecture
constituted by a vascular core surrounded by spindle- or
oval-shaped cells, with frequent mitoses, and significant
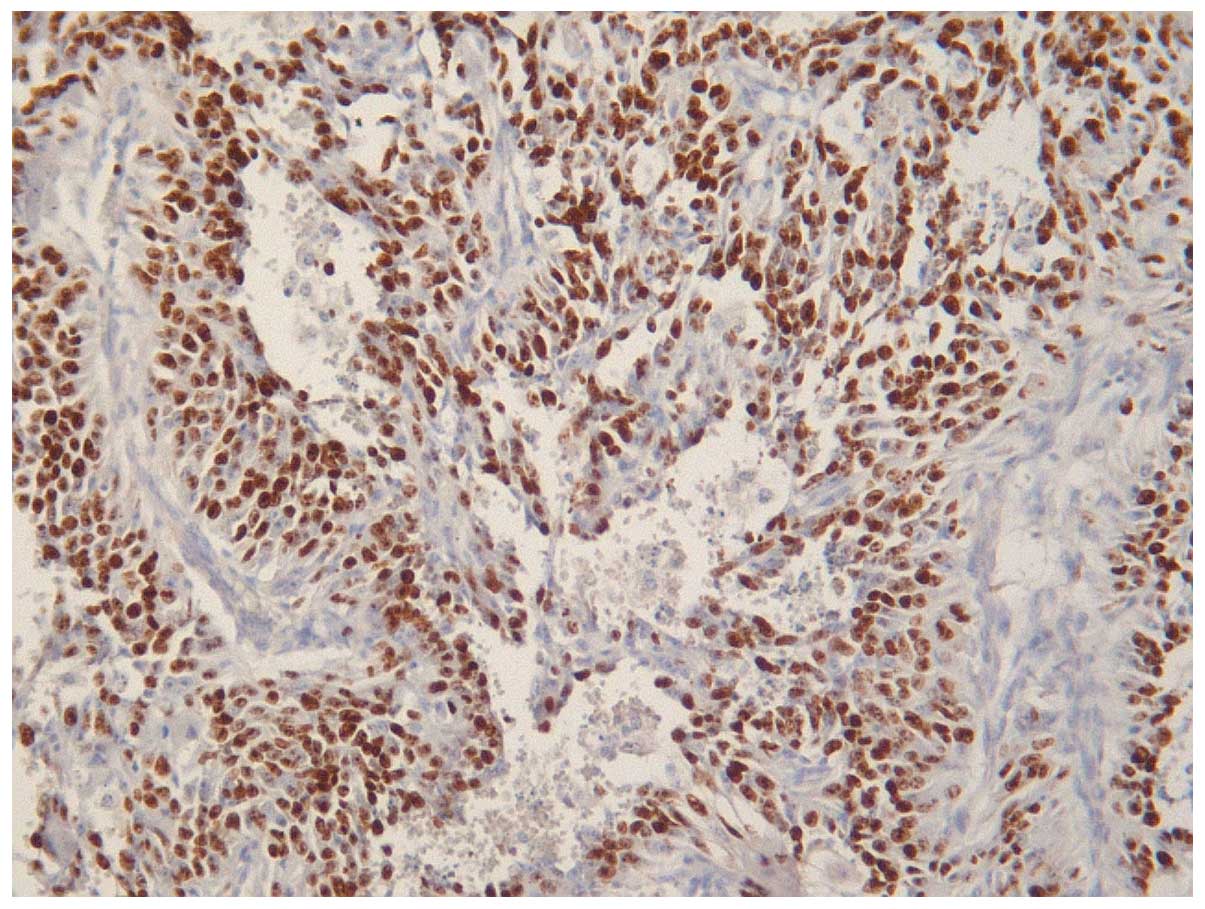
infiltration of the superficial and deep dermis (Fig. 3). An increased rate of neoplastic cell
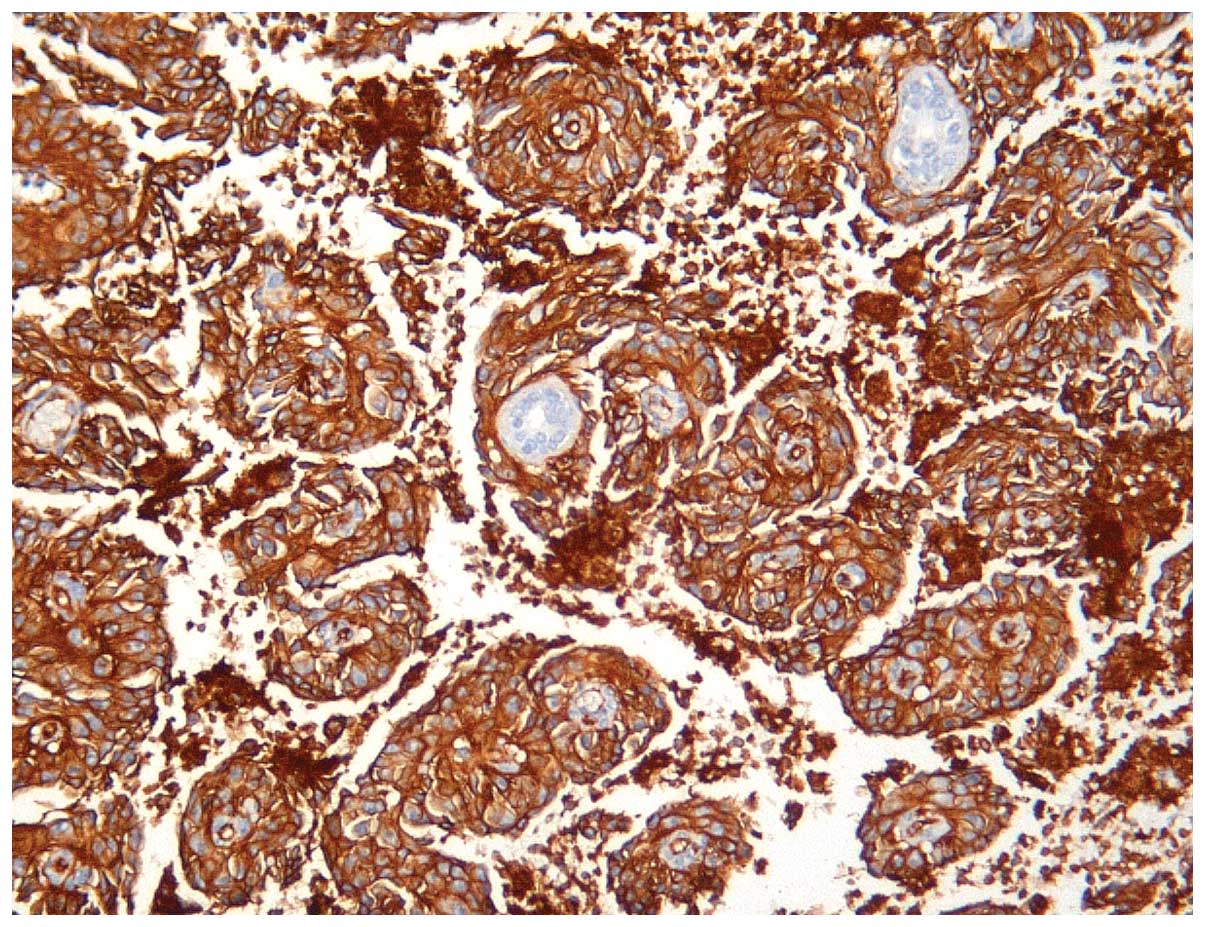
proliferation was revealed by the high MIB-1 LI (>80%; Fig. 4). On immunostaining, the evident
cytoplasmic immunoreactivity for CD31 and CD34 confirmed the
endothelial nature of the proliferating cells (Figs. 5 and 6),
and the immunopositivity for vimentin further supported the
mesenchymal origin. Surgical margins were unaffected and clear.
The patient's in-hospital stay was uneventful, the
drainage was removed, and she was discharged on the third
postoperative day. No complementary treatment was prescribed. At 25
months post-surgery, the patient was well and free of any clinical
local recurrence or distant metastases. In the follow-up period,
locoregional ultrasound examination findings were normal, and
whole-body scintigraphy and brain-thoracoabdominal computed
tomography scans (LightSpeed VCT; GE Healthcare, Fairfield, CT,
USA) did not reveal any recurrence or metastatic lesions.
Informed consent for the current report was obtained
from the patient.
Discussion
Angiosarcomas represent <2% of all soft tissue
sarcomas (1,5). BAs are rare neoplasms that develop from
the endothelial lining of the blood vessels (1–3). These
tumours are considered as primary in the absence of known risk
factors and, with an uncertain aetiology, they affect typically
women aged <40 years (1,2).
Secondary BAs generally occur in elderly patients
subsequent to adjuvant external-beam radiation therapy performed
with a breast-conserving surgery, with or without lymphoedema
(5). The first case of BA following
conservative surgery in association with radiation was reported in
1987 (9). A number of reports
indicate that, following the initial surgical and radiation
therapies, the interval of latency for the onset of an angiosarcoma
is 3–12 years (1,5,6). These
tumours are infiltrative, non-capsulated, cutaneous, soft-tissue
sarcomas (2). Their incidence has
been rising over the past 30 years (3). Histologically, they are characterised by
high cellularity, consisting of pleomorphic endothelial cells,
spindle-shaped, rounded or oval-shaped, arranged in loose or
cohesive clusters or sheets, or sometimes as single cells with a
scanty pale blue cytoplasm (6). BAs
are classified according to Donnel's Classification (10). Well-differentiated tumours include
open anastomosing vascular sinusoids, with a single layer of
abnormal endothelial cells that exhibit hyperchromatic nuclei and
few mitoses (2). In increasingly
aggressive disease, classified as a moderately differentiated
angiosarcoma, the vascular channels are less clearly defined, and
are associated with small foci of spindle-shaped cells, which are
multilayered or arranged in pseudopapillary structures with several
mitoses (6). The poorly
differentiated variety exhibits malignant endothelial cells
organised in continuous sheets, generally with epithelioid
features, blood lakes and necrosis (2).
Immunohistochemistry is useful to confirm the
diagnosis of BA (2,6,10).
Typically, the tumors are positive for endothelial markers,
including CD31, CD34, von Willebrand factor and vascular
endothelial growth factor (2). The
pathological differential diagnosis of this tumour includes
phyllodes sarcoma, stromal sarcoma, benign hemangioma,
myoepithelioma fibromatosis, fibrosarcoma, liposarcoma, metaplastic
carcinoma, squamous cell carcinoma with sarcomatoid features and
high-grade mammary carcinoma (3). The
diagnosis of secondary BA is predominantly clinical at first
observation, yet its appearance is highly variable in form
(5,6).
In the literature, these tumours have been described as a palpable
masses, which may be painful or painless, or as an erythematous
area or even as a lipoma (1,3,11). A
fine-needle aspiration biopsy is highly recommended (2,6).
A wide-margin surgical excision represents the
treatment of choice (2,5,12);
supplementary radiotherapy boost is typically avoided in cases of
radiation-associated BA (2).
Generally, BAs are localised and the tumour recurrences are most
frequent within 1 year from surgical treatment (5,12).
Affected or unclear surgical margins and large tumour size are
considered poor prognostic factors (2,5). Due to
the increase in complementary radiotherapy following breast
conservative treatment, great attention to skin alterations is
recommended during the follow-up period in order to allow the early
detection of secondary lesions (1,5). Biopsies
must be encouraged, and radiological results should be analysed by
breast surgery specialists.
In conclusion, the current study reports a case of
BA in an elderly woman which recurred twice, 11 years after a
breast-conserving surgery with adjuvant radiotherapy, and 5 years
after the patient's first angiosarcoma excision. To the best of our
knowledge, this has not previously been reported in the literature.
Clinicians should be aware of this unusual occurrence and of any
possible misdiagnosis.
Acknowledgements
The authors wish to thank Dr Giuseppe Campisi, a
member of the surgical team at the University Hospital of
Messina.
References
|
1
|
Vorburger SA, Xing Y, Hunt KK, Lakin GE,
Benjamin RS, Feig BW, Pisters PW, Ballo MT, Chen L, Trent J III, et
al: Angiosarcoma of the breast. Cancer. 104:2682–2688. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Young RJ, Brown NJ, Reed MW, Hughes D and
Woll PJ: Angiosarcoma. Lancet Oncol. 11:983–991. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Scow JS, Reynolds CA, Degnim AC, Petersen
IA, Jakub JW and Boughey JC: Primary and secondary angiosarcoma of
the breast: The mayo clinic experience. J Surg Oncol. 101:401–407.
2010.PubMed/NCBI
|
|
4
|
Zelek L, Llombart-Cussac A, Terrier P,
Pivot X, Guinebretiere JM, Le Pechoux C, Tursz T, Rochard F,
Spielmann M and Le Cesne A: Prognostic factors in primary breast
sarcomas: A series of patients with long-term follow-up. J Clin
Oncol. 21:2583–2588. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Monroe AT, Feigenberg SJ and Mendenhall
NP: Angiosarcoma after breast-conserving therapy. Cancer.
97:1832–1840. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gherardi G, Rossi S, Perrone S and Scanni
A: Angiosarcoma after breast-conserving therapy: Fine-needle
aspiration biopsy, immunocytochemistry and clinicopathologic
correlates. Cancer. 105:145–151. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Madden JL: Modified radical mastectomy.
Surg Gynecol Obstet. 121:1221–1230. 1965.PubMed/NCBI
|
|
8
|
Wildiers H, Kunkler I, Biganzoli L,
Fracheboud J, Vlastos G, Bernard-Marty C, Hurria A, Extermann M,
Girre V, Brain E, et al: International Society of Geriatric
Oncology: Management of breast cancer in elderly individuals:
recommendations of the International Society of Geriatric Oncology.
Lancet Oncol. 8:1101–1115. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Body G, Sauvanet E, Calais G, Fignon A,
Fetissof F and Lansac J: Cutaneous angiosarcoma of the breast
following surgery and irradiation of breast adenocarcinoma. J
Gynecol Obstet Biol Reprod (Paris). 16:479–483. 1987.PubMed/NCBI
|
|
10
|
Donnell RM, Rosen PP, Lieberman PH,
Kaufman RJ, Kay S, Braun DW Jr and Kinne DW: Angiosarcoma and other
vascular tumors of the breast. Am J Surg Pathol. 5:629–642. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Meroni S, Moscovici O, Menna S, Renne G,
Sosnovskikh I, Rossi V and Cassano E: Ultrasound challenge:
Secondary breast angiosarcoma mimicking lipoma. Breast J.
19:437–438. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Biswas T, Tang P, Muhs A and Ling M:
Angiosarcoma of the breast: A rare clinicopathological entity. Am J
Clin Oncol. 32:582–586. 2009. View Article : Google Scholar : PubMed/NCBI
|