Introduction
Extragonadal germ cell tumours (EGCTs) mostly
originate from primordial germ cell or thymus cells which may
transform to germ cells, accounting for 2–5% of all germ cell
tumours (1). EGCTs are further
differentiated into seminoma, non-seminoma and mixed-cell tumours.
Seminoma is the most common type of EGCT, and all three types are
treated using radiotherapy and chemotherapy-based comprehensive
treatments. EGCTs mostly present in the medial side of the body,
including the mediastinum and retroperitoneum (2). Primary mediastinal seminoma is a rare
extragonadal germ cell tumour that mainly occurs in males (3). Primary mediastinal seminoma commonly
occurs in the anterior mediastinum of men with an average age of 33
years, and it is rarely observed in women. The incidence rate of
primary mediastinal seminoma accounts for 1–4% of mediastinal
tumors (4). As primary mediastinal
seminoma is a highly radiosensitive tumour, radiotherapy is
currently considered to be the most important means of treatment,
though chemotherapy may also be used (4).
Case report
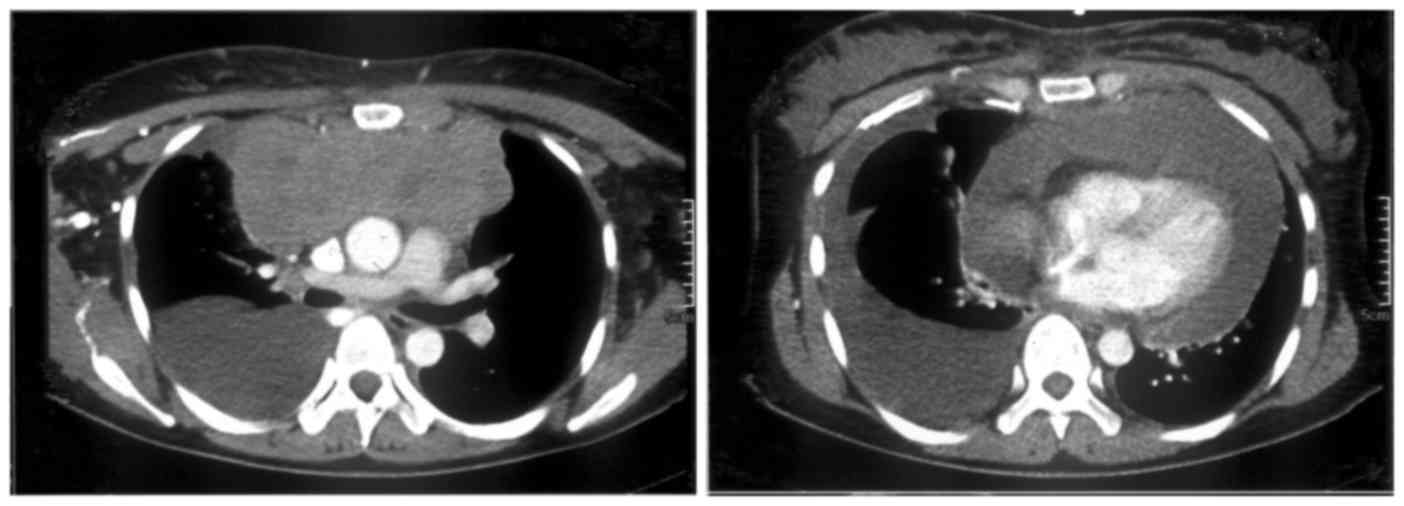
In November 2008, a 27-year-old woman presented at
The Second Xiangya Hospital of Central South University (Changsha,
China) with the signs and symptoms of superior vena cava syndrome
(swollen neck), which had been present for 10 days, and was
admitted to the present department. The patient had given birth 2
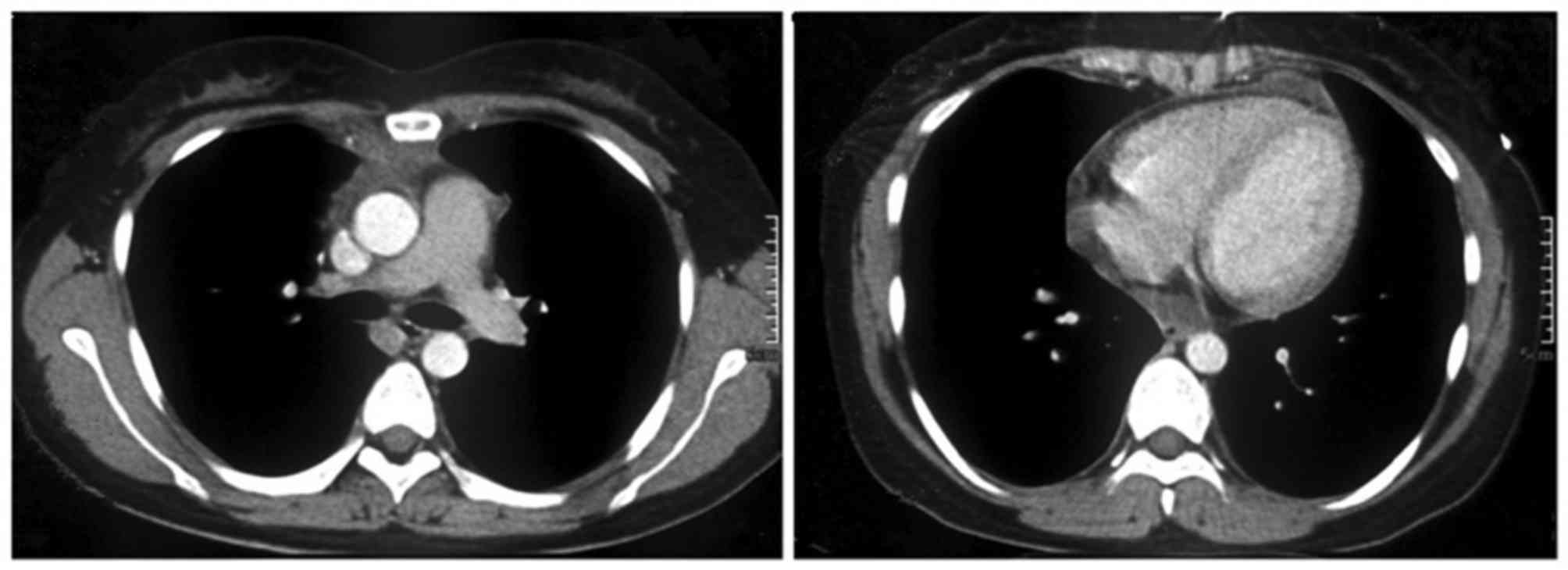
months prior to presentation. CT (Siemens) revealed a 12×6-cm mass
in the anterior mediastinum, and water density shadow was observed
inside the thickened pericardium (Fig.
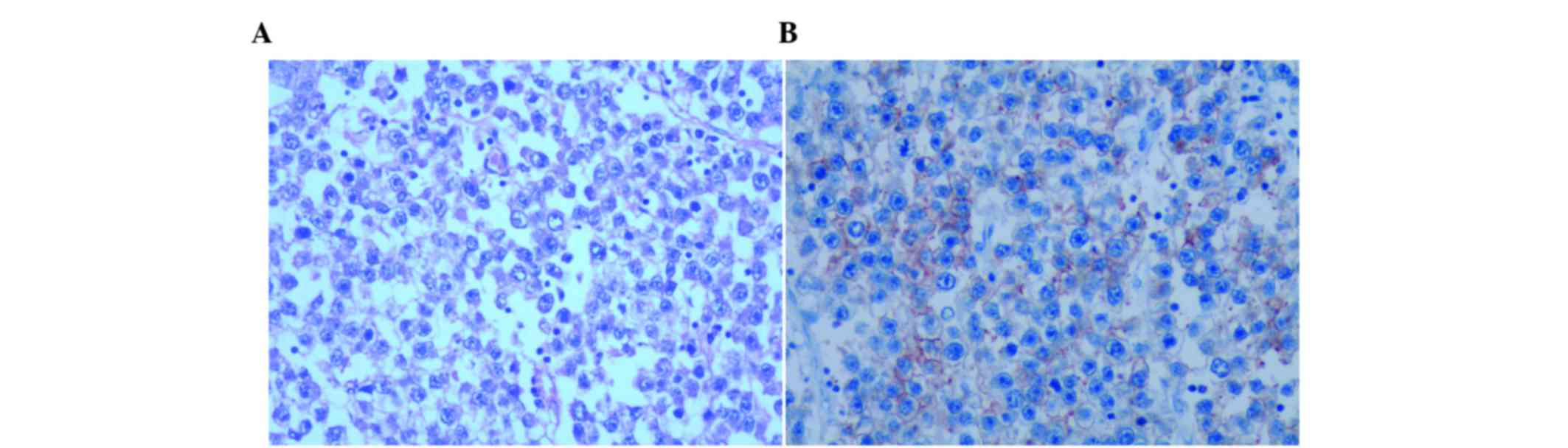
1). Examination of the mediastinal mass biopsy (prepared using
a BARD biopsy gun; Bard Company, Murray Hill, NJ, USA) in December
2008 revealed distributed macro-nucleic cells under microscope
(N-117M CKX41; Olympus Corporation, Tokyo, Japan), with the
following immunohistochemical findings: Strong expression of
placental alkaline phosphatase (PLAP); expression of cluster of
differentiation (CD)3 (dilution, 1:100; GD-x0297M-AF03; Abcam,
Cambridge, UK), CD45 (dilution, 1:100; GD-x0297M-AF20; Abcam) and
CD20 (dilution, 1:100; GD-x0297M-AF20; Abcam); and no expression of
CD79a (dilution, 1:100; GD-x0297M-AF79a), cytokeratin (dilution,
1:500; GD-cyt-001; Abcam), S100 (dilution, 1:100; GD-S-100; Abcam),
terminal deoxynucleotidyl transferase (dilution, 1:200; GD-te-001;
Abcam), CD5 (dilution, 1:100; GD-x0297M-AF05; Abcam), CD30
(dilution, 1:100; GD-x0297M-AF30; Abcam), CD15 (dilution, 1:100;
GD-x0297M-AF15; Abcam), anaplastic lymphoma kinase (dilution,
1:500; GD-ana-001; Abcam), B cell lymphoma-2 (dilution, 1:100;
GD-bcl-005; Abcam) and CD10 (dilution, 1:100; GD-x097M-AF10; Abcam)
(Fig. 2). These findings were
consistent with the diagnosis of primary mediastinal seminoma and
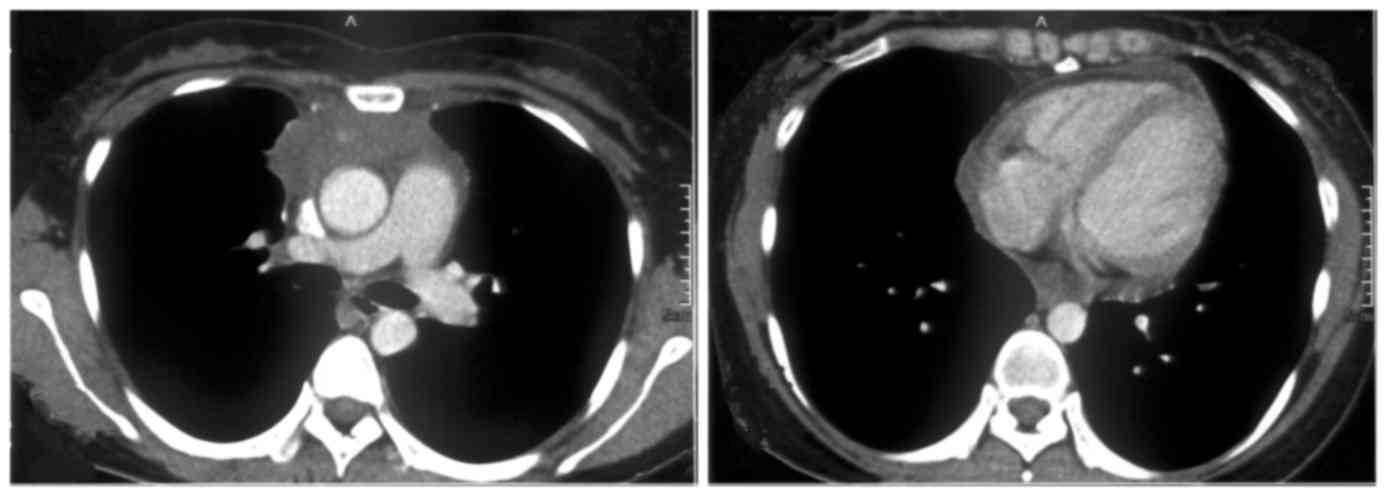
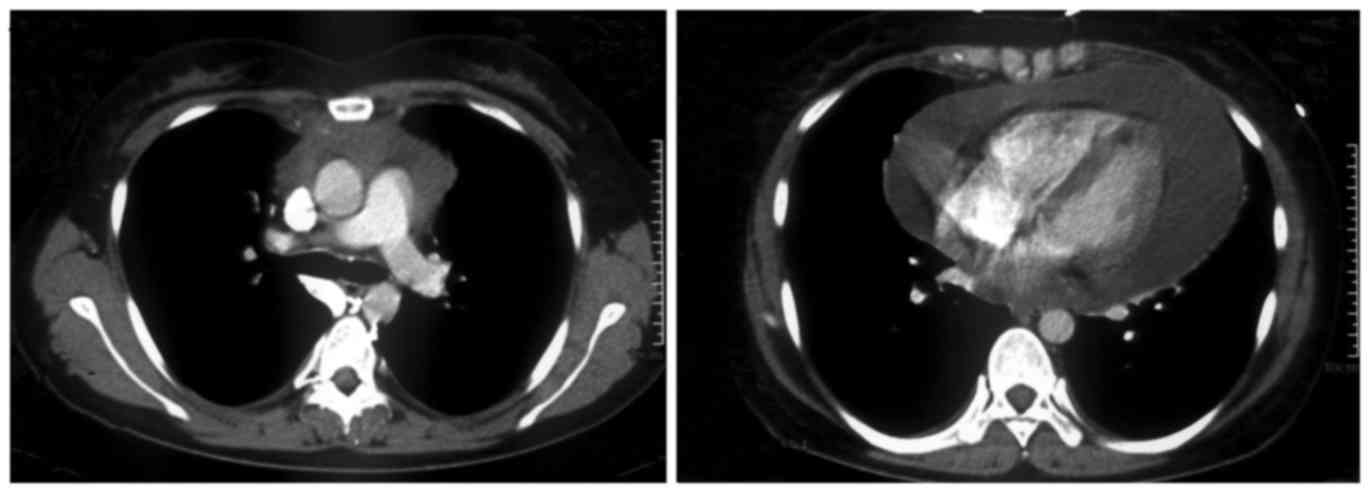
stage IV disease. The patient was administered with 2 cycles of the
bleomycin, etoposide and cisplatin (BEP) chemotherapy regimen (120
mg cisplatin, 0.45 g etoposide and 60 mg bleomycin, once every 3
weeks). CT re-examination showed a distinctly reduced mediastinum
mass size, decreased pericardial effusion and disappearance of the
right mediastinal exudates (Fig. 3).
The BEP regimen was prolonged with the same dosages for an
additional 2 cycles. CT re-examination showed mild shrinkage of the
mediastinal mass, but pericardial effusion had increased (Fig. 4). Thus, the chemotherapy regimen was
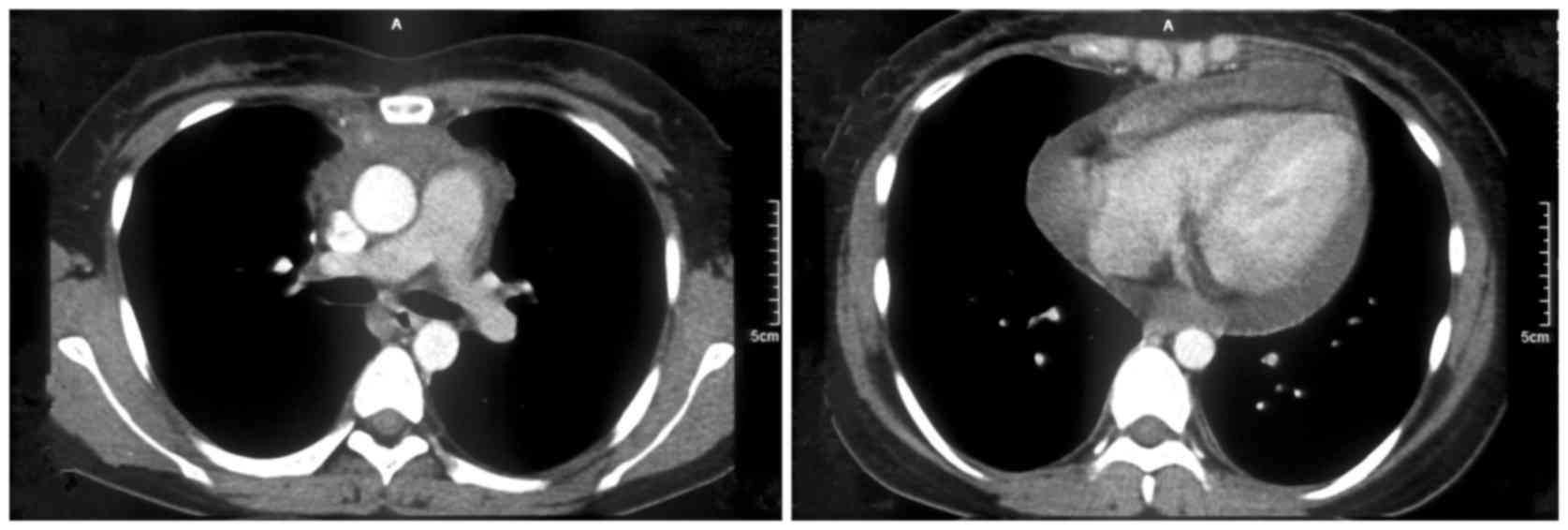
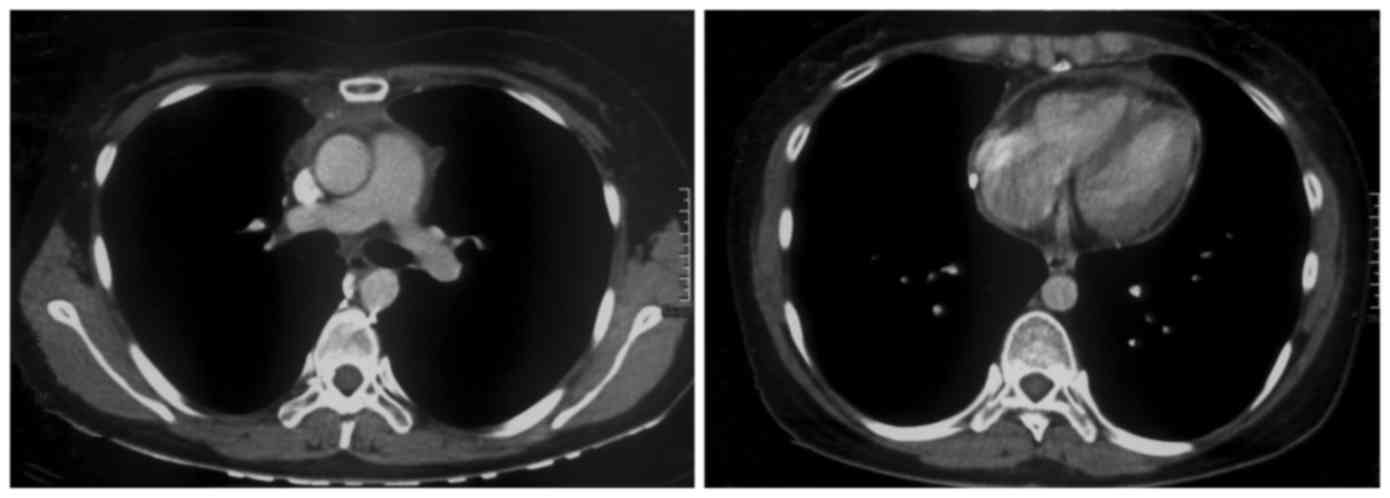
revised to the iphosphamide, epirubicin and cisplatin regimen. CT
re-examination (Fig. 5) shows that
the mediastinal mass had decreased in size again, with reduced
pericardial effusion, considering the treatment efficacy the
regimen was prolonged. Another CT re-examination was performed 3
weeks subsequently, which showed the advancement of disease with an
enlarged mediastinal mass and increased volume of pericardial
effusion (Fig. 6). The patient was
administered with intensity-modulated radiotherapy therapy from
June 2008. A dose of 50 Gy/18 fractions was administered to the
upper mediastinum and a dose of 30 Gy/18 fractions was administered
to the pericardial area. Pericardiocentesis was performed
post-radiotherapy, which drained 700 ml of red fluid, together with
the infusion of 1 g fluorouracil. Post-radiotherapy CT examination
showed that the mediastinal mass had disappeared, with a mild
amount of pericardial effusion (Fig.
7). For 5 years subsequent to treatment, to the present time,
there has been no relapse of the tumour and the patient is leading
a normal life.
Discussion
In 2004, the World Health Organization defined
mediastinal seminoma as a type of extragonadal low-grade malignant
germ cell tumour that commonly occurs in the anterior mediastinum
of men, with the average age of 33 years, and it is rarely observed
in women (4). The clinical data show
that primary mediastinal seminoma accounts for 0.5–5% of all
mediastinal tumours (5).
Clinical records show that the most common clinical
symptoms of primary mediastinal seminoma include chest pain,
dyspnoea and hoarseness of voice (1).
In the majority of cases, CT shows heterogeneously distributed
density of the mediastinal mass (6).
Monitoring of serum tumour markers is significantly important for
the diagnosis and prognostic evaluation of patients with
mediastinal seminoma. According to the 2010 American Society of
Clinical Oncology clinical guidelines, increased levels of
biomarkers such as HCG, LDH and AFP should determine the presence
of relapse or metastasis of the disease (7). In addition, 80–90% of mediastinal
seminoma cases are found to be PLAP-positive by
immunohistochemistry (2). The
diagnosis of primary mediastinal seminoma in the present patient
was confirmed by the clinical presentation, CT and the
morphological appearance of the tumour. In addition,
immunohistochemical analysis was performed for PLAP, CD3, CD20 and
CD45, all of which were found to be expressed.
Among mediastinal tumours, seminoma is a highly
radiosensitive tumour, and therefore long-term radiotherapy is
considered the most important means of treatment and increases the
long-term survival rate of patients by 60–80% (8). Patients administered with platinum-based
chemotherapy had an overall long-term survival rate of 90%. At
present, the most commonly accepted treatment methods for
mediastinal seminoma may be classified as two types. Radiotherapy
is used if patients develop post-chemotherapeutic local recurrence
and remnant lesions and surgery is used in patients with
post-chemotherapeutic remnant lesions >3 cm in size.
In the present case, there was recurrent relapse of
the disease and the case was unique as the patient was female. The
chemotherapeutic effect varies between men with primary mediastinal
seminoma (9). Another explanation is
that the patient was diagnosed with mediastinal seminoma through
biopsy. However, the pathological biopsy specimen was small, and
the tumour may have contained non-seminomatous germ cell tumour
type cells, which were not biopsied. In addition, mixed-type
gonadal cell tumours account for 13–34% of mediastinal tumours and
they are less sensitive to chemotherapy compared with cases of
seminoma (2). The present patient had
large amounts of pericardial effusion, which is a contraindication
for radiotherapy. However, considering that the patient was
resistant to chemotherapy and the challenging nature of surgery due
to extensive invasion, with no significant cardiac compression
symptoms, such as dyspnoea or shock, the patient was advised to
undergo radiotherapy. Subsequent to the aforementioned treatments
the patient did not experience any relapse or metastasis during the
5 years of follow-up.
Thus, the present study shows that various
comprehensive treatment methods should be used for the effective
treatment of mediastinal seminoma. Although radiotherapy is
contraindicated in pericardial effusion, the present study
indicates that it could be considered if there are no other means
of treatment and with no evident signs of cardiac compression.
References
|
1
|
Hsu YJ, Pai L, Chen YC, Ho CL, Kao WY and
Chao TY: Extragonadal germ cell tumors in Taiwan: An analysis of
treatment results of 59 patients. Cancer. 95:766–774. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wick MR, Perlman EJ, Orazi A,
Müller-Hermelink HK, Zettl A, Göbel U, Bokemeyer C, Hartmann JT and
Marx A: Germ cell tumors of the mediastinum. World Health
Organization Classification of TumoursPathology and Genetics of
Tumours of the Lung, Pleura, Thymus and Heart. Travis WD, Brambilla
E, Müller-Hermelink HK and Harris CC: IARC Press; Lyon: pp.
198–219. 2004
|
|
3
|
Moran CA and Suster S: Primary germ cell
tumors of the mediastinum: I. Analysis of 322 cases with special
emphasis on teratomatous lesions and a proposal for histopathologic
classification and clinical staging. Cancer. 80:681–690. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schrader M, Kempkensteffen C, Christoph F,
Hinz S, Weikert S, Lein M, Krause H, Stephan C, Jung K, Hoepfner M,
et al: Germ cell tumors of the gonads: A selective review
emphasizing problems in drug resistance and current therapy
options. Oncology. 76:77–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Iwasa S, Ando M, Ono M, Hirata T, Yunokawa
M, Nakano E, Yonemori K, Kouno T, Shimizu C, Tamura K, et al:
Relapse with malignant transformation after chemotherapy for
primary mediastinal seminoma: Case report. Jpn J Clin Oncol.
39:456–459. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Xu X, Sun C, Zhang L and Liang J: A case
of mediastinal seminoma presenting as superior vena cava syndrome.
Intern Med. 51:1269–1272. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gilligan TD, Hayes DF, Seidenfeld J and
Temin S: ASCO clinical practice guideline on uses of serum tumor
markers in adult males with germ cell tumors. J Oncol Pract.
6:199–202. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Feldman DR, Patil S, Trinos MJ, Carousso
M, Ginsberg MS, Sheinfeld J, Bajorin DF, Bosl GJ and Motzer RJ:
Progression-free and overall survival in patients with
relapsed/refractory germ cell tumors treated with single-agent
chemotherapy: Endpoints for clinical trial design. Cancer.
118:981–986. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu TZ, Zhang DS, Liang Y, Zhou NN, Gao
HF, Liu KJ and Wu HY: Treatment strategies and prognostic factors
of patients with primary germ cell tumors in the mediastinum. J
Cancer Res Clin Oncol. 137:1607–1612. 2011. View Article : Google Scholar : PubMed/NCBI
|