|
1
|
Wang C, Tian F, Zhou Y, He W and Cai Z:
The incidence of cervical spondylosis decreases with aging in the
elderly, and increases with aging in the young and adult
population: A hospital based clinical analysis. Clin Interv Aging.
11:47–53. 2016.PubMed/NCBI
|
|
2
|
Que Q, Ye X, Su Q, Weng Y, Chu J, Mei L,
Huang W, Lu R and Zheng G: Effectiveness of acupuncture
intervention for neck pain caused by cervical spondylosis: Study
protocol for a randomized controlled trial. Trials. 14:1862013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Strine TW and Hootman JM: US national
prevalence and correlates of low back and neck pain among adults.
Arthritis Rheum. 57:656–665. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hilibrand AS, Carlson GD, Palumbo MA,
Jones PK and Bohlman HH: Radiculopathy and myelopathy at segments
adjacent to the site of a previous anterior cervical arthrodesis. J
Bone Joint Surg Am. 81:519–528. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Matsumoto M, Okada E, Ichihara D, Watanabe
K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami
A, et al: Anterior cervical decompression and fusion accelerates
adjacent segment degeneration: comparison with asymptomatic
volunteers in a ten year magnetic resonance imaging follow-up
study. Spine. 35:36–43. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fernström U: Arthroplasty with
intercorporal endoprothesis in herniated disc and in painful disc.
Acta Chir Scand Suppl. 357:154–159. 1966.PubMed/NCBI
|
|
7
|
Leung C, Casey AT, Goffin J, Kehr P,
Liebig K, Lind B, Logroscino C and Pointillart V: Clinical
significance of heterotopic ossification in cervical disc
replacement: A prospective multicenter clinical trial.
Neurosurgery. 57:759–763. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Malham GM, Parker RM, Ellis NJ, Chan PG
and Varma D: Cervical artificial disc replacement with ProDisc-C:
Clinical and radiographic outcomes with long-term follow-up. J Clin
Neurosci. 21:949–953. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sasso RC, Anderson PA, Riew KD and Heller
JG: Results of cervical arthroplasty compared with anterior
discectomy and fusion: Four-year clinical outcomes in a
prospective, randomized controlled trial. Orthopedics. 34:8892011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Burkus JK, Haid RW, Traynelis VC and
Mummaneni PV: Long term clinical and radiographic outcomes of
cervical disc replacement with the Prestige disc: results from a
prospective randomized controlled clinical trial. J Neurosurg
Spine. 13:308–318. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lau J, Ioannidis JP and Schmid CH:
Quantitative synthesis in systematic reviews. Annals of internal
medicine. 127:820–826. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
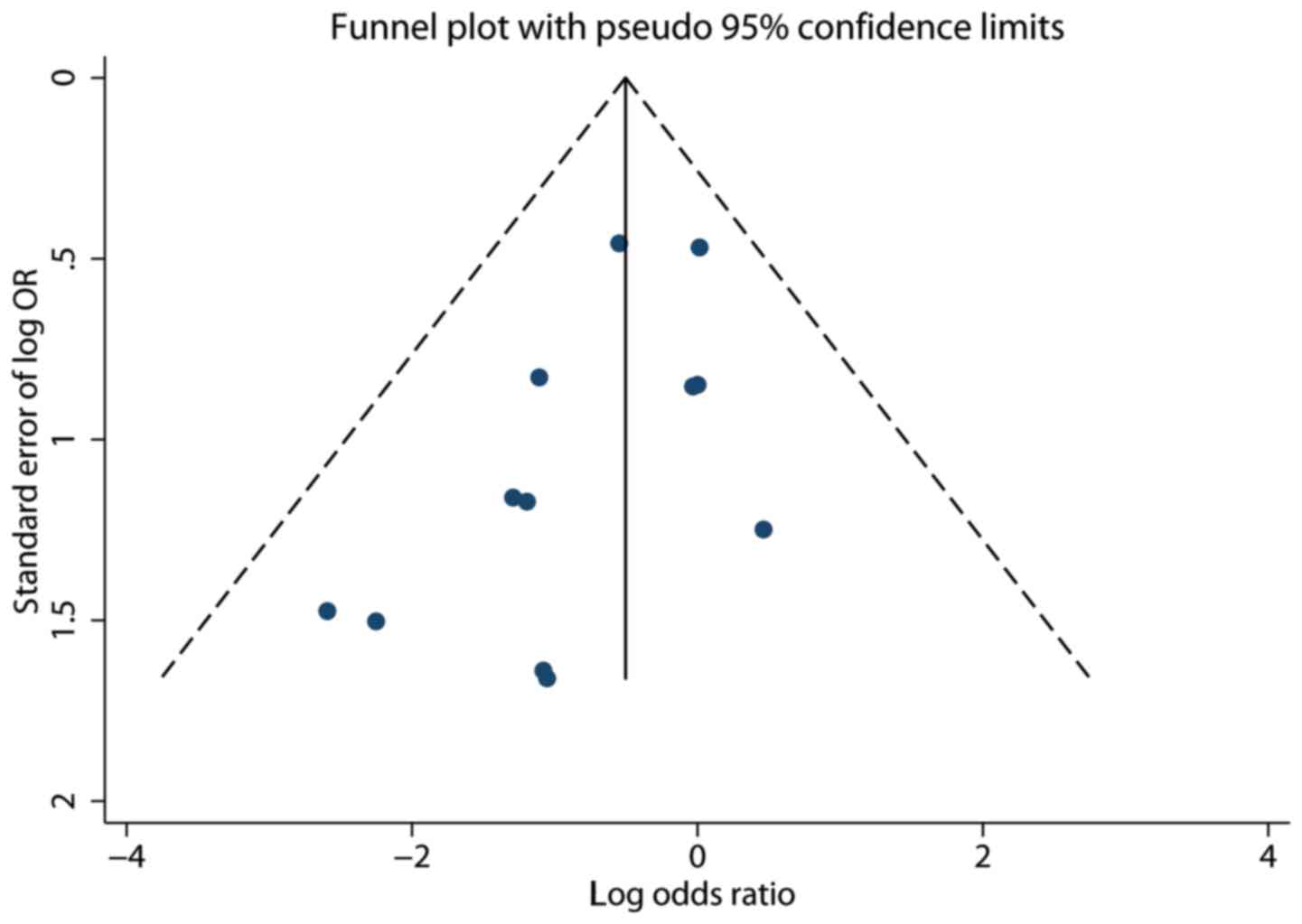
Begg CB and Mazumdar M: Operating
characteristics of a rank correlation test for publication bias.
Biometrics. 50:1088–1101. 1994. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sterne JA, Egger M and Smith GD:
Systematic reviews in health care: Investigating and dealing with
publication and other biases in meta analysis. BMJ. 323:101–105.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Copas J and Shi JQ: Meta analysis, funnel
plots and sensitivity analysis. Biostatistics. 1:247–262. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
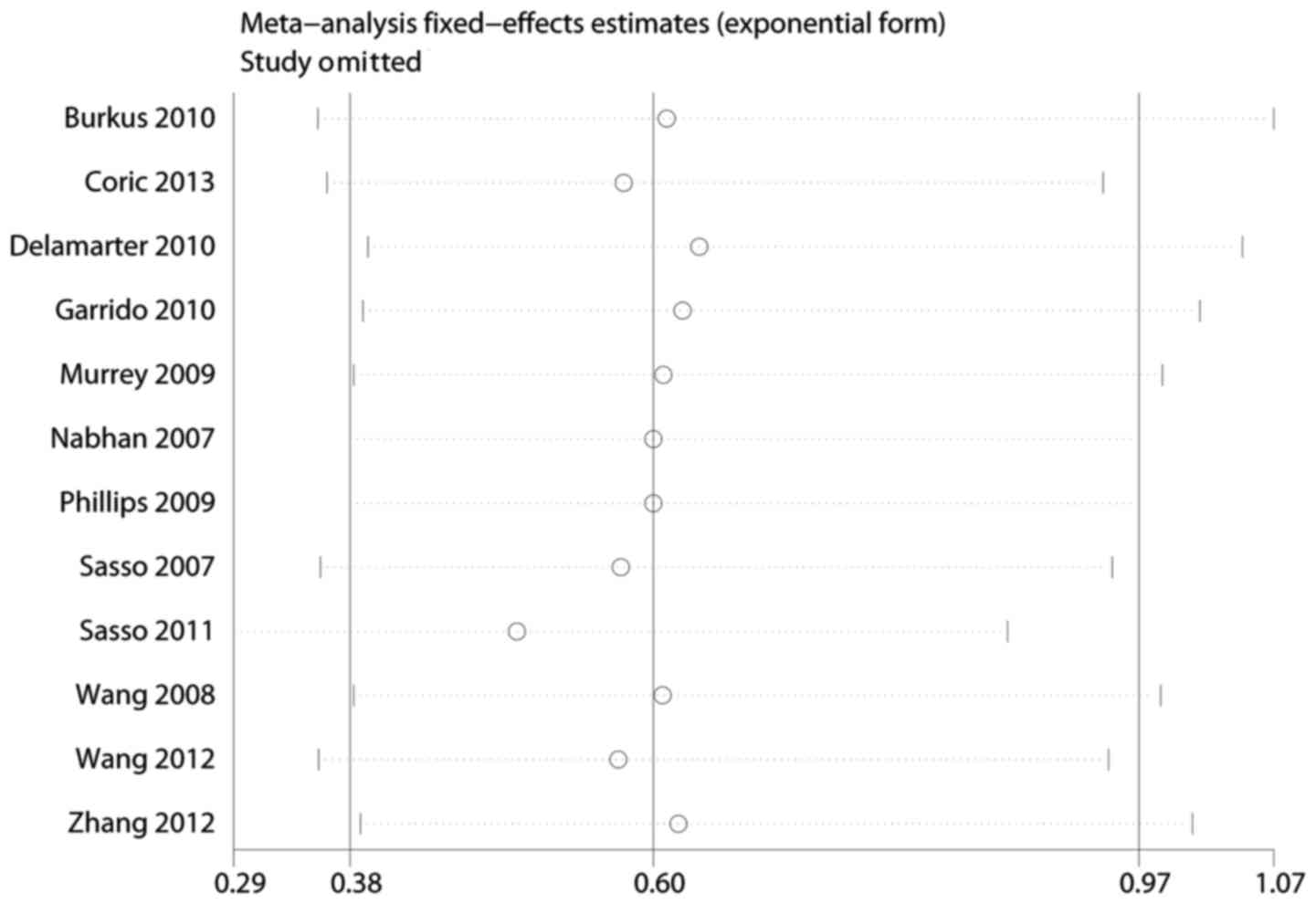
Leimu R and Koricheva J: Cumulative meta
analysis: A new tool for detection of temporal trends and
publication bias in ecology. Proc Biol Sci. 271:1961–1966. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Coric D, Kim PK, Clemente JD, Boltes MO,
Nussbaum M and James S: Prospective randomized study of cervical
arthroplasty and anterior cervical discectomy and fusion with long
term follow-up: results in 74 patients from a single site. J
Neurosurg Spine. 18:36–42. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Delamarter RB, Murrey D, Janssen ME, et
al: Results at 24 months from the prospective, randomized,
multicenter Investigational Device Exemption trial of ProDisc C
versus anterior cervical discectomy and fusion with 4 year
follow-up and continued access patients. SAS journal. 4:122–128.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Garrido BJ, Taha TA and Sasso RC: Clinical
outcomes of Bryan cervical disc arthroplasty a prospective,
randomized, controlled, single site trial with 48 month follow-up.
J Spinal Disord Tech. 23:367–371. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zigler JE, Delamarter R, Murrey D, Spivak
J and Janssen M: ProDisc C and anterior cervical discectomy and
fusion as surgical treatment for single level cervical symptomatic
degenerative disc disease: five year results of a Food and Drug
Administration study. Spine. 38:203–209. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Murrey D, Janssen M, Delamarter R, et al:
Results of the prospective, randomized, controlled multicenter Food
and Drug Administration investigational device exemption study of
the ProDisc C total disc replacement versus anterior discectomy and
fusion for the treatment of 1 level symptomatic cervical disc
disease. Spine J. 9:275–286. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sasso RC, Smucker JD, Hacker RJ and Heller
JG: Clinical outcomes of BRYAN cervical disc arthroplasty: a
prospective, randomized, controlled, multicenter trial with 24
month follow-up. J Spinal Disord Tech. 20:481–491. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nabhan A, Ahlhelm F, Shariat K, et al: The
ProDisc C prosthesis: clinical and radiological experience 1 year
after surgery. Spine. 32:1935–1941. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang HX, Shao YD, Chen Y, et al: A
prospective, randomised, controlled multicentre study comparing
cervical disc replacement with anterior cervical decompression and
fusion. Int Orthop. 38:2533–2541. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang X, Zhang Y and Xiao S: Medium and
long term result of the single level cervical disc arthroplasty for
cervical spondylosis meylopathy. Zhongguo Ji Zhu Ji Sui Za Zhi.
22:879–883. 2012.(In Chinese).
|
|
25
|
Zhang X, Chen C, Zhang Y, et al:
Randomized, controlled, multicenter, clinical trial comparing BRYAN
cervical disc arthroplasty with anterior cervical decompression and
fusion in China. Spine. 37:433–438. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang Y, Cai B, Zhang XS, et al: Clinical
outcomes of single level Bryan cervical disc arthroplasty: A
prospective controlled study. Zhonghua Wai Ke Za Zhi. 46:328–0332.
2008.(In Chinese). PubMed/NCBI
|
|
27
|
Riina J, Patel A, Dietz JW, Hoskins JS,
Trammell TR and Schwartz DD: Comparison of single level cervical
fusion and a metal on metal cervical disc replacement device. Am J
Orthop (Belle Mead NJ). 37:E71–E77. 2008.PubMed/NCBI
|
|
28
|
Phillips FM, Allen TR, Regan JJ, et al:
Cervical disc replacement in patients with and without previous
adjacent level fusion surgery: A prospective study. Spine.
34:556–565. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Peng-Fei S and Yu-Hua J: Cervical disc
prosthesis replacement and interbody fusion: A comparative study.
Int Orthop. 32:103–106. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Heller JG, Sasso RC, Papadopoulos SM, et
al: Comparison of BRYAN cervical disc arthroplasty with anterior
cervical decompression and fusion: clinical and radiographic
results of a randomized, controlled, clinical trial. Spine.
34:101–107. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim SW, Limson MA, Kim SB, Arbatin JJ,
Chang KY, Park MS, Shin JH and Ju YS: Comparison of radiographic
changes after ACDF versus Bryan disc arthroplasty in single and
bi-level cases. Eur Spine J. 18:218–231. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Goffin J, Geusens E, Vantomme N, Quintens
E, Waerzeggers Y, Depreitere B, Van Calenbergh F and van Loon J:
Long term follow-up after interbody fusion of the cervical spine. J
Spinal Disord Tech. 17:79–85. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Porchet F and Metcalf NH: Clinical
outcomes with the Prestige II cervical disc: Preliminary results
from a prospective randomized clinical trial. Neurosurg Focus.
17:E62004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gao Y, Liu M, Li T, Huang F, Tang T and
Xiang Z: A meta-analysis comparing the results of cervical disc
arthroplasty with anterior cervical discectomy and fusion (ACDF)
for the treatment of symptomatic cervical disc disease. J Bone
Joint Surg Am. 95:555–561. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yin S, Yu X, Zhou S, Yin Z and Qiu Y: Is
cervical disc arthroplasty superior to fusion for treatment of
symptomatic cervical disc disease? A meta analysis. Clin Orthop
Relat Res. 471:1904–1919. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang Y, Liang C, Tao Y, Zhou X, Li H, Li
F and Chen Q: Cervical total disc replacement is superior to
anterior cervical decompression and fusion: A meta-analysis of
prospective randomized controlled trials. PLoS One.
10:e01178262015. View Article : Google Scholar : PubMed/NCBI
|