Introduction
In 2022, there were 10.6 million new cases of
tuberculosis (TB) worldwide, with 1.3 million deaths globally due
to TB, and the number of newly-diagnosed patients with TB in China
was 748,000 in 2022 (1). Acute
myeloid leukemia (AML) is a frequently fatal bone marrow stem cell
cancer characterized by unbridled proliferation of malignant marrow
stem cells with associated infection, anemia and bleeding (2). The basic treatment strategy for newly
diagnosed AML remains intensive therapy based on combination
chemotherapy, inducing a complete remission (CR) with initial
therapy, followed by consolidation therapy after remission
(3). For older adults with AML
considered appropriate for antileukemic therapy but not for
intensive antileukemic therapy, the ASH guideline panel suggests
using either of the options when choosing between
hypomethylating-agent monotherapy and low-dose-cytarabine
monotherapy (4). Chemotherapy
typically results in bone marrow suppression, prolonged neutropenia
and a decrease in immune function in patients (5). Additionally, due to the weakened
immune system in patients with AML, these patients are more
susceptible to acquiring new infections and the reactivation of
latent infections, including TB (6,7).
Treating AML complicated by active pulmonary TB poses significant
challenges for clinicians. Although TB is highly prevalent in
developing countries, its common symptoms such as fever and
lymphadenopathy may also occur in patients with AML, leading to
delayed diagnosis in these patients with atypical clinical
presentations (7). In terms of
treatment, patients with AML and active TB may face multiple issues
such as cumulative toxicity from various medications, drug
interactions and an inability to tolerate traditional intensive
chemotherapy regimens (8). Finding
the optimal timing for treatment of both AML and TB is complex. Our
previous study reports the case of a patient with AML and active
pulmonary TB who, in early 2022, was treated with a venetoclax,
homoharringtonine (HHT) and azacitidine regimen, and achieved CR
whilst achieving excellent control of the active pulmonary TB
(9). The present study reports the
diagnosis and treatment process of two patients with AML, which
demonstrated that following a combination of a venetoclax-based
anti-AML regimen combined with an intensive and then individualized
anti-TB regimen, CR was achieved as well as good control of active
TB. A balance was observed in the treatment of these patients,
effectively treating acute myeloid leukemia, while safely
controlling active pulmonary tuberculosis, thus making it a safer
treatment option.
Case report
Case 1
A 33-year-old female patient was diagnosed with
AML-M5b (8) in March 2022 at The
First Affiliated Hospital of Medical School of Zhejiang University
(Hangzhou, China). Next-generation sequencing (NGS) (10) indicated AML1-ETO-positive and
mutated fms-like tyrosine kinase 3 (FLT3)-internal tandem
duplication (ITD; 2.56%). The DNA was extracted using the QIAGEN
QIAseq FX DNA Library Kit (cat. no. 180479; Qiagen GmbH). The
samples were analyzed using the Agilent 2100 Bioanalyzer (Agilent
Technologies, Inc.) to assess the integrity of the DNA and to
determine the concentration of the sample. DNA quality scores were
used to ensure the sample quality. The sequencing kits used
included the NovaSeq 6000 S4 Reagent Kit v1.5 (300 cycles; cat. no.
20028312; Illumina, Inc.), NovaSeq 6000 S2 Reagent Kit v1.5 (300
cycles; cat. no. 20028314; Illumina, Inc.), NovaSeq 6000 S1 Reagent
Kit v1.5 (300 cycles; cat. no. 20028317; Illumina, Inc.) and
NovaSeq 6000 SP Reagent Kit v1.5 (300 cycles; cat. no. 20028400;
Illumina, Inc.). Paired-end sequencing with a nucleotide length of
150×2 bp was performed. Both strands were sequenced (forward and
reverse). The concentration was determined using the
NadPrep® Hybrid Capture Reagents kit
[1005101; Nanoda (Nanjing) Biotechnology Co., Ltd.]. The target
regions in the library were captured with a custom blood cancer
panel. High-fidelity DNA polymerase (KK2621; Kapa Biosystems; Roche
Diagnostics) was used to perform PCR amplification of the target
regions. The amplification conditions were as follows: 98°C for 45
sec, 98°C for 15 sec, 65°C for 30 sec and 72°C for 30 sec with 8
cycles. After the last reaction cycle, the PCR reaction was further
extended at 72°C for 1 min and then cooled to 10°C. The Applied
Biosystems 7500 Fast Real-Time PCR System (Thermo Fisher
Scientific, Inc.) was used for detection. The loading concentration
of the final library was ≥10 ng/µl. The software used for data
analysis included Burrows-Wheeler Aligner (0.7.10; http://sourceforge.net/projects/bio-bwa/files/),
Sequence Alignment/Map (1.9; Wellcome Sanger Institute) and Genome
Analysis Toolkit (3.5; Broad Institute). Lung computed tomography
(CT) revealed inflammation in the upper lobe of the left lung and
multiple nodules in both lungs, some of which were ground-glass
nodules (data not shown). The patient commenced chemotherapy with
oral venetoclax (100 mg on day 1, 200 mg on day 2 and 300 mg on
days 3–10), intravenous HHT (3 mg on days 1–5), intravenous
aclarubicin (17 mg on days 1–5) and subcutaneous cytarabine (70 mg
on days 1–5; VHAA) for 10 days, followed by an 18-day rest (1
cycle), along with oral isoniazid (300 mg) and rifampicin (450 mg)
for TB prophylaxis. After two cycles of the VHAA regimen, bone
marrow cytomorphology examination (Wright-Giemsa composite stain at
25°C for 15 min; light microscope) results indicated that the
proportions of mature and immature monocytes were 4 and 1%,
respectively (data not shown). Lung CT revealed scattered
ground-glass nodules in both lungs, with an increasing number of
new-onset nodules (data not shown). Furthermore, the T cells spot
test of TB infection (11) was
positive for TB infection and Mycobacterium tuberculosis was
detected in the sputum culture. The complete blood cell count
showed a white blood cell count of 32.3×109/l (normal
reference values, 3.5–9.5×109/l), hemoglobin levels of
65 g/l (normal reference values, 120–170 g/l) and a platelet count
of 102×109/l (normal reference values,
100–300×109/l). After being transferred to Hangzhou Red
Cross Hospital (Hangzhou, China) in April 2022, the patient
underwent a chest CT scan, which revealed scattered ground-glass
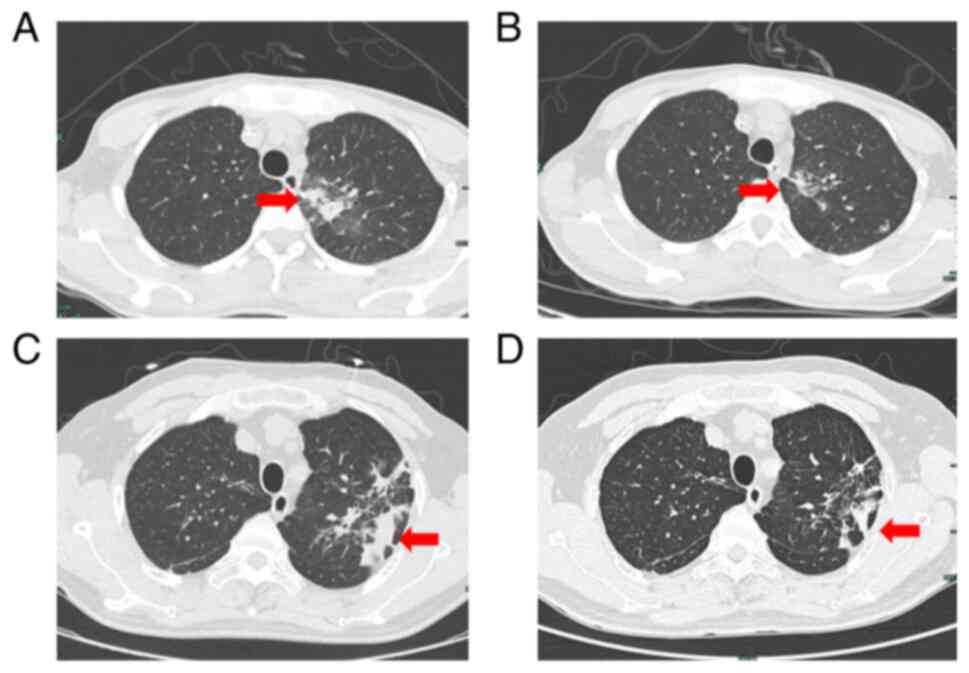
nodules in both lungs, with increasing new-onset nodules (Fig. 1A), and was treated with intensive
anti-TB therapy with oral isoniazid (300 mg), rifampicin (450 mg),
pyrazinamide (1.25 g) and ethambutol (750 mg) (HRZE). After 10
days, acid-fast bacillus (AFB) was not detected in the sputum. The
patient was then treated with oral venetoclax (100 mg on day 1, 200
mg on day 2 and 300 mg on days 3–10), intravenous HHT (3 mg on days
1–5) and subcutaneous cytarabine (70 mg q12 h, on days 1–5; V + HA)
for 10 days, followed by an 18-day rest (1 cycle). The anti-TB
regimen was changed to oral isoniazid (300 mg), pyrazinamide (1.25
g), ethambutol (750 mg) (HZE) with levofloxacin (500 mg). In May
2022, a lung CT suggested absorption of the lung lesions (Fig. 1B). The patient continued to receive
the V + HA for antileukemia regimen and eventually achieved CR. The
patient underwent hematopoietic stem cell transplant (HSCT) after
achieving CR and received oral levofloxacin (500 mg) for anti-TB
therapy for 1 year. The patient is followed up in the outpatient
clinic every 2 weeks for a routine blood test. Additionally, a
routine bone marrow cytomorphology examination is repeated once
every quarter. As of July 2024, the patient was in good condition
with no recurrence.
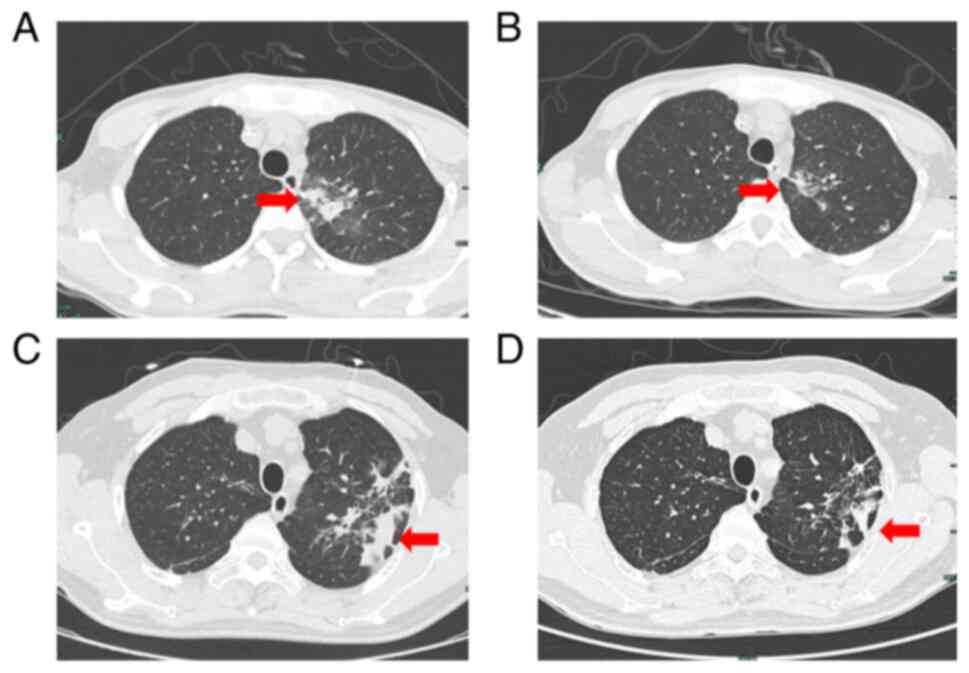 | Figure 1.Chest CT in case 1 and case 2. (A) As
indicated by the red arrow, in April 2022, lung CT revealed
scattered ground-glass nodules in both lungs, with increasing
new-onset nodules, in case 1. (B) As indicated by the red arrow, in
May 2022, lung CT demonstrated absorption of lung lesions in case
1. (C) As indicated by the red arrow, in April 2023, lung CT
indicated TB in the upper lobes of both lungs in case 2. (D) As
indicated by the red arrow, in August 2023, lung CT indicated TB in
the upper lobes of both lungs with a certain degree of absorption
compared with the condition at the time of admission in case 2. CT,
computed tomography; TB, tuberculosis. |
Case 2
In April 2023, a 57-year-old male patient was
diagnosed with active TB at a local hospital (Yiwu Central
Hospital, Yiwu, Jinhua, China), and Mycobacterium
tuberculosis was detected in the sputum culture. After
undergoing anti-TB therapy with oral ethambutol hydrochloride,
pyrazinamide, rifampicin and isoniazid tablet II (8 tablets per
day), the complete blood cell count revealed a white blood cell
count of 4.45×109/l (normal reference values,
3.5–9.5×109/l), hemoglobin levels of 108 g/l (normal
reference values, 120–170 g/l) and a platelet count of
76×109/l (normal reference values,
100–300×109/l). Manual classification (12) revealed that 13% of cells were
primitive. The patient was transferred to the Department of
Oncology and Hematology (Hangzhou Red Cross Hospital, Hangzhou,
China) in April 2023 for TB, and lung CT indicated TB in the upper
lobes of both lungs (Fig. 1C). The
patient was treated with regular intensive anti-TB therapy using
the oral isoniazid (300 mg), rifampicin (600 mg), pyrazinamide (1.0
g) and ethambutol (750 mg) (HRZE) regimen. Furthermore, the patient
was diagnosed with AML-M2a (8). NGS
(10) indicated double mutation of
CCAAT enhancer binding protein α and isocitrate dehydrogenase
(IDH)2. Regular anti-TB therapy with the HRZE regimen was
administered for 15 days, and no AFB was detected in any of the
three sputum smears. Subsequently, the anti-TB regimen was changed
to oral isoniazid (300 mg), pyrazinamide (1.0 g), ethambutol (750
mg) (HZE) and moxifloxacin (400 mg), along with antileukemia
therapy that included oral venetoclax (100 mg on day 1, 200 mg on
day 2 and 300 mg on days 3–21) and subcutaneous azacitidine (100 mg
on days 1–7; VA) for 21 days, followed by a 7-day rest (1 cycle).
The bone marrow test after one cycle of treatment suggested
primitive granulocytes of 1.0 and promyelocytes of 1.0. Flow
cytometry of bone marrow (13)
aspirates revealed no abnormal cells (Fig. S1). The marrow sample was mixed with
EDTA anticoagulant and the following antibodies were added for
incubation in a dark environment at room temperature for 15 min:
CD10-mFlour450 (cat. no. S010MF14; Caprico Biotechnologies),
CD117-allophycocyanin (APC)-A750 (cat. no. A80249; Beckman Coulter,
Inc.), CD11b-APC (cat. no. 652819; BD Biosciences), CD11c-PC7 (cat.
no. B36300; Beckman Coulter, Inc.), CD123-phycoerythrin (PE) (cat.
no. 649453; BD Biosciences), CD13-PC7 (cat. no. 338425; BD
Biosciences), CD13-PE (cat. no. 347406; BD Biosciences), CD14-PC5
(cat. no. A70204; Beckman Coulter, Inc.), CD15-FITC (cat. no.
340703; BD Biosciences), CD16-mFlour450 (cat. no. IM0814U; Beckman
Coulter, Inc.), CD19-PC7 (cat. no. 348804; BD Biosciences),
CD20-APC-A750 (cat. no. 641396; BD Biosciences), CD22-APC (cat. no.
340932; BD Biosciences), CD33-PC5.5 (cat. no. A70198; Beckman
Coulter, Inc.), CD34-APC (cat. no. IM2472U; Beckman Coulter, Inc.),
CD36-FITC (cat. no. B49201; Beckman Coulter, Inc.), CD38-PC5 (cat.
no. A70205; Beckman Coulter, Inc.), CD3-APC (cat. no. Z6410048;
Beijing Quantobio Biotechnology Co., Ltd.), CD45-mFluor540 (cat.
no. 340942; BD Biosciences), CD4-APC-A750 (cat. no. 340672; BD
Biosciences), CD56-PC5.5 (cat. no B49189; Beckman Coulter, Inc.),
CD5-PC7 (cat. no. 348790; BD Biosciences), CD64-APC-A750 (cat. no.
B96769; Beckman Coulter, Inc.), CD7-PE (cat. no. 340656; BD
Biosciences), CD8-FITC (cat. no. S008FI04; Caprico
Biotechnologies), HLA-DR-mFlour450 (cat. no. Z6410082; Beijing
Quantobio Biotechnology Co., Ltd.), kappa-FITC (cat. no. 643774; BD
Biosciences) and lambda-PE (cat. no. 642924; BD Biosciences). Lysis
buffer (2,000 µl) was added to each tube, followed by incubation at
room temperature for 10–15 min and centrifugation at 160 × g for 5
min at room temperature. The supernatant was discarded and PBS
(1,000 µl) was added, followed by centrifugation at 160 × g for 5
min at room temperature. The washing procedure was repeated once
more. After discarding the supernatant again, the cells were
resuspended with an appropriate volume of PBS (500–2,000 µl) based
on the cell concentration. Specimens were examined using flow
cytometry (BD Facs Canto II; BD Biosciences) after mixing. The
detected data were analyzed using Kaluza software (version no.
A82959; Beckman Coulter, Inc.). A CR without significant infection
due to agranulosis was achieved after clinical evaluation. The
patient was on the fourth cycle of the VA regimen whilst continuing
the anti-TB therapy, and the blood concentration of venetoclax
fluctuated between 1,270 and 4,580 ng/ml. The results of the bone
marrow test and flow cytometry (13) were normal (Fig. S2), and no significant agranulosis
was observed. Lung CT indicated TB in the upper lobes of both
lungs, with a certain degree of absorption compared with the
condition at the time of admission (Fig. 1D). The patient continued the anti-TB
therapy with HZE and moxifloxacin for 1 year and the patient is
being treated with the VA regimen. The patient continues to be
hospitalized every 28 days for examination and treatment until such
time as the disease recurs or the current treatment regimen becomes
intolerable. As of July 2024, the patient was in good
condition.
Discussion
Due to the uniqueness of Mycobacterium
tuberculosis, balancing the timing of treatment for AML and
active TB is a great challenge for clinicians. A previous study
reported 15 patients with active TB at the time of initial AML
diagnosis in whom the first induction chemotherapy lasted for 2
months (14). TB was controlled and
leukemia went into remission in 13 patients, but the other 2
patients did not achieve remission and subsequently died. However,
the aforementioned study included few cases and, to the best of our
knowledge, there are no large-scale studies or guidelines for
clinical work guidance. When diagnosing pulmonary TB, clinicians
should carefully collect medical history, understand whether there
is a history of contact with pulmonary TB, and perform detailed
physical examinations, chest imaging, tuberculin skin tests and
laboratory tests (15). It is not
appropriate to consider only TB recurrence when the patient has
been diagnosed with pulmonary TB in the past and when the number of
lung lesions increases, as patients with AML can have one or many
concomitant pulmonary concomitant diseases (16–19).
However, when diagnosing pulmonary TB, it is necessary to
differentiate it from other lung diseases, such as lung cancer,
chronic pulmonary aspergillosis (CPA) and pulmonary leukemic
infiltration (PLI). Clinical symptoms serve a crucial role in the
differential diagnosis between TB and lung cancer. For instance,
cough, phlegm, fever, hemoptysis, weight loss and dyspnea are
common symptoms of both diseases; however, sudden weight loss,
hemoptysis and a history of smoking are more common in lung cancer.
Nevertheless, the diagnosis of TB and lung cancer still requires
comprehensive analysis through pathological and microbiological
tests (16). Additionally,
pulmonary CT has good application value in distinguishing between
TB and lung cancer alone (17). The
clinical manifestations of CPA, such as weight loss, fatigue,
fever, chronic coughing, chest discomfort and occasional
hemoptysis, are similar to those of most patients with TB. The
diagnosis of TB and CPA infection still requires a comprehensive
analysis combining etiological examination and radiographic
examination (18). PLI is most
commonly manifested as nodules or masses, but interstitial
abnormalities, such as thickening of bronchovascular bundles, are
also seen. Clinical confirmation requires radiographic examination
and lesion biopsy (19,20). However, a previous study (19) suggests that PLI often occurs in the
terminal stage. In the 2 cases in the present study, the platelet
counts of the patients were low, making percutaneous biopsy
impractical. However, after anti-TB treatment, the pulmonary
lesions in the 2 patients were notably reduced in size. Moreover,
sputum cultures for AFB were positive with conversion to negative.
Therefore, we hypothesize that the pulmonary infection in the
patients was active TB.
A total of four drugs are usually used
simultaneously during the intensive phase of anti-TB therapy. This
is due to the stronger synergistic bactericidal effect that is
capable of killing a larger number of reproducing Mycobacterium
tuberculosis in <2 weeks, thereby triggering a significant
decline in its virulence (21). In
the 2 cases in the present study, venetoclax-based antileukemia
regimens combined with individualized anti-TB regimens were
commenced after 10–15 days of intensive anti-TB therapy with the
HRZE regimen and three negative sputum cultures. Eventually, the
AML went into remission, and the active TB was well-controlled
without any significant adverse effects. Therefore, the
venetoclax-based antileukemia regimens combined with individualized
anti-TB therapy that were administered to the 2 patients after a
short period of intensive anti-TB therapy, were practically
feasible.
Patients with concurrent AML and active pulmonary TB
cannot tolerate traditional intensive therapy (8). Therefore, physicians must consider
choosing the best combination therapy. AML cells are dependent on
Bcl-2 for survival, and the inhibitory effect of venetoclax can
induce the endogenous apoptotic pathway, leading to rapid apoptosis
of AML cells and eradication of leukemic stem cells in the
stationary phase (22,23). Azacitidine increases the sensitivity
of AML cells to T cells, making them more susceptible to T
cell-mediated cytotoxicity (24).
The VA regimen achieves improved therapeutic effects and is the
standard treatment for newly diagnosed patients with AML who are
unsuited for intensified chemotherapy (8). Additionally, the VA regimen can
overcome certain high-risk genes such as FLT3-ITD and IDH1/2, but
has poor efficacy for certain genes such as FLT3-tyrosine kinase
domain (TKD) (25,26). The patient in case 2, who did not
have a FLT3 mutation, received the VA regimen and achieved CR with
just one course. Our previous report described a case in which the
patient was diagnosed with AML-M5b, accompanied by mutations in DNA
methyltransferase 3α, FLT3-TKD and IDH2, as well as active
pulmonary tuberculosis (9). The
response to the VA regimen of the patient was evaluated as no
response. A study has shown that HHT can inhibit the anti-apoptotic
proteins myeloid cell leukemia 1 and Bcl-xL and synergistically
exerts anti-AML effects with venetoclax (27). Li et al (28) elucidated the high sensitivity of
FLT3-mutated AML to HHT treatment. The patient in our previous
report was then administered HHT in addition to the VA regimen,
forming the VA+H regimen, which resulted in a CR, followed by a
HSCT (9). Zhou et al
(29) reported that the overall
response rate (CR + partial response) of the venetoclax combined
with HHT, cytarabine and aclacinomycin (VHAA) regimen was 97.5% and
the CR rate was 95.0% (29);
however, the VHAA regimen is associated with severe bone marrow
suppression, and the common adverse reactions are infections and
fever (29). A recent study by Liu
et al (30) reported that
the CR rate of venetoclax combined with HHT and cytarabine (V + HA)
was as high as 97.9% in elderly or intensive chemotherapy
ineligible patients with newly diagnosed AML. The patient in case 1
received the VHAA regimen followed by the V + HA regimen, achieved
CR, and underwent HSCT. Therefore, after achieving CR with a
venetoclax-based anti-AML regimen, high-risk patients are
recommended to undergo HSCT as soon as possible. Low-risk patients
can be treated with venetoclax-based regimen. After stable TB
control is achieved at 6 months, patients can be treated with a
standard anti-AML regimen; however, further studies are required to
confirm this finding.
The individual differences in blood venetoclax
concentration are large, and blood venetoclax concentration is
associated with the objective response rate and safety events
(31). Therefore, venetoclax-based
antileukemia regimens were selected in the present cases to detect
the changes in blood concentrations over time. Previous studies
have also demonstrated that small-dose, short-course
venetoclax-based combination regimens achieve better remission with
few adverse effects and are well tolerated by patients (32–34).
In the present study, both patients were treated with a small dose
of short-course venetoclax, and achieved CR. Intensive anti-TB
therapy, HRZE, was chosen to be used to promptly kill a large
number of reproducing and active susceptible bacteria in a short
period. Rifampicin was then replaced with a quinolone, which is
also capable of killing both intracellular and extracellular
bacteria (35), to compose an
individualized anti-TB regimen of HZE and quinolone to prevent
rifampicin, a strong inducer of cytochrome P450 3A4 enzymes, from
affecting the concentration of venetoclax. Both patients with AML
achieved good control of active TB and CR for AML.
In addition, another study demonstrated that
Mycobacterium tuberculosis increases the expression of Bcl-2
at the transcriptional level (36).
Based on the aforementioned study, we hypothesized that venetoclax,
as a Bcl-2 inhibitor, may reduce the expression of Mycobacterium
tuberculosis-induced Bcl-2, which may affect TB stability in
patients with active pulmonary TB. This provides a direction for
future research and clinical trials and is expected to bring new
breakthroughs in the treatment of concurrent active pulmonary TB
and AML.
How to treat AML combined with active TB is
currently a clinical issue that doctors and patients face together
and urgently need to solve, and the treatment plan for patients
with TB and AML is constantly being explored. A total of 4 other
patients with the same diagnoses after November 2023 were treated
and achieved good treatment results (Ji et al, unpublished
data). Future studies should build on these efforts and carry out
scientific research based on clinical problems, so as to provide
more patients with effective treatment and explore the possibility
of a breakthrough in the combined fields of TB and AML.
In summary, AML combined with active TB has unique
characteristics, and its clinical diagnosis and treatment are
challenging. For patients with AML combined with active TB, a
venetoclax-based anti-AML regimen combined with an intensive and
then individualized anti-TB regimen is efficacious with few side
effects. More cases should be collected to further clarify its
efficacy and safety and promote its application, thereby improving
the overall survival of patients with concurrent AML and active
pulmonary TB.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by the Research Fund of Hangzhou
Municipal Health and Health Commission (grant no. A20210210).
Availability of data and materials
The next-generation sequencing data generated in the
present study may be found in the Sequencing Read Archive under
accession number PRJNA1118206 or at the following URL: https://www.ncbi.nlm.nih.gov/bioproject/PRJNA1118206.
All other data generated in the present study may be requested from
the corresponding author.
Authors' contributions
XFX designed the chemotherapy plans. YQX was
responsible for tuberculosis management and nursing. WY, LJG and
BYZ were responsible for the clinical diagnosis and treatment of
the patients. LJ mainly collected the data for the manuscript,
drafted the manuscript, and revised key intellectual content. XFX
and LJ are responsible for the manuscript, ensuring that issues
related to the integrity of any part of the work were appropriately
investigated and resolved, and confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The publication of the present case reports was
approved by the Ethics Committee of Hangzhou Red Cross Hospital
[Hangzhou, China; approval no. 118(2023)].
Patient consent for publication
Written informed consent for publication of the
article, including clinical data and images, was obtained from the
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization (WHO), . Global
Tuberculosis report. WHO; Geneva: 2023, http://www.who.int/tb/publications/global_report/en/November
7–2023
|
|
2
|
Shimony S, Stahl M and Stone RM: Acute
myeloid leukemia: 2023 update on diagnosis, risk-stratification,
and management. Am J Hematol. 98:502–526. 2023. View Article : Google Scholar
|
|
3
|
Döhner H, Wei AH, Appelbaum FR, Craddock
C, DiNardo CD, Dombret H, Ebert BL, Fenaux P, Godley LA, Hasserjian
RP, et al: Diagnosis and management of AML in adults: 2022
recommendations from an international expert panel on behalf of the
ELN. Blood. 140:1345–1377. 2022. View Article : Google Scholar
|
|
4
|
Sekeres MA, Guyatt G, Abel G, Alibhai S,
Altman JK, Buckstein R, Choe H, Desai P, Erba H, Hourigan CS, et
al: American Society of Hematology 2020 guidelines for treating
newly diagnosed acute myeloid leukemia in older adults. Blood Adv.
4:3528–3549. 2020. View Article : Google Scholar
|
|
5
|
Kantarjian H: Acute myeloid leukemia-major
progress over four decades and glimpses into the future. Am J
Hematol. 91:131–145. 2016. View Article : Google Scholar
|
|
6
|
Malone JL, Ijaz K, Lambert L, Rosencrans
L, Phillips L, Tomlinson V, Arbise M, Moolenaar RL, Dworkin MS and
Simoes EJ: Investigation of healthcare-associated transmission of
Mycobacterium tuberculosis among patients with malignancies at
three hospitals and at a residential facility. Cancer.
101:2713–2721. 2004. View Article : Google Scholar
|
|
7
|
Jain A, Prakash G, Singh C, Lad D, Khadwal
A, Suri V, Malhotra P, Kumari S, Varma N and Varma S: Analysis of
clinical profile and outcome of tuberculosis in patients with acute
leukemia. Indian J Hematol Blood Transfus. 34:430–442. 2018.
View Article : Google Scholar
|
|
8
|
Leukemia & Lymphoma Group, Chinese
Society of Hematology and Chinese Medical Association, . Chinese
guidelines for diagnosis and treatment of adult acute myeloid
leukemia (not APL) (2023). Zhonghua Xue Ye Xue Za Zhi. 44:705–712.
2023.(In Chinese).
|
|
9
|
Ji L, Yang W, Xu XF and Xu YQ: A case
report of complete remission of acute myeloid leukemia combined
with DNMT3A, FLT3-TKD, and IDH2 gene mutations and active pulmonary
tuberculosis treated with homeharringtonine + venetoclax +
azacytidine. Front Med (Lausanne). 10:11807572023. View Article : Google Scholar
|
|
10
|
Hematology Oncology Committee of China
Anti-Cancer Association; Chinese Society of Hematology Chinese
Medical Association; Chinese Society of Pathology Chinese Medical
Association, . Expert consensus on the application of
next-generation sequencing in hematological neoplasms (2018).
Zhonghua Xue Ye Xue Za Zhi. 39:881–886. 2018.(In Chinese).
|
|
11
|
Sun Y, Yao X, Ni Y, Peng Y and Shi G:
Diagnostic Efficacy of T-SPOT.TB for active tuberculosis in adult:
A retrospective study. Infect Drug Resist. 15:7077–7093. 2022.
View Article : Google Scholar
|
|
12
|
Experimental Diagnosis Group and
Hematology Society Chinese Medical Association, . Consensus of
Chinese experts on morphologic analysis of blood cells. Zhonghua
Xue Ye Xue Za Zhi. 34:558–560. 2013.(In Chinese).
|
|
13
|
Chinese Society of Immunology and Clinical
Flow Cytometry Group, . Expert consensus on minimal residual
disease detection of acute leukemia and plasma cell neoplasms by
multi-parameter flow cytometry. Zhonghua Xue Ye Xue Za Zhi.
38:1001–1011. 2017.(In Chinese).
|
|
14
|
Li J and Niu T: Clinical research progress
of hematological malignancies complicated with active tuberculosis.
Zhonghua Xue Ye Xue Za Zhi. 34:1076–1079. 2013.(In Chinese).
|
|
15
|
World Health Organization (WHO), . WHO
operational handbook on tuberculosis Module 2. Screening Systematic
screening for tuberculosis disease. WHO; Geneva: 2021
|
|
16
|
Sheikhpour M, Mirbahari SN, Sadr M, Maleki
M, Arabi M and Abolfathi H: A comprehensive study on the
correlation of treatment, diagnosis and epidemiology of
tuberculosis and lung cancer. Tanaffos. 22:7–18. 2023.
|
|
17
|
Sun W, Zhang L, Liang J, Li X, Yang Y, Sun
W and Hou J: Comparison of clinical and imaging features between
pulmonary tuberculosis complicated with lung cancer and simple
pulmonary tuberculosis: A systematic review and meta-analysis.
Epidemiol Infect. 150:e432022. View Article : Google Scholar
|
|
18
|
Mei ZX, Han JF, Yu HW, Zhang Y, Ji P, Xie
Y and Hsueh PR: Detection of serum Aspergillus-specific IgM and IgG
antibody levels for the diagnosis of chronic pulmonary
aspergillosis developed in patients with tuberculosis. Eur J Clin
Microbiol Infect Dis. 42:1081–1089. 2023. View Article : Google Scholar
|
|
19
|
Gosangi B, Hatabu H and Hammer MM: Imaging
features of pulmonary leukemic infiltration with comparison of
lymphoid and myeloid leukemias. Curr Probl Diagn Radiol.
50:164–167. 2021. View Article : Google Scholar
|
|
20
|
Yoshifuji K, Toya T, Yanagawa N, Sakai F,
Nagata A, Sekiya N, Ohashi K and Doki N: CT classification of acute
myeloid leukemia with pulmonary infiltration. Jpn J Radiol.
39:1049–1058. 2021. View Article : Google Scholar
|
|
21
|
Dickinson JM, Aber VR and Mitchison DA:
Bactericidal activity of streptomycin, isoniazid, rifampin,
ethambutol, and pyrazinamide alone and in combination against
Mycobacterium tuberculosis. Am Rev Respir Dis. 116:627–635. 1977.
View Article : Google Scholar
|
|
22
|
Zhang Y and Jin J: Application of Bcl-2
inhibitor venetoclax in acute myeloid leukemia. Zhonghua Xue Ye Xue
Za Zhi. 42:438–440. 2021.(In Chinese).
|
|
23
|
DiNardo CD, Jonas BA, Pullarkat V, Thirman
MJ, Garcia JS, Wei AH, Konopleva M, Döhner H, Letai A, Fenaux P, et
al: Azacitidine and Venetoclax in Previously Untreated Acute
Myeloid Leukemia. N Engl J Med. 383:617–629. 2020. View Article : Google Scholar
|
|
24
|
Lee JB, Khan DH, Hurren R, Xu M, Na Y,
Kang H, Mirali S, Wang X, Gronda M, Jitkova Y, et al: Venetoclax
enhances T cell-mediated antileukemic activity by increasing ROS
production. Blood. 138:234–245. 2021. View Article : Google Scholar
|
|
25
|
Bouligny IM, Murray G, Doyel M, Patel T,
Boron J, Tran V, Gor J, Hang Y, Alnimer Y, Zacholski K, et al:
Venetoclax with decitabine or azacitidine in the first-line
treatment of acute myeloid leukemia. EJHaem. 4:381–392. 2023.
View Article : Google Scholar
|
|
26
|
De Leeuw DC, Ossenkoppele GJ and Janssen
JJWM: Older patients with acute myeloid leukemia deserve
individualized treatment. Curr Oncol Rep. 24:1387–1400. 2022.
View Article : Google Scholar
|
|
27
|
Yuan F, Li D, Li G, Cheng C and Wei X:
Synergistic efficacy of homoharringtonine and venetoclax on acute
myeloid leukemia cells and the underlying mechanisms. Ann Transl
Med. 10:4902022. View Article : Google Scholar
|
|
28
|
Li C, Dong L, Su R, Bi Y, Qing Y, Deng X,
Zhou Y, Hu C, Yu M, Huang H, et al: Homoharringtonine exhibits
potent anti-tumor effect and modulates DNA epigenome in acute
myeloid leukemia by targeting SP1/TET1/5hmC. Haematologica.
105:148–160. 2020. View Article : Google Scholar
|
|
29
|
Zhou Z, Zhao X, Suo X, Bai G, Shi Z, Luo
Y, Tan Y, Lu X, Yuan L, Zhang C, et al: Venetoclax combined with
homoharringtonine, cytarabine, and aclacinomycin (HAAV) as
induction therapy in newly diagnosed young adult acute myeloid
leukemia. Blood. 142 (Supplement 1):S15172023. View Article : Google Scholar
|
|
30
|
Liu K, Suo X, Bai G, Yan Z, Li Y, Zhang B,
He J, Li J, Wei S, Li Q, et al: Venetoclax combined with
homoharringtonine and cytarabine (HAV) as induction treatment in
elder or intensive chemotherapy (IC) ineligible patients with newly
diagnosed acute myeloid leukemia. Blood. 142 (Supplement
1):S42722023. View Article : Google Scholar
|
|
31
|
Li K, Zhao W, Liu Y, Gao X, Zhou F, Chen
Q, Chang Y and Wang W: The value of venetoclax blood concentration
monitoring in the treatment of acute myeloid leukemia and the
efficacy and safety of combined azacytidine in the treatment of
acute myeloid leukemia. J Clin Hematol. 35:812–816. 2022.(In
Chinese).
|
|
32
|
Jin H, Zhang Y, Yu S, Du X, Xu N, Shao R,
Lin D, Chen Y, Xiao J, Sun Z, et al: Venetoclax combined with
azacitidine and homoharringtonine in relapsed/refractory AML: A
multicenter, Phase 2 trial. J Hematol Oncol. 16:422023. View Article : Google Scholar
|
|
33
|
Mirgh S, Sharma A, Shaikh MRMA, Kadian K,
Agrawal N, Khushoo V, Mehta P, Ahmed R and Bhurani D:
Hypomethylating agents+venetoclax induction therapy in acute
myeloid leukemia unfit for intensive chemotherapy-novel avenues for
lesser venetoclax duration and patients with baseline infections
from a developing country. Am J Blood Res. 11:290–302. 2021.
|
|
34
|
Vachhani P, Flahavan EM, Xu T, Ma E,
Montez M, Gershon A, Onishi M, Jin H, Ku G, Flores B, et al:
Venetoclax and hypomethylating agents as first-line treatment in
newly diagnosed patients with AML in a predominately community
setting in the US. Oncologist. 27:907–918. 2022. View Article : Google Scholar
|
|
35
|
Millanao AR, Mora AY, Villagra NA, Bucarey
SA and Hidalgo AA: Biological Effects of Quinolones: A family of
broad-spectrum antimicrobial agents. Molecules. 26:71532021.
View Article : Google Scholar
|
|
36
|
Ramon-Luing LA, Olvera Y, Flores-Gonzalez
J, Palacios Y, Carranza C, Aguilar-Duran Y, Vargas MA, Gutierrez N,
Medina-Quero K and Chavez-Galan L: Diverse cell death mechanisms
are simultaneously activated in macrophages infected by virulent
mycobacterium tuberculosis. Pathogens. 11:4922022. View Article : Google Scholar
|