Introduction
Epithelioid angiomyolipoma (EAML) is a rare
mesenchymal neoplasia (1). At
present, EAML is considered a member of the perivascular
epithelioid cell (PEC) tumors known as PEComas (2), which are a type of epithelioid tumors
adjacent to vessels and different from hamartomas (3). EAML is generally considered benign and
the majority of patients with EAML usually have a good prognosis.
However, EAML possesses malignant potential, which may lead to a
poor prognosis (4,5). The treatment for patients with single
lesion hepatic EAML is surgical resection (1,6–14). Multiple lesion hepatic EAML is usually
metastatic, which indicates a poor prognosis of the patients. For
these patients, no good treatments can be conducted. Therefore,
early diagnosis of EAML is very important (15–17).
The majority of EAMLs originate in the kidneys, and
primary hepatic EAML appears to be much less common than renal EAML
(1). In the present study, 3 cases of
hepatic EAML are presented, and a review of the relevant English
literature is conducted.
Case report
Clinical data and literature
review
Clinical data of the 3 EAML cases described in the
present study were obtained from the records of the China-Japan
Union Hospital of Jilin University (Changchun, China). The current
study was approved by the ethics committee of the China-Japan Union
Hospital of Jilin University.
For the literature review, different keyword
combinations, including ‘liver and EAML’, ‘liver and epithelioid
angiomyolipoma’, ‘hepatic monotypic epithelioid angiomyolipoma’ and
‘atypical angiomyolipoma’, were used for searching studies on
hepatic EAML published in PubMed (www.ncbi.nlm.nih.gov/pubmed), MEDLINE (www.proquest.com/products-services/medline_ft.html)
and Google Scholar (http://scholar.google.com). Articles were selected
when full-text versions were available and contained adequate
patient information for comparison. Literature reviews and
duplicate reports were excluded. Table
I lists the collected information, including author names and
year of publication, as well as patient's age, gender, medical
history, presence of single or multiple tumors, tumor site, tumor
size, symptoms, treatment, results of immunohistochemical staining
and follow-up (6–18). A total of 17 publications met the
selection criteria, which corresponded to 24 patients, including
the 3 present cases. Demographic and clinical data of the 24
patients are presented in Table I.
The mean age of the patients was 47±15 years (range, 23–80 years).
Of the 24 patients, 17 were females, and 4 exhibited multiple
hepatic EAML, all patients had a history of renal EAML, 3 of which
had been previously diagnosed as tuberous sclerosis (TSC). Tumor
diameters of patients with single lesions varied from 2.8 to 32.0
cm. Tumors were equally distributed between the two lobes of the
liver. Of the patients with single lesions, 2 underwent surgery,
and relapsed after 5 months and 9 years, respectively. All patients
were positive for human melanoma black (HMB)-45 or melan A
staining.
 | Table I.Demographic and clinical data of
hepatic EAML reports. |
Table I.
Demographic and clinical data of
hepatic EAML reports.
| Author, year | Case | Age, years | Gender | Medical history | Tumor number | Tumor site | Tumor size, cm | Symptoms | Treatment | IHC | Follow-up | Refs. |
|---|
| Dalle et al,
2000 | 1 | 70 | F | Breast cancer | Single | Right lobe | ф15.0 | Fever, abdominal
pain, dyspnoea | Partial
hepatectomy | HMB-45+,
NKI/C3+, CK-, CEA-, VIM- | Recurrence after 5
months | (6) |
| Yamasaki et
al, 2000 | 2 | 30 | F | Nil | Single | Right lobe | ф3.0 | Nil | Partial
hepatectomy | HMB-45+,
S-100+, VIM+−desmin+−,
SMA+−, EMA−,CK− | 12 months aw | (1) |
| Mai et al,
2001 | 3 | 51 | F | Renal EAML | Multiple | Whole liver | ф5.0 (max) | Lumbar pain, weight
loss, low-grade fever | N/A | HMB-45+,
SMA+, PAS+, CK−, AFP−,
AE1/AE3−, | N/A | (15) |
| Hino et al,
2002 | 4 | 34 | M | TSC, renal EAML | Multiple | Whole liver | N/A | Nil | Partial
hepatectomy | HMB-45+,
SMA+, VIM+, S-100−, Ki-67
1.6% | N/A | (18) |
| Tryggvason et
al, 2004 | 5 | 42 | F | Nil | Single | Left lobe | ф7.0 | Abdominal pain,
change in bowel habits, weight loss | Partial
hepatectomy | HMB-45+,
melan A+, CEA−, EMA−,
CD117−, SMA−, S-100−,
AE1/AE3− | N/A | (7) |
| Parfitt et al,
2006 | 6 | 60 | F | Nil | Single | Right lobe | 14.0 ×11.0 | Abdominal pain | Right hepatic
lobectomy | HMB-45+,
melan A+, SMA+, S100−,
AE1/AE3−, VIM−, MSA−,
CD31−, CD34− | Recurrence after 9
years | (8) |
| Alatassi and Sahoo,
2009 | 7 | 23 | F | Bilateral renal
AML, TSC | Multiple | Whole liver | ф4.0 −11.0 | Abdominal pain | N/A | HMB-45+,
SMA+, CK−, S-100− | N/A | (16) |
| Xie et al,
2012 | 8 | 32 | F | Bilateral renal
AMLs, TSC, seizures, cardiac rhabdomyomas, cutaneous angiofibromas,
multiple giant cell astrocytomas | Multiple | Whole liver | ф4.0 (max) | Progressive
dyspnea, cough, fever | N/A | HMB-45+,
melan A+, SMA+, MSA+,
CD34+, desmin−, EMA−,
TTF1− | N/A | (17) |
| Occhionorelli et
al, 2013 | 9 | 25 | F | Nil | Single | Left lobe | ф9.0 | Abdominal pain,
hypotension | Left-liver
lobectomy | HMB-45+,
melan A+, S-100−, actin−,
CK−, CK7−, desmin−, Ki-67 2% | N/A | (9) |
| Zhou et al,
2014 | 10 | 34 | F | Nil | Single | Left lobe | 30.0×25.0
×15.0 | Abdominal
discomfort | Left-liver
lobectomy | HMB-45+,
melan A+, S-100+,CD10−,
CD34−, CD117−, CK−,
AE1/AE3−, EMA−, AFP−, Ki-67
<1% | 71 months aw | (10) |
| Tajima et
al, 2014 | 11 | 38 | M | Nil | Single | Right | 10.5×9.5 ×7.0 | Abdominal pain | Right-liver
lobectomy | HMB-45+,
αSMA+, E-cadherin+−, β-catenin+−,
Ki-67 <1% | N/A | (11) |
| Dai et al,
2014 | 12 | Mean, 56.5 | 2M 3F | Nil | Single (all) | Right lobe
(3); left lobe (2) | 3.1×2.5-
7.0×5.2 | Abdominal pain
(2); no symptoms (3) | Partial
hepatectomy | N/A | N/A | (12) |
| Barbier et
al, 2014 | 13 | 80 | F | Breast cancer | Single | Right lobe | 11.0×7.0 ×7.0 | Nil | Right-liver
lobectomy | HMB-45+,
melan A+, SMA+, KL-1−,
AE1/AE3−, VIM−, desmin− | 28 months aw | (13) |
| Huang et al,
2015 | 14 | 70 | M | Gastric GIST | Single | Left lobe | ф2.8 | N/A | Partial
hepatectomy | pAKT−,
pp70S6K−, pS6+−, β-catenin− | 37 months aw | (14) |
| Huang et al,
2015 | 15 | 54 | F | Parathyroid
adenoma | Single | Left lobe | ф6.5 | N/A | Partial
hepatectomy | pAKT−,
pp70S6K+- pS7+, β-catenin− | 41 months aw | (14) |
| Huang et al,
2015 | 16 | 28 | F | Nil | Single | Left lobe | ф6.9 | N/A | Partial
hepatectomy | pAKT−,
pp70S6K+ pS8+−, β-catenin− | 44 months aw | (14) |
| Huang et al,
2015 | 17 | 31 | F | Nil | Single | Right lobe | ф1.5 | N/A | Partial
hepatectomy | pAKT−,
pp70S6K+- pS9+, β-catenin− | 15 years aw | (14) |
| Liu et al,
2016 | 18 | 60 | F | Nil | Single | Left lobe | 4.0×4.4 ×3.3 | Nil | Partial
hepatectomy | HMB-45+,
melan A+, SMA+, CD34+,
S-100+, VIM+, EMA−,
hepatocyte−, CK−, Ki-67 1% | 6 months aw | Present study Case
1 |
| Liu et al,
2016 | 19 | 46 | M | Nil | Single | Right lobe | ф2.8 | Nil | Partial
hepatectomy | HMB-45+,
melan A+, SMA+, CD34+,
S-100−, VIM+, EMA−,
hepatocyte−, CK−, Ki-67 <1% | 16 months aw | Present study, Case
2 |
| Liu et al,
2016 | 20 | 37 | M | Nil | Single | Left lobe | ф32.0 | Abdominal pain | Partial
hepatectomy | HMB-45+,
melan A+, SMA+, CD34+,
S-100−, VIM+, EMA−,
hepatocyte−, CK−, Ki-67 2% | 5 months aw | Present study, Case
3 |
Case 1
A 60-year-old woman was admitted to the China-Japan
Union Hospital of Jilin University on August 22, 2014, due to the
presence of liver masses, which were noted during routine physical
examination. The medical history of the patient was significant for
type B hepatitis. The levels of serum alpha-fetoprotein (AFP) were
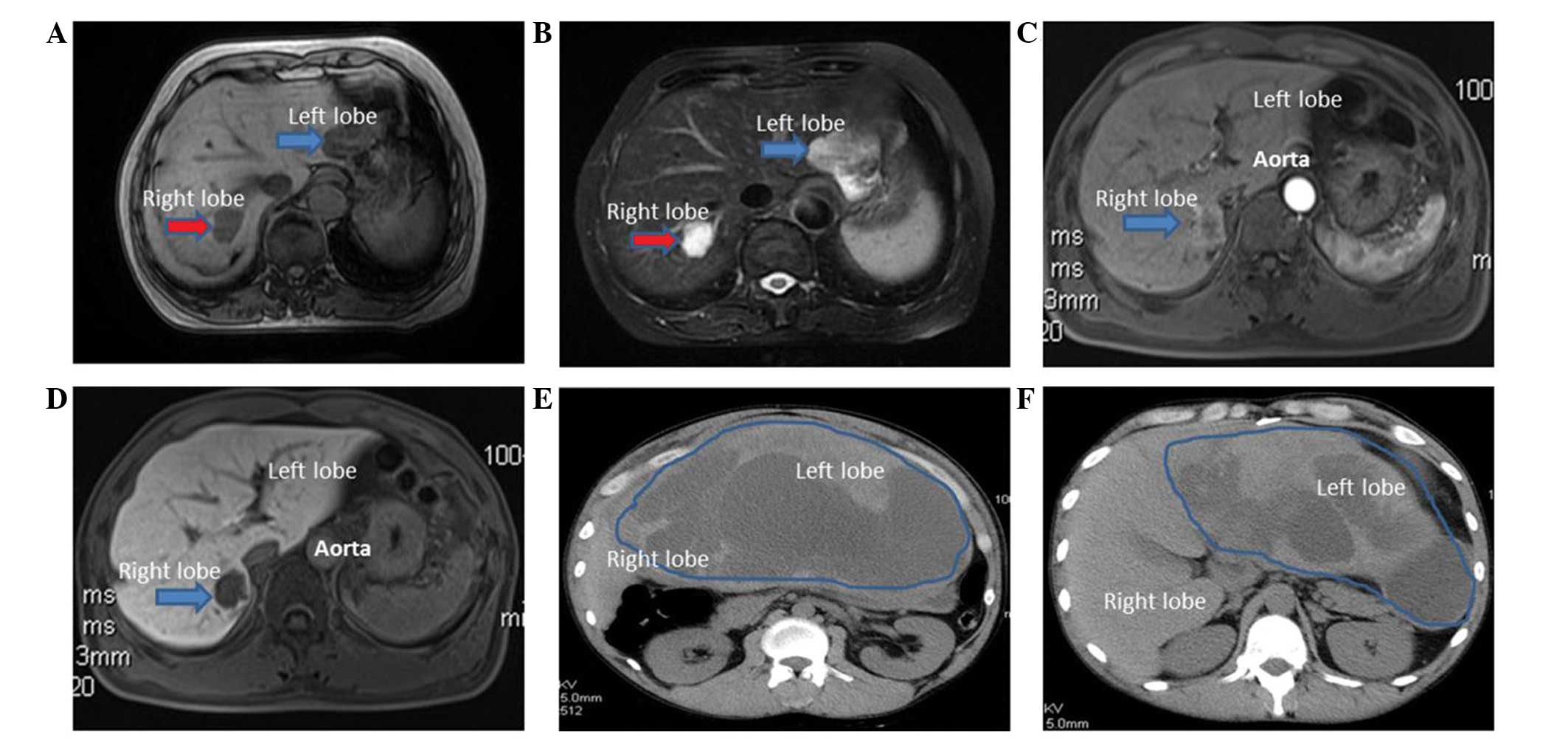
normal (3.0 µg/l; normal range, 0–20 µg/l). Abdominal magnetic
resonance imaging (MRI; MAGNETOM Avanto 1.5; Siemens AG, Munich,
Germany) revealed two hepatic masses. The mass in the right lobe
was hypointense on T1-weighted images and hyperintense on
T2-weighted images, which were typical features of hepatic
hemangioma (3). The other mass was
located in the left lobe, and was unequally isointense on
T1-weighted images and mildly hyperintense on T2-weighted images
(Fig. 1), thus being difficult to
differentiate from hepatoma. A laparoscopic hepatic left lateral
lobectomy was performed, and a neoplasia of 4 cm in diameter, which
was protruding from the liver surface, was identified.
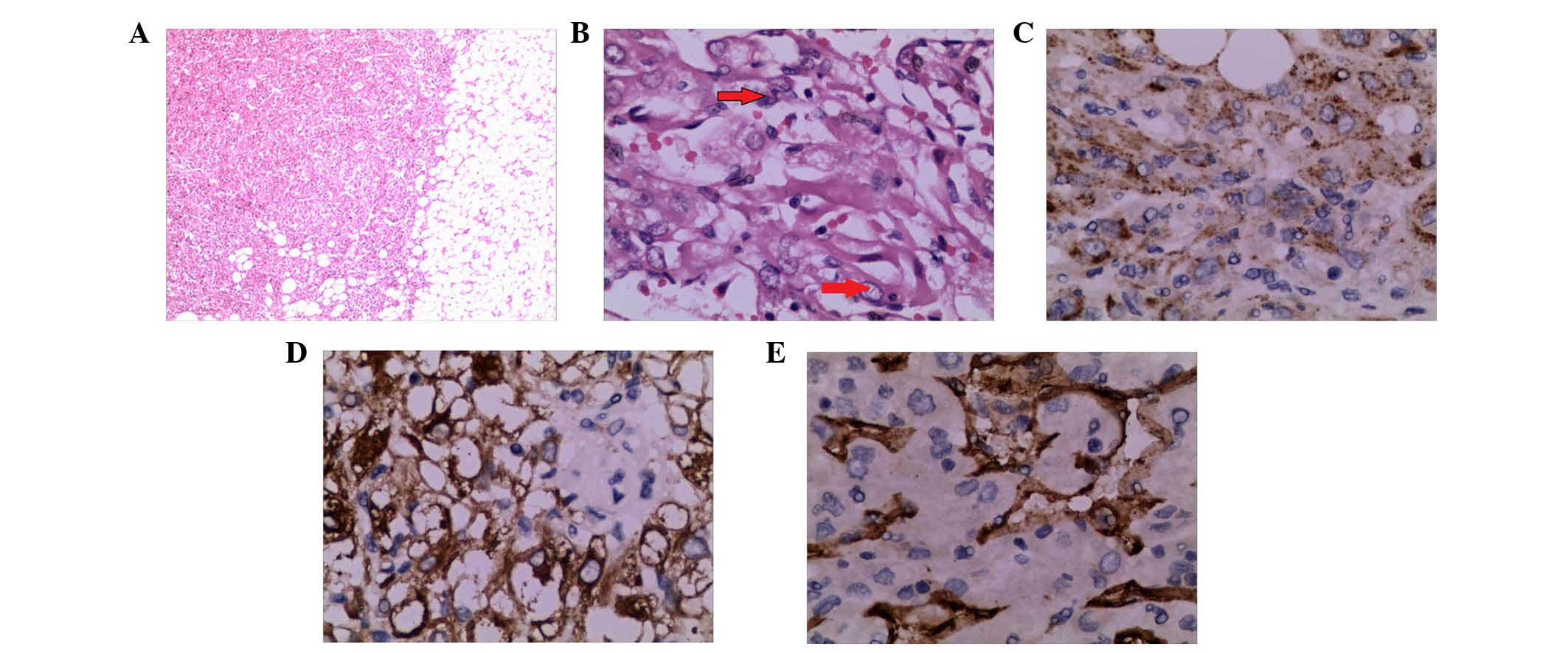
Post-surgical pathology concluded that the tumor was a hepatic
EAML. For immunohistochemistry, specimens were incubated overnight
at 4°C with the following antibodies: Monoclonal mouse anti-human
HMB-45 (#ab787; Abcam, Cambridge, UK), monoclonal mouse anti-human
melan A (#sc-271432; Santa Cruz Biotechnology, Inc., Dallas, TX,
USA), monoclonal rabbit anti-S-100 (#ab52642; Abcam), monoclonal
rabbit anti-vimentin (VIM; #ab92547; Abcam), monoclonal mouse
anti-human cluster of differentiation (CD)34 (#sc-19587; Santa Cruz
Biotechnology, Inc.), monoclonal mouse anti-pan-cytokeratin (CK;
#ab6401; Abcam), monoclonal mouse anti-human hepatocyte (#ab75677;
Abcam), polyclonal rabbit anti-α smooth muscle actin (SMA; #ab5694;
Abcam) and monoclonal rabbit anti-glypican-3 (#ab124829; Abcam).
All antibodies were diluted to a dilution ratio of 1:500 with 1%
bovine serum albumin, 0.05% sodium azide and 0.01 M
phosphate-buffered saline (pH 7.2). Staining demonstrated the tumor
to be positive for HMB-45, melan A, S-100, SMA, VIM and CD34, but
negative for CK, hepatocyte and glypican-3 (GPC-3).
Ki-67+ cells accounted for 1%.
Case 2
A 46-year-old man was admitted to hospital on August
30, 2013, due to a mass in the right hepatic lobe, which was
noticed during routine physical examination. Viral hepatitis
serology was negative and serum AFP levels were normal (5.7 µg/l;
normal range, 0–20 µg/l). MRI revealed a 2.8-cm mass in the right
posterior lobe, which was hypointense on T1-weighted images and
hyperintense on T2-weighted images. The tumor exhibited
ring-enhancements in the arterial phase, with a decrease in the
portal venous/delayed phase (Fig. 1).
The pathology results of an ultrasound (iU22 xMATRIX; Philips
Healthcare, Andover, MA, USA)-guided fine-needle aspiration biopsy
(FNAB) revealed hyperplastic lesions of pleomorphic cells. The
neoplasia was removed by surgical resection. Post-surgical
pathology confirmed the diagnosis of hepatic EAML. For
immunohistochemistry, specimens were incubated overnight at 4°C
with the following antibodies: Monoclonal mouse anti-human HMB-45,
monoclonal mouse anti-human melan A, monoclonal mouse anti-human
CD34, monoclonal rabbit anti-VIM, monoclonal rabbit anti-S-100,
polyclonal rabbit anti-epithelial membrane antigen (EMA; #P15941;
Abgent, Inc., San Diego, CA, USA), monoclonal mouse anti-pan-CK and
monoclonal mouse anti-human hepatocyte. All antibodies were diluted
with 1% bovine serum albumin, 0.05% sodium azide and 0.01 M
phosphate-buffered saline (pH, 7.2). Tumor cells were positive for
HMB-45, melan A, SMA, CD34 and VIM, but negative for S-100, EMA, CK
and hepatocyte. Ki-67+ cells accounted for <1%.
Case 3
A 37-year-old man presented to the emergency room on
September 26, 2014, complaining of persistent abdominal pain,
nausea and vomiting. Serum carbohydrate antigen 19–9 levels were
elevated (168.55 U/ml; normal range, 0.00–37.00 U/ml). Abdominal
contrast-enhanced computed tomography (CT; Discovery CT750 HD; GE
Healthcare Bio-Sciences, Pittsburgh, PA, USA) revealed a giant
hepatic tumor in the left lateral lobe. The tumor was 15.6×6.3×28.9
cm in size, and contained cystic and solid components (Fig. 1). The margins and septa of the tumor
were enhanced in the arterial phase and decreased in the portal
venous/delayed phase. The surgically resected specimen contained a
ruptured tumor with an outflow of kermesinus fluid from the
ruptured area (Fig. 2). The net
weight of the tumor was 10 kg and its diameter was 32.0 cm.
Pathology confirmed the diagnosis of hepatic EAML. Part of the
tumor tissue was necrotic. For immunohistochemistry, specimens were
incubated overnight at 4°C with the following antibodies:
Monoclonal mouse anti-human HMB-45, monoclonal mouse anti-human
melan A, monoclonal mouse anti-human CD34, monoclonal rabbit
anti-S-100, polyclonal rabbit anti-EMA (#P15941; Abgent, Inc., San
Diego, CA, USA), polyclonal rabbit anti-human AFP (#ab182645;
Abcam), monoclonal mouse anti-pan-CK, monoclonal mouse anti-human
hepatocyte, polyclonal rabbit anti-chromogranin (#P10645; Abgent,
Inc.) and polyclonal rabbit anti-synaptophysin (#ab14692; Abcam).
All antibodies were diluted with 1% bovine serum albumin, 0.05%
sodium azide and 0.01 M phosphate-buffered saline (pH, 7.2). All
antibodies were diluted with 1% bovine serum albumin. 0.05% sodium
azide and 0.01 M phosphate-buffered saline (pH, 7.2). Staining was
positive for HMB-45, melan A, SMA and CD34, but negative for S-100,
EMA, AFP, CK, hepatocyte, GPC-3, chromogranin and synaptophysin
(Fig. 3). Ki-67+ cells
accounted for 2%.
Discussion
In 2002, the World Health Organization recognized
PEComas as a group of neoplasms with PEC differentiation (19). PEComas include AML,
lymphangioleiomyomatosis and clear cell ‘sugar’ tumor (19). EAML is a type of AML composed almost
exclusively of epithelioid cells with pronounced abnormal blood
vessels and few or no lipocytes (20). One of the criteria for EAML in the
kidney is that epithelioid cells occupy >10% of the tumor
(21).
EAML mostly occurs in the kidney, although in rare
cases, it develops in the liver, which is known as hepatic EAML
(22). Hepatic EAML mostly affects
females (male to female ratio, ~0.4). The majority of hepatic
tumors reported in the literature are single lesions (1,6–14). In total, 4 of the patients identified
with hepatic EAML in the current literature review presented
multiple lesions, and all of them had a history of renal EAML.
Therefore, it is very likely that their hepatic tumors corresponded
to metastatic lesions that originated in the kidneys. In addition,
3 of these patients had been diagnosed as TSC with loss of
heterozygosity at TSC1 (9q34) and TSC2 (16p13), which suggests that
EAML may be associated with those genes (23).
Usually, patients with hepatic EAML are clinically
asymptomatic when the tumors are small (13,14).
However, when the tumors are very large, patients may present with
abdominal distension and pain (7,8,16). According to the present literature
review and the 3 cases reported in the current study, a tumor
measuring >5 cm in diameter may be associated with abdominal
pain, fever, weight loss and changes in bowel habits (9). The tumor diameter observed in case 3
(32.0 cm) was the largest reported thus far (10). Tumor size is also an important factor
for predicting tumor rupture (9). To
the best of our knowledge, the patient of case 3 is the 7th case of
hepatic AML rupture that has been reported in the literature to
date (11).
Imaging features of hepatic EAML vary from case to
case and may lack specificity (24).
Usually, the imaging features of the tumors are associated with
histological components (24). Thus,
the majority of reported hepatic EAML tumors were completely devoid
of adipose tissue, and fat attenuation was rarely observed in CT or
MRI images (24). By contrast, nearly
all tumors were markedly enhanced in the arterial phase, indicating
that hepatic EAML is a hypervascularized tumor (7). There are two types of enhancement
patterns in the portal venous/delayed phase (25): Lesions with abundant central vessels
exhibited a rapid contrast decrease, whereas lesions with small or
no vessels demonstrated prolonged enhancement (26). The majority of lesions exhibited a
significantly reduced contrast in the portal venous/delayed phase
(24). Accordingly, the tumor in case
2 revealed ring-enhancements in the arterial phase with a decrease
in the portal venous/delayed phase, while the margins and septa of
the tumor in case 3 were enhanced in the arterial phase and
decreased in the portal venous/delayed phase.
Immunohistochemistry is one of the most important
diagnostic tools for hepatic EAML (7,15). This
type of tumor usually displays immunoreactivity for both
melanocytic (HMB-45 and melan A) and myoid (SMA and muscle-specific
actin) markers (27). All the 3 cases
described in the present report were positive for HMB-45, melan and
SMA, but negative for hepatocyte and CK. Thus, FNAB appears to be
important for diagnosing hepatic EAML prior to surgery (17).
In conclusion, surgical resection is the first
therapeutic option for primary hepatic EAML, which should be
conducted as early as possible, due to the risks of progressive
increase and eventual rupture of the tumor. Furthermore, hepatic
EAML has a metastasis potential, particularly in patients with a
prior medical history of TSC. The responses of neoplastic hepatic
EAML to conventional chemotherapy and radiotherapy remain poorly
documented, and required to be evaluated by further clinical
trials.
References
|
1
|
Yamasaki S, Tanaka S, Fujii H, Matsumoto
T, Okuda C, Watanabe G and Suda K: Monotypic epithelioid
angiomyolipoma of the liver. Histopathology. 36:451–456. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Martignoni G, Pea M, Reghellin D, Zamboni
G and Bonetti F: PEComas: The past, the present and the future.
Virchows Arch. 452:119–132. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brown MA and Semelka RC: MRI Basic
Principles and Applications (3rd). John Wiley & Sons, Inc.
Hoboken, NJ: 2003. View Article : Google Scholar
|
|
4
|
Harris GC, McCulloch TA, Perks G and
Fisher C: Malignant perivascular epithelioid cell tumour (“PEComa”)
of soft tissue: A unique case. Am J Surg Pathol. 28:1655–1658.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lehman NL: Malignant PEComa of the skull
base. Am J Surg Pathol. 28:1230–1232. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dalle I, Sciot R, de Vos R, Aerts R, van
Damme B, Desmet V and Roskams T: Malignant angiomyolipoma of the
liver: A hitherto unreported variant. Histopathology. 36:443–450.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tryggvason G, Blöndal S, Goldin RD,
Albrechtsen J, Björnsson J and Jónasson JG: Epithelioid
angiomyolipoma of the liver: Case report and review of the
literature. APMIS. 112:612–616. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Parfitt JR, Bella AJ, Izawa JI and Wehrli
BM: Malignant neoplasm of perivascular epithelioid cells of the
liver. Arch Pathol Lab Med. 130:1219–1222. 2006.PubMed/NCBI
|
|
9
|
Occhionorelli S, Dellachiesa L, Stano R,
Cappellari L, Tartarini D, Severi S, Palini GM, Pansini GC and
Vasquez G: Spontaneous rupture of a hepatic epithelioid
angiomyolipoma: Damage control surgery. A case report. G Chir.
34:320–322. 2013.PubMed/NCBI
|
|
10
|
Zhou Y, Chen F, Jiang W, Meng Q and Wang
F: Hepatic epithelioid angiomyolipoma with an unusual pathologic
appearance: Expanding the morphologic spectrum. Int J Clin Exp
Pathol. 7:6364–6369. 2014.PubMed/NCBI
|
|
11
|
Tajima S, Suzuki A and Suzumura K:
Ruptured hepatic epithelioid angiomyolipoma: A case report and
literature review. Case Rep Oncol. 7:369–375. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dai CL, Xue LP and Li YM: Multi-slice
computed tomography manifestations of hepatic epithelioid
angiomyolipoma. World J Gastroenterol. 20:3364–3368. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Barbier L, Torrents J and Hardwigsen J:
Hepatic angiomyolipoma: What management? Acta Chir Belg.
114:139–142. 2014.PubMed/NCBI
|
|
14
|
Huang SC, Chuang HC, Chen TD, Chi CL, Ng
KF, Yeh TS and Chen TC: Alterations of the mTOR pathway in hepatic
angiomyolipoma with emphasis on the epithelioid variant and loss of
heterogeneity of TSC1/TSC2. Histopathology. 66:695–705. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mai KT, Yazdi HM, Perkins DG and Thijssen
A: Fine needle aspiration biopsy of epithelioid angiomyolipoma. A
case report. Acta Cytol. 45:233–236. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Alatassi H and Sahoo S: Epithelioid
angiomyolipoma of the liver with striking giant cell component:
Fine-needle aspiration biopsy findings of a rare neoplasm. Diagn
Cytopathol. 37:192–194. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xie L, Jessurun J, Manivel JC and
Pambuccian SE: Hepatic epithelioid angiomyolipoma with trabecular
growth pattern: A mimic of hepatocellular carcinoma on fine needle
aspiration cytology. Diagn Cytopathol. 40:639–650. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hino A, Hirokawa M, Takamura K and Sano T:
Imprint cytology of epithelioid angiomyolipoma in a patient with
tuberous sclerosis. A case report. Acta Cytol. 46:545–549. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hornick JL and Fletcher CD: PEComa: What
do we know so far? Histopathology. 48:75–82. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mai KT, Perkins DG and Collins JP:
Epithelioid cell variant of renal angiomyolipoma. Histopathology.
28:277–280. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Aydin H, Magi-Galluzzi C, Lane BR, Sercia
L, Lopez JI, Rini BI and Zhou M: Renal angiomyolipoma:
Clinicopathologic study of 194 cases with emphasis on the
epithelioid histology and tuberous sclerosis association. Am J Surg
Pathol. 33:289–297. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Eble JN: Angiomyolipoma of kidney. Semin
Diagn Pathol. 15:21–40. 1998.PubMed/NCBI
|
|
23
|
Ooi SM, Vivian JB and Cohen RJ: The use of
the Ki-67 marker in the pathological diagnosis of the epithelioid
variant of renal angiomyolipoma. Int Urol Nephrol. 41:559–565.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ji JS, Lu CY, Wang ZF, Xu M and Song JJ:
Epithelioid angiomyolipoma of the liver: CT and MRI features. Abdom
Imaging. 38:309–314. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Xu PJ, Shan Y, Yan FH, Ji Y, Ding Y and
Zhou ML: Epithelioid angiomyolipoma of the liver: Cross-sectional
imaging findings of 10 immunohistochemically-verified cases. World
J Gastroenterol. 15:4576–4581. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xiao W, Zhou M, Lou H, Wang Z and Zhang M:
Hemodynamic characterization of hepatic angiomyolipoma with least
amount of fat evaluated by contrast-enhanced magnetic resonance
angiography. Abdom Imaging. 35:203–207. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Park HK, Zhang S, Wong MK and Kim HL:
Clinical presentation of epithelioid angiomyolipoma. Int J Urol.
14:21–25. 2007. View Article : Google Scholar : PubMed/NCBI
|