Introduction
Radiation cystitis frequently occurs following
radiotherapy treatment for cervical, colorectal and prostate
cancer, in addition to other pelvic tumors, with an incidence rate
of ≤5% of all patients that undergo radiotherapy (1). Previous studies have reported that acute
radiation cystitis, which typically develops 2–4 weeks after
radiotherapy with a severity of <II [Radiation Therapy Oncology
Group staging system (2)], occurs in
21–25% of all patients that undergo radiotherapy, while chronic
radiation cystitis has an incidence rate of 1% (3). The occurrence and severity of radiation
cystitis has gradually decreased due to technical advances in the
field of radiotherapy (4). To the
best of our knowledge, the occurrence of a peritoneal bladder
fistula as a result of radiation cystitis following radiotherapy
for cervical cancer has not been reported in the literature. The
present study reports a case of a peritoneal bladder fistula, which
occurred 20 years after the administration of radiotherapy for
cervical cancer, and discusses the possible causes and potential
treatments for this condition.
Case report
A 50-year-old woman, who was previously diagnosed
with cervical cancer and treated with radiotherapy 20 years ago in
June 1994, was admitted to the First Affiliated Hospital of Xi'an
Jiatong University (Xi'an, China). No recurrence or metastasis was
observed during the periodic examinations that followed the
diagnosis. The patient began experiencing intermittent increased
urination frequency, urination urgency and hematuria 10 years ago,
and was subsequently treated with Chinese medicine for 1 year,
which alleviated the symptoms. However, 3 years ago, the patient
experienced sudden abdominal pain and bowel difficulties following
urination. B-ultrasound examination at The People's Hospital of
Tongchuan (Tongchuan, China) detected the presence of abdominal
pelvic fluid. Following antibiotic (levofloxacin for 5 days) and
ascites extraction treatment, symptoms were relieved without any
recurrence. Five days prior to admission to the First Affiliated
Hospital of Xi'an Jiatong University on June 25, 2014, the patient
experienced difficulty urinating, abdominal pain and bloating, but
did not experience frequent urination, hematuria or fever.
B-ultrasound examination indicated a rough bladder wall and a large
pelvic effusion. Laboratory examinations performed 5 days prior to
admission revealed mild urinary occult blood, severe urinary
protein, blood urea nitrogen (BUN) levels of 12.34 mmol/l and
creatinine (CREA) levels of 268 umol/l. Further examinations
revealed that blood pressure, heart rate, temperature and chest
X-ray were all normal, in addition to abdominal tension, no
tenderness or rebound tenderness, no liver or spleen palpation, no
percussion pain in the kidney area, positive shifting dullness and
normal bowel sounds. Gynecological examination was normal. The
diagnosis at admission was suspected as i) ascites of unknown
reason and ii) cervical cancer. Routine blood and liver function
tests following admission were normal, and tumor marker levels,
including cancer antigen (CA)125, CA153, CA199, carcinoembryonic
antigen and squamous cell carcinoma antigen, were also normal.
Chest and abdominal computed tomography and pelvic magnetic
resonance imaging examination excluded tumor recurrence and
metastasis. BUN and CREA levels in ascites, blood and urine were
tested following hospital admission and are presented in Table I. Routine biochemical tests were
performed for ascites and urine, which indicated that the ascitic
fluid was transudate (Tables II and
III). Pathological examination of
ascites revealed the presence of mesothelial cells and lymphocytes;
however, no malignant tumor cells were identified. Therefore, a
peritoneal bladder fistula was suspected and urine ascites were
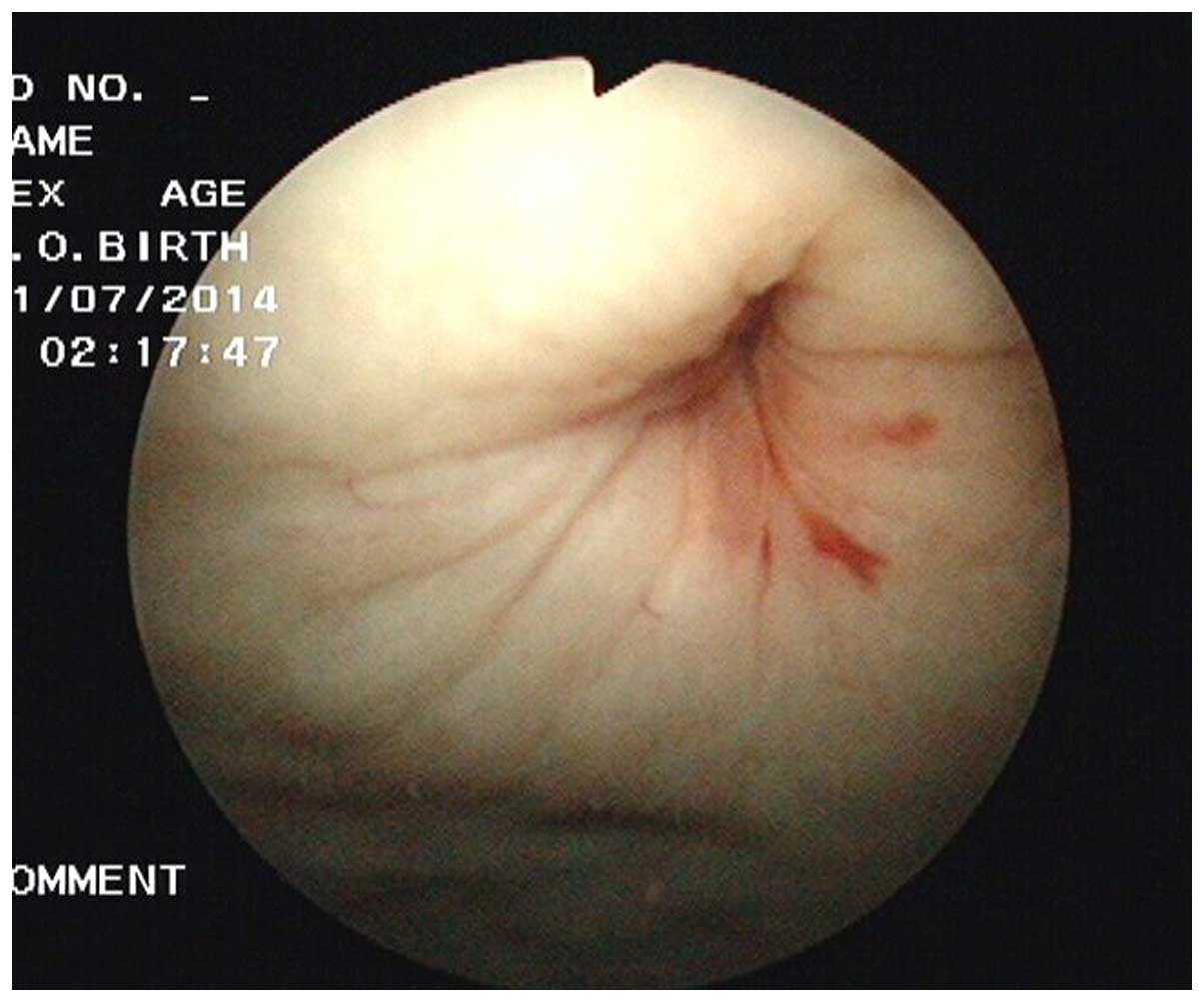
subsequently obtained. Cystoscopic examination revealed pale and
thick bladder mucosa, vascular thickening and the formation of a
visible fistula on the bladder wall measuring 1×1 cm in diameter
(Fig. 1). The preliminary diagnosis
was the presence of a peritoneal bladder fistula with radiation
cystitis. Following catheterization and ascites extraction, the
symptoms were relieved and the blood BUN and CREA levels had
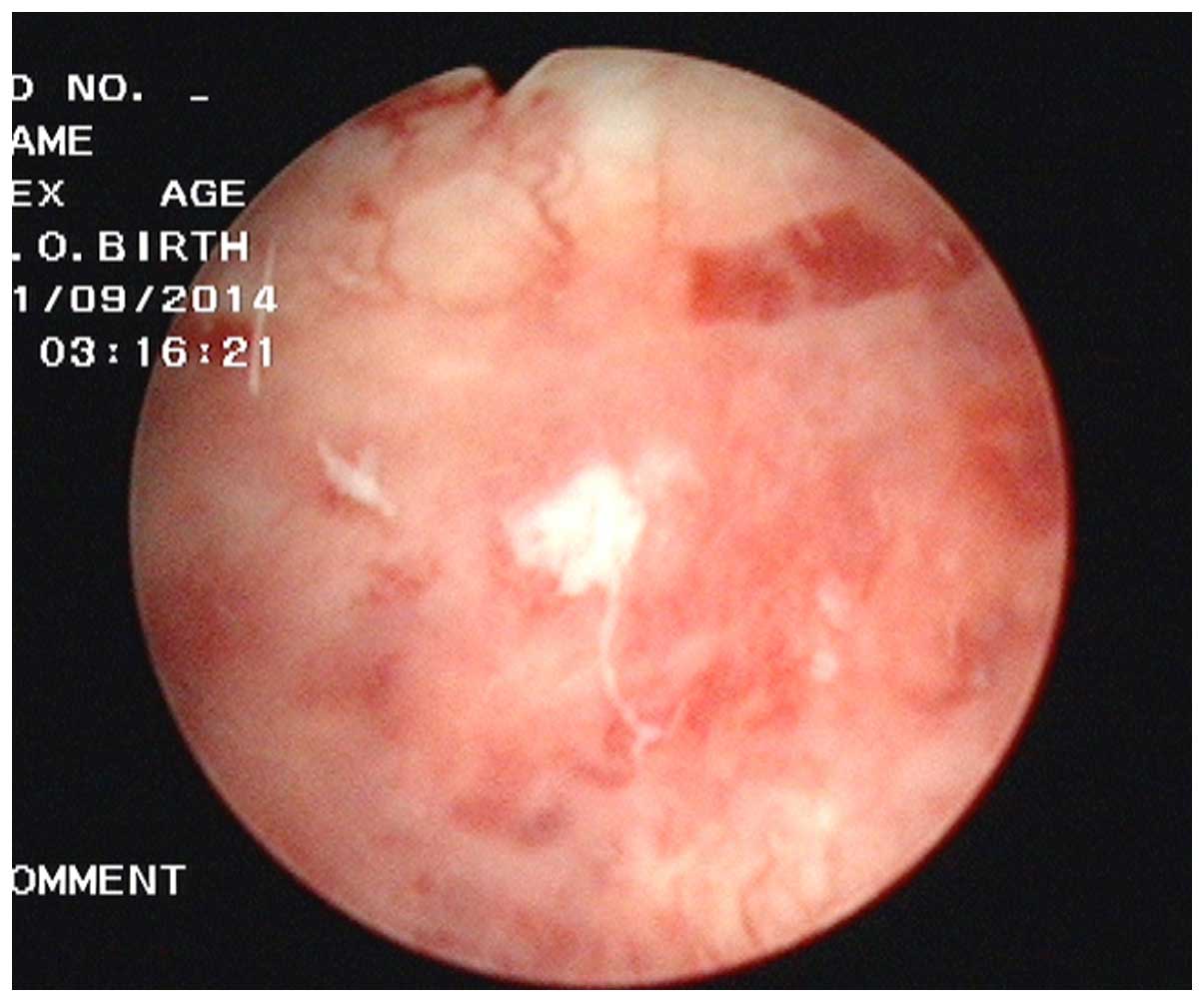
reduced to 6.4 mmol/l and 166 umol/l, respectively. Cytoscopic
examination 1 month later revealed no evidence of the fistula
(Fig. 2). The final diagnosis was
confirmed as a peritoneal bladder fistula as a result of
radiotherapy for cervical cancer. The patient was followed up
everyday 3 months for a year and a half, and is currently alive and
well.
 | Table I.Patient BUN and CREA levels in the
blood, urine and ascites following hospital admission. |
Table I.
Patient BUN and CREA levels in the
blood, urine and ascites following hospital admission.
|
| Blood (normal
range) | Urine | Ascites |
|---|
| BUN, mmol/l | 18.53
(2.60–7.50) | 72.24 | 31.05 |
| CREA, mmol/l |
288
(41.00–73.00) | 12124 | 1371 |
 | Table II.Examination results for ascites and
urine. |
Table II.
Examination results for ascites and
urine.
| Parameters | Ascites | Urine |
|---|
| Color | Light yellow | Light yellow |
| Transparency | Transparent | Transparent |
| Clot | No clot | No clot |
| Rivalta test | Negative | Negative |
| Total cells |
72×106/l |
21×106/l |
| White blood
cells |
38×106/l |
11×106/l |
 | Table III.Biochemical test results for ascites
and urine. |
Table III.
Biochemical test results for ascites
and urine.
| Biochemical
parameters | Ascites | Urine |
|---|
| Total protein,
g/l | 7.53 (<40) | 3.02 (60–80) |
| Glucose, mmol/l | 9.15 (3.60–6.10) | 3.14 (3.60–6.10) |
| Lactate
dehydrogenase, U/l | 40.6 (109–245) | 32.2 (109–245) |
| Chlorine, mmol/l | 96.9 (96–108) | 35.6 (96–108) |
| Adenosine deaminase,
U/l | 0.7
(<20) |
0 (<20) |
Discussion
Radiation cystitis typically affects the trigone of
the urinary bladder and the surrounding tissues (5). Generally, the tolerated radiation dose
of the bladder is considered to be 60 Gy; therefore, radiation
cystitis may occur if the dose exceeds this. A previous study
reported that radiation cystitis develops after receiving a dose
that is 10% higher than the regular dose (60 Gy) (6,7). The
primary pathological symptoms of radiation cystitis include ulcers
accompanied by bleeding, inflammatory cell infiltration and
epithelial cell atrophy or hyperplasia (8). Biopsies of bladder tissues exhibiting
radiation cystitis usually demonstrate shedding of bladder
transitional epithelial cells and cellulose inflammatory exudates.
Necrotic tissue below the epithelium is also often observed, in
addition to a thin layer of granulation containing numerous
thin-walled blood vessels and fibrous tissue hyperplasia with
hyaline degeneration, which involves the muscular layer and the
outer membrane (9). Shedding of
bladder epithelial mucosal cells results in the loss of epithelial
protection and the permeability barrier (9). Consequently, extensive amounts of water
and urea permeate into the smooth muscle layer of the bladder,
resulting in nerve hyperexcitability, detrusor muscle dysfunction
and sudden, painless hematuria associated with bladder irritation
(9).
Radiation cystitis may be divided into three types
according to the time of occurrence and severity: Acute radiation
cystitis, chronic radiation cystitis and radiation bladder fistula
(10). Acute radiation cystitis
usually occurs within 6 months of radiotherapy and is characterized
by gross or microscopic hematuria associated with urinary tract
irritation symptoms, including increased urinary frequency and
urgency. These symptoms may be relieved when radiotherapy is
terminated or following relevant treatment (11). Chronic radiation cystitis accounts for
80% of cases of radiation cystitis and usually occurs 2–4 years
after radiotherapy due to the delayed healing of acute radiation
cystitis or late stage radiation injuries (11). Radiation bladder fistulas present
further development of chronic radiation cystitis. Obstetric
fistulas are the most common, while peritoneal bladder fistulas are
rare (12). Radiation bladder
fistulas are associated with the distribution of the radiation dose
(5). The trigone of the urinary
bladder receives the highest radiation doses during pelvic
radiotherapy; therefore, radiation cystitis and obstetric fistulas
usually occur in this region (5). To
the best of our knowledge, no cases of peritoneal bladder fistulas
as a result of radiotherapy have been reported previously. The
primary causes of bladder fistulas are trauma, surgery, tumors and
radiotherapy, and surgery is the standard treatment option
(13).
In the present study, a peritoneal bladder fistula
occurred as a result of radiotherapy, bladder cystitis and
excessive urinary holding. Long-term radiation bladder cystitis
leads to fibrosis of bladder mucosa and a reduction in bladder wall
tension. Therefore, sudden increases in bladder capacity and wall
tension may result in rupture. Notably, the rupture observed in the
patient of the present study was not located in the trigone of the
urinary bladder and was instead located in the back wall of the
bladder, thus resulting in the development of a peritoneal bladder
fistula and leakage of urine into the peritoneal cavity. In the
early stages of the disease, catheterization and other symptomatic
treatments, including hemostasis, anti-inflammatory and sodium
hyaluronate treatment, may heal the fistula via bladder self-repair
(13). However, in patients with
delayed healing, long-term stimulation of the peritoneum by urine
may result in abdominal pain and infection, and life-threatening
infectious peritonitis. The present case demonstrates that urinary
holding must be avoided in patients with a history of pelvic
radiotherapy as it may lead to the formation of a bladder fistula.
In addition, patients with sudden urinary difficulties and ascites
following radiotherapy must be monitored for the development of
peritoneal bladder fistulas. Cystoscopy is the preferred method of
examination and diagnosis, and early detection and treatment may
significantly improve the patient prognosis.
In conclusion, the occurrence of peritoneal bladder
fistulas following radiation therapy is rare and may easily be
misdiagnosed as peritoneal metastasis with ascites. If a patient
that has undergone abdominal or pelvic radiotherapy and been
diagnosed with chronic radiation cystitis experiences sudden
abdominal pain, severe unexplained ascites and dysuria, the
possibility of a peritoneal bladder fistula should be considered.
Early cystoscopic examination and timely treatment may
significantly improve the prognosis.
References
|
1
|
Liem X, Saad F and Delouya G: A practical
approach to the management of radiation induced hemorrhagic
cystitis. Drugs. 75:1471–1482. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cox JD, Stetz J and Pajak TK: Toxicity
criteria of the Radiation Therapy Oncology Group (RTOG) and the
European Organization for Research and Treatment of Cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Coman JM, Mcclure D, Pritchett R,
Kozlowski P and Hampson NB: Treatment of radiation induced
hemorrhagic cystitis with hyperbaric oxygen. J Urol. 169:2200–2202.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wit EM and Horenblas S: Urological
complications after treatment of cervical cancer. Nat Rev Urol.
11:110–117. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pourquier H, Delard R, Achille E, Daly NJ,
Horiot JC, Keiling R, Pigneux J, Rozan R, Schraub S and Vrousos C:
A quantified approach to the analysis and prevention of urinary
complications in radiotherapeutic treatment of cancer of the
cervix. A quantified approach to the analysis and prevention of
urinary complications in radiotherapeutic treatment of cancer of
the cervix. 13:1025–1033. 1987.
|
|
6
|
Appelt AL, Bentzen SM, Jakobsen A and
Vogelius IR: Dose-response of acute urinary toxicity of long course
preoperative chemoradiotherapy for rectal cancer. Acta Oncol.
54:179–186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rosewall T, Catton C, Currie G, Bayley A,
Chung P, Wheat J and Milosevic M: The relationship between external
beam radiotherapy dose and chronic urinary dysfunction - a
methodological critique. Radiother Oncol. 97:40–47. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kanai A, Epperly M, Pearce L, Birder L,
Zeidel M, Meyers S, Greenberger J, de Groat W, Apodaca G and
Peterson J: Differing roles of mitochondrial nitric oxide synthase
in cardiomyocytes and urothelial cells. Am J Physiol Heart Circ
Physiol. 286:H13–H21. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li A, Sun J and Chao H: Late bladder
complications following radiotherapy of carcinoma of the uterine
cervix. Zhonghua Fu Chan Ke Za Zhi. 30:741–743. 1995.(In Chinese).
PubMed/NCBI
|
|
10
|
Brzozowska A, Idziak M, Burdan F and
Mazurkiewicz M: Symptoms and treatment of radiation-induced
reactions. Pol Merkur Lekarski. 38:283–287. 2015.(In Polish).
PubMed/NCBI
|
|
11
|
Tasdemir N, Abali R, Celik C, Yazici CM
and Akkus D: The use of an anterior abdominal wall peritoneal flap
in the laparoscopic repair of vesicouterine fistula. Int Surg.
99:673–676. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Iloabachie GC and Njoku O: Vesico-uterine
fistula. Br J Urol. 57:438–439. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chuang YC, Kim DK, Chiang PH and
Chancellor MB: Bladder botulinum toxin A injection can benefit
patients with radiation and chemical cystitis. BJU Int.
102:704–706. 2008. View Article : Google Scholar : PubMed/NCBI
|