Introduction
Thyroid cancer (TC) accounts for 1% of all
epithelial malignancies and is the most frequent endocrine neoplasm
(1). Due to the accuracy and
convenience of diagnostic technology such as ultrasound and
fine-needle aspiration, the TC incidence rate has been increasing
worldwide in recent decades (2). TC
includes a number of histological types, with the most frequent
type being papillary thyroid carcinoma (PTC) (3), which accounts for ~88% of cases
(4).
PTC characterized by a high rate of lymph node (LN)
invasion on initial diagnosis gradually leads to remote metastasis
(5). However, the prognosis of PTC
is more favourable compared with other types of TC, following
administration of appropriate treatments, such as surgery, adjuvant
radioactive iodine and thyroid-stimulating hormone (TSH)
suppression therapy. The 10-year survival rate of PTC is 93% in the
United States and the mortality rate is ~10% (4,6). The
major factors influencing the prognosis of PTC are patient age,
sex, tumor size, histological findings, extrathyroidal extension,
clinical lymph node metastasis and remote metastasis (7). Gene mutations such as
BRAFV600E and TERT have become a popular topic in recent
decades (8,9).
The common sites of distant PTC metastasis are the
lymph nodes, lungs and bones. The incidence of skin metastasis in
PTC is <1% (10). The first
study of skin metastasis in PTC in 1964 reported a poor prognosis,
with a mean survival time of 19 months (11,12),
and the 5-year survival rate was 28–53.3% (13). Skin metastases of PTC may present as
erythematous papules and plaques or as flesh-coloured and tender
nodules, with or without pruritus and ulceration (14,15).
The present study reports the case of a 26-year-old female patient
with skin metastasis from PTC, who had undergone thyroid cancer
surgery 2.5 years previously.
Case report
Patient
In March 2021, a 23-year-old woman underwent a
routine physical examination followed by a thyroid ultrasound at
Yantaishan Hospital (Yantai, China), which revealed an
~3.1×1.9×1.6-cm hypoechoic nodule with microcalcifications in the
right thyroid lobe and no enlarged neck lymph nodes. No family
history of thyroid disease or exposure to external radiation were
reported. The patient then underwent a right thyroidectomy and
isthmus resection with central cervical lymph node dissection, and
the tissue pathology results demonstrated PTC with capsular
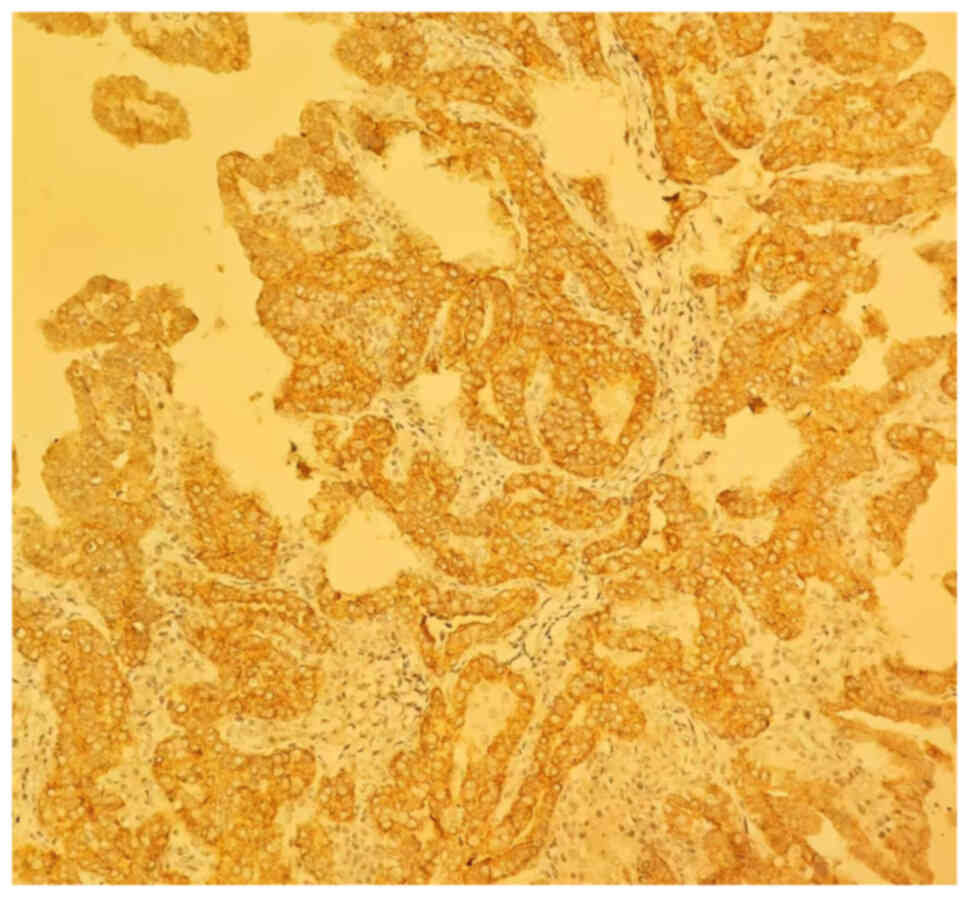
invasion. The mmunohistochemical analysis of the biopsy specimen
indicated a positive BRAFV600E mutation genotype,
as areas of BRAFV600E-positive tumour cytoplasmic
staining were observed (Fig.
1).
Of the 12 lymph nodes, one had metastatic PTC, and
after surgery, oral levothyroxine therapy (75 µg daily) was
administered. Starting in March 2021, during follow-ups performed
every every 3 months, the patient's thyroxine and triiodothyronine
levels were normal (ranges, 12.00–22.00 and 3.10–6.80 pmol/l,
respectively), and the thyroid-stimulating hormone (TSH) level was
0.83 µIU/ml (range, 0.27–4.20 µIU/ml); however, the serum
thyroglobulin (Tg) level remained below the threshold at 1.20 ng/ml
(range, 1.40–78.00 ng/ml), and there was no other documented
evidence of local recurrence or distant metastasis.
In September 2023, the patient observed two palpable
small nodules on the left anterior neck ~4 cm above the first
surgical scar, ~2.5 years after the first operation in 2021; the
nodules were firm, tough and painless (Fig. 2). For further evaluation,
ultrasound-guided punch biopsies of the lesions were performed at
Yantai Yuhuangding Hospital (Yantai, China), which led to the
diagnosis of skin metastasis of PTC through pathological
assessment. Consequently, the patient presented to Yantaishan
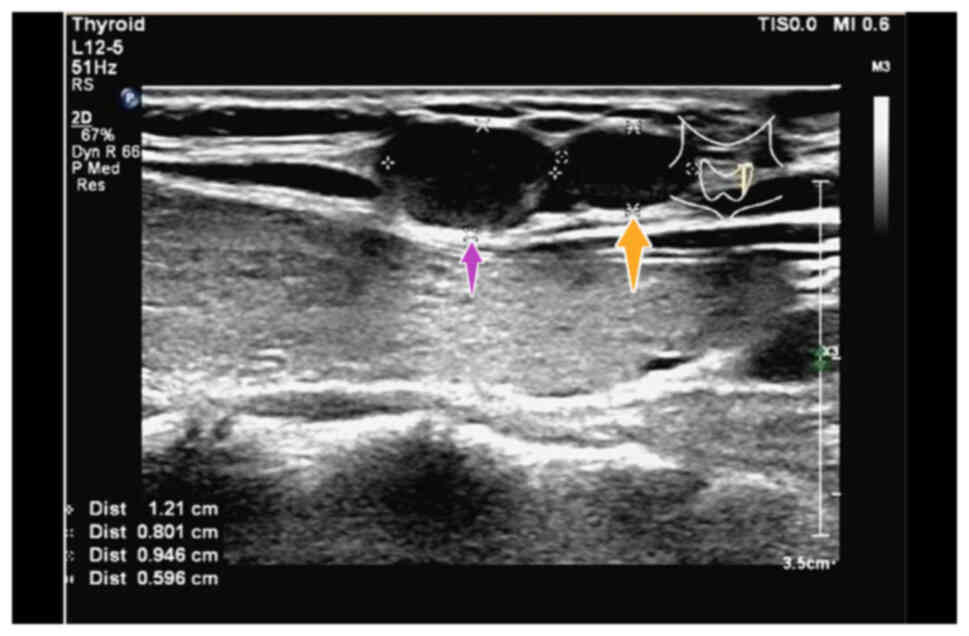
Hospital for surgical resection in October 2023. Neck ultrasound
scans demonstrated two hypoechoic subcutaneous nodules with clear
boundaries, which measured ~1.2×0.8 and 0.9×0.6 cm in size
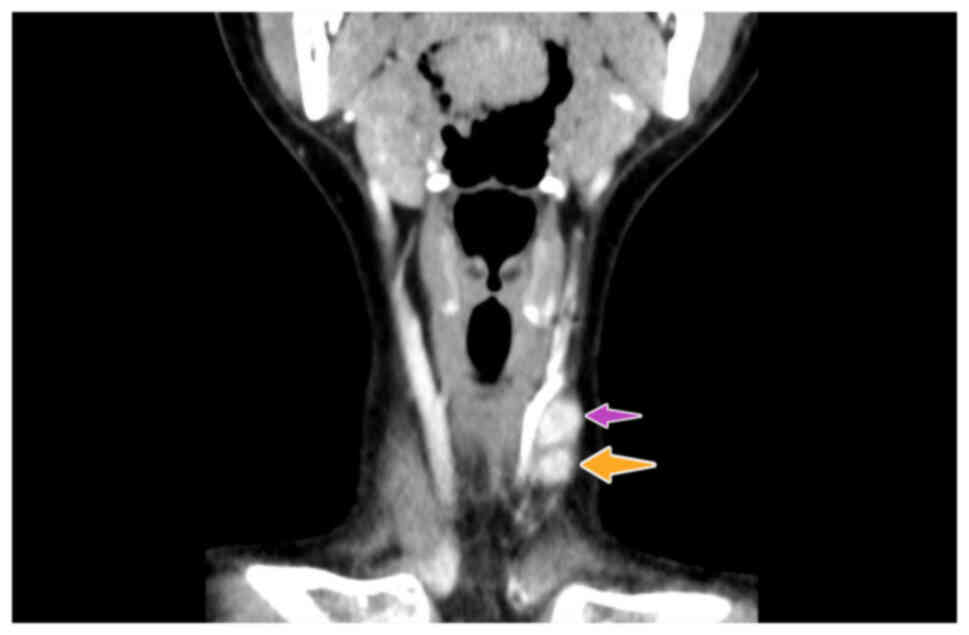
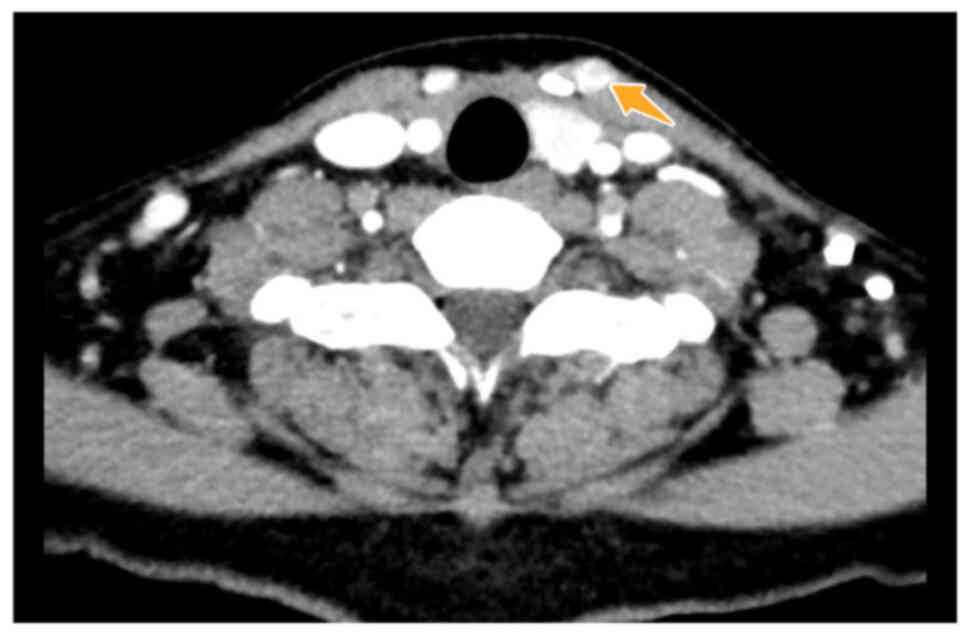
(Fig. 3). Contrast-enhanced
computed tomography (CT) scans of the patients neck demonstrated
two adjacent enhanced nodules (Fig.
4, Fig. 5, Fig. 6) on the left side of the neck. No
evidence of local recurrence in the operative bed of the previously
resected lesion was observed. Chest CT scans did not indicate
recurrence or metastasis. The patient's TSH level was 0.79 µIU/ml
with oral levothyroxine therapy (75 µg daily) and the Tg level was
16.40 µg/l. For the diagnosis and treatment of the nodules, the
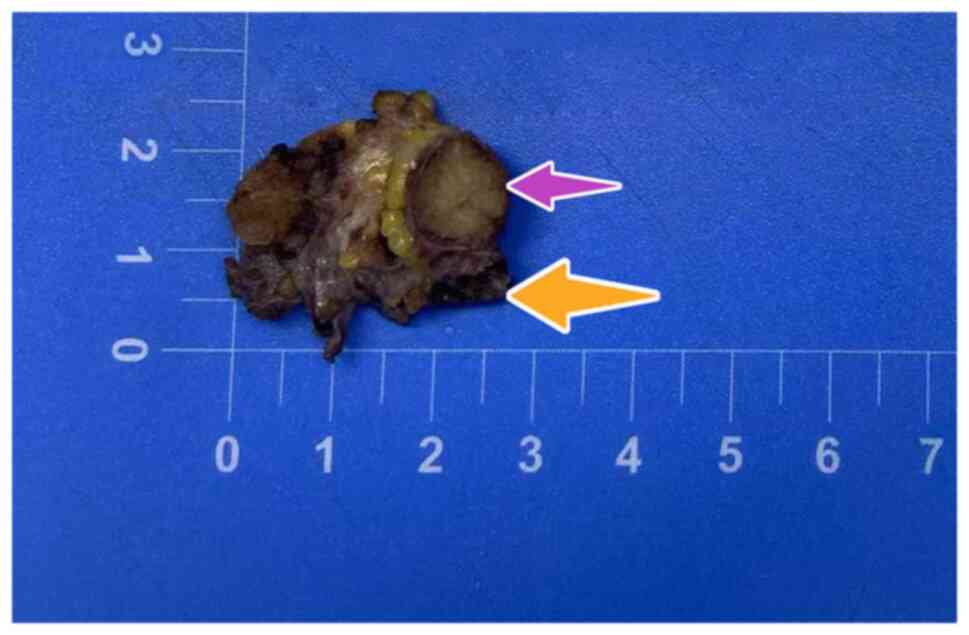
patient's first surgical scar was reopened, and the two nodules
underlying the subcutaneous fat were removed. Surgical pathology
demonstrated two separate foci of metastatic PTC with diameters of
1.1 and 0.7 cm, a gray-brown colour and clear resection margins
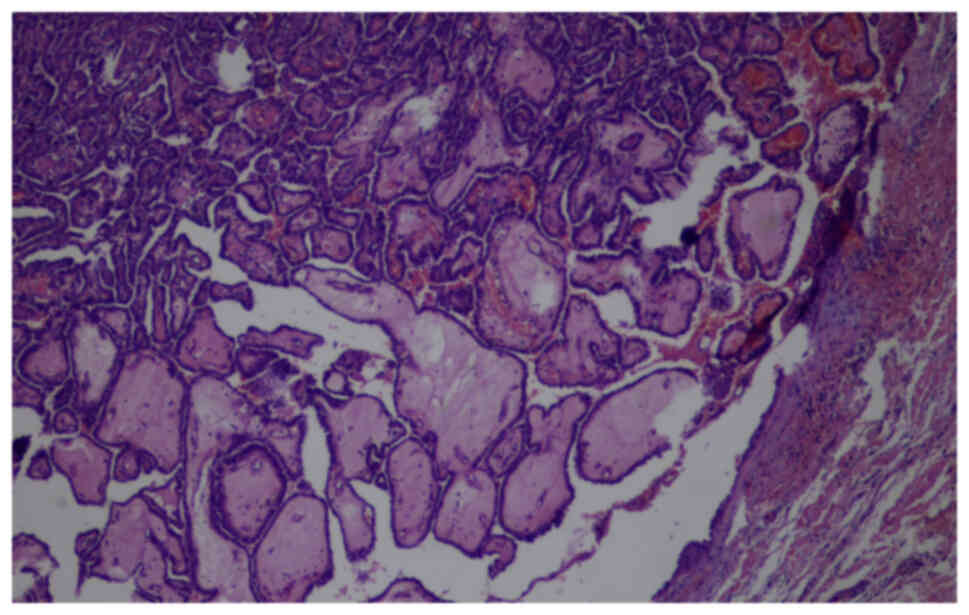
(Fig. 7). Tissue pathology of
paraffin-embedded samples demonstrated that these lesions were skin
metastases of PTC (Fig. 8). As the
metastatic nodules were completely removed, the patient was
discharged from the hospital with continued oral levothyroxine
therapy. The patient has been followed up every 3 months and the
prognosis is good. At the time of writing, no evidence of
recurrence has been found (TSH level, 0.83 µIU/ml and Tg level,
15.70 µg/l).
Tissue analysis
The tissue samples were all fixed in 10% neutral
formalin solution and embedded in paraffin at room temperature for
24 h. Tissue samples were sectioned into 3-µm thick sections.
Samples were blocked using 3% H2O2 at 37°C
for 8 min. Primary antibody staining was performed using the
VENTANA® anti-BRAF V600E (VE1) mouse monoclonal antibody
immunohistochemistry kit (cat. no. 07862270001; antibody dilution,
0.2%; Roche Diagnostics, Ltd.), incubated at 37°C for 40 min.
Secondary antibody staining was performed using the ultraView
universal DAB detection kit (cat. no. 05269806001; Roche
Diagnostics, Ltd.), which uses the horseradish peroxidase
conjugate, and incubated at 37°C for 8 min. The stained sections
were counterstained with haematoxylin and eosin at room temperature
for 5 min, and images were captured using a light microscope
(Olympus BX51; Olympus Corporation).
Discussion
Among the sites of skin metastasis of PTC, the
scalp, face and neck are the most common, probably due to the rich
dermal capillary network, which can capture tumour cell emboli from
the blood circulation and provide an optimal background for
metastasis to occur (11,12,16–20).
Other potential mechanisms for skin metastasis may include direct
extension, haematogenous or lymphatic spread, needle-tract seeding,
surgical drainage and inappropriate surgical procedures (20,21).
The general risk of PTC implantation metastasis is <0.009%
(22). Excisional biopsy rather
than fine-needle aspiration biopsy (FNAB) is advised for a definite
diagnosis of PTC due to inconclusive results using FNAB (13).
After more demolitive surgery, interventions are
affected due to more severe complications. The VEGF pathway has
been suggested as a useful marker for the identification of
non-advanced PTC patients with structural recurrence (23). Fluorine 18-fluorodeoxyglucose PET/CT
has been suggested to be superior to conventional imaging in
identifying disease persistence (24). For patients who do not tolerate
invasive exams, transcutaneous laryngeal ultrasonography is an
alternative painless and inexpensive method in the evaluation of
vocal fold function (25).
To further explore the characteristics of skin
metastases in patients with PTC, including various
clinicopathological characteristics, a literature review of
published articles from the past decade was performed. The search
strategy of the PubMed (https://www.ncbi.nlm.nih.gov/pubmed/) database was as
follows: i) Key words ‘papillary thyroid carcinoma’ AND ‘skin
metastasis’; and ii) English-language articles published between
January 2014 and January 2024. The results of this analysis are
shown in Table I.
 | Table I.Analysis of included studies of
patients with skin metastasis from PTC. |
Table I.
Analysis of included studies of
patients with skin metastasis from PTC.
| First author,
year | Country of
residence | Age, years | Sex | First surgery | RAI | Tg level, µg/l | Levothyr-oxine
therapy | Distant meta
stasis | Interval,
yearsa | Skin metastasis
location | Size, cm | Treatment | Follow-up,
months | Outcome | Gene mutation | Positive IHC
results | (Refs.) |
|---|
| Kwon et al,
2014 | Korea | 55 | Female | TT and CCLND | Yes | 0.08 | NM | No | 3 | Right anterior
neck | 0.6×0.4 and 0.3 | EB | 4 | SD | NM | TTF-1 and Tg | (10) |
| Soylu et al,
2017 | Turkey | 83 | Female | TT | Yes | NM | Yes | No | 3 | Right upper neck | 1.1 and 1.1 | EB | NM | NM | NM | PAX-8 | (13) |
|
| Turkey | 65 | Female | TT and CCLND | Yes | NM | Yes | No | 5 | Left side of
neck | 0.4 and 0.3 | EB | NM | NM | NM | TTF-1 and Tg |
|
| Cheng and Hu,
2020 | China | 63 | Female | TT and LND | No | NM | NM | Yes | 0.83 | Left
supracla-vicular fossa | Irregularly
shaped | External beam
radiotherapy | 6 | Died | NM | TTF-1 and Tg | (15) |
| Alwhaid et
al, 2022 | Saudi Arabia | 70 | Female | TT | No | 3.431 | Yes | Yes | 30 | Scalp and right
arm | 1.0×1.0 and
1.5×1.5 | Sorafenib | 6 | Died | NM | TTF-1 and Tg | (18) |
| Liu et al,
2022 | China | 57 | Male | TCS and CLND | NM | NM | NM | NM | 7 | Right shoulder neck
axilla | 17.0×15.0, 3.0×1.5
and 7.5×5.0 | EB | 60 | SD | NM | TTF-1 | (26) |
| Choi et al,
2023 | Korea | 44 | Female | TT | Yes | 1.00 | Yes | No | 10 | Right side of
neck | 1.0×0.8, 0.3×0.2
and 0.2×0.2 | EB | NM | NM |
BRAFV600E and
TERTC228T | NM | (21) |
| Present case | China | 26 | Female | TCS and CCLND | No | 1.20 | Yes | No | 2.5 | left anterior neck
above the first surgical scar | 1.2×0.8 and
0.9×0.6 | EB | 5 | SD |
BRAFV600E | NM |
|
The analysis included 7 patients, 1 male (14.3%) and
6 females (85.7%). The evaluated patients were all from
Asian-European countries, and the mean age was 62.43±12.32 years.
Female patients were more frequently reported and therefore
appeared to be more susceptible to developing skin metastasis from
PTC, although the findings of Soylu et al (13) yielded a different conclusion: there
was no sex predominance in the skin metastasis of PTC. The onset of
skin metastasis ranged from 1 month to 30 years after the first
surgery for PTC, and the mean interval between the first surgery
and skin metastasis was 8.3 years, which is similar to that
reported by Alwhaid et al (18). This study reported the case of a
70-year-old woman with an 8-month history of two painful and itchy
skin nodules over the scalp and the medial aspect of the right arm.
The patient had a history of total thyroidectomy for PTC 30 years
prior and a computed tomography-positron emission tomography scan
showed multiple lung and skeletal metastases.
The present analysis showed that all patients
underwent thyroid cancer surgeries, with or without central
cervical lymph node dissection and radioactive iodine treatment.
The included patients had a range of skin metastasis sizes (from
0.2 to 17.0 cm) and locations (including the neck, supraclavicular
fossa, scalp, axilla and arm), but that the lesions were
predominantly located on the neck, and that the patients were given
different treatments, including thyroid cancer surgery, radioactive
iodine and external beam therapy, according to their specific
diagnosis. Of the included patients, 2 patients with distant
metastases succumbed to the metastasis 6 months later, and the
remaining 5 patients had stable disease or no reported disease
during the follow-up period. A total of 71.4% of patients' skin
metastases were resected. Except for 1 patient without a diagnosis
of skin metastasis by immunohistochemistry (IHC), the other 6
patients reported similar IHC test results: Thyroid transcription
factor (TTF-1) and Tg were positive, due to a thyroid cell origin
of the lesions. The roles of gene mutations, particularly
BRAF and telomerase reverse transcriptase (TERT)
mutations, in PTC have been investigated over the past decades.
Choi et al (21) examined
the patient tissue sample for BRAF and TERT
mutations, and the results were positive for both. There was
insufficient data on Tg levels and the use of oral levothyroxine
within the literature. The present study reported the case of a
26-year-old female patient. This was younger than the mean age of
the included literature patients (62.43±12.32 years). Regarding the
present study, the patient's skin metastasis may have resulted from
PTC cells that contaminated the surrounding tissue. Furthermore, it
may be that the surgeons had insufficient experience in this
procedure, as this was the only patient to have presented with PTC
skin metastasis in Yantaishan Hospital up to that time.
In terms of epidemiology, skin metastasis of PTC is
rarely observed, and treatment may be delayed for a long time due
to an unclear diagnosis and result in a poor prognosis. IHC
testing, such as for TTF-1 and Tg, can be used to distinguish
primary skin tumours from PTC skin metastases (26). Skin metastasis may be suspected in
patients with a history of PTC who develop an upper body skin
lesion (24). The patient of the
present study had a BRAFV600E mutation, and the
case reported by Choi et al (21) had both BRAF and TERT
gene mutations. Both patients underwent surgery and were provided
long-term surveillance for recurrence (21).
The treatments for skin metastasis of PTC are as
follows: i) Isolated skin metastasis may be successfully treated
through surgical resection (10);
and ii) for skin metastasis with systemic disease, treatment with
radioiodine therapy, external beam radiation therapy or targeted
therapy such as sorafenib, has been suggested (10,18,22,26).
In particular, patients with co-occurring BRAF and
TERT promoter mutations in PTC should undergo long-term
surveillance for recurrence due to the high risk of aggressive
characteristics and distant metastasis (21).
According to the diagnostic and therapeutic results
of the present case study and the literature review, in individuals
with a prior medical history of PTC, occurrence of PTC skin
metastasis should be considered even in the presence of normal
blood or other parameters, such as neck ultrasounds and CT, during
follow-up. When skin metastasis of PTC is suspected, excisional
biopsy, IHC testing and gene mutation testing may be performed, and
the patient's past medical history should be assessed. The use of
these methods as early as possible could improve the diagnosis and
therapeutic results of patients with skin metastasis from PTC. For
high-risk patients, i.e., those with skin metastasis from PTC with
BRAF and TERT gene mutations, long-term surveillance
for recurrence should be advised for patients with a poor
prognosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
HC was responsible for the conception and design of
the study. YQ provided CT images, performed the first and second
surgery, and gave administrative support. DW performed the
ultrasound-guided punch biopsy and provided related information for
pathology. All authors helped to write the manuscript. All authors
read and approved the final version of the manuscript. HC, DW and
YQ confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
The present study was approved by the Clinical Trial
Ethics Committee of Yantaishan Hospital (Yantai, China; approval
no. LL-2024-101-L).
Patient consent for publication
The patient provided written informed consent for
publication of the associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pelizzo MR, Dobrinja C, Casal Ide E, Zane
M, Lora O, Toniato A, Mian C, Barollo S, Izuzquiza M, Guerrini J,
et al: The role of BRAF(V600E) mutation as poor prognostic factor
for the outcome of patients with intrathyroid papillary thyroid
carcinoma. Biomed Pharmacother. 68:413–417. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhao H, Li H and Huang T: High urinary
iodine, thyroid autoantibodies, and thyroid-stimulating hormone for
papillary thyroid cancer risk. Biol Trace Elem Res. 184:317–324.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Davies L and Welch HG: Increasing
incidence of thyroid cancer in the United States, 1973–2002. JAMA.
295:2164–2167. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tufano RP, Teixeira GV, Bishop J, Carson
KA and Xing M: BRAF mutation in papillary thyroid cancer and its
value in tailoring initial treatment: A systematic review and
meta-analysis. Medicine (Baltimore). 91:274–286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ryu YJ and Yoon JH: Chronic lymphocytic
thyroiditis protects against recurrence in patients with cN0
papillary thyroid cancer. Surg Oncol. 34:67–73. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Paschke R, Lincke T, Müller SP, Kreissl
MC, Dralle H and Fassnacht M: The treatment of well-differentiated
thyroid carcinoma. Dtsch Arztebl Int. 112:452–458. 2015.PubMed/NCBI
|
|
7
|
Ito Y, Miyauchi A, Kobayashi K, Kihara M
and Miya A: Static and dynamic prognostic factors of papillary
thyroid carcinoma. Endocr J. 61:1145–1151. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xing M, Alzahrani AS, Carson KA, Viola D,
Elisei R, Bendlova B, Yip L, Mian C, Vianello F, Tuttle RM, et al:
Association between BRAF V600E mutation and mortality in patients
with papillary thyroid cancer. JAMA. 309:1493–1501. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chung JH: BRAF and TERT promoter
mutations: Clinical application in thyroid cancer. Endocr J.
67:577–584. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kwon H, Kim H, Park S, Song DE, Kim WG,
Kim TY, Shong YK and Kim WB: Solitary skin metastasis of papillary
thyroid carcinoma. Endocrinol Metab. 29:579–583. 2014. View Article : Google Scholar
|
|
11
|
Cawley EP and Weary PE: The evaluation of
neoplastic metastases to the skin. Arch Dermatol. 90:262–265. 1964.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dahl PR, Brodland DG, Goellner JR and Hay
ID: Thyroid carcinoma metastatic to the skin: A cutaneous
manifestation of a widely disseminated malignancy. J Am Acad
Dermatol. 36:531–537. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Soylu S, Arikan AE, Teksoz S, Ozcan M and
Bukey Y: Skin metastasis on the neck: An unusual presentation of
recurrence of papillary thyroid carcinoma. Gland Surg. 6:594–597.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Song HJ, Xue YL, Xu YH, Qiu ZL and Luo QY:
Rare metastases of differentiated thyroid carcinoma: Pictorial
review. Endocr-Relat Cancer. 18:R165–174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cheng SH and Chu-Sung Hu S: Skin
metastasis from papillary thyroid carcinoma: A rare case with an
unusual clinical presentation. Australas J Dermatol. 61:e374–e376.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Avram AM, Gielczyk R, Su L, Vine AK and
Sisson JC: Choroidal and skin metastases from papillary thyroid
cancer: Case and a review of the literature. J Clin Endocr Metab.
89:5303–5307. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cohen PR: Metastatic papillary thyroid
carcinoma to the nose: Report and review of cutaneous metastases of
papillary thyroid cancer. Dermatol Pract Concept. 5:7–11. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Alwhaid MS, Mhish O, Tunio MA, AlMalki S,
Al Asiri M and Al-Qahtani K: Skin metastasis occurring 30 years
after thyroidectomy for papillary thyroid carcinoma. Cureus.
14:e221802022.PubMed/NCBI
|
|
19
|
Reusser NM, Holcomb M, Krishnan B, Rosen T
and Orengo IF: Cutaneous metastasis of papillary thyroid carcinoma
to the neck: A case report and review of the literature. Dermatol
Online J. 21:82014.
|
|
20
|
Farina E, Monari F, Tallini G, Repaci A,
Mazzarotto R, Giunchi F, Panzacchi R, Cammelli S, Padula GD,
Deodato F, et al: Unusual thyroid carcinoma metastases: A case
series and literature review. Endocr Pathol. 27:55–64. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Choi JH, Yu HW, Lee JK, Kim W, Choi JY, Na
HY, Park SY, Ahn CH, Moon JH, Choi SI, et al: BRAFV600Eand TERT
promoter C228T mutations on ThyroSeq v3 analysis of delayed skin
metastasis from papillary thyroid cancer: A case report and
literature review. World J Surg Oncol. 21:492023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Polyzos SA and Anastasilakis AD: A
systematic review of cases reporting needle tract seeding following
thyroid fine needle biopsy. World J Surg. 34:844–851. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Marotta V, Sciammarella C, Capasso M,
Testori A, Pivonello C, Chiofalo MG, Gambardella C, Grasso M,
Antonino A, Annunziata A, et al: Germline polymorphisms of the
VEGF-pathway predict recurrence in non-advanced differentiated
thyroid cancer. J Clin Endocr Metab. 102:661–671. 2017.PubMed/NCBI
|
|
24
|
Gambardella C, Offi C, Patrone R, Clarizia
G, Mauriello C, Tartaglia E, Di Capua F, Di Martino S, Romano RM,
Fiore L, et al: Calcitonin negative medullary thyroid carcinoma: A
challenging diagnosis or a medical dilemma? BMC Endocr Disord.
19:452019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gambardella C, Offi C, Romano RM, De Palma
M, Ruggiero R, Candela G, Puziello A, Docimo L, Grasso M and Docimo
G: Transcutaneous laryngeal ultrasonography: A reliable,
non-invasive and inexpensive preoperative method in the evaluation
of vocal cords motility-A prospective multicentric analysis on a
large series and a literature review. Updates Surg. 72:885–892.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Liu Z, Liu X, Xu Q and Lin C: Papillary
thyroid carcinoma with shoulder skin metastasis: A case report and
literature review. Asian J Surg. 45:1966–1967. 2022. View Article : Google Scholar : PubMed/NCBI
|