Introduction
Lung cancer is a major cause of cancer-associated
mortality worldwide, with non-small cell lung cancer (NSCLC)
accounting for ~85% of all cases (1). Despite the improvements that have been
made in the early detection of NSCLC, the majority of patients are
initially diagnosed at an advanced stage, and the median survival
rate is <13 months (2,3). Therefore, valuable prognostic factors
are urgently required for the diagnosis of patients with NSCLC. The
aim of the present study was to investigate the clinical
significance of complete blood cell parameter values prior to
disease treatment, and their association with the progression-free
survival (PFS) and overall survival (OS) of Chinese patients with
advanced NSCLC.
The hypothesis proposed by Rudolf Virchow in 1863 on
cancer and inflammation is now widely accepted (4). An emerging body of evidence has
confirmed that inflammation of the microenvironment serves a
pivotal role in the development and progression of malignancies by
inhibiting apoptosis and promoting angiogenesis (5). Numerous studies have reported on the
association between the inflammatory index and prognosis of
patients with NSCLC, including the complete blood count parameters,
neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio (PLR)
and lymphocyte/white blood cell ratio (LWR) (6–8). Yuan
et al (9) reported on the
association between the complete blood cell parameter values prior
to disease treatment and prognosis in patients with curatively
resected NSCLC, and suggested that elevated neutrophil/white blood
cell ratio (NWR) and monocyte/lymphocyte ratio (MLR) may be
independent prognostic factors in curatively resected NSCLC. Feng
et al (10) examined the
association between various blood test parameters and prognosis in
patients with gastric cancer, and revealed that high MLR, NLR, PLR,
NWR and monocyte/white blood cell ratio (MWR), and low LWR, were
associated with poor prognosis in patients with gastric cancer.
To the best of our knowledge, the prognostic value
of complete blood cell parameters in advanced NSCLC has not yet
been investigated. Therefore, the present study aimed to
investigate the prognostic value of various blood test parameters
in patients with advanced NSCLC. Since the main pathological types
of NSCLC are adenocarcinoma and squamous cell carcinoma, these two
types were primarily investigated in this study.
Materials and methods
Patients
A total of 268 patients diagnosed with unresectable
NSCLC at The Affiliated Hospital of Qingdao University (Qingdao,
China) between January 2009 and December 2015 were retrospectively
analyzed. Clinicopathological information and laboratory parameters
of the patients were obtained from electronic records, including
sex, age, smoking history, tumor location, histological type,
Eastern Cooperative Oncology Group (ECOG) performance status
(11), tumor-node-metastasis (TNM)
staging and blood results (12).
Laboratory blood tests from patients were obtained within 7 days
prior to treatment. The blood sample results were obtained via the
electronic medical system and patient consent was provided by the
participants or their families via telephone. ‘Pre-treatment’ is
used to represent the blood parameter results that were collected
before treatment. The major inclusion criterion was pathological
confirmation of NSCLC at an advanced stage (stage IIIB-IV).
Patients with infection, inflammation-associated disease, other
malignant tumors, insufficient blood test data or that were lost to
follow-up were excluded. The present study was approved by the
Ethics Committee of The Affiliated Hospital of Qingdao University
(approval no. QYFYW2LL 25620). All patients were restaged according
to the 7th International Classification System for Lung Cancer
(12). The last follow-up visit
occurred in November 2018.
The following parameters were assessed: NWR, NLR,
platelet/white blood cell ratio (PWR), platelet/lymphocyte ratio
(PLR), MWR, monocyte/lymphocyte ratio (MLR) and LWR. MWR is
calculated by dividing the monocyte count by the white blood cell
count. NLR is calculated by dividing the neutrophil count by the
lymphocyte count. PWR is calculated by dividing the platelet count
by the white blood count. PLR is calculated by dividing the
platelet count by the lymphocyte count. MWR is calculated by
dividing the monocyte count by the white blood cell count. MLR is
calculated by dividing the monocyte count by the lymphocyte count.
LWR is calculated by dividing the lymphocyte count by the white
blood cell count.
Statistical analysis
Receiver operating characteristic (ROC) curves were
used to assess the optimal cut-off values. Kaplan-Meier survival
curves were generated to assess PFS and OS, and differences among
the curves were determined using the log-rank test. Variables that
were identified to be statistically significant at the level of
univariate analysis were then submitted to the Cox proportional
hazards regression model for multivariate analysis. Meaningless
variables were also further analyzed to determine the values of all
indicators following multivariate analysis. Categorical variables
were compared using the χ2 test or Fisher's exact tests.
OS was defined as the period from the date of the first diagnosis
to the date of mortality or the last follow-up. PFS was calculated
from the date of the first diagnosis to the date of disease
progression, or the last follow-up if the disease had not
progressed. Continuous variable is presented as the average value
(minimum to maximum). SPSS version 20.0 (IBM Corp.) was used to
perform the statistical analysis. P<0.05 was considered to
indicate a statistically significant value.
Results
Optimal cut-off values for the blood
test parameters
ROC curve analysis was used to determine the most
appropriate cut-off values for the complete blood cell parameters.
According to the ROC curve analysis, the cut-off point for NWR was
0.67. Therefore, 0.67 was selected as the cut-off value for NWR.
Similarly, the optimal points based on the ROC curves revealed
cut-off values of 2.85 for NLR, 37.23 for PWR, 166.56 for PLR,
0.074 for MWR, 0.31 for MLR and 0.24 for LWR. Consequently, these
parameters were categorized as optimal cut-off values.
Basic characteristics of patients
Clinical characteristics of all the patients are
shown in Table I. The median (range)
age of patients was 59.10 (33–79) years, and 128(47.8%) of them
were <60 years old. The study was comprised of 161 (60.1%) male
patients and 107 (39.9%) female patients. A total of 46 (17.2%) and
222 (82.8%) patients presented with TNM stages IIIB and IV,
respectively. Out of the total patients 225 (84.0%) were diagnosed
with adenocarcinoma and 43 (16.0%) were diagnosed with squamous
cell carcinoma. Of the 268 patients, 133 (49.6%) had never smoked
compared with 135 patients (50.4%) who were former or current
smokers. Patients with performance status 0, 1 or 2 accounted for
10.8, 78.0 and 11.2% of the patients, respectively. With 112
(41.8%) of the patients, the tumor was located on the left, whereas
with 156 (58.2%) of the patients, the tumor was located on the
right.
 | Table I.Characteristics of patients with
advanced non-small cell lung cancer. |
Table I.
Characteristics of patients with
advanced non-small cell lung cancer.
|
Characteristics | Patients (%) |
|---|
| Total number | 268 |
| Age |
|
| <60
years | 128 (47.8) |
| ≥60
years | 140 (52.2) |
| Sex |
|
|
Male | 161 (60.1) |
|
Female | 107 (39.9) |
| Stage |
|
|
III | 46 (17.2) |
| IV | 222 (82.8) |
| Histological
type |
|
|
Adenocarcinoma | 225 (84.0) |
|
Sqcc | 43 (16.0) |
| Smoking
history |
|
|
Never | 133 (49.6) |
|
Current/Previous | 135 (50.4) |
| Performance
status |
|
| 0 | 29 (10.8) |
| 1 | 209 (78.0) |
| 2 | 30 (11.2) |
| Tumor location |
|
|
Left | 112 (41.8) |
|
Right | 156 (58.2) |
Univariate and multivariate analysis
for PFS and OS
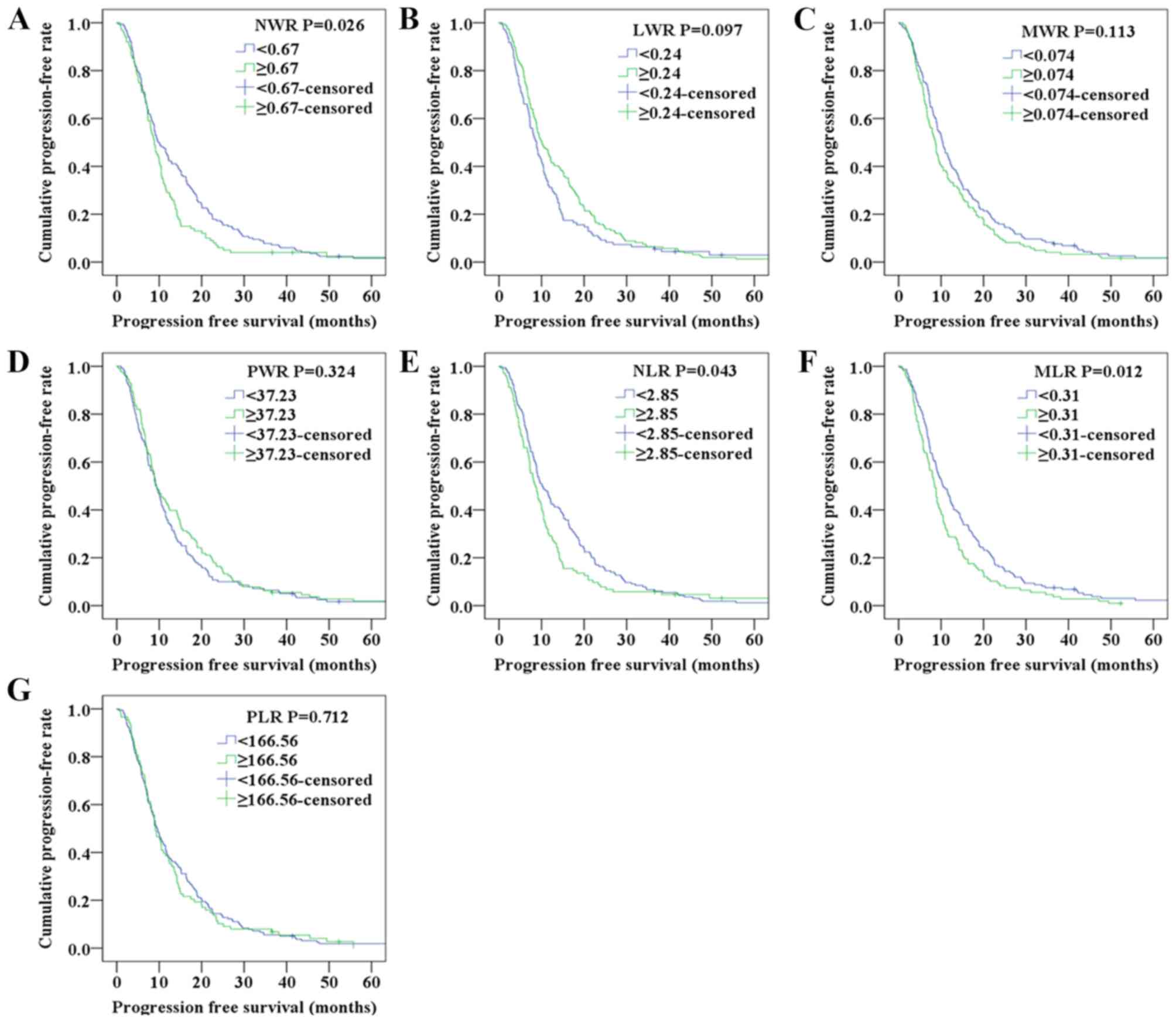
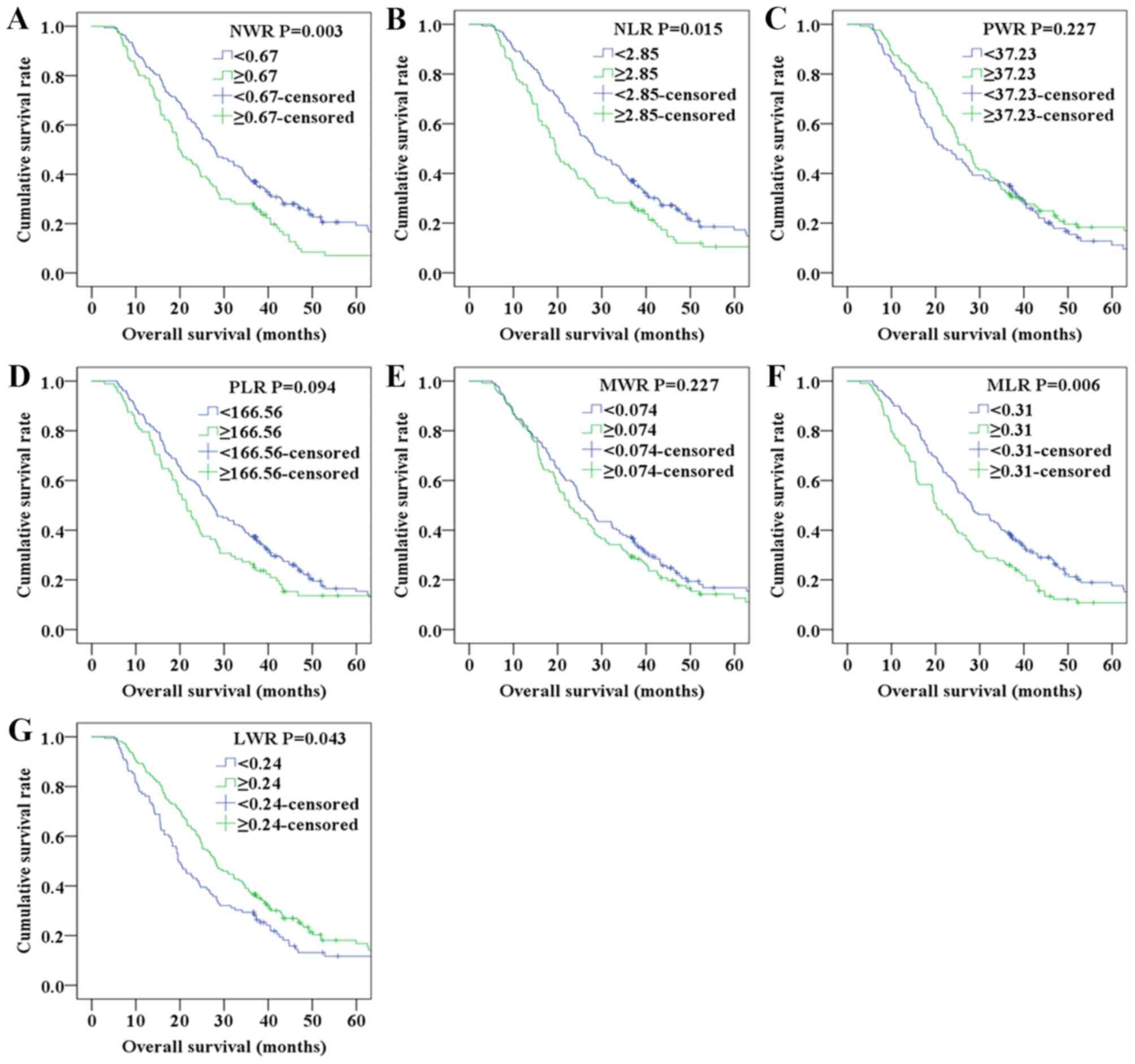
Kaplan-Meier analyses were performed to determine
the differences in PFS and OS among the blood test parameters
classified by the optimal cut-off values. The Kaplan-Meier survival
curves shown in Fig. 1 indicated
that the NWR and MLR values were associated with PFS, whereas the
survival curves shown in Fig. 2
indicated that elevated NWR, NLR, MLR and decreased LWR were
associated with poor OS.
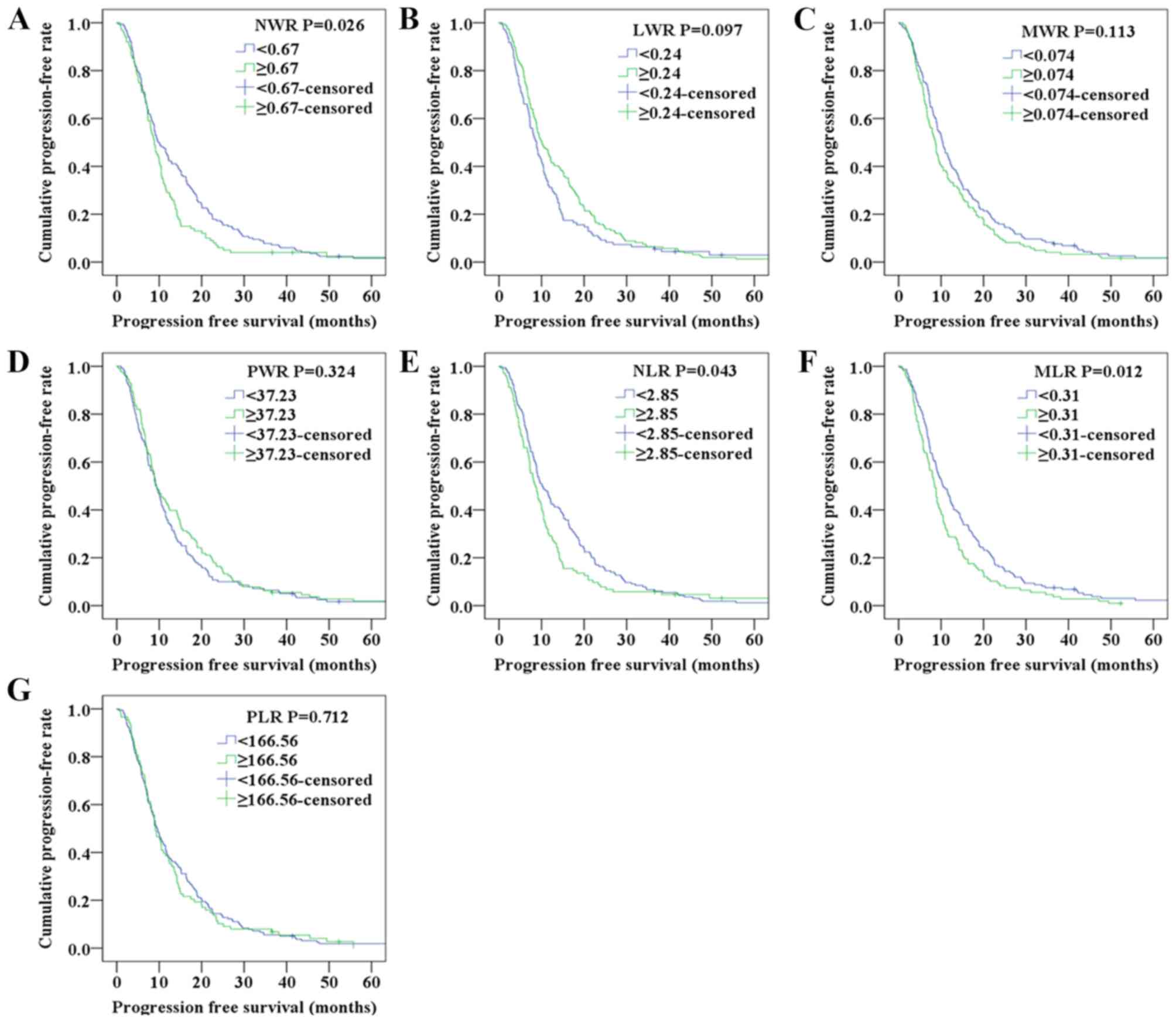 | Figure 1.Progression-free survival of patients
with non-small cell lung cancer according to (A) NWR, (B) LWR, (C)
MWR, (D) PWR, (E) NLR, (F) MLR and (G) PLR.LWR, lymphocyte/white
blood cell ratio; MLR, monocyte/lymphocyte ratio; MWR,
monocyte/white blood cell ratio; NLR, neutrophil/lymphocyte ratio;
NWR, neutrophil/white blood cell ratio; PLR, platelet/lymphocyte
ratio; PWR, platelet/white blood cell ratio. |
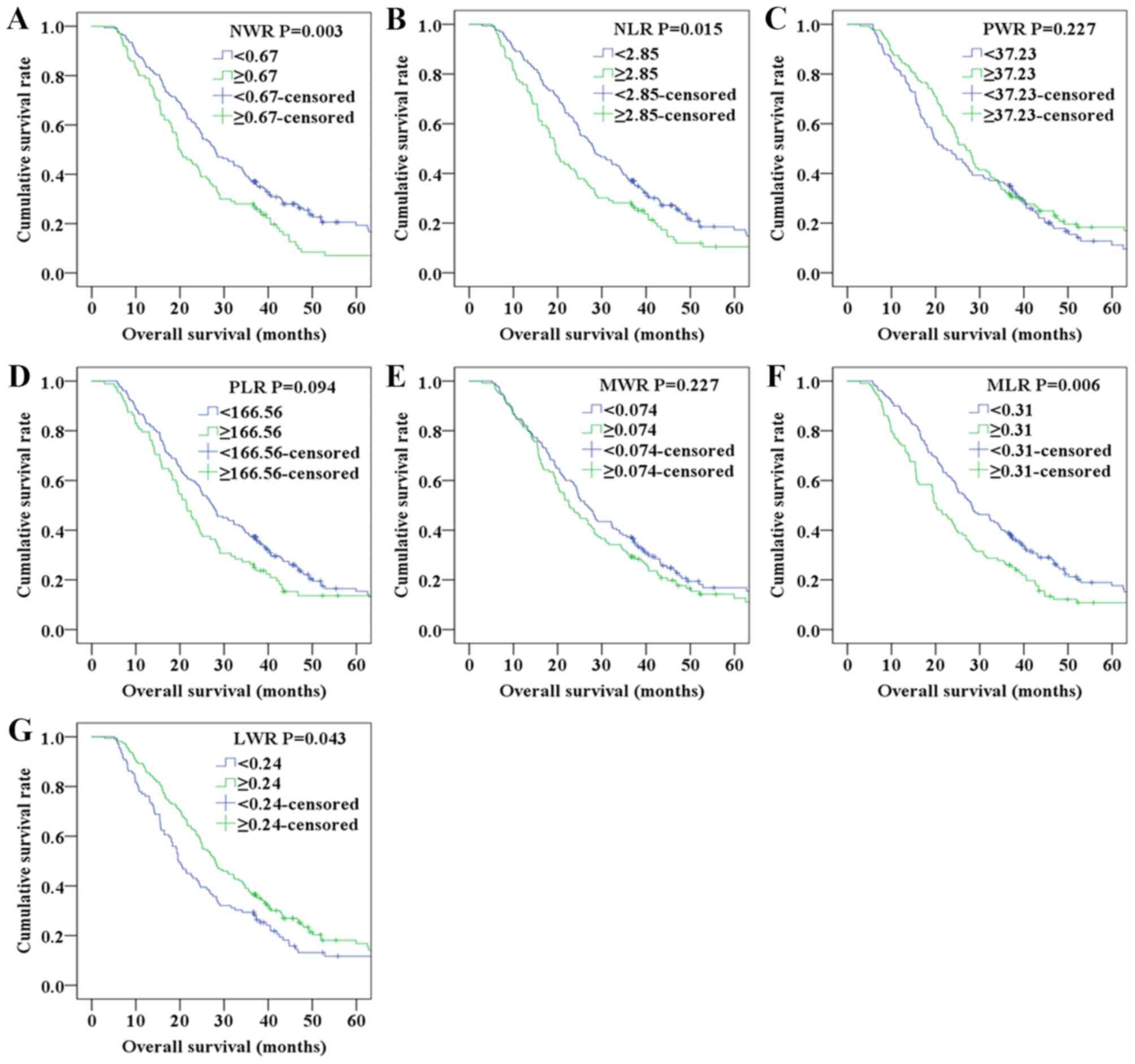 | Figure 2.Overall survival of patients with
NSCLC according to (A) NWR, (B) NLR, (C) PWR, (D) PLR, (E) MWR, (F)
MLR and (G) LWR.LWR, lymphocyte/white blood cell ratio; MLR,
monocyte/lymphocyte ratio; MWR, monocyte/white blood cell ratio;
NLR, neutrophil/lymphocyte ratio; NSCLC, non-small cell lung
cancer; NWR, neutrophil/white blood cell ratio; PLR,
platelet/lymphocyte ratio; PWR, platelet/white blood cell
ratio. |
As shown in Table
II, sex (P=0.038), histological type (P<0.0001), NWR
(P=0.026), NLR (P=0.044) and MLR (P=0.012) of the patients were
significantly associated with PFS according to the univariate
analysis. As presented in Table
III, histological type (P=0.003), NWR (P=0.003), NLR (P=0.015),
MLR (P=0.006) and LWR (P=0.043) were significantly associated with
OS in the univariate analysis. To determine the independent
predictors, further Cox multivariate analyses were performed.
Multivariate analysis demonstrated that histological type [hazard
ratio (HR)=0.577; 95% confidence interval (CI)=0.404–0.822;
P=0.002] was an independent factor for PFS (Table II). Correspondingly, histological
type (HR=0.582; 95% CI=0.401–0.846; P=0.005), NWR (HR=0.673; 95%
CI=0.511–0.888; P=0.005), NLR (HR=0.703; 95% CI=0.530–0.931;
P=0.014), MLR (HR=0.669; 95% CI=0.504–0.889; P=0.006) and LWR
(HR=1.351; 95% CI=1.022–1.785; P=0.034) were independent prognostic
factors for OS (Table III).
 | Table II.Univariate and multivariate analyses
of clinical characteristics for progression-free survival of
patients with advanced non-small-cell lung cancer. |
Table II.
Univariate and multivariate analyses
of clinical characteristics for progression-free survival of
patients with advanced non-small-cell lung cancer.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variables | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age (<60/≥60
years) | 1.181 | 0.925–1.507 | 0.182 | 1.224 | 0.955–1.569 | 0.111 |
| Sex
(Male/female) | 0.766 | 0.595–0.985 | 0.038 | 0.786 | 0.566–1.092 | 0.152 |
| Stage (III/IV) | 0.866 | 0.628–1.194 | 0.380 | 0.854 | 0.615–1.186 | 0.346 |
| Histological type
(Adeno/sqcc) | 0.540 | 0.387–0.753 | 0.000 | 0.577 | 0.404–0.822 | 0.002 |
| Smoking history
(None/yes) | 0.815 | 0.639–1.041 | 0.101 | 0.999 | 0.715–1.395 | 0.995 |
| ECOG PS
(0+1/2) | 0.856 | 0.581–1.262 | 0.433 | 0.874 | 0.588–1.298 | 0.504 |
| Tumor location
(Left/right) | 0.977 | 0.765–1.249 | 0.855 | 1.000 | 0.780–1.280 | 0.997 |
| NWR
(≥0.67/<0.67) | 0.750 | 0.582–0.967 | 0.026 | 0.793 | 0.609–1.032 | 0.085 |
| NLR
(≥2.85/<2.85) | 0.772 | 0.601–0.993 | 0.044 | 0.835 | 0.643–1.084 | 0.175 |
| PWR
(≥37.23/<37.23) | 1.129 | 0.886–1.439 | 0.325 | 1.124 | 0.867–1.456 | 0.378 |
| PLR
(≥166.56/<166.56) | 0.953 | 0.736–1.234 | 0.713 | 1.060 | 0.806–1.394 | 0.676 |
| MWR
(≥0.074/<0.074) | 0.822 | 0.645–1.048 | 0.114 | 0.901 | 0.698–1.162 | 0.422 |
| MLR
(≥0.31/<0.31) | 0.728 | 0.568–0.933 | 0.012 | 0.798 | 0.611–1.042 | 0.098 |
| LWR
(≥0.24/<0.24) | 1.233 | 0.962–1.579 | 0.098 | 1.135 | 0.876–1.472 | 0.338 |
 | Table III.Univariate and multivariate analyses
of clinical characteristics for overall survival of patients with
advanced non-small cell lung cancer. |
Table III.
Univariate and multivariate analyses
of clinical characteristics for overall survival of patients with
advanced non-small cell lung cancer.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variables | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age (<60/≥60
years) | 1.172 | 0.902–1.523 | 0.234 | 1.248 | 0.955–1.632 | 0.105 |
| Sex
(Male/female) | 0.837 | 0.641–1.093 | 0.192 | 0.827 | 0.560–1.222 | 0.340 |
| Stage (III/IV) | 0.975 | 0.682–1.393 | 0.889 | 1.042 | 0.724–1.500 | 0.824 |
| Histological type
(Adeno/sqcc) | 0.577 | 0.415–0.801 | 0.003 | 0.582 | 0.401–0.846 | 0.005 |
| Smoking history
(None/yes) | 0.882 | 0.680–1.145 | 0.345 | 1.116 | 0.753–1.653 | 0.586 |
| ECOG PS
(0+1/2) | 1.223 | 0.806–1.854 | 0.344 | 1.316 | 0.861–2.012 | 0.204 |
| Tumor location
(Left/right) | 1.003 | 0.769–1.308 | 0.982 | 0.997 | 0.763–1.302 | 0.981 |
| NWR
(≥0.67/<0.67) | 0.669 | 0.512–0.875 | 0.003 | 0.673 | 0.511–0.888 | 0.005 |
| NLR
(≥2.85/<2.85) | 0.718 | 0.549–0.938 | 0.015 | 0.703 | 0.530–0.931 | 0.014 |
| PWR
(≥37.23/<37.23) | 1.174 | 0.904–1.525 | 0.228 | 1.172 | 0.889–1.544 | 0.260 |
| PLR
(≥166.56/<166.56) | 0.790 | 0.599–1.042 | 0.095 | 0.789 | 0.594–1.047 | 0.101 |
| MWR
(≥0.074/<0.074) | 0.852 | 0.656–1.106 | 0.228 | 0.863 | 0.657–1.132 | 0.287 |
| MLR
(≥0.31/<0.31) | 0.692 | 0.531–0.901 | 0.006 | 0.669 | 0.504–0.889 | 0.006 |
| LWR
(≥0.24/<0.24) | 1.318 | 1.008–1.723 | 0.043 | 1.351 | 1.022–1.785 | 0.034 |
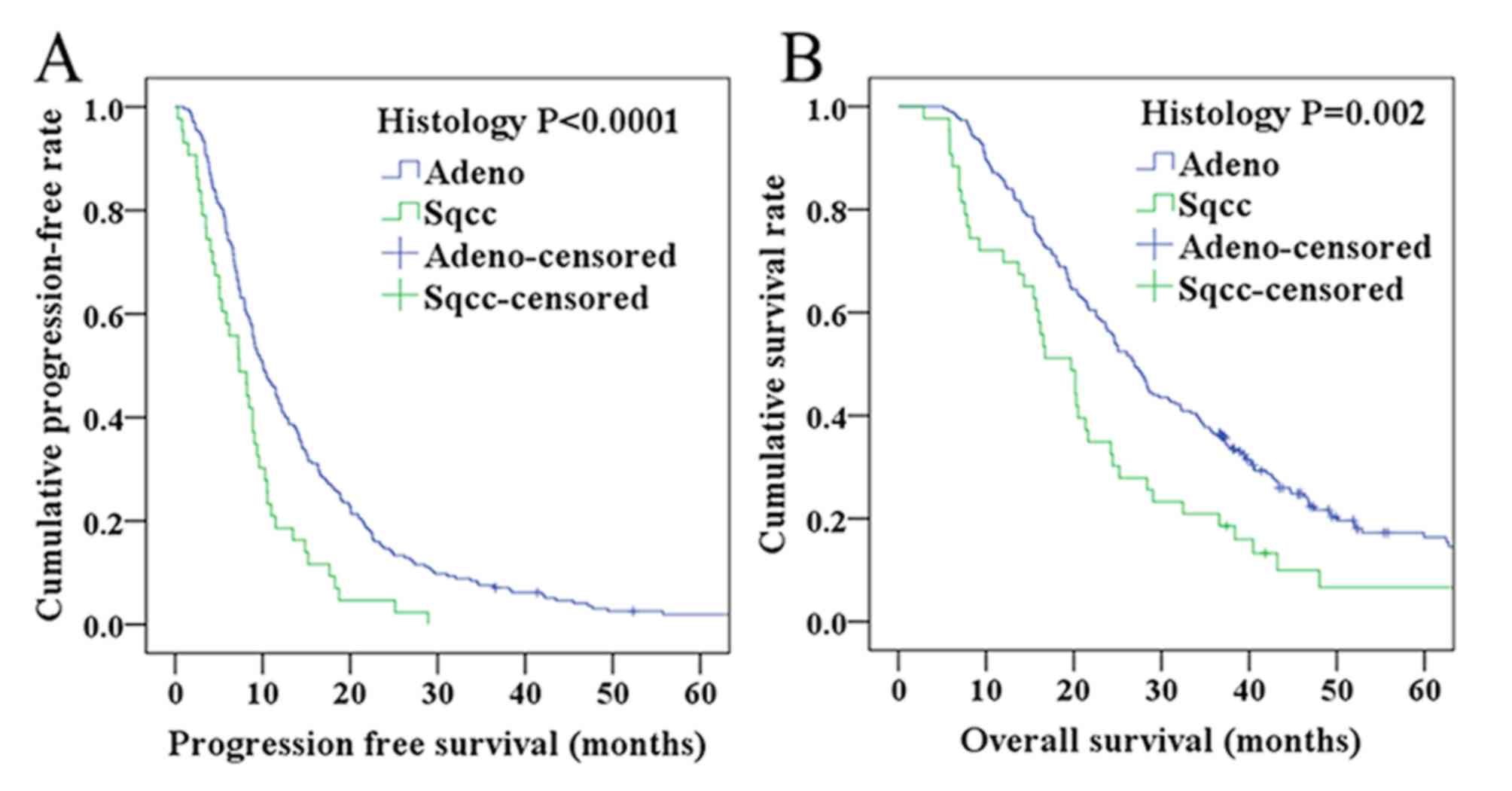
PFS and OS according to histological
type
As shown in Tables
II and III, multivariate
analysis revealed that histological type was significantly
associated with PFS and OS (HR=0.577; 95% CI=0.404–0.822; P=0.002
for PFS, and HR=0.582; 95% CI=0.401–0.846, and P=0.005 for OS). To
analyze these results further, graphical representations of the PFS
and OS of different pathological types were prepared according to
histology. In the squamous cell carcinoma group, the 1-, 2-and
3-year PFS rates were 18.6, 4.7 and 0.0% respectively, whereas in
the adenocarcinoma group, the PFS rates were 42.7, 14.7 and 7.4%
(Fig. 3A). Correspondingly, the 1-,
2- and 3-year OS rates were 69.8, 34.9 and 20.9% in the squamous
cell carcinoma group, and 85.8, 56.4 and 36.4% in the
adenocarcinoma group (Fig. 3B).
Taken together, these results demonstrated that the PFS and OS
rates in the adenocarcinoma group were longer compared with
patients in the squamous cell carcinoma group.
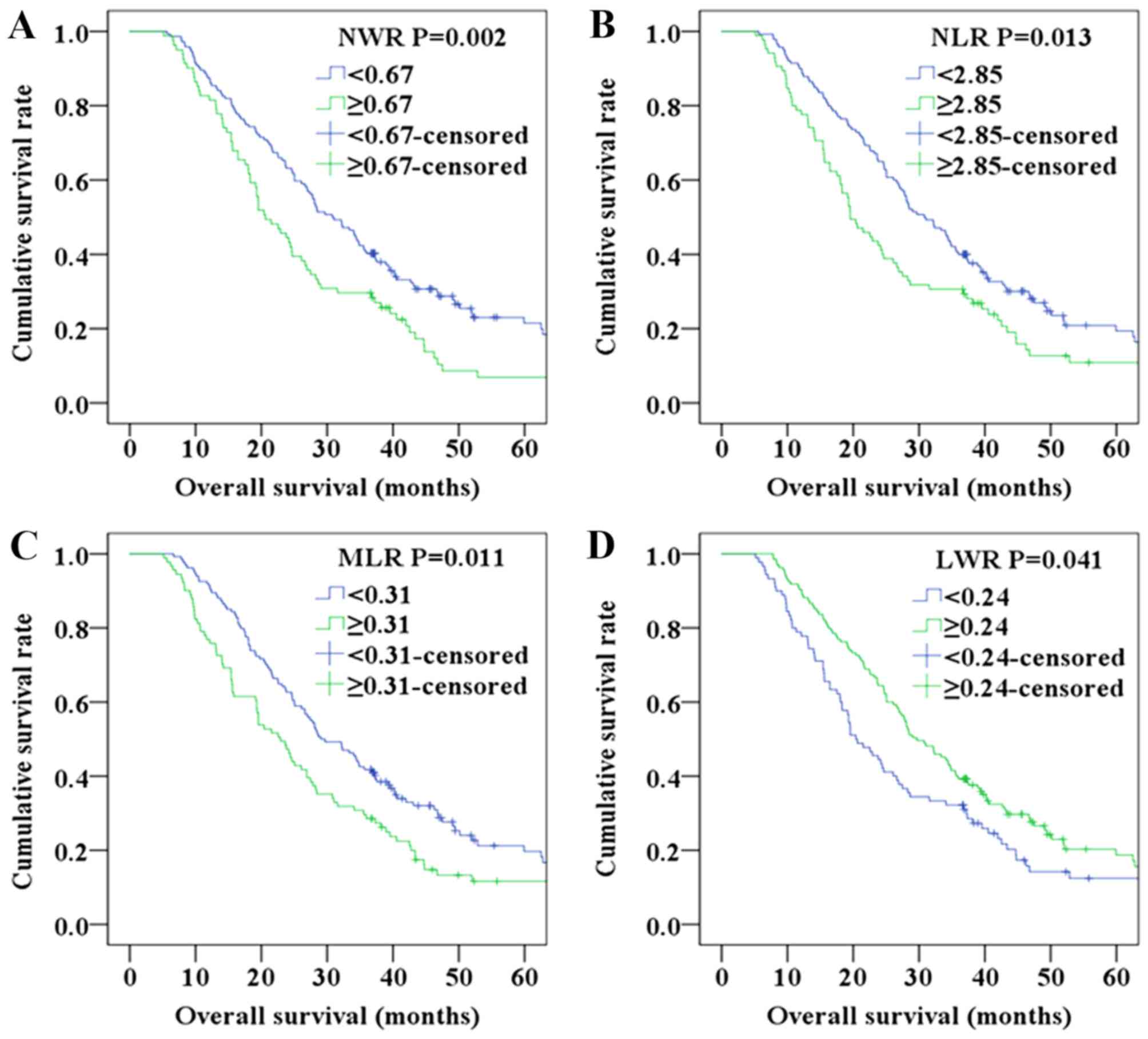
Prognostic factors of patients with
adenocarcinoma according to NWR, NLR, MLR and LWR
Further analyses were performed in subgroups
(adenocarcinoma and squamous cell carcinoma). Since the number of
patients with squamous cell carcinoma was relatively small, only
adenocarcinoma was analyzed. Patients with NWR<0.67,
NLR<2.85, MLR<0.31 and LWR≥0.24,were found to exhibit a
higher OS compared with those with NWR≥0.67, NLR≥2.85, MLR≥0.31 and
LWR<0.24 in the adenocarcinoma subgroup (P=0.002 for NWR,
Fig. 4A; P=0.013 for NLR, Fig. 4B; P=0.011, Fig. 4C; P=0.041, Fig. 4D).
Association between blood test
parameters and clinicopathological variables
The associations between NWR, NLR, MLR, LWR and
clinical factors of the patients with NSCLC are shown in Tables IV and V. A total of 168 (62.7%) patients were in
the NWR<0.67 group and 100 (37.3%) patients were in the NWR≥0.67
group, whereas 165 (61.6%) patients were in the NLR<2.85 group
and 103 (38.4%) patients were in the NLR≥2.85 group. In addition,
160 (59.7%) patients were in the MLR<0.31 group and 108 (40.3%)
patients were in the MLR≥0.31 group, and 109 (40.7%) patients were
in the LWR<0.24 group, whereas 159 (59.3%) patients were in the
LWR≥0.24 group. The present study revealed that NLR and MLR were
markedly associated with sex, whereas LWR was closely associated
with sex and ECOG performance status.
 | Table IV.Association between NWR, NLR and
clinical parameters of patients with non-small cell lung
cancer. |
Table IV.
Association between NWR, NLR and
clinical parameters of patients with non-small cell lung
cancer.
|
| NWR |
| NLR |
|
|---|
|
|
|
|
|
|
|---|
| Variables | <0.67 | ≥0.67 | P-value | <2.85 | ≥2.85 | P-value |
|---|
| Age |
|
|
|
|
|
|
| <60
years | 77 | 51 |
| 75 | 53 |
|
| ≥60
years | 91 | 49 | 0.413 | 90 | 50 | 0.330 |
| Sex |
|
|
|
|
|
|
|
Male | 95 | 66 |
| 91 | 70 |
|
|
Female | 73 | 34 | 0.156 | 74 | 33 | 0.041 |
| Stage |
|
|
|
|
|
|
|
III | 26 | 20 |
| 28 | 18 |
|
| IV | 142 | 80 | 0.403 | 137 | 85 | 0.915 |
| Histological
type |
|
|
|
|
|
|
|
Adeno | 144 | 81 |
| 140 | 85 |
|
|
Sqcc | 24 | 19 | 0.308 | 25 | 18 | 0.612 |
| Smoking
history |
|
|
|
|
|
|
|
None | 86 | 47 |
| 85 | 48 |
|
|
Yes | 82 | 53 | 0.507 | 80 | 55 | 0.434 |
| ECOG PS |
|
|
|
|
|
|
| 0 | 153 | 85 |
| 151 | 87 |
|
|
Others | 15 | 15 | 0.161 | 14 | 16 | 0.110 |
| Tumor location |
|
|
|
|
|
|
|
Left | 70 | 42 |
| 67 | 45 |
|
|
Right | 98 | 58 | 0.957 | 98 | 58 | 0.619 |
 | Table V.Association between MLR, LWR and
clinical parameters of patients with non-small cell lung
cancer. |
Table V.
Association between MLR, LWR and
clinical parameters of patients with non-small cell lung
cancer.
|
| MLR |
| LWR |
|
|---|
|
|
|
|
|
|
|---|
| Variables | <0.31 | ≥0.31 | P-value | <0.24 | ≥0.24 | P-value |
|---|
| Age |
|
|
|
|
|
|
| <60
years | 72 | 56 |
| 54 | 74 |
|
| ≥60
years | 88 | 52 | 0.271 | 55 | 85 | 0.629 |
| Sex |
|
|
|
|
|
|
|
Male | 86 | 75 |
| 75 | 86 |
|
|
Female | 74 | 33 | 0.011 | 34 | 73 | 0.016 |
| Stage |
|
|
|
|
|
|
|
III | 30 | 16 |
| 18 | 28 |
|
| IV | 130 | 92 | 0.509 | 91 | 131 | 0.870 |
| Histological
type |
|
|
|
|
|
|
|
Adeno | 134 | 91 |
| 90 | 135 |
|
|
Sqcc | 26 | 17 | 1.000 | 19 | 24 | 0.615 |
| Smoking
history |
|
|
|
|
|
|
|
None | 83 | 50 |
| 49 | 84 |
|
|
Yes | 77 | 58 | 0.370 | 60 | 75 | 0.205 |
| ECOG PS |
|
|
|
|
|
|
| 0 | 146 | 92 |
| 91 | 147 |
|
|
Others | 14 | 16 | 0.166 | 18 | 12 | 0.022 |
| Tumor location |
|
|
|
|
|
|
|
Left | 60 | 52 |
| 49 | 63 |
|
|
Right | 100 | 56 | 0.083 | 60 | 96 | 0.385 |
Discussion
Although all 268 patients with advanced NSCLC in
this study undergo active anticancer treatment, including
chemotherapy, radiotherapy, targeted therapy and immunotherapy,
recurrence and metastasis are inevitable, thus leading to treatment
failure. Of the 268 patients recruited in the present study, all
developed recurrence and metastasis. The purpose of the present
study was to reveal the association between blood test parameters
prior to disease treatment and the prognosis of patients with
advanced NSCLC. Previously, significant attention has been paid to
the underlying mechanism that links malignancies with inflammation
(4). NLR, PLR and LWR, as
cancer-associated inflammatory variables, have been widely studied,
and are regarded as important prognostic factors in multiple types
of malignancy, including breast (13), lung (8,14),
gastric (15,16) and colorectal cancer (17). Recently, an increasing number of
studies has evaluated the association between complete blood
parameters and patient prognosis. Moreover, high NWR and MLR have
been identified as independent prognostic factors in curatively
resected NSCLC (9,10,18,19). The
present study is, to the best of our knowledge, the first attempt
to address the issue of the prognostic significance of complete
blood parameters in patients with advanced NSCLC.
Lymphocytes fulfill a crucial role in host immune
response and possess potent anticancer activities that lead to
inhibition of tumor cell proliferation and metastasis (20,21). A
previous study demonstrated that a decrease in the level of
lymphocytes was able to induce the release of several inhibitory
immunological mediators, such as transforming growth
factor-bandinterleukin-10 (22). It
is now widely considered that increased lymphocyte levels are
associated with improved clinical outcomes in various types of
cancer (20,23). Consistent with these results, high
NLR and MLR, and low LWR, were associated with poor prognosis in
patients with advanced NSCLC in the present study.
It has previously been reported that high levels of
monocytes are associated with poor prognosis of various tumor
types, including rectal, breast and prostate cancer (24–26).
Monocytes are an important component in the inflammatory
microenvironment that stimulate tumor cell growth, promote
angiogenesis and suppress the host anticancer immune response
(27,28). Monocytes also influence the
development of malignant cells by producing pro-inflammatory
cytokines, including tumor necrosis factor, interleukin-1 and
interleukin-6 (28). On the other
hand, cytokines and chemokines produced by tumor cells may induce
the differentiation of monocytes into tumor-associated macrophages
(29). Tumor-associated macrophages
are able to weaken the antitumor immune response, stimulate
migration and promote metastasis of tumor cells (30). In the present study, elevated MLR was
identified as an independent factor for poor prognosis in advanced
NSCLC, a finding that was consistent with previous research.
Peripheral neutrophils are recognized as markers of
acute and chronic inflammation (31). It has been reported that neutrophils
are able to produce vascular endothelial growth factor and matrix
metalloproteinase-9, which can promote tumor angiogenesis and
progression (32,33). In addition, elevated neutrophil
levels may inhibit the antitumor system by influencing the activity
of natural killer cells, lymphocytes and activated T cells
(34–37). The combination of neutrophilia and
lymphocytopenia could be considered as a useful marker that
reflects the balance between inflammation and immune reaction. A
high NLR level has long been demonstrated to be associated with
poor prognosis of a variety of tumor types, such as colorectal
cancer and renal cell carcinoma (38). Meta-analysis studies have revealed
that elevated NLR may be associated with poor prognosis in NSCLC
(6,39). In the present study, it was also
demonstrated that NLR was an independent prognostic factor in
advanced NSCLC; however, the underlying mechanisms require further
study.
Previous studies have suggested that thrombocytosis
may be linked to poor clinical outcomes in various types of cancer,
such as gastric cancer (40,41). Platelets are involved in the
proliferation and adhesion of tumor cells by activating and
secreting growth factors, thereby promoting the occurrence and
invasion of tumors (42). In studies
concerned with NSCLC, PLR was found to be an independent risk
factor influencing the prognosis of patients (43). In the present study, PLR did not
achieve statistical significance, and this may be attributed to a
relatively small sample size, although the underlying reasons still
need to be elucidated.
The current study demonstrated that sex,
histological type, NWR, NLR and MLR were associated with PFS in
patients with advanced NSCLC. However, only histological type was
an independent prognostic factor for PFS. In addition, this study
revealed that histological type, NWR, NLR, MLR and LWR were
independent prognostic factors for OS in patients with advanced
NSCLC. In addition, these four indicators (NWR, NLR, MLR and LWR)
were associated with OS in patients with adenocarcinoma. It should
be noted that it was not possible to analyze these in squamous cell
carcinoma due to the insufficient number of patients in this study.
Therefore, the association between these four indicators and
squamous cell carcinoma requires further study in the future. It
was also observed that the prognosis of adenocarcinoma was better
compared with that of squamous cell carcinoma, with regards to PFS
and OS.
However, there were certain limitations associated
with the present study. Firstly, this study was performed in a
single medical center and only 268 patients were included.
Therefore, analyzing a large sample associated with a clinical
multicenter is required to confirm the predictive value of the
parameters measured in this study. Secondly, the cut-off values of
the present and previous studies were different (9,14). Thus,
a reasonable cut-off value should be identified to predict the
outcomes of advanced NSCLC. Finally, the prognosis of advanced
NSCLC is affected by a variety of factors, and the influence of
those factors should be excluded as far as possible in subsequent
studies.
In conclusion, in the present study, high NWR, NLR
and MLR values, and a low LWR value, were associated with poor
prognosis in patients with advanced NSCLC. Furthermore, these
indicators were identified to be independent prognostic factors in
advanced NSCLC.
Acknowledgements
Not applicable.
Funding
The present study was funded by the Natural Science
Foundation of Shandong Province (grant no. ZR2017MH062) and the
Science and Technology for People's Livelihood Project of Qingdao
(grant no. 17-3-3-33-nsh).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
LW, JW, LF and ZY acquired the data, performed the
literature review and designed the present study. HS, WZ and SD
analyzed the data. All authors were involved in writing the initial
manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The Affiliated Hospital of Qingdao University
(approval no. QYFYW2LL 25620). Consent to participate was provided
from patients or their families via telephone.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dela Cruz CS, Tanoue LT and Matthay RA:
Lung cancer: Epidemiology, etiology, and prevention. Clin Chest
Med. 32:605–644. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Herbst RS, Heymach JV and Lippman SM: Lung
cancer. N Engl J Med. 359:1367–1380. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moro-Sibilot D, Smit E, de Castro Carpeño
J, Lesniewski- Kmak K, Aerts J, Villatoro R, Kraaij K, Nacerddine
K, Dyachkova Y, Smith KT, et al: Outcomes and resource use of
non-small-cell lung cancer (NSCLC) patients treated with first-line
platinum-based chemotherapy across Europe: FRAME prospective
observational study. Lung Cancer. 88:215–222. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Coussens LM and Werb Z: Inflammation and
cancer. Nature. 420:860–867. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McMillan DC: Systemic inflammation,
nutritional status and survival in patients with cancer. Curr Opin
Clin Nutr Metab Care. 12:223–226. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gu XB, Tian T, Tian XJ and Zhang XJ:
Prognostic significance of neutrophil-to-lymphocyte ratio in
non-small-cell lung cancer: A meta-analysis. Sci Rep. 5:124932015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang H, Gao L, Zhang B, Zhang L and Wang
C: Prognostic value of platelet to lymphocyte ratio in
non-small-cell lung cancer: A systematic review and meta-analysis.
Sci Rep. 6:226182016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li W, Ma G, Wu Q, Deng Y, Liu Y and Wang
J: Prognostic value of lymphocyte-to-monocyte ratio among Asian
lung cancer patients: A systematic review and meta-analysis.
Oncotarget. 8:110606–110613. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yuan C, Li N, Mao X, Liu Z, Ou W and Wang
SY: Elevated pretreatment neutrophil/white blood cell ratio and
monocyte/lymphocyte ratio predict poor survival in patients with
curatively resected non-small-cell lung cancer: Results from a
large cohort. Thorac Cancer. 8:350–358. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Feng F, Sun L, Zheng G, Liu S, Liu Z, Xu
G, Guo M, Lian X, Fan D and Zhang H: Low lymphocyte-to-white blood
cell ratio and high monocyte-to-white blood cell ratio predict poor
prognosis in gastric cancer. Oncotarget. 8:5281–5291. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Groome PA, Bolejack V, Crowley JJ, Kennedy
C, Krasnik M, Sobin LH and Goldstraw P; IASLC International Staging
Committee; Cancer Research and Biostatistics; Observers to the
Committee; Participating Institutions, : The IASLC Lung Cancer
Staging Project: Validation of the proposals for revision of the T,
N, and M descriptors and consequent stage groupings in the
forthcoming (seventh) edition of the TNM classification of
malignant tumours. J Thorac Oncol. 2:694–705. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Losada B, Guerra JA, Malón D, Jara C,
Rodriguez L and Del Barco S: Pretreatment neutrophil/lymphocyte,
platelet/lymphocyte, lymphocyte/monocyte, and neutrophil/monocyte
ratios and outcome in elderly breast cancer patients. Clin Transl
Oncol. 21:855–863. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang L, Liang D, Xu X, Jin J, Li S, Tian
G, Gao Z, Liu C and He Y: The prognostic value of neutrophil to
lymphocyte and platelet to lymphocyte ratios for patients with lung
cancer. Oncol Lett. 14:6449–6456. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ma JY and Liu Q: Clinicopathological and
prognostic significance of lymphocyte to monocyte ratio in patients
with gastric cancer: A meta-analysis. Int J Surg. 50:67–71. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang Y, Lu JJ, Du YP, Feng CX, Wang LQ
and Chen MB: Prognostic value of neutrophil-to-lymphocyte ratio and
platelet-to-lymphocyte ratio in gastric cancer. Medicine
(Baltimore). 97:e01442018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ying HQ, Deng QW, He BS, Pan YQ, Wang F,
Sun HL, Chen J, Liu X and Wang SK: The prognostic value of
preoperative NLR, d-NLR, PLR and LMR for predicting clinical
outcome in surgical colorectal cancer patients. Med Oncol.
31:3052014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cananzi FCM, Minerva EM, Samà L, Ruspi L,
Sicoli F, Conti L, Fumagalli Romario U and Quagliuolo VL:
Preoperative monocyte-to-lymphocyte ratio predicts recurrence in
gastrointestinal stromal tumors. J Surg Oncol. 119:12–20. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Feng F, Tian Y, Liu S, Zheng G, Liu Z, Xu
G, Guo M, Lian X, Fan D and Zhang H: Combination of PLR, MLR, MWR,
and tumor size could significantly increase the prognostic value
for gastrointestinal stromal tumors. Medicine (Baltimore).
95:e32482016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Quigley DA and Kristensen V: Predicting
prognosis and therapeutic response from interactions between
lymphocytes and tumor cells. Mol Oncol. 9:2054–2062. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang SC, Chou JF, Strong VE, Brennan MF,
Capanu M and Coit DG: Pretreatment neutrophil to lymphocyte ratio
independently predicts disease-specific survival in resectable
gastroesophageal junction and gastric adenocarcinoma. Ann Surg.
263:292–297. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Salazar-Onfray F, López MN and
Mendoza-Naranjo A: Paradoxical effects of cytokines in tumor immune
surveillance and tumor immune escape. Cytokine Growth Factor Rev.
18:171–182. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang L, Conejo-Garcia JR, Katsaros D,
Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H,
Schlienger K, Liebman MN, et al: Intratumoral T cells, recurrence,
and survival in epithelial ovarian cancer. N Engl J Med.
348:203–213. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang LN, Xiao W, OuYang PY, You K, Zeng
ZF, Ding PR, Pan ZZ, Xu RH and Gao YH: The prognostic impact of
preoperative blood monocyte count in pathological T3N0M0 rectal
cancer without neoadjuvant chemoradiotherapy. Tumour Biol.
36:8213–8219. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wen J, Ye F, Huang X, Li S, Yang L, Xiao X
and Xie X: Prognostic significance of preoperative circulating
monocyte count in patients with breast cancer: Based on a Large
Cohort Study. Medicine (Baltimore). 94:e22662015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lindholm PF, Sivapurapu N, Jovanovic B and
Kajdacsy-Balla A: Monocyte-induced prostate cancer cell invasion is
mediated by chemokine ligand 2 and nuclear factor-κB activity. J
Clin Cell Immunol. 6:3082015.PubMed/NCBI
|
|
27
|
Gabrilovich DI and Nagaraj S:
Myeloid-derived suppressor cells as regulators of the immune
system. Nat Rev Immunol. 9:162–174. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mantovani A, Schioppa T, Porta C, Allavena
P and Sica A: Role of tumor-associated macrophages in tumor
progression and invasion. Cancer Metastasis Rev. 25:315–322. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ikemoto S, Sugimura K, Yoshida N, Wada S,
Yamamoto K and Kishimoto T: TNF alpha, IL-1 beta and IL-6
production by peripheral blood monocytes in patients with renal
cell carcinoma. Anticancer Res. 20:317–321. 2000.PubMed/NCBI
|
|
30
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kolaczkowska E and Kubes P: Neutrophil
recruitment and function in health and inflammation. Nat Rev
Immunol. 13:159–175. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tan KW, Chong SZ, Wong FH, Evrard M, Tan
SM, Keeble J, Kemeny DM, Ng LG, Abastado JP and Angeli V:
Neutrophils contribute to inflammatory lymphangiogenesis by
increasing VEGF-A bioavailability and secreting VEGF-D. Blood.
122:3666–3677. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bausch D, Pausch T, Krauss T, Hopt UT,
Fernandez-del- Castillo C, Warshaw AL, Thayer SP and Keck T:
Neutrophil granulocyte derived MMP-9 is a VEGF independent
functional component of the angiogenic switch in pancreatic ductal
adenocarcinoma. Angiogenesis. 14:235–243. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kay HD and Smith DL: Regulation of human
lymphocyte-mediated natural killer (NK) cell activity. I.
Inhibition in vitro by peripheral blood granulocytes. J Immunol.
130:475–483. 1983.PubMed/NCBI
|
|
35
|
Petrie HT, Klassen LW and Kay HD:
Inhibition of human cytotoxic T lymphocyte activity in vitro by
autologous peripheral blood granulocytes. J Immunol. 134:230–234.
1985.PubMed/NCBI
|
|
36
|
el-Hag A and Clark RA: Immunosuppression
by activated human neutrophils. Dependence on the myeloperoxidase
system. J Immunol. 139:2406–2413. 1987.PubMed/NCBI
|
|
37
|
Shau HY and Kim A: Suppression of
lymphokine-activated killer induction by neutrophils. J Immunol.
141:4395–4402. 1988.PubMed/NCBI
|
|
38
|
Templeton AJ, McNamara MG, Šeruga B,
Vera-Badillo FE, Aneja P, Ocaña A, Leibowitz-Amit R, Sonpavde G,
Knox JJ, Tran B, et al: Prognostic role of neutrophil-to-lymphocyte
ratio in solid tumors: A systematic review and meta-analysis. J
Natl Cancer Inst. 106:dju1242014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Peng B, Wang YH, Liu YM and Ma LX:
Prognostic significance of the neutrophil to lymphocyte ratio in
patients with non-small-cell lung cancer: A systemic review and
meta-analysis. Int J Clin Exp Med. 8:3098–3106. 2015.PubMed/NCBI
|
|
40
|
Xin-Ji Z, Yong-Gang L, Xiao-Jun S, Xiao-Wu
C, Dong Z and Da-Jian Z: The prognostic role of neutrophils to
lymphocytes ratio and platelet count in gastric cancer: A
meta-analysis. Int J Surg. 21:84–91. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Rachidi S, Metelli A, Riesenberg B, Wu BX,
Nelson MH, Wallace C, Paulos CM, Rubinstein MP, Garrett-Mayer E,
Hennig M, et al: Platelets subvert T cell immunity against cancer
via GARP-TGFβ axis. Sci Immunol. 2:eaai79112017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Majeti BK, Lee JH, Simmons BH and Shojaei
F: VEGF is an important mediator of tumor angiogenesis in malignant
lesions in a genetically engineered mouse model of lung
adenocarcinoma. BMC Cancer. 13:2132013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Qiang G, Liang C, Xiao F, Yu Q, Wen H,
Song Z, Tian Y, Shi B, Guo Y and Liu D: Prognostic significance of
platelet-to-lymphocyte ratio in non-small-cell lung cancer: A
meta-analysis. Onco Targets Ther. 9:869–876. 2016. View Article : Google Scholar : PubMed/NCBI
|