|
1
|
Croitoru A and Balgradean M:
Treatment-associated side effects in patients with
steroid-dependent nephrotic syndrome. Maedica (Bucur). 17:285–290.
2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Schijvens AM, Teeninga N, Dorresteijn EM,
Teerenstra S, Webb NJ and Schreuder MF: Steroid treatment for the
first episode of childhood nephrotic syndrome: Comparison of the 8
and 12 weeks regimen using an individual patient data
meta-analysis. Eur J Pediatr. 180:2849–2859. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Torres VE, Ahn C, Barten TRM, Brosnahan G,
Cadnapaphornchai MA, Chapman AB, Cornec-Le Gall E, Drenth JPH,
Gansevoort RT, Harris PC, et al: KDIGO 2025 clinical practice
guideline for the evaluation, management, and treatment of
autosomal dominant polycystic kidney disease (ADPKD): Executive
summary. Kidney Int. 107:234–254. 2025.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Alssum LR: Repeated implants failure in
young patient with idiopathic nephrotic syndrome: A case report
with brief review of the literature. BMC Oral Health.
24(25)2024.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Thorn GW, Forsham PH, Frawley TF, Hill SR
Jr, Roche M, Staehelin D and Wilson DL: The clinical usefulness of
ACTH and cortisone. N Engl J Med. 242:824–834. 1950.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zulfiqar Z, Lanewala F, Khatri S, Bajeer
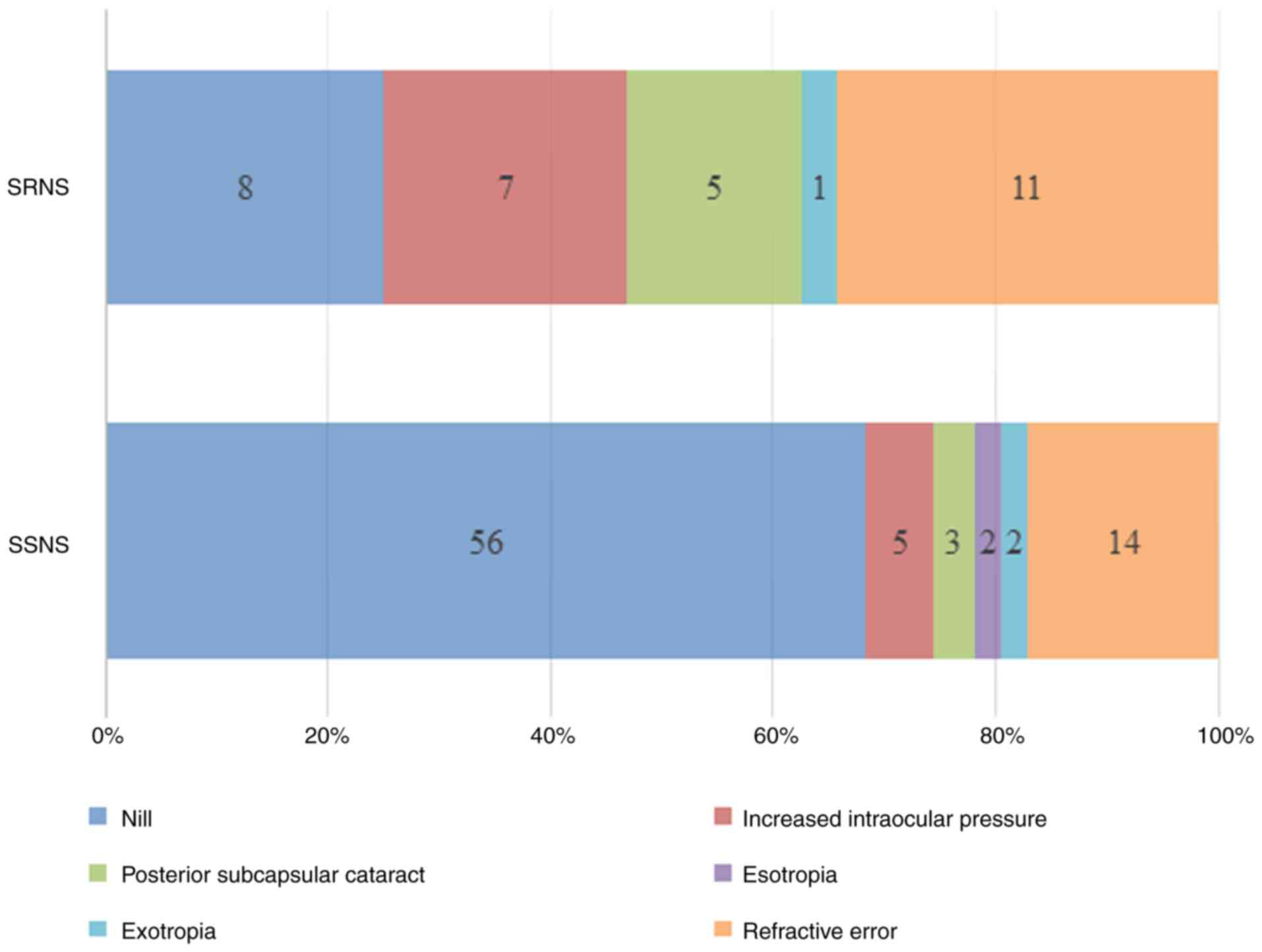
I, Aziz M and Hashmi S: Steroid induced ocular complications in
idiopathic nephrotic syndrome: A cross sectional single center
study. J Pak Med Assoc. 74:315–319. 2024.PubMed/NCBI View Article : Google Scholar
|
|
7
|
James ER: The etiology of steroid
cataract. J Ocul Pharmacol Ther. 23:403–420. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu D, Ahmet A, Ward L, Krishnamoorthy P,
Mandelcorn ED, Leigh R, Brown JP, Cohen A and Kim H: A practical
guide to the monitoring and management of the complications of
systemic corticosteroid therapy. Allergy Asthma Clin Immunol.
9(30)2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Agrawal V, Devpura K, Mishra L and Agarwal
S: Study on steroid induced ocular findings in children with
nephrotic syndrome. J Clin Diagn Res. 11:SC05–SC06. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sato M, Ishikura K, Ando T, Kikunaga K,
Terano C, Hamada R, Ishimori S, Hamasaki Y, Araki Y, Gotoh Y, et
al: Prognosis and acute complications at the first onset of
idiopathic nephrotic syndrome in children: A nationwide survey in
Japan (JP-SHINE study). Nephrol Dial Transplant. 36:475–481.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Elsharkawy MM, Abd Elrahman HM, Omar KAA
and Deiaeldin YA: Assessment of ocular manifestations in children
with nephrotic syndrome during steroid treatment. Egypt J Hosp Med.
91:4672–4678. 2023.
|
|
12
|
Gaur S, Joseph M, Nityanandam S,
Subramanian S, Koshy AS, Vasudevan A, Phadke KD and Iyengar A:
Ocular complications in children with nephrotic syndrome on long
term oral steroids. Indian J Pediatr. 81:680–683. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Toruan YML, Trihono PP, Sitorus RS and
Dwipoerwantoro PG: Ocular complications in pediatric nephrotic
syndrome treated with corticosteroids. Paediatr Indones. 64:1–9.
2024.
|
|
14
|
Veltkamp F, Rensma LR and Bouts AHM:
LEARNS consortium. Incidence and relapse of idiopathic nephrotic
syndrome: Meta-analysis. Pediatrics.
148(e2020029249)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Niaudet P and Boyer O: Idiopathic
nephrotic syndrome in children: Clinical aspects. In: Avner E,
Harmon W, Niaudet P and Yoshikawa N (eds) Pediatric Nephrology.
Springer, Berlin, Heidelberg, pp667-702, 2009.
|
|
16
|
Zotta F, Vivarelli M and Emma F: Update on
the treatment of steroid-sensitive nephrotic syndrome. Pediatr
Nephrol. 37:303–314. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Falkner B, Gidding SS, Baker-Smith CM,
Brady TM, Flynn JT, Malle LM, South AM, Tran AH and Urbina EM:
American Heart Association Council on Hypertension et al.
Pediatric primary hypertension: An underrecognized condition: A
scientific statement from the American heart association.
Hypertension. 80:e101–e111. 2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lombel RM, Gipson DS and Hodson EM: Kidney
Disease. Improving Global Outcomes: Treatment of steroid-sensitive
nephrotic syndrome: New guidelines from KDIGO. Pediatr Nephrol.
28:415–426. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Al-Khafaji ZNH and Al Salam MSN:
VisualAcuity threshold for CataractsSurgeryat a tertiary eye center
in Iraq. Pak J Ophthalmol. 39:319–322. 2023.
|
|
20
|
Olonan LRN, Pangilinan CAG and Yatco MM:
Steroid-induced cataract and glaucoma in pediatric patients with
nephrotic syndrome. Philipp J Ophthalmol. 34:59–62. 2009.
|
|
21
|
Ozaltin F, Heeringa S, Poyraz CE, Bilginer
Y, Kadayifcilar S, Besbas N, Topaloglu R, Ozen S, Hildebrandt F and
Bakkaloglu A: Eye involvement in children with primary focal
segmental glomerulosclerosis. Pediatr Nephrol. 23:421–427.
2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Phulke S, Kaushik S, Kaur S and Pandav SS:
Steroid-induced glaucoma: An avoidable irreversible blindness. J
Curr Glaucoma Pract. 11:67–72. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hayasaka Y, Hayasaka S and Matsukura H:
Ocular findings in Japanese children with nephrotic syndrome
receiving prolonged corticosteroid therapy. Ophthalmologica.
220:181–185. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kyrieleis HA, Löwik MM, Pronk I, Cruysberg
HR, Kremer JA, Oyen WJ, van den Heuvel BL, Wetzels JF and
Levtchenko EN: Long-term outcome of biopsy-proven, frequently
relapsing minimal-change nephrotic syndrome in children. Clin J Am
Soc Nephrol. 4:1593–1600. 2009.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Green MB and Duker JS: Adverse ocular
effects of systemic medications. Life (Basel).
13(660)2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mohan R and Muralidharan AR: Steroid
induced glaucoma and cataract. Indian J Ophthalmol. 37:13–16.
1989.PubMed/NCBI
|