Introduction
Pulmonary large-cell neuroendocrine carcinoma
(LCNEC) is a rare type of lung cancer that accounts for <1% of
all primary lung malignancies (1).
Since the biological behavior of LCNEC is similar to that of small
cell lung cancer (SCLC), patients with LCNEC are often misdiagnosed
and have an extremely poor prognosis (2). The 5-year survival rates for patients
with LCNEC have been revealed to be significantly decreased
compared with patients with other histological types of non-small
cell lung cancer (NSCLC) (2,3).
The common sites of metastasis from LCNEC are the
liver, adrenal glands, bone, and brain, with hematogenous
metastasis being the primary cause of treatment failure. Until
recently, the rare sites of metastases from LCNEC which have been
reported include the ovaries, small intestine, mandible, tonsil,
vulva and prostate (4–9). In addition, Tsimpas et al
(10) reported a case of LCNEC
metastasis in the cauda equina; however, the patient in this study
did not receive a cerebrospinal fluid (CSF) test and was not able
to be diagnosed with leptomeningeal metastasis. Paydas et al
(11) reported a case of
leptomeningeal metastasis from LCNEC, but no cytological
examination had been performed and no line-enhancement imaging for
the diagnosis of leptomeningeal metastasis was performed for the
patient. To the best of our knowledge, the present case report is
the first to describe leptomeningeal metastasis from pulmonary
LCNEC confirmed by neuroimaging and CSF cytology. Thus, the present
case report describes a rare case of leptomeningeal metastasis from
LCNEC alongside a review of the literature.
Case report
A 39-year-old male was admitted to Norman Bethune
First Hospital (Changchun, China) in April 2013 complaining of a
cough and blood-stained sputum that lasted for 10 days. The patient
had a 20-year history of drinking and smoking. A computed
tomography (CT) scan of the chest revealed a mass in the right
pulmonary hilum that was accompanied by an enlargement of the right
supraclavicular and mediastinal lymph nodes. A transbronchial
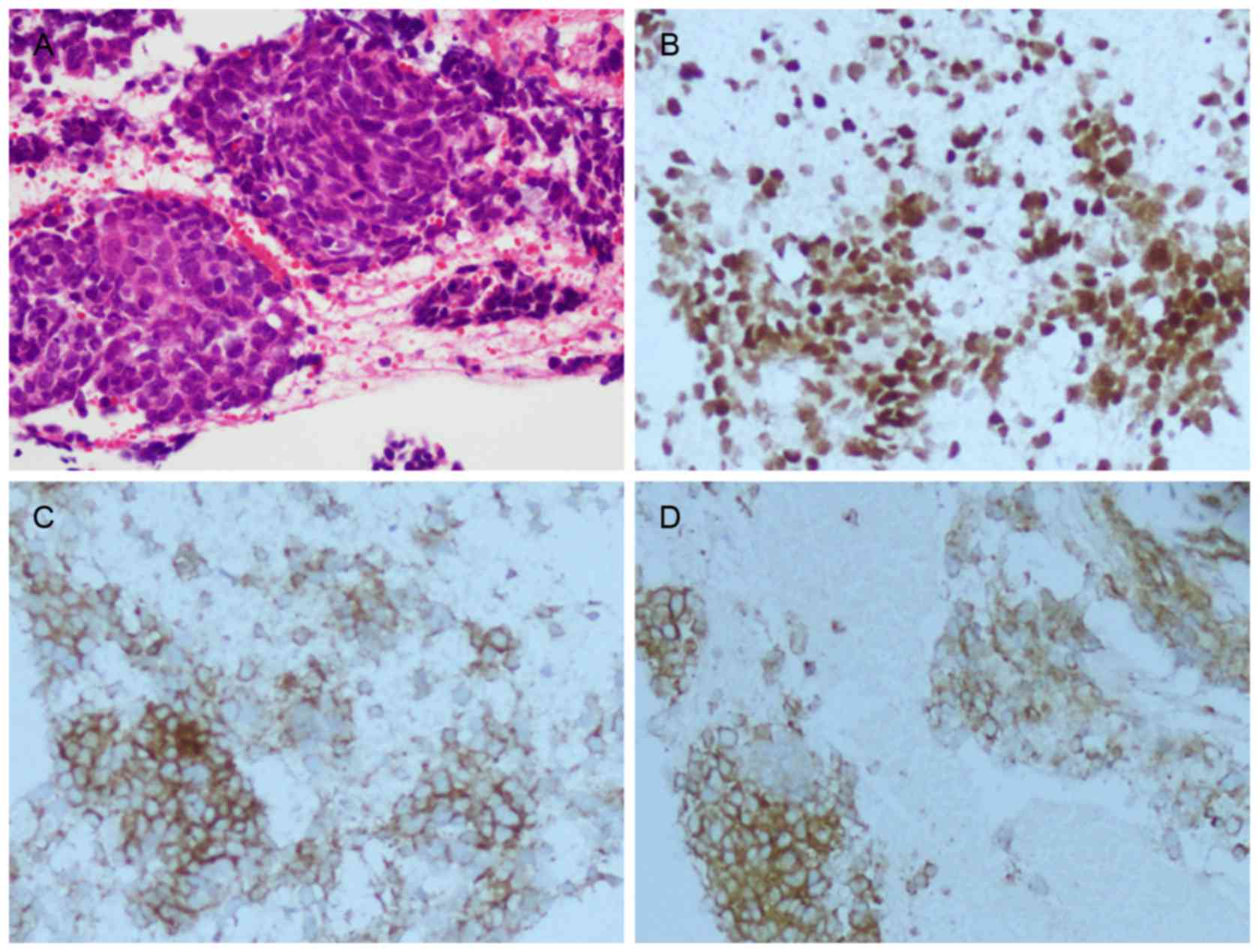
biopsy revealed that the tumor cells exhibited an unclear boundary,
with infiltrative growth and numerous cells which were arranged as
flaky, cord-like, adenoid or chrysanthemum-shaped clusters. The
cells commonly presented with large volumes, polygonal shape, small
cytoplasm, filamentous chromatin and intensely stained nuclei.
Three to four abnormal mitotic events were observed in each
high-power field. A wide range of tumor necrosis was visualized in
the area of poor differentiation (Fig.
1A). Staining of the patient's tumor was positive for thyroid
transcription factor-1 (TTF-1), cluster of differentiation 56
(CD56; also known as neural cell adhesion molecule), synaptophysin
(Syn) (Fig. 1B-D) and p63
(interspersed), and negative for leucocyte common antigen. This
supported the histological diagnosis of LCNEC. Pathological
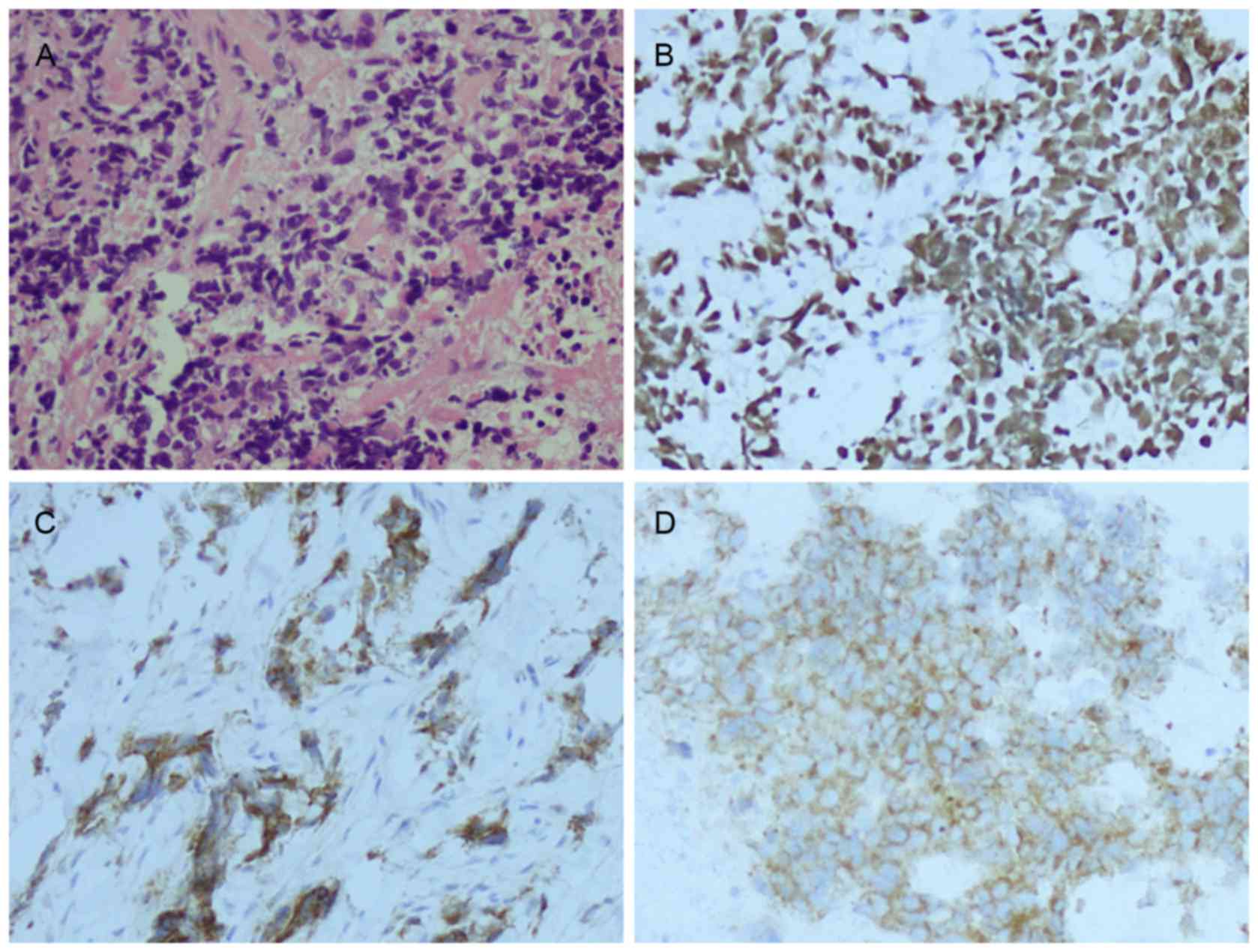
examination of the right supraclavicular lymph node indicated
metastatic cancer invasion (Fig. 2A).
This observation was confirmed by negative immunohistochemical
staining for cytokeratin 5/6, and positive staining for TTF-1,
CD56, Syn (Fig. 2B-D) and p63
(partial). This supported the histological diagnosis of a
neuroendocrine carcinoma with a pulmonary origin. No other
metastases were detected using an abdominal CT scan.
The patient had a partial response to six cycles of
systemic chemotherapy with gemcitabine (2 g on day 1) and cisplatin
(50 mg on days 1–3). The lesion decreased in size following two
cycles of chemotherapy and the patient achieved partial disease
control. No severe adverse effects were detected. At 2 months after
the last chemotherapy cycle, the patient began to experience
radiating pain and numbness in his left lower limb, hoarseness,
epileptic seizures and blurred vision. Additionally, the patient
suffered a seizure due to symptom aggravation. Conventional
biochemical examinations including routine blood, urine, liver and
kidney function tests were normal. Serum levels of tumor markers
were 22.31 U/ml cancer antigen 153 (CA153), 1.16 ng/ml
carcinoembryonic antigen (CEA), 14.6 ng/ml neuron-specific enolase
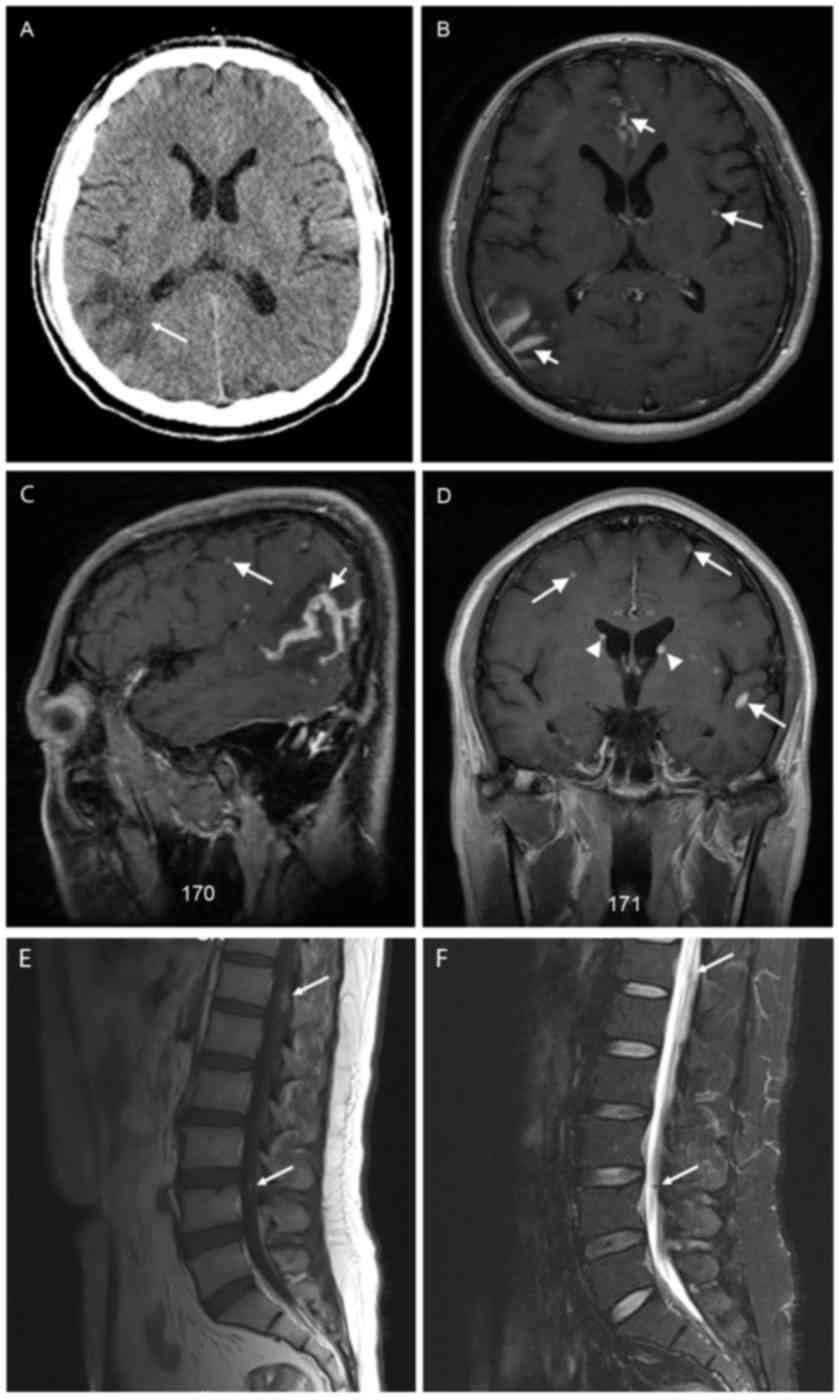
(NSE) and 0.7 ng/ml CYFRA21-1. A CT scan of the brain revealed
irregular low-density shadows from edema on the right
parietal-occipital area (Fig. 3A).
Magnetic resonance imaging (MRI) of the brain identified metastatic
nodules in the inferior cortex, sulci and gyri and internal
ventricles, and line-enhancements in the leptomeningeal mater
(Fig. 3B-D). Gadolinium enhancement
scans of the lumbar spine revealed flake-enhanced lesions in the
T12 vertebra of the spine and nodular-enhanced lesions along the
cauda equina nerve in the L3-4 space (Fig. 3E). A low signal nodule-like lesion
along the cauda equina nerve was observed using T2-weighted imaging
(T2WI; Fig. 3F). Results from a
lumbar puncture revealed that the patient's CSF was colorless,
intracranial pressure was 200 mmH2O, the protein level
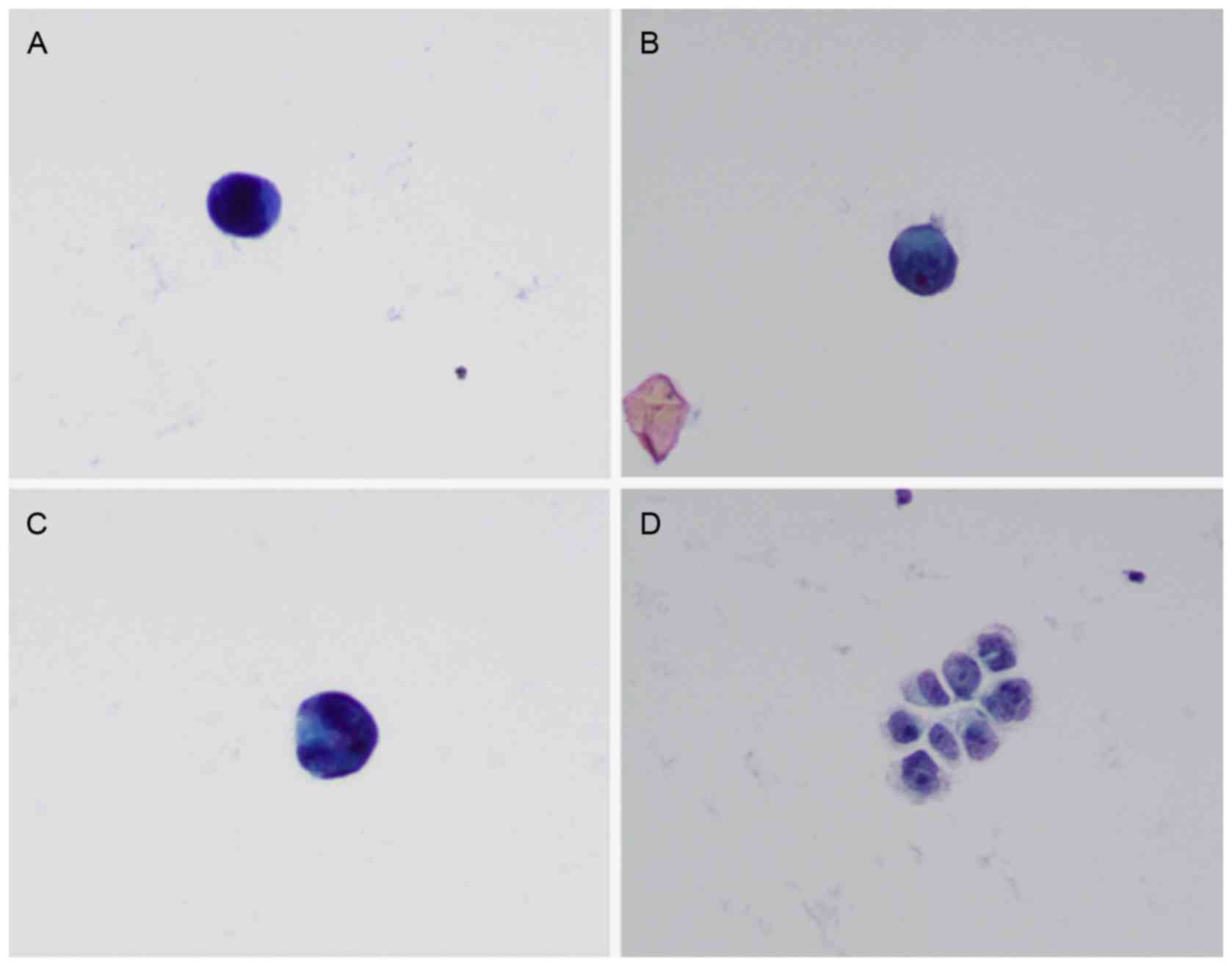
was 0.75 g/l and the glucose level was 3.35 mmol/l. Tumor cells
were identified within the patient's CSF via liquid-based
technology (ThinPrep TCT2000) combined with Papanicolaou staining
(Fig. 4). Tumor marker levels in CSF
were 1.00 U/ml CA153, 0.20 ng/ml CEA, 25.8 ng/ml NSE and 2.5 ng/ml
CYFRA21-1. On the basis of these results, a diagnosis of
leptomeningeal metastasis was made. The patient's Karnofsky
performance status (KPS) (12) score
was determined to be 40–50 points.
The patient's treatment regimen involved
three-dimensional conformal radiotherapy with a 6 MV X-ray to the
whole brain and thoracolumbar spinal canal, which consisted of a 40
Gy total radiation dose administered in 20 fractions over a 4-week
period. Simultaneous administration of intrathecal chemotherapy
using methotrexate (MTX, 15 mg) and dexamethasone (5 mg) was
performed once a week. The first intrathecal chemotherapy began on
the first day of radiotherapy. Three cycles of intrathecal
chemotherapy and 14 days of radiotherapy (20 Gy in 10 fractions)
markedly alleviated the patient's symptoms and his KPS score
increased to 60 points. The patient declined further treatment for
personal reasons and was discharged from the hospital. After 2
months, the patient began to experience headaches and numbness and
succumbed due to disease progression. The patient's overall
survival (OS) time was 11 months, and the patient had survived for
4.9 months from the time of diagnosis of leptomeningeal
metastasis.
Written informed consent was obtained from the next
of kin of the patient for publication of this case report and any
accompanying images.
Discussion
Leptomeningeal metastasis is a fatal complication of
malignant cancers and occurs in 5% of patients diagnosed with solid
tumors (13). This type of metastasis
results from invasion of the subarachnoid space by the migratory
tumor cells and dissemination through the CSF. Thus, patients
usually have pleomorphic and multifocal neurological complaints due
to disperse involvement of the central nervous system. Despite
having an aggressive treatment regimen, the median OS time is
between 2 and 3 months (13).
Leptomeningeal metastasis often occurs in patients with melanoma,
breast or lung cancer. Although lung cancer is one of the most
common malignant solid tumors prone to invade the meninges, to the
best of our knowledge, there has been no report concerning
leptomeningeal metastasis from pulmonary LCNEC. To the best of our
knowledge, the present case report documents the first
cytologically confirmed case of leptomeningeal involvement from
LCNEC.
In 1991, Travis et al (14) first described the histological
characteristics of LCNEC, which included large cells with abundant
cytoplasm, a high mitotic rate, extensive necrosis and a
neuroendocrine growth pattern. In 2001, the World Health
Organization suggested that, in order to confirm the neuroendocrine
origin of the tumor cells and thereby diagnose LCNEC, a
neuroendocrine morphology and positive immunohistochemical staining
for at least one neuroendocrine-specific marker, e.g. chromogranin,
CD56 or Syn, must be present (15).
In the present case report, histopathological examination of the
patient's primary lung tumor and cervical lymph nodes combined with
immunohistochemistry confirmed the diagnosis of LCNEC.
An MRI examination is a critical auxiliary diagnosis
for leptomeningeal metastasis (13).
The major imaging features include dot- and line-enhancements in
the leptomeningeal mater, metastatic nodules in the sulci and gyri,
inferior cortex, internal ventricles and seeding nodules along the
cauda equina nerve (13). In the
present case report, the patient exhibited all of the clinical
imaging manifestations mentioned above that conformed to the
characteristics of implantation metastases. In particular,
line-enhancements in the sulci and gyri and implanted metastatic
nodules along the cauda equina nerve are considered specific
imaging features for leptomeningeal metastasis, which may be used
as a diagnostic tool (14).
CSF cytological analysis provides the optimum
assessment of leptomeningeal metastasis (13). In this case, the tumor cells exhibited
evident characteristics of malignancy that included large cellular
volumes, pleomorphism, markedly increased nuclear-to-cytoplasmic
ratio and markedly stained chromatin.
There are a limited number of reports describing the
treatment regimens for patients with LCNEC. Several studies have
demonstrated that the response rate of LCNEC to cisplatin-based
chemotherapy was similar to that of small cell carcinoma (16). In 2013, a multicenter prospective
study reported the median progression-free survival and OS time for
42 patients with advanced stage LCNEC were 5.2 months and 7.7
months respectively, following cisplatin-irinotecan chemotherapy
(17).
Patients with leptomeningeal metastasis, which is a
fatal complication of malignant tumor, have a very poor prognosis.
The main objective of leptomeningeal metastasis treatment is to
alleviate symptoms of the nervous system, improve quality of life
and prolong the survival time of the patient (13). Owing to the direct exposure of the
central nervous system to cancer cells, a whole central nervous
system therapy using intrathecal chemotherapy alone or in
combination with local radiotherapy should be performed (13). MTX remains the most widely used and
clinically effective intrathecal chemotherapeutic drug used to
treat leptomeningeal metastasis from solid tumors (13). Currently, an intrathecal injection of
10–15 mg MTX twice weekly is more commonly used in the initial
treatment (13). Radiotherapy on
bulky disease observed on MRI or sites of symptomatic disease
eliminates locally aggregated tumor cells and re-establishes the
normal CSF circulation to improve the efficacy, as well as decrease
the toxicity of intrathecal chemotherapy. In addition, metastatic
lesions in the brain parenchyma may also be effectively treated
simultaneously (13). The regimen of
whole brain radiotherapy commonly consists of a total radiation
dose of 30 Gy in 10 fractions for 2 weeks (13). In the present case, the patient
received simultaneous intrathecal chemotherapy with radiotherapy.
To reduce neurotoxicity, the single radiotherapy dosage was set at
2 Gy and the density of the regimen of intrathecal MTX was reduced
to once per week. The treatment was well tolerated by the patient
and the symptoms were alleviated rapidly. There was no severe
adverse reaction. However, the patient failed to complete all
treatments owing to personal reasons and succumbed to disease
progression.
Currently, there is no standard therapy regimen for
leptomeningeal metastasis from solid tumors. Intrathecal
chemotherapy and radiotherapy are valuable treatment approaches,
but an optimal combination of distinct treatments has not been
extensively studied. The male patient in the present case report
presented multiple adverse prognostic factors including a low KPS
score as well as severe and pleomorphism nerve dysfunction.
Previous studies indicated that intrathecal chemotherapy does not
improve OS times in solid tumors (18–20) and
National Comprehensive Cancer Network (NCCN) guidelines suggest
that radiation therapy alone may produce a positive effect with
less toxicity. However, studies have demonstrated that radiation
therapy alone only alleviated symptoms of the nervous system and
did not prolong patient OS times (21,22).
NCCN guidelines suggest the use of simultaneous
intrathecal chemotherapy and radiation in leptomeningeal
metastasis, but this combination treatment has not been extensively
studied. Therefore, this approach was adopted to treat
leptomeningeal metastasis in patients with adverse prognostic
factors. Untreated patients with leptomeningeal metastasis have a
median survival time of 4–6 weeks; this survival time may be
prolonged to 2–3 months in patients with NSCLC from leptomeningeal
metastasis by using effective treatments (13). In the present case report, the patient
did not suffer obvious toxic effects and survived for 4.9 months
from the time of diagnosis of leptomeningeal metastasis. This time
was longer than the median survival time previously reported,
suggesting a benefit of administration of simultaneous treatments
to alleviate neurological symptoms and extend survival times.
In conclusion, pulmonary LCNEC with leptomeningeal
metastasis is a rare disease that is associated with poor
prognosis. Nevertheless, the present case report and review of the
literature suggest that doctors should realize the potential of
leptomeningeal metastasis from pulmonary LCNEC, and aggressive
treatment may result in improved symptoms and possibly
survival.
Acknowledgements
The authors wish to thank Dr Yongxiang Wang for her
expert technical assistance with cytological analysis of
cerebrospinal fluid.
References
|
1
|
Gollard R, Jhatakia S, Elliott M and Kosty
M: Large cell/neuroendocrine carcinoma. Lung Cancer. 69:13–18.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sun JM, Ahn MJ, Ahn JS, Um SW, Kim H, Kim
HK, Choi YS, Han J, Kim J, Kwon OJ, et al: Chemotherapy for
pulmonary large cell neuroendocrine carcinoma: Similar to that for
small cell lung cancer or non-small cell lung cancer? Lung Cancer.
77:365–370. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Le Treut J, Sault MC, Lena H, Souquet PJ,
Vergnenegre A, Le Caer H, Berard H, Boffa S, Monnet I, Damotte D
and Chouaid C: Multicentre phase II study of cisplatin-etoposide
chemotherapy for advanced large-cell neuroendocrine lung carcinoma:
The GFPC 0302 study. Ann Oncol. 24:1548–1552. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bugiantella W, Cavazzoni E, Graziosi L,
Valiani S, Franceschini MS and Donini A: Small bowel metastasis
from lung cancer: A possible cause of acute abdomen. Case report
and literature review. G Chir. 32:120–122. 2011.PubMed/NCBI
|
|
5
|
Murakawa T, Nakajima J, Fukami T, Tanaka
M, Takeuchi E and Takamoto S: Tonsillar metastasis from large cell
carcinoma of the lung. Jpn J Thorac Cardiovasc Surg. 49:377–380.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nelson BE, Carcangiu ML and Chambers JT:
Intraabdominal hemorrhage with pulmonary large cell carcinoma
metastatic to the ovary. Gynecol Oncol. 47:377–381. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rocconi RP, Leath CA III, Johnson WM III,
Barnes MN III and Conner MG: Primary lung large cell carcinoma
metastatic to the vulva: A case report and review of the
literature. Gynecol Oncol. 94:829–831. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shimizu K, Goto T, Maeshima A, Oyamada Y
and Kato R: Prostatic metastasis of pulmonary large cell
neuroendocrine carcinoma. J Cancer. 3:96–99. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yoshii T, Muraoka S, Sano N, Furudoi S and
Komori T: Large cell carcinoma of the lung metastatic to the
mandibular gingiva. J Periodontol. 73:571–574. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tsimpas A, Post NH, Moshel Y and
Frempong-Boadu AK: Large cell neuroendocrine carcinoma of the lung
metastatic to the cauda equina. Spine J. 10:e1–e5. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Paydas S, Bicakci K and Yavuz S: Dramatic
response with capecitabine after cranial radiation to the brain
parenchymal and leptomeningeal metastases from lung cancer. Eur J
Intern Med. 20:96–99. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schag CC, Heinrich RL and Ganz PA:
Karnofsky performance status revisited: Reliability, validity, and
guidelines. J Clin Oncol. 2:187–193. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Le Rhun E, Taillibert S and Chamberlain
MC: Carcinomatous meningitis: Leptomeningeal metastases in solid
tumors. Surg Neurol Int. 4:(Suppl 4). S265–S288. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Travis WD, Linnoila RI, Tsokos MG,
Hitchcock CL, Cutler GB Jr, Nieman L, Chrousos G, Pass H and
Doppman J: Neuroendocrine tumors of the lung with proposed criteria
for large-cell neuroendocrine carcinoma. An ultrastructural,
immunohistochemical, and flow cytometric study of 35 cases. Am J
Surg Pathol. 15:529–553. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brambilla E, Travis WD, Colby TV, Corrin B
and Shimosato Y: The new World Health Organization classification
of lung tumours. Eur Respir J. 18:1059–1068. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yamazaki S, Sekine I, Matsuno Y, Takei H,
Yamamoto N, Kunitoh H, Ohe Y, Tamura T, Kodama T, Asamura H, et al:
Clinical responses of large cell neuroendocrine carcinoma of the
lung to cisplatin-based chemotherapy. Lung Cancer. 49:217–223.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Niho S, Kenmotsu H, Sekine I, Ishii G,
Ishikawa Y, Noguchi M, Oshita F, Watanabe S, Nakajima R, Tada H and
Nagai K: Combination chemotherapy with irinotecan and cisplatin for
large-cell neuroendocrine carcinoma of the lung: A multicenter
phase II study. J Thorac Oncol. 8:980–984. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chamberlain MC, Glantz M, Groves MD and
Wilson WH: Diagnostic tools for neoplastic meningitis: Detecting
disease, identifying patient risk, and determining benefit of
treatment. Semin Oncol. 36:(4 Suppl 2). S35–S45. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chamberlain MC, Tsao-Wei D and Groshen S:
Neoplastic meningitis-related encephalopathy: Prognostic
significance. Neurology. 63:2159–2161. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Brem SS, Bierman PJ, Black P, Blumenthal
DT, Brem H, Chamberlain MC, Chiocca EA, DeAngelis LM, Fenstermaker
RA, Fine HA, et al: Central nervous system cancers: Clinical
practice guidelines in oncology. J Natl Compr Canc Netw. 3:644–690.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gani C, Müller AC, Eckert F, Schroeder C,
Bender B, Pantazis G, Bamberg M and Berger B: Outcome after whole
brain radiotherapy alone in intracranial leptomeningeal
carcinomatosis from solid tumors. Strahlenther Onkol. 188:148–153.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Morris PG, Reiner AS, Szenberg OR, Clarke
JL, Panageas KS, Perez HR, Kris MG, Chan TA, DeAngelis LM and Omuro
AM: Leptomeningeal metastasis from non-small cell lung cancer:
Survival and the impact of whole brain radiotherapy. J Thorac
Oncol. 7:382–385. 2012. View Article : Google Scholar : PubMed/NCBI
|