Introduction
Anaplastic lymphoma kinase (ALK)-positive large
B-cell lymphoma (LBCL) is a rare variant of diffuse large B-cell
lymphoma (DLBCL) with an incidence of ≥1% of DLBCL (1). It was originally described by Delsol
et al (2) in 1997, and only
<60 cases have been identified to date (3–5). It is
charac terized by a sinusoidal growth pattern and was composed of a
monomorphic population of large immunoblast-like or
plasmablast-like cells, marked ALK/epithelial membrane antigen
(EMA) protein expression, lack of CD20 expression and an aggressive
clinical course (3). Despite this
subtype of lymphoma being recognized in the 2008 World Health
Organization classification (1), its
identification in routine pathology laboratories remains
challenging, particularly in differential diagnosis among
ALK-positive ALCL of null cell lineage and poorly differentiated
anaplastic carcinoma (1). Recognition
of this variant of DLBCL is important as the conventional therapy
used for typical DLBCL is of limited efficacy in this disease
phenotype. Novel front-line intensive chemotherapy regimens should
be evaluated in this group of patients.
Cluster of differentiation (CD)4 is normally a T
helper cell-associated antigen, which is expressed in mature T-cell
and natural killer cell lymphomas (1), but it has also been observed in certain
ALK-positive LBCL cases (3).
Pan-cytokeratin (CK) is a useful biomarker for epithelial cells,
which has been observed in certain lymphomas, including
ALK-positive LBCLs (3,6–8), and this
may result in misdiagnosis. In the present study, a relapsed case
of ALK-positive LBCL with unusual expression levels of CD4 and CK
were observed, which appeared positive in the relapsed lesion.
Case report
Description of the case
A 28-year-old Chinese male presented with a
submaxillary mass 4.0 cm in diameter in February 2011. The patient
then suffered from a progressive enlargement of cervical nodes for
5 months without exhibiting any systemic symptoms. He received his
treatment in the Peking University Cancer Hospital (Beijing,
China), and a computed tomography (CT) scan revealed cervical,
submaxillary and submentum lymphadenopathy. An excisional biopsy of
the right cervical lymph node was performed prior to diagnosis as
ALK-positive anaplastic large cell lymphoma (ALCL) and the
patient's clinical stage was classified as IIB. The patient
underwent 6 cycles of cyclophosphamide, doxorubicin, vincristine
and prednisolone (CHOP). The restaging CT scan revealed complete
remission following treatment. In May 2014, a solitary enlarged
cervical lymph node was detected by a thorough examination and was
surgically biopsied and it was again pathologically diagnosed as
ALK-positive ALCL. A follow-up investigation was performed and the
CT scan indicated that it was a progressive disease. The patient
subsequently underwent 2 cycles of dexamethasone, ifosfamide,
carboplatin and etoposide followed by autologous stem cell
transplantation using cyclophosphamide, doxorubicin and vincristine
treatment as a high-dose therapy regimen in January 2015. The
disease relapsed again 6 weeks post-transplantation. A CT scan
revealed a bulky mediastinal mass with axillary, supraclavicular,
bilateral cervical and retroperitoneal lymphadenopathy, the
patient's left breast and liver were also possibly involved. A core
biopsy was performed, which revealed ALK-positive ALCL. The patient
finally succumbed to the disease owing to respiratory failure in
April 2015. A revision of the previous pathological diagnosis was
performed as requested by the oncologist and the final diagnosis
was ALK-positive LBLC with complex ALK gene rearrangements, CD4
continuously expressed and CK observed in the tumor specimen. These
phenotypes were difficult for the pathologists to identify.
Histological and immunohistochemical
(IHC) results
Paraffin-embedded samples from the two excisions and
the final core biopsies were obtained and cut into 5-µm thick
sections, then deparaffinized in xylene and rehydrated. The routine
hematoxylin and eosin stains were then carried out for histological
review under light microscope (Olympus X51; Olympus, Watford, UK),
lymph node demonstrated a complete effacement of the normal
structure by the diffuse proliferation of large neoplastic cells.
Tumor cells proliferated in sheets and infiltrated sinuses
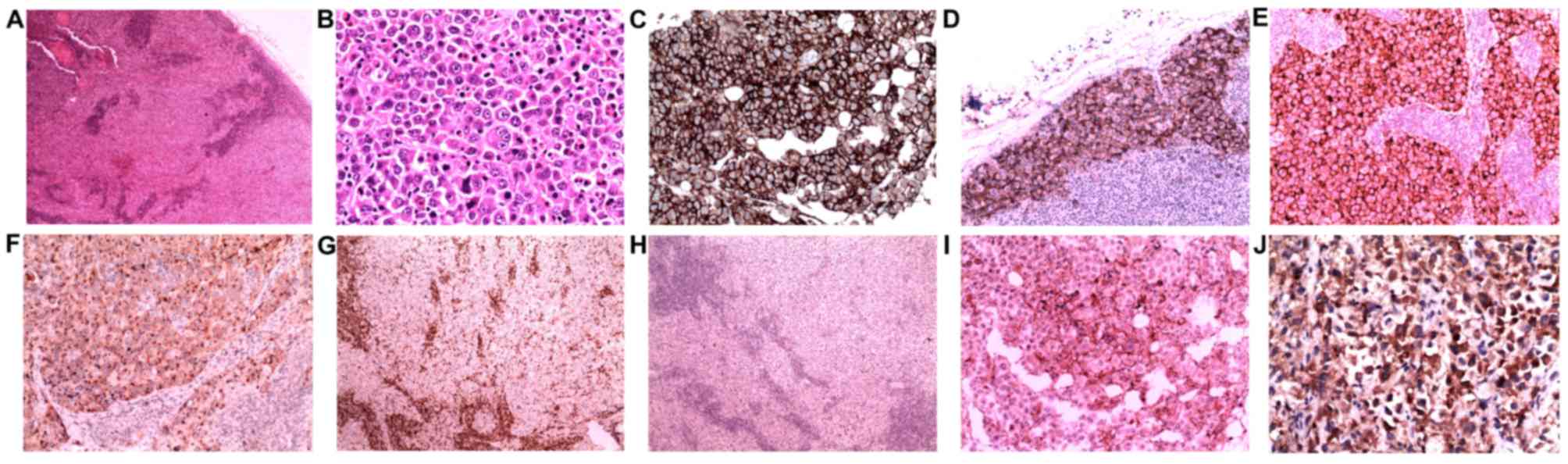
(Fig. 1A) in certain regions.
Atypical tumor cells were observed with immunoblastic features
(round pale nuclei, large prominent nucleoli and abundant
cytoplasm; Fig. 1B). A number of
multinucleated cells were also presented, but the classical
hallmark cell of ALCL was not observed.
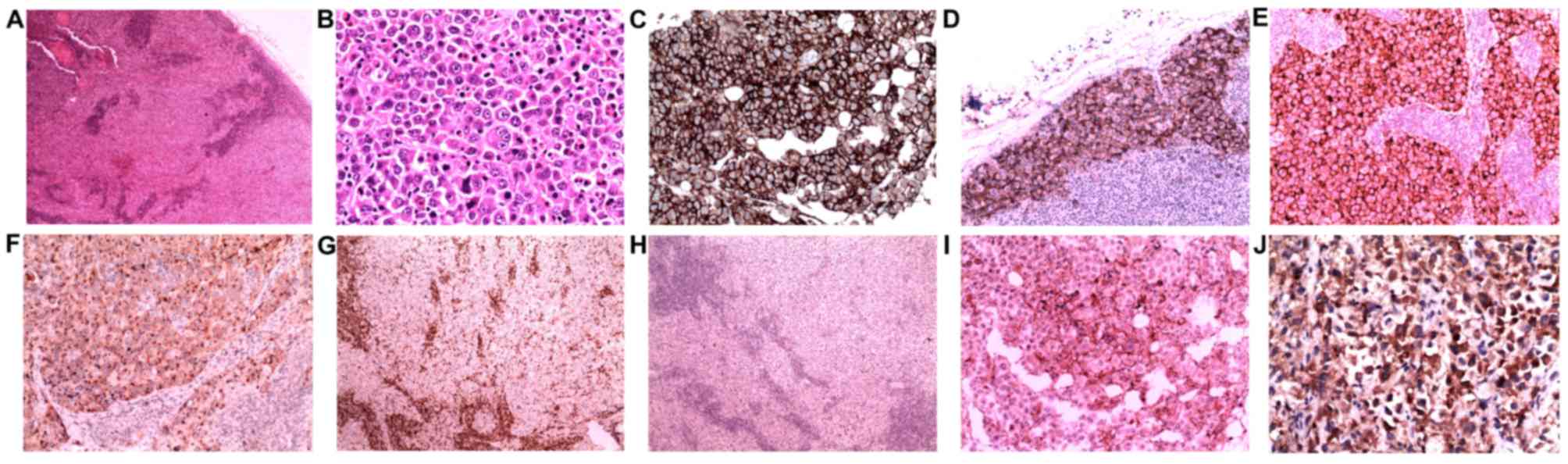 | Figure 1.Lymph node biopsies reveal diffuse and
sinus proliferation of large lymphocytes with immunoblastic
features. (A) H&E stain; magnification, ×40. (B) H&E
stain;magnification, ×400. The lymphoma cells were positive for (C)
CD45, (D) CD138 and (E) epithelial membrane antigen, and they
exhibited (F) granular cytoplasmic anaplastic lymphoma kinase
positivity. Stains for (G) CD43 and (H) CD30 were negative. A
subset of tumor cells was moderately positive for (I) CD4. (J)
CytokeratinAE1/3 staining of neoplastic cells was positive in the
last relapsed needle biopsy. (C and J) Immunoperoxidase stain;
magnification, ×400. (D, E, F, I) Immunoperoxidase stain;
magnification, ×200. (G and H) Immunoperoxidase stain;
magnification, ×40. H&E, hematoxylin and eosin; CD, cluster of
differentiation. |
The 4-µm-thick formalin-fixed paraffin-embedded
tumor tissue sections were used for all IHC staining, and the
staining was performed using a BenchMark ULTRA automated IHC
staining instrument and an ultraVIEW kit (Benchmark XT; Ventana
Medical Systems, Tucson, AZ). All procedures including incubation
time and temperature were performed according to the manufacture's
protocol. The primary antibodies applied in the biopsies were as
following: CD20 (cat. no., GA60461-2; dilution, 1:100; Dako;
Agilent Technologies, Santa Clara, CA, USA,), Bcl-6 (cat. no.,
IS62530-2; dilution, 1:100; Dako; Agilent Technologies), MUM-1
melanoma-associated antigen (mutated) 1 (cat. no., M725929-2;
dilution, 1:100; Dako; Agilent Technologies), and CD10 (cat. no.,
CD10-270-L-CE; dilution, 1:50; Novocastra, Leica Biosystems, UK)
was performed. CD30(cat. no., CD30-591-L-CE; dilution, 1:50;
Novocastra), CD15(cat. no., IR06261-2; dilution, 1:100; Dako;
Agilent Technologies), EMA (cat. no., M061329-2; dilution, 1:100;
Dako; Agilent Technologies), ALK-1(cat. no., IR64161-2; dilution,
1:50; Dako; Agilent Technologies), CD45(cat. no., GA75161-2;
dilution, 1:100; Dako; Agilent Technologies), CD43(cat. no.,
GA63661-2; dilution, 1:100; Dako; Agilent Technologies), CD3(cat.
no., CD3-565-L-CE; dilution, 1:100; Novocastra), CD4(cat. no.,
IS64930-2, dilution, 1:100, Dako, Agilent Technologies), paired box
5/PAX5(cat. no., PA1-109, dilution, 1:100, Thermo Fisher, Rockford,
USA), Ki67(cat. no., GA62661-2; dilution, 1:100; Dako; Agilent
Technologies), B-cell lymphoma 2/bcl2 (cat. no., M088729-2;
dilution, 1:50; Dako; Agilent Technologies), CK (ca. no.,
M351501-2; dilution, 1:100; Dako; Agilent Technologies) and cam5.2
(cat. no., 349205; dilution, 1:100; BD Biosciences, San Jose, CA,
USA); and CD138 (cat. no., GA64261-2; dilution, 1:100; Dako;
Agilent Technologies) and CD79a (cat. no., M705029-2; dilution,
1:100; Dako; Agilent Technologies) were added during the revision.
The results of IHC analysis revealed that almost all the large
neoplastic cells were markedly positive for CD45, CD138 and EMA
(Fig. 1C-E). ALK-1 staining was
markedly positive in neoplastic cells with a granular cytoplasmic
pattern (Fig. 1F) and MUM1 was
expressed partially in tumor cells. Immunostaining of Ki67
demonstrated a proliferation index of ~45%. Neoplastic cells were
negative for CD43 (Fig. 1G), CD30
(Fig. 1H), CD20, CD79a, CD15, PAX5
and CD3 in the patient's malignancies. Subsets of neoplastic cells
were positive for CD4 (Fig. 1I). CK
(Fig. 1J) was negative in excision
biopsies, but was moderately positive in the needle biopsy.
Epstein-Barr virus (EBV) in situ
hybridization
Tissue sections were hybridized as described
(9) with a biotin-labeled nucleic
acid probe (Pan Path, Budel, The Netherlands) to determine the
existence of EBV. Specimens with EBER nuclear expression would
indicate latent EBV infection by the presence of RNA which was
complementary to EBV. However, no EBV infection was detected by
in situ hybridization in the present case.
Fluorescence in situ hybridization
(FISH)
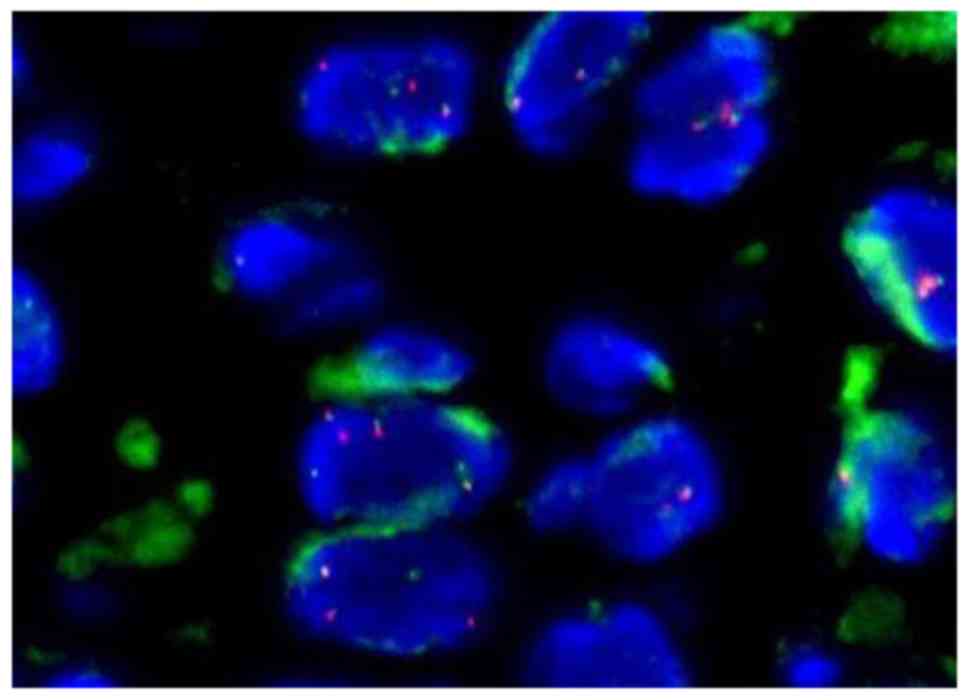
Interphase FISH analysis was performed during the
needle biopsy using the VysisLSI ALK Dual Color Break Apart
Rearrangement Probe (Abbott Pharmaceutical Co., Ltd., Lake Bluff,
IL, USA), which contains loci flanking the typical ALK gene
breakpoint at 2p23.3 in order to detect suspected ALK gene
rearrangement. The FISH slides were reviewed and under a
fluorescence microscope (BX60, Olympus), and images were captured
via camera and molecular genetics software (Cytovision Genus v7.1;
Leica Microsystems, Ltd, Milton Keynes, UK). The break-apart
pattern is a fusion signal (native ALK) and became two
separated signals (one orange and one green). The distance between
two separated signals was estimated using at least twice the
largest signal size and positive cases were defined as ≥15 cells
with a break-apart pattern in 100 tumor cells. ALK gene
translocation in this case was demonstrated as positive, with 1 or
2 extra copies of ALK gene presented (Fig. 2) in ≥30% of cells.
Clonality studies
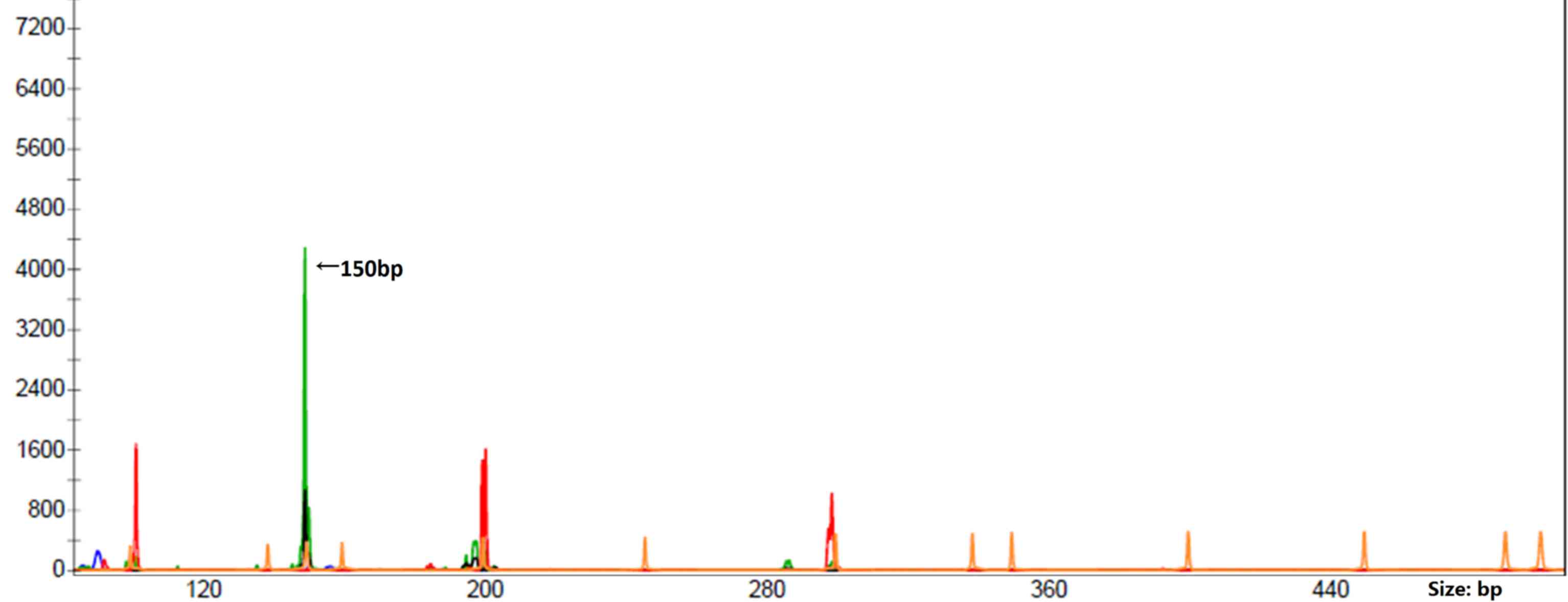
The polymerase chain reaction (PCR) was performed
using a multiplex PCR of European BIOMED-2 assays (Yuanqi Bio,
Shanghai, China). Primers for detecting clonally rearranged
immunoglobulin (Ig) were set in 8 multiplex PCR tubes: A total of 5
Ig heavy locus (IGH; including3 variable-joining domains and
2diversity-joining domains), 2 Ig κ locus (IGK) and 1 Ig λ
locus (IGL). T-cell receptor (TCR) gene rearrangement
was performed using primers in 6 multiplex PCR tubes: A total of 3
TCRβ, 2 TCRγ and 1 TCRδ. The clonal rearrangement was detected only
in the A tube of the IGK gene (Fig. 3). No IGH, IGL or
TCR gene rearrangements were detected.
Discussion
The results of the present relapsed case tumor
morphology and immunophenotype investigations from the routine
pathological department led to differential diagnoses of
hematopoietic and non-hematopoietic neoplasms, in particular ALK
positive-ALCL and metastatic carcinoma. First, CK expression may
mislead to a poorly differentiated carcinoma, but marked expression
of CD45 (LCA) would easily exclude this misdiagnosis. Secondly, the
IHC results demonstrated that tumor cells were positive for ALK-1
and EMA, but negative for commonly used T- and B-cell markers
(CD20, CD79a, CD3 and CD43), with the exception of a low expression
level of CD4, which is generally considered a T helper cell marker
and is normally expressed in ALCL. Thus, the diagnosis of
ALK-positive ALCL of null cell lineage was suggested to be the most
suitable, although CD30 staining was repeated twice and revealed
negative results at the beginning.
The initial misdiagnosis of the present study may
also be attributed to not identifying the ALK-positive LBCL entity
owing to its rarity. Further plasma cell differentiated markers and
clonality studies for T- or B-cell origin would be useful to
confirm a correct diagnosis. The additional IHC staining for CD138
was positive, which was consistent with the reported positive ratio
of CD138, EMA, CD20 and CD79a in ALK-positive LBCL, which were
100,97.6, 11 and 18%, respectively (5). Expression of the T-cell marker CD4 was
identified in between 37.8 and 40% of ALK-positive LBCL cases
(3,5),
which may be the reason for the confusion over the origin of the
tumor cell. The final definite diagnosis of the present case was
based on the clonality analysis. However, as indicated in a
previous study, PCR clonal analyses for IGH were identified in a
majority of patients demonstrating rearrangement genes (5), but there was also a similar case
reported by with rearrangement if IGH genes were solely
detected (10), thus making it more
difficult to reach a precise diagnosis, particularly in
demonstrating no T- nor B-cell immunophenotypes. Thus, the BIOMED-2
PCR assays for IGK and IGL gene rearrangements are
essential for B-cell clonality analysis in this subtype of
lymphoma, and a previous study also revealed IGK gene
rearrangements (10); however, there
appeared to be no IGL gene rearrangements reported in the
ALK-positive LBCL cases.
The majority of the ALK fusion protein in
ALK-positive LBCL came from cytogenetic fusion of the ALK
gene at chromosome 2p23 and clathrin heavy-chain (CLTC) gene
at chromosome 17q23 (1,3). The nucleophosmin gene at chromosome5q35
was the most common partner observed in ALK positive ALCL (7,11–16). The granular cytoplasmic ALK staining
pattern demonstrated in the present case was similar to the
correlation with the CLTC-ALK fusion observed in a previous
study by Gascoyne et al (17)
and De Paepe et al (18) in
2003. The present case also exhibited one or two extra ALK copies
demonstrating the high genetic instability detected using FISH,
which is characteristic of ALK-positive LBCLs (16). However, ALK protein expression and
genomic alteration was not useful for the differential diagnosis
between ALK positive ALCL and ALK positive LBCL.
To the best of our knowledge, CK expression has been
identified in <5 ALK positive LBCL cases previously (5,8), whereas
CD4 expressed has been observed in >5 previous ALK positive LBCL
cases. The aberrant expression levels of CK and CD4 in ALK-positive
LBCL are rare. Only the final relapsed malignancy in the present
case was positive for CK. It was previously reported that
CLTC was located at chromosomal locus 17q23 and a cluster of
human keratin-associated protein genes were revealed to be embedded
at chromosomal locus 17q12-21 (19),
which is in proximity to CLTC. This suggested that the
translocation and instability of the CLTC gene may induce an
incidental activation of the keratin-associated gene and CK
expression. Further investigation of this is required.
The recognition of ALK-positive DLBCL is also
clinically important as the majority of patients follow a more
aggressive disease course and unfavorable prognosis (3). ALK-positive LBCLs are unlikely to
respond favorably to the current standard CHOP therapy for ALCL.
They require distinct modalities of treatment and candidates for
novel treatment approaches, with or without autologous stem cell
transplantation; novel biological agents including anti-CD138 or
anti-ALK monoclonal antibodies or other immune conjugates (20,21) may
provide future treatment strategies. The aggressive clinical course
of the present case further confirmed the diagnosis of ALK-positive
LBCL, an aggressive form of DLBCL with ectopic ALK expression due
to CLTC-ALK gene fusion (3).
In conclusion, ALK-positive large B-cell lymphoma
expressed cluster of differentiation 4 and cytokeratin are
extremely rare and easily be misdiagnosed, thus
standardizedBIOMED-2 PCR assays that encompass the IGH,
IGL and, particularly, IGK gene rearrangements are
essential in B-cell gene clonality analysis for this subtype of
lymphoma.
Acknowledgements
The authors thank all their colleagues who
participated in the analyses and revision of the present case.
References
|
1
|
Swerdlow SH, Campo E, Harris N.L, Jaffe
E.S, Pileri S.A, Stein H, Thiele J and Vardiman J.W: WHO
classification tumours of haematopoietic and lymphoid tissues. 4th.
Lyon, France: IARC Press; pp. 244–255. 2008
|
|
2
|
Delsol G, Lamant L, Mariamé B, Pulford K,
Dastugue N, Brousset P, Rigal-Huguet F, Al Saati T, Cerretti DP,
Morris SW and Mason DY: A new subtype of large B-cell lymphoma
expressing the ALK kinase and lacking the 2; 5 translocation.
Blood. 89:1483–1490. 1997.PubMed/NCBI
|
|
3
|
Laurent C, Do C, Gascoyne RD, Lamant L,
Ysebaert L, Laurent G, Delsol G and Brousset P: Anaplastic lymphoma
kinase-positive diffuse large B-cell lymphoma: A rare
clinicopathologic entity with poor prognosis. J Clin Oncol.
27:4211–4216. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang RF, CHEN G, GONG LP and LU LL:
Pathologic and molecular genetic study of anaplastic lymphoma
kinase-positive large B-cell lymphoma. Zhonghua Bing Li Xue Za Zhi.
40:169–172. 2011.(In Chinese). PubMed/NCBI
|
|
5
|
Yu H, Huang J, Sun J, Wang C, Lin M and Li
H: Anaplastic lymphoma kinase-positive large B-cell lymphoma: A
potential diagnostic pitfall. Indian J Pathol Microbiol.
58:241–245. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gustmann C, Altmannsberger M, Osborn M,
Griesser H and Feller AC: Cytokeratin expression and vimentin
content in large cell anaplastic lymphomasand other non-Hodgkin's
lymphomas. Am J Pathol. 138:1413–1422. 1991.PubMed/NCBI
|
|
7
|
Zhang Q, Ming J, Zhang S, Li B, Han X and
Qiu X: Cytokeratin positivity in anaplastic large cell lymphoma: A
potential diagnostic pitfall in misdiagnosis of metastatic
carcinoma. Int J Clin Exp Pathol. 6:798–801. 2013.PubMed/NCBI
|
|
8
|
Nguyen TT, Kreisel FH, Frater JL and
Bartlett NL: Anaplastic large cell lymphoma with aberrant
expression of multiple cytokeratins masquerading as metastatic
carcinoma of unknown primary. J Clin Oncol. 31:e443–e445. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shi Y and Li X: Clinicopathologic features
and association with Epstein-Barr virus infection in 235 cases of
Hodgkin lymphoma from northern China. Zhonghua Bing Li Xue Za Zhi.
44:84–89. 2015.(In Chinese). PubMed/NCBI
|
|
10
|
Lin SY, Chuang SS, Jhuang JY, Sakamoto K,
Takeuchi K, Bahrami A and Tsai CC: ALK positive large B-cell
lymphoma with a massive neutrophilic infiltrate: Report of a case
mimicking epithelioid inflammatory myofibroblastic tumour. J Clin
Pathol. 68:496–498. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Reichard KK, McKenna RW and Kroft SH:
ALK-positive diffuse large B cell lymphoma: Report of four cases
and review of the literature. Mod Pathol. 20:310–319. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rudzki Z, Rucińska M, Jurczak W, Skotnicki
AB, Maramorosz-Kurianowicz M, Mruk A, Piróg K, Utych G, Bodzioch P,
Srebro-Stariczyk M, et al: ALK-positive diffuse largeB-cell
lymphoma: Two more cases and a brief literature review. Pol J
Pathol. 56:37–45. 2005.PubMed/NCBI
|
|
13
|
Onciu M, Behm FG, Downing JR, Shurtleff
SA, Raimondi SC, Ma Z, Morris SW, Kennedy W, Jones SC and Sandlund
JT: ALK-positive plasmablastic B-cell lymphoma with expression of
the NPM-ALK fusion transcript: Report of 2 cases. Blood.
102:2642–2644. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Adam P, Katzenberger T, Seeberger H,
Gattenlöhner S, Wolf J, Steinlein C, Schmid M, Müller-Hermelink HK
and Ott G: A case of a diffuse large B-cell lymphoma of
plasmablastic type associated with the t(2;5)(p23;q35) chromosome
translocation. Am J Surg Patho. 27:1473–1476. 2003. View Article : Google Scholar
|
|
15
|
Lee HW, Kim K, Kim W and Ko YH:
ALK-positive diffuse large B-cell lymphoma: Report of three cases.
Hematol Oncol. 26:108–113. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shi M, Miron PM, Hutchinson L, Woda BA,
Nath R, Cerny J and Yu H: Anaplastic lymphoma kinase-positive large
B-cell lymphoma with complex karyotype and novel ALK gene
rearrangements. Hum Pathol. 42:1562–1567. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gascoyne RD, Lamant L, Martin-Subero JI,
Lestou VS, Harris NL, Müller-Hermelink HK, Seymour JF, Campbell LJ,
Horsman DE, Auvigne I, et al: ALK-positive diffuse large B-cell
lymphoma is associated with Clathrin-ALK rearrangements: Report of
6 cases. Blood. 102:2568–2573. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
de Paepe P, Baens M, van Krieken H,
Verhasselt B, Stul M, Simons A, Poppe B, Laureys G, Brons P,
Vandenberghe P, et al: ALK activation by the CLTC-ALK fusion is a
recurrent eventin in large B-cell lymphoma. Blood. 102:2638–2641.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rogers MA, Langbein L, Winter H, Ehmann C,
Praetzel S, Korn B and Schweizer J: Characterization of a cluster
of human high/ultrahigh sulfur keratin-associated protein genes
embedded in the type I keratin gene domain on chromosome 17q12-21.
J Biol Chem. 276:19440–19451. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Castillo JJ, Chavez JC,
Hernandez-Ilizaliturri FJ and Montes-Moreno S: CD20-negative
diffuse large B-cell lymphomas: Biology and emerging therapeutic
options. Expert Rev Hematol. 8:343–354. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Roskoski R Jr: Anaplastic lymphoma kinase
(ALK): Structure, oncogenic activation, and pharmacological
inhibition. Pharmacol Res. 68:68–94. 2013. View Article : Google Scholar : PubMed/NCBI
|