Introduction
PTCL is a rare type of NHL that arises from mature
T-cells. PTCL-NOS is a heterogeneous group comprised of
predominantly nodal T-cell lymphomas that do not fit the criteria
for the other subtypes of PTCL and carry a poor prognosis (1). Management is often challenging due to
advanced-stage detection and resistance to standard chemotherapy.
PTCL-NOS commonly affects systemic lymph nodes; however, extra
nodal sites such as the liver, spleen, lungs, pancreas, and bone
marrow are rare (2). At the same
time, there are a few case reports of primary liver involvement in
PTCL (3,4); however, there have been no documented
cases of PTCL with primary pancreatic involvement. Here, we report
an atypical case of primary pancreatic PTCL-NOS with secondary
involvement of the liver presenting as AP without peripheral
lymphadenopathy.
Case report
A 55-year-old male with no known medical history
presented to the emergency room in November 2022 at Jacobi Medical
center, with epigastric pain, nausea, non-bloody non-bilious
vomiting, jaundice, and unquantifiable weight loss. He had no
history of tobacco, alcohol, recreational drug use, abdominal
surgeries, and no family history of gastrointestinal malignancy.
Vital signs were within normal limits. The physical exam was
remarkable for scleral icterus, generalized yellowish skin
discoloration, and epigastric tenderness. Laboratory workup showed
a white blood cell count of 1.09/nl (normal: 3.90–10.60/nl),
absolute neutrophil count of 0.58/nl (normal: 1.90–8.70/nl),
absolute lymphocyte count of 0.29/nl (normal: 0.65–4.20/nl), and
platelet count 9/nl (normal: 150-440/nl). The liver function tests
revealed a cholestatic pattern, with elevated levels of alanine
aminotransferase 85 U/l (normal: 1–40 U/l), aspartate
aminotransferase 146 U/l (normal: 1–40 U/l), alkaline phosphatase
225 U/l (40–129 U/l), total bilirubin 31 mg/dl (normal: 0.1–0.3
mg/dl), and direct bilirubin 24 mg/dl (normal: 0.1–0.3 mg/dl).
Lipase and lactate dehydrogenase (LDH) were 876 U/l (normal: 7–60
U/l) and 805 U/l (normal: 100–210 U/l), respectively. Serologic
tests, including human immunodeficiency virus, syphilis, and
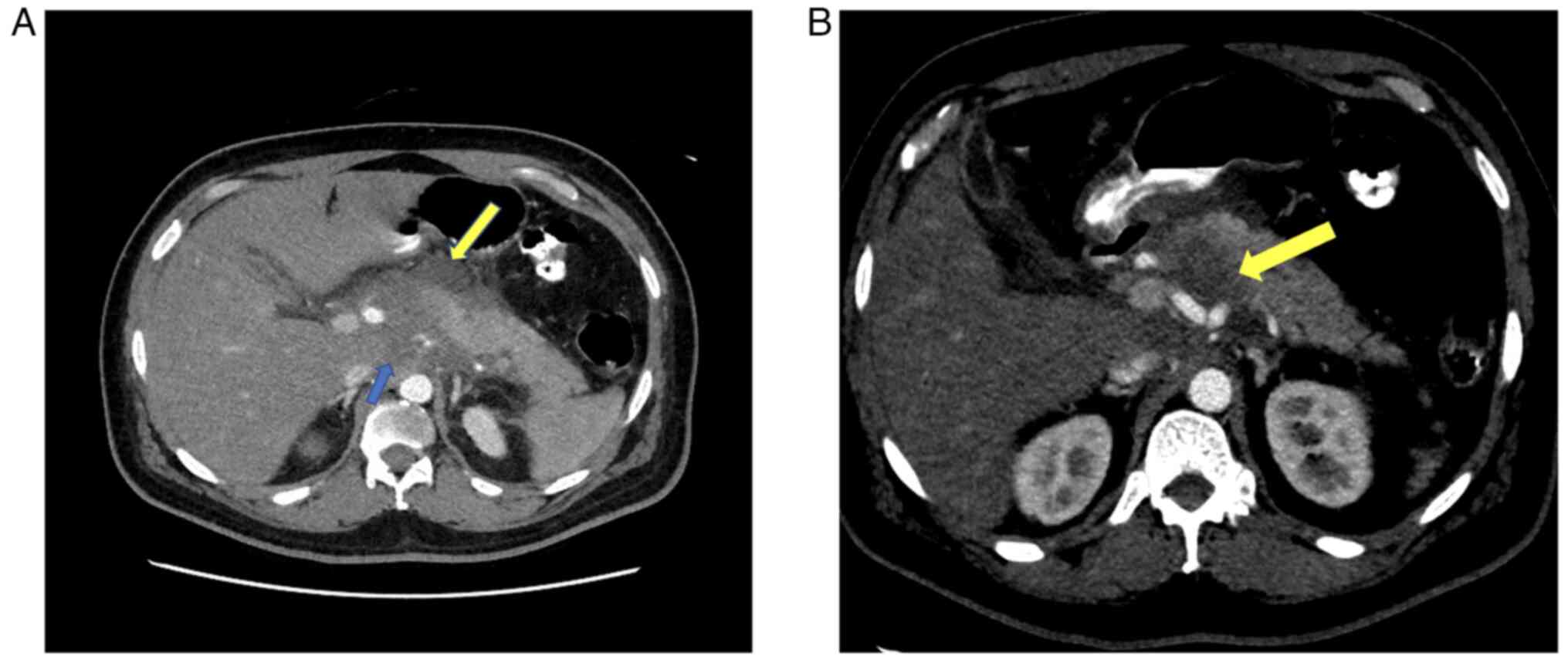
hepatitis panel, were within normal limits. Computed tomography
(CT) scan abdomen/pelvis with contrast showed AP with localized
peripancreatic fluid and ill-defined soft tissue mass within the
pancreatic head (Fig. 1) without
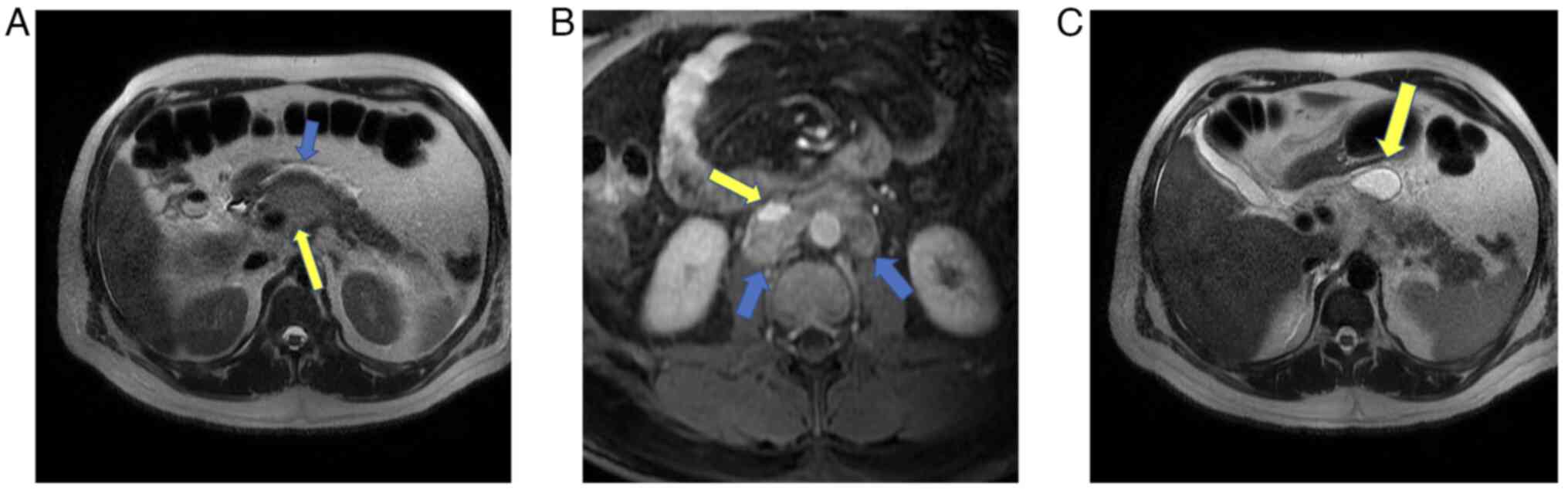
biliary or pancreatic duct dilatation. Magnetic Resonance
Cholangiopancreatography (MRCP) revealed a T2 hypointense
retroperitoneal soft tissue mass (4.4 cm) involving the pancreatic
head with superimposed pancreatitis and pseudocyst (Fig. 2A and C) and extensive paraaortic
lymphadenopathy (Fig. 2B)
consistent with pancreatic adenocarcinoma. However, tumor markers
carcinoembryonic antigen 19-9 and carcinoembryonic antigen levels
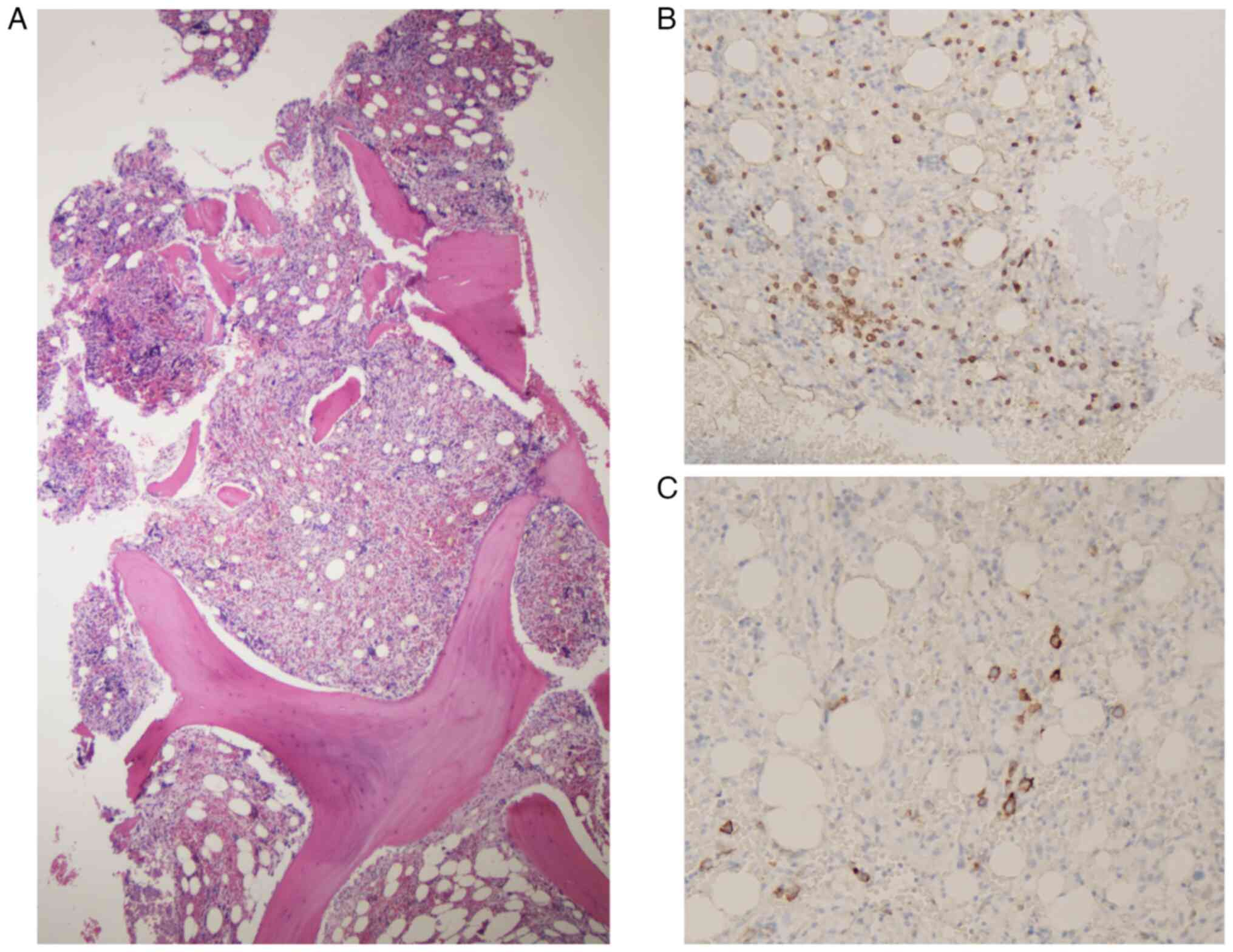
were normal. At this point, the cause of bicytopenia
(thrombocytopenia and neutropenia) was still unclear; hence bone
marrow (BM) biopsy was performed, which revealed hypercellular
marrow (60%) with scarce CD3-positive cells (Fig. 3B) and CD30-positive atypical
lymphoid infiltration (~5%) (Fig.
3C). At this point, there was a strong suspicion of lymphoma,
and considering abnormal liver enzymes and easy accessibility to
the liver, an ultrasound-guided liver core biopsy was performed.
However, before the biopsy, the patient received intravenous (IV)
steroids and platelets transfusion to stabilize the platelet
counts. A liver biopsy revealed the presence of mature T-cell
lymphoma, characterized by co-expression of the markers CD4, CD30,
and FOXP3 (Fig. 4). The CT scan for
the head, neck, and chest was negative. Our patient's
immunohistochemistry markers for mature T-cell lymphoma did not
meet the criteria for specific types of mature T-cell lymphoma
defined by the World Health Organization (WHO) (5). Therefore, the diagnosis of PTCL-NOS is
favored. The patient was subsequently initiated on an ACHP regimen
(brentuximab vedotin, cyclophosphamide, doxorubicin, and
prednisone), per the ECHELON 2 trial (6). The patient is currently getting his
chemotherapy sessions, with the tentative plan of hematopoietic
stem cell transplantation.
Discussion
PTCL is an aggressive entity comprising 5–15% of all
NHL (1). The median age at
diagnosis is 60 years, with a higher incidence in men (2:1 ratio).
Approximately 35% of patients diagnosed with PTCL exhibit B
symptoms (fevers, diaphoresis, and anorexia), 50% have elevated
LDH, and 14% demonstrate hypergammaglobulinemia (2). Our patient had no evidence of B
symptoms, but LDH levels were elevated. PTCL is prevalent in
immunosuppressed patients, such as patients with human
immunodeficiency virus/human T-cell leukemia virus (HIV/HTLV)
infections, lupus, or using immunosuppressive therapy (7). However, in this case, serologic tests
were negative for HIV, HBV, HCV, and HTLV, leading to speculation
that PTCL can occur in immunocompetent individuals.
AP is a well-documented complication of pancreatic
adenocarcinoma reported in 14% of cases; however, it is a rare
complication in pancreatic PTCL (8). The postulated pathogenesis underlying
AP is pancreatic duct obstruction, rupture of the pancreatic duct
with a direct parenchymal invasion, and ischemia secondary to
vascular occlusion by the tumor (9,10). In
our case, no pancreatic duct involvement was detected despite the
extensive infiltration of lymphoma cells in the pancreatic head.
Therefore, the probable pathogenesis of AP is attributable to
tumor-induced ischemia resulting from vascular occlusion.
Primary hepatic lymphoma generally presents as a
single, well-defined nodule, whereas secondary hepatic lymphoma can
present in various forms, ranging from one or multiple nodules to
diffuse infiltration (11). In our
case, neither CT nor MRCP scan could identify liver lesions
(possibly due to their small size) but revealed a hypointense
retroperitoneal mass within the pancreatic head, indicating primary
pancreatic involvement with secondary metastasis to the liver. At
the same time, previous reports have documented several cases of
primary hepatic PTCL (3,4). However, we present a unique case of
primary pancreatic PTCL with an unusual clinical manifestation as
AP, alongside liver and bone marrow involvement at the time of
diagnosis.
Imaging, particularly CT scans, is crucial for
diagnosing and characterizing pancreatic lymphoma. There are two
morphologic patterns for pancreatic lymphoma: well-circumscribed
tumors that may resemble pancreatic adenocarcinoma and diffuse
infiltrating types that can mimic acute pancreatitis on CT scans.
Key distinctions include the lack of pancreatic duct dilation in
lymphoma, lymph node involvement below the renal veins, and
invasive growth (12,13). Calcification or necrosis is not
typical in untreated cases. MRI findings parallel CT, with
well-circumscribed tumors showing low signal intensity on
T1-weighted images and subtle enhancement (13). Diffuse infiltrating masses display
low signal intensity on both T1 and T2-weighted images with
mild-to-moderate enhancement (13).
However, our patient CT scan showed ill-defined soft tissue mass
within the pancreatic head and MRCP revealed a T2 hypointense
retroperitoneal soft tissue mass (4.4 cm) involving the pancreatic
head which was initially concerning for pancreatic adenocarcinoma,
however our patient had no pancreatic duct involvement, and tumors
makers like Carcinoembryonic Antigen (CEA) and Cancer Antigen 19-9
(CA 19-9) were also negative in our patient, leading us to a
possibility of considering other diagnosis.
PTCL is often a perplexing diagnosis associated with
poor outcomes (14). Literature
reports a case series of 15 patients with nodal PTCL-NOS was found
to have an aggressive clinical course. Of these patients, 10 passed
away within 6 months of their diagnosis, with a median survival
time of only 3.5 months (15).
Moreover, Weisenburger et al (2) proposed that higher Kiel 67(Ki-67) was
associated with poor response to therapy and worse prognosis.
Several case reports have highlighted atypical presentation for
PTCL, such as Liu et al (16) report PTCL presenting as
rhabdomyolysis in a patient with alcohol abuse. Moreover, in
another case, PTCL presented as peripheral neuropathy compatible
with subacute demyelinating polyradiculoneuropathy (17). In essentially all of these cases,
the diagnosis was delayed or complex due to the atypical
presentation of a notoriously heterogeneous disease. In conclusion,
considering the rapidly progressive nature of PTCL, prompt invasive
biopsy should be performed. Early recognition of this uncommon
tumor is crucial for remission and early stem cell transplantation.
Furthermore, this case highlights the potential biases of
radiologists towards more common diagnoses, as in our case, it was
first diagnosed as pancreatic adenocarcinoma based on imaging
findings. It emphasizes the need for a critical and discerning
approach to an accurate diagnosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
FV and DK conceived and designed the study. FV, SV,
AM, SN and SP obtained data and treated this patient. FV and SV
analyzed the data and drafted the manuscript. FV and SH analyzed
the data using pathological methods. FV and DK confirm the
authenticity of the pathological data. FV and SH confirm the
authenticity of all other raw data. SV, AM, SN, SP and DK revised
the manuscript before submission. All authors read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed patient consent was obtained to
publish the article.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Swerdlow SH, Campo E, Pileri SA, Harris
NL, Stein H, Siebert R, Advani R, Ghielmini M, Salles GA, Zelenetz
AD and Jaffe ES: The 2016 revision of the World Health Organization
classification of lymphoid neoplasms. Blood. 127:2375–2390. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weisenburger DD, Savage KJ, Harris NL,
Gascoyne RD, Jaffe ES, MacLennan KA, Rüdiger T, Pileri S, Nakamura
S, Nathwani B, et al: Peripheral T-cell lymphoma, not otherwise
specified: A report of 340 cases from the international peripheral
T-cell lymphoma project. Blood. 117:3402–3408. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee J, Park KS, Kang MH, Kim Y, Son SM,
Choi H, Choi JW and Ryu DH: Primary hepatic peripheral T-cell
lymphoma mimicking hepatocellular carcinoma: A case report. Ann
Surg Treat Res. 93:110–114. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Petrova M, Gomes MM, Carda JPN and Pereira
de Moura J: Hepatosplenic T-cell lymphoma in a young
immunocompetent man. BMJ Case Rep. 2016:bcr20162144142016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jiang M, Bennani NN and Feldman AL:
Lymphoma classification update: T-cell lymphomas, Hodgkin
lymphomas, and histiocytic/dendritic cell neoplasms. Expert Rev
Hematol. 10:239–249. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Horwitz S, O'Connor OA, Pro B, Trümper L,
Iyer S, Advani R, Bartlett NL, Christensen JH, Morschhauser F,
Domingo-Domenech E, et al: The ECHELON-2 Trial: 5-Year results of a
randomized, phase III study of brentuximab vedotin with
chemotherapy for CD30-positive peripheral T-cell lymphoma. Ann
Oncol. 33:288–298. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Avlonitis VS and Linos D: Primary hepatic
lymphoma: A review. Eur J Surg. 165:725–729. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Thomas PC, Nash GF and Aldridge MC:
Pancreatic acinar cell carcinoma presenting as acute pancreatitis.
HPB (Oxford). 5:111–113. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Safadi R, Or R, Bar Ziv J and Polliack A:
Lymphoma-associated pancreatitis as a presenting manifestation of
immunoblastic lymphoma. Leuk Lymphoma. 12:317–319. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
To CA, Quigley MM, Saven A and Nicholson
L: Masquerade without a mass: An unusual cause of severe acute
pancreatitis. J Gastrointest Oncol. 4:114–117. 2013.PubMed/NCBI
|
|
11
|
Gazelle GS, Lee MJ, Hahn PF, Goldberg MA,
Rafaat N and Mueller PR: US, CT, and MRI of primary and secondary
liver lymphoma. J Comput Assist Tomogr. 18:412–415. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Saif MW: Primary pancreatic lymphomas.
JOP. 7:262–273. 2006.PubMed/NCBI
|
|
13
|
Merkle EM, Bender GN and Brambs HJ:
Imaging findings in pancreatic lymphoma: Differential aspects. AJR
Am J Roentgenol. 174:671–675. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Foss FM, Zinzani PL, Vose JM, Gascoyne RD,
Rosen ST and Tobinai K: Peripheral T-cell lymphoma. Blood.
117:6756–6767. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jeon YK, Kim JH, Sung JY, Han JH and Ko
YH; Hematopathology Study Group of the Korean Society of
Pathologists, : Epstein-Barr virus-positive nodal T/NK-cell
lymphoma: An analysis of 15 cases with distinct clinicopathological
features. Hum Pathol. 46:981–990. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Liu Z, Medeiros LJ and Young KH:
Peripheral T-cell lymphoma with unusual clinical presentation of
rhabdomyolysis. Hematol Oncol. 35:125–129. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kawanishi K, Ohyama Y, Kanai Y, Hirase T,
Tanaka H, Miyatake J, Tatsumi Y, Ashida T, Nakamine H and Matsumura
I: Sub-acute demyelinating polyradiculoneuropathy as an initial
symptom of peripheral T cell lymphoma, not otherwise specified
(PTCL-NOS). Intern Med. 51:2015–2020. 2012. View Article : Google Scholar : PubMed/NCBI
|