Introduction
Currently, carotid artery stenting (CAS) remains an
effective treatment method for carotid artery stenosis (1). However, following stenting, carotid
artery restenosis is still prone to relapse (2). When restenosis after CAS becomes more
severe, surgical treatments are most likely required. However, when
the stent grows into the carotid artery plaque and even penetrates
the carotid artery adventitia, it creates tremendous difficulty for
treatment (3). For in-stent restenosis
cases, balloon dilatation angioplasty or another stenting method
can be feasible treatment options; however, due to the restriction
of the existing stent, it is difficult to perform balloon
dilatation in a narrow carotid artery; moreover, it is also
difficult for the currently used self-expanding stents to maintain
the blood vessels at a normal diameter (4). For cases of restenosis after stenting, it
is also effective to perform carotid endarterectomy (CEA), a
procedure that can remove the stent together with arteriosclerotic
plaques, which completely solves the issue of carotid artery
stenosis (5). However, because the
stent reinforces the plaques and introduces damage to the blood
vessel, performing CEA with simultaneous stent removal becomes very
difficult. Due to the lack of reports on the treatment of carotid
artery restenosis after stenting by CAS, the present paper reports
one relevant case that was treated in the Neurosurgery Department
of the First Hospital of Jilin University.
Case report
The patient was a 74-year-old male. At 10 months
prior to being re-hospitalized, he underwent a neck blood vessel
examination due to ‘dizziness and fatigue’, and severe stenosis was
identified in the left internal carotid artery. Left internal
carotid stenting was then performed. A 9×40 mm Acculink
self-expanding stent was used, and the stenting process went
smoothly. After the stent was released, the imaging demonstrated
that the residual stenosis was <30%. The patient recovered well
following the surgery, and his preoperative symptoms disappeared,
according to his own statement. After the surgery, he was given
aspirin as an anti-platelet aggregation treatment and a long-term
oral administration of Lipitor to lower blood cholesterol. The
patient was asked to stop smoking and to strictly control his blood
pressure. After surgery, the patient was followed up via telephone.
The patient had been prescribed medication regularly and stopped
smoking, and his blood pressure was stably controlled.
In the last month of follow-up, the patient
gradually felt ‘somnolence and fatigue’, and he returned to the
hospital for treatment. A physical examination revealed no positive
signs of nervous system involvement. A neck ultrasound indicated
that the stent extended from the left common carotid artery to the
internal carotid artery, and restenosis appeared in the left
internal carotid artery, with a stenosis degree of 70–99%. The
continuity of the lattice-like pattern in the hyperechoic shadow of
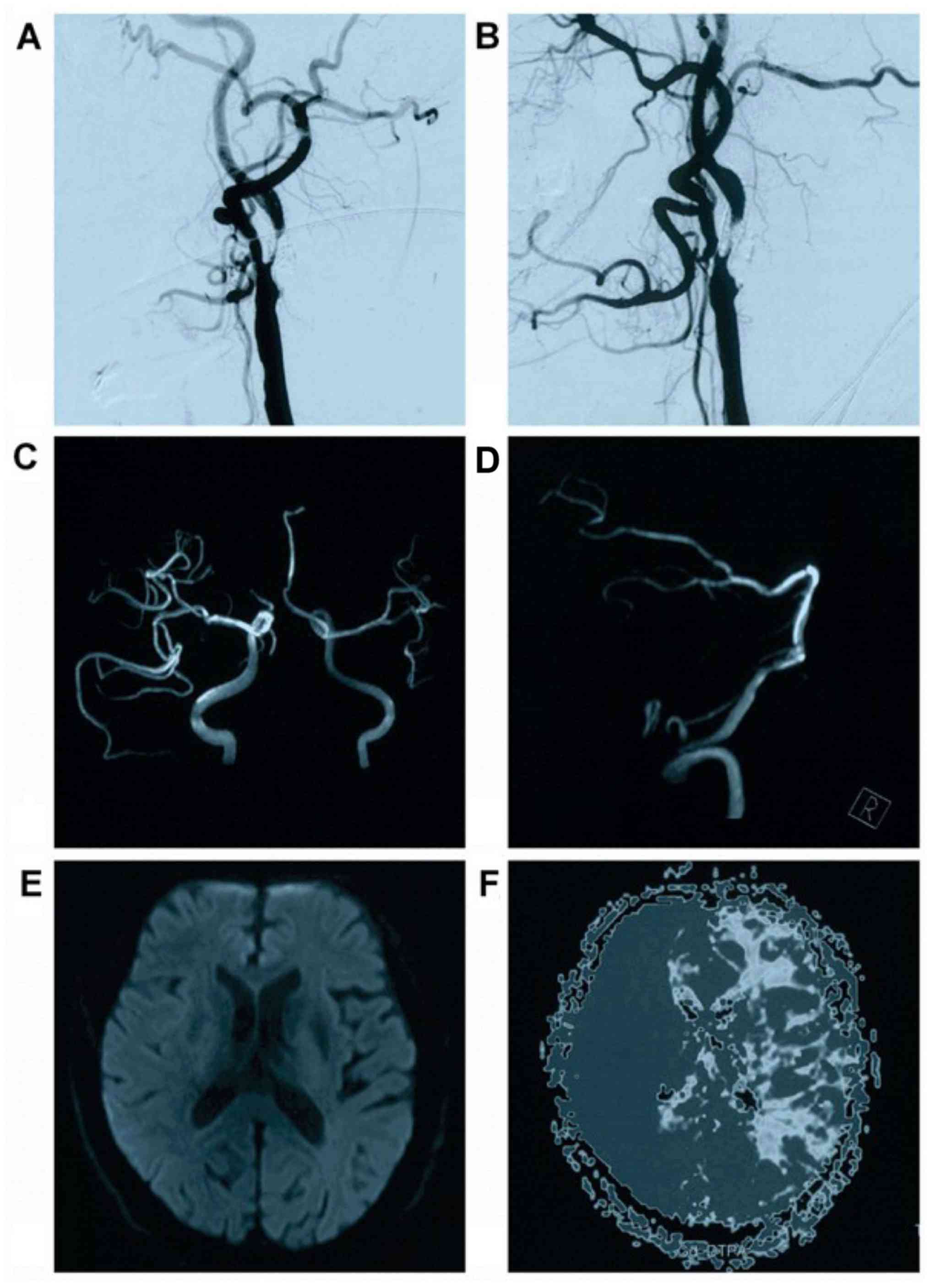
the stent was poor in two locations. Head magnetic resonance
angiography revealed a slightly weaker imaging of the intracranial
left internal carotid artery system and a slight stenosis in the
lower basilar artery. Magnetic resonance imaging did not present
fresh thrombosis, and perfusion magnetic resonance indicated that
the left cerebral hemisphere had ischemic changes. Further neck
digital subtraction angiography examination revealed severe
stenosis in the initial segment of the left internal carotid
artery, with a stenosis degree of ~90%. The stent image could be
seen inside plaques in the left internal carotid artery (Fig. 1).
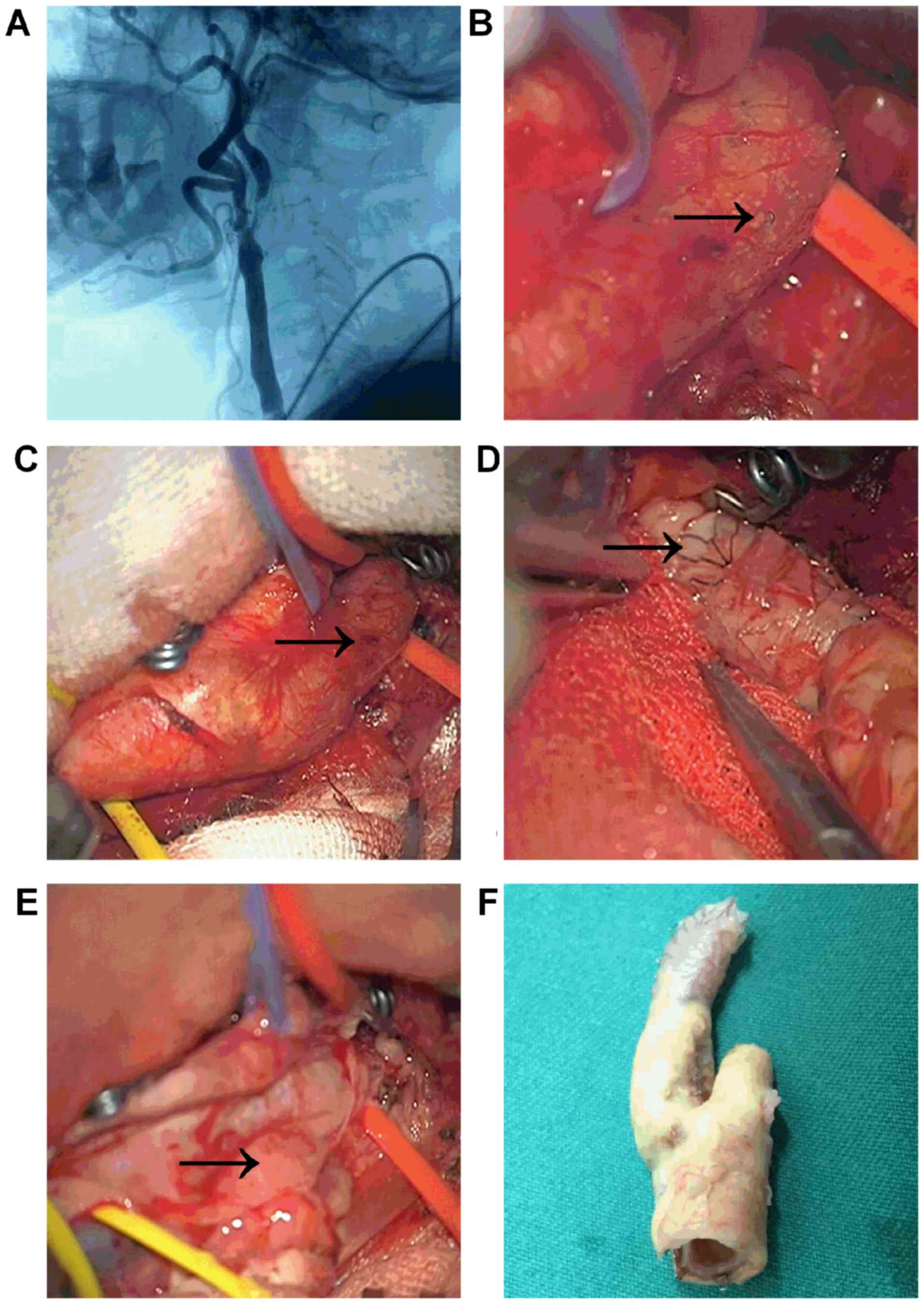
At this point, the patient's condition was clearly
diagnosed as in-stent stenosis after stenting in the carotid
artery, and CEA with simultaneous stent removal was planned. The
surgery was performed under general anesthesia, during which a
longitudinal incision medial to sternocleidomastoid muscle was used
to expose the carotid sheath. After the carotid sheath was opened,
the upper edge of the carotid artery stent was visible and palpable
through the carotid artery wall. After the common carotid artery,
internal carotid artery and external carotid artery were
sufficiently exposed, they were temporarily ligated. The common
carotid artery and internal carotid artery were incised at the
location where the stent remained, and the carotid artery stent
together with the carotid arterial intima and media were then
peeled off until normal arterial lumen was exposed. The surgery
removed the stent and plaques completely, and the adventitia of the
common carotid artery and internal carotid artery were shown to be
intact. The adventitia was then sutured continuously, and the
carotid artery lumen was determined to be unobstructed following
suture (Fig. 2). The patient was
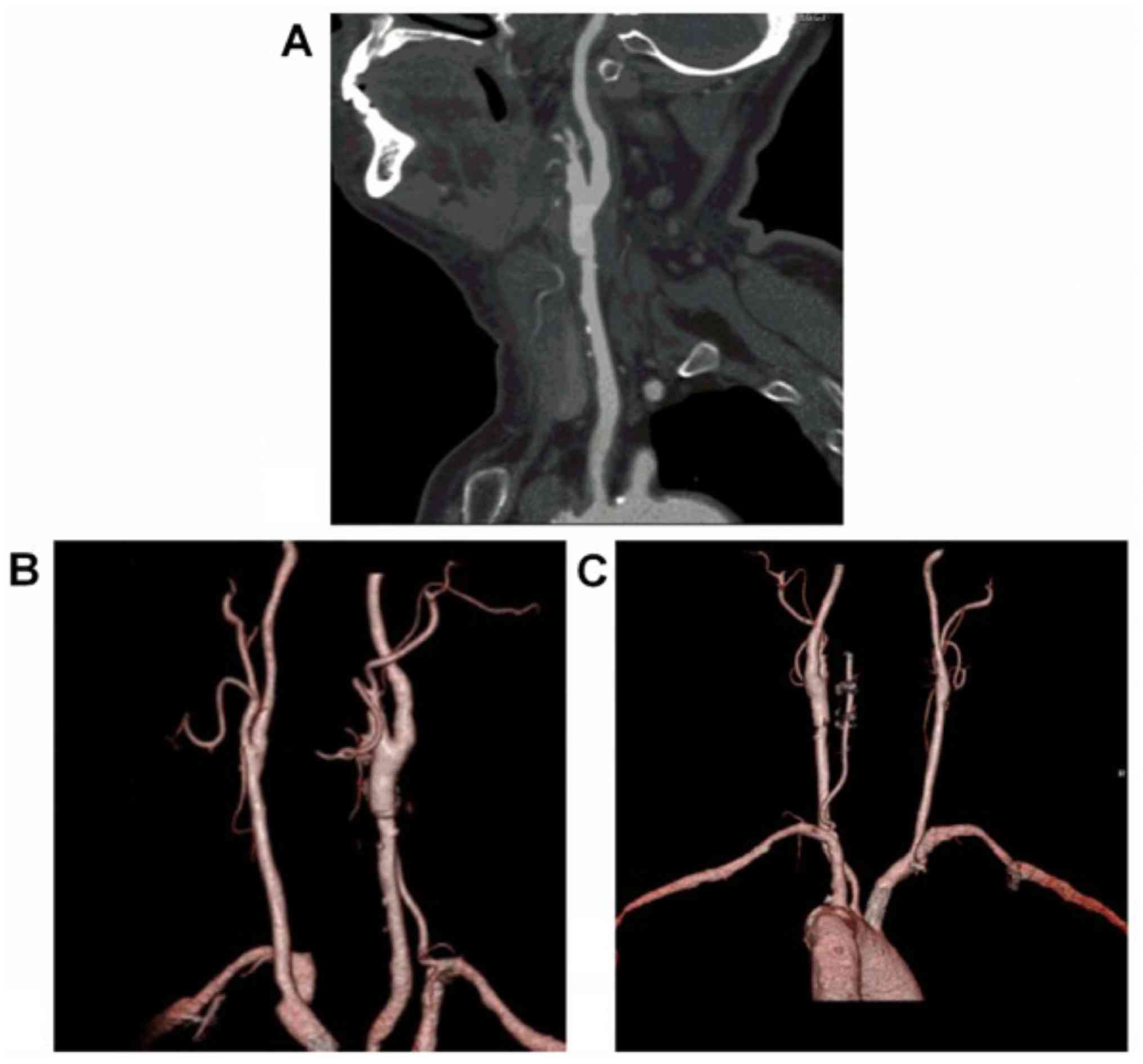
discharged after good postoperative recovery. After being
discharged, the patient received regular dual antiplatelet therapy
and lipid-lowering treatment. Half a year following surgery, head
computed tomography angiography revealed that the lumen of the
internal carotid artery was unobstructed without any stenosis
(Fig. 3).
Discussion
Carotid stenosis in patients is not rare. When its
extent reaches severe stenosis (70–99%) or a moderate degree of
stenosis accompanied by clinical symptoms, patients require
surgical treatment; otherwise, the risk for ischemic stroke is very
high (6,7). At present, the treatment methods for
carotid artery stenosis mainly include CEA and CAS. CEA can remove
atherosclerotic plaques, while CAS uses a balloon to dilate the
stenosis and then implants a self-expanding stent; both methods are
effective methods for treating carotid artery stenosis (8). The results of randomized controlled
clinical trials demonstrated that both CEA and CAS could
effectively treat carotid artery stenosis and that the differences
in complications and long-term prognosis were not significant
(9). In the present case, the patient
received CAS when the carotid stenosis was initially identified,
but he developed in-stent restenosis within 10 months, a shorter
interval than previously reported. Rates of in-stent restenosis
after CAS vary according to literature sources and the definition
of restenosis, ranging from 1% to 21% over 12–18 months (10). There are many causes for in-stent
restenosis. For example, in-stent restenosis was more common in an
open-cell stent group when compared with a closed-cell stent group
after CAS (11). Whether optimal
postoperative oral medication treatment was provided, treatment
with optimal medical therapy, including anti-platelets and statins,
seems to have a beneficial effect on preventing in-stent restenosis
in patients undergoing CAS (12). The
patient in the present case received the best available
postoperative medical therapy, and the risk factors for ischemic
stroke were controlled. The Acculink stent used has an open-cell
design, supporting the research conclusion that open-cell stents
are prone to inducing restenosis.
Restenosis after CAS must be treated. Different
treatment methods are available, such as balloon dilatation
angioplasty, restenting, CEA with simultaneous stent removal, and
carotid bypass reconstruction (13).
If an early carotid stenosis tendency is found after CAS, treatment
with cilostazol may be effective (14). If in-stent stenosis is quite severe, it
can only be addressed with surgical treatment. For example, in
2014, Gandini et al (15)
suggested that drug-eluting balloon dilatation angioplasty for the
treatment of refractory recurrent carotid in-stent restenosis has
great potential (15). Performing
overlap stenting for in-stent restenosis following CAS is also
sometimes feasible (16). However, for
severe restenosis after stenting, particularly in cases with hard
plaques and calcifications, regardless of whether balloon
dilatation or stenting is used, both treatment outcomes could be
poor. In such a case, CEA may be the only option; in the present
case, the patient experienced restenosis after stenting and
received CEA with simultaneous stent removal. In 2013, Zheng et
al (17) reported one case of
endarterectomy following in-stent stenosis occurred. After
reviewing previous reports, they suggested that CEA with stent
removal in the management of in-stent restenosis was a safe,
feasible and effective technique. However, in-stent restenosis
after carotid angioplasty and stenting was a challenge for the
vascular surgeon (18).
The case reported in this paper describes
successfully peeling off the stent, though with great difficulty.
After reviewing previous reports in the literature, the authors
summarize the treatments as follows. First, the design of the
surgical incision should be longer than that of a normal CEA, and
the length of the exposure is necessary to dissect out the metallic
stent. The upper end of the incision must be extended to the
mastoid process along the posterior margin of the parotid gland.
Secondly, apart from a larger incision, when dissecting muscles, it
should be emphasized that the exposure must be sufficient. When
dissecting the sternocleidomastoid muscle, intraoperative incision
of the digastric muscle is not necessary, but the
sternocleidomastoid muscle must be mobilized towards the mastoid
process, and the mobilization of the digastric and
sternocleidomastoid muscles must be sufficient so that the distal
end of the internal carotid artery can be clearly exposed.
Moreover, CEA with stent explantation is more difficult to perform.
During the peeling process, because the stent is already immersed
in the medium of the carotid artery wall and is only wrapped by
adventitia and because plaques have already grown inside the stent,
the surface of the stent is not covered by the carotid artery
intima. Therefore, when opening and cutting the artery, care is
required to remove the stent to avoid vessel wall perforation
(19).
For the case reported in this paper, due to careful
peeling, the carotid adventitia was preserved completely and was
directly sutured. However, when the stent penetrates the carotid
artery, CEA may cause defects in the carotid artery, and patches
may be needed to repair the defects. For example, the report by
Reedy et al mentioned the use of patches (20). Because endarterectomy for the
restenosis after stenting is very difficult to perform, the
incidence of experiencing complications in the course of the
treatment is very high. For example, of the 15 cases reported by
Reichmann et al in 2011 (21),
one case had minor ischemic stroke, and two cases had neck
hematoma; however, the prognoses were all good. It was suggested
that CEA with stent explantation for in-stent restenosis after CAS
seems effective.
Based on the present report and this literature
review of previous endarterectomy treatments for cases of
restenosis after stenting, the authors suggest that CEA of in-stent
stenosis following CAS is beneficial. However, surgical treatment
for in-stent stenosis remains a challenging option.
References
|
1
|
Calvet D and Mas JL: Recent advances in
carotid angioplasty and stenting. Int J Stroke. 11:19–27. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shankar JJ, Zhang J, dos Santos M, Lesiuk
H, Mohan R and Lum C: Factors affecting long-term restenosis after
carotid stenting for carotid atherosclerotic disease.
Neuroradiology. 54:1347–1353. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gonzalez A, Drummond M, McCord S and
Garrett HE Jr.: Carotid endarterectomy for treatment of in-stent
restenosis. J Vasc Surg. 54:1167–1169. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
van Haaften AC, Bots ML, Moll FL and de
Borst GJ: Therapeutic options for carotid in-stent restenosis:
Review of the literature. J Vasc Interv Radiol. 21:1471–1477. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Akin E, Knobloch K, Pichlmaier M and
Haverich A: Instent restenosis after carotid stenting necessitating
open carotid surgical repair. Eur J Cardiothorac Surg. 26:442–443.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rosenfield K, Matsumura JS, Chaturvedi S,
Riles T, Ansel GM, Metzger DC, Wechsler L, Jaff MR and Gray W: ACT
I Investigators: Randomized Trial of Stent versus Surgery for
Asymptomatic Carotid Stenosis. N Engl J Med. 374:1011–1020. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huang JF and Meschia JF: Interventions for
Extracranial Carotid Artery Stenosis: An Update. Curr Treat Options
Cardiovasc Med. 18:342016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Morris S, Patel NV, Dobson J, Featherstone
RL, Richards T, Luengo-Fernandez R, Rothwell PM and Brown MM:
International Carotid Stenting Study investigators: Cost-utility
analysis of stenting versus endarterectomy in the International
Carotid Stenting Study. Int J Stroke. 11:446–453. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Howard G, Roubin GS, Jansen O, Hendrikse
J, Halliday A, Fraedrich G, Eckstein HH, Calvet D, Bulbulia R,
Bonati LH, et al: Carotid Stenting Trialists' Collaboration:
Association between age and risk of stroke or death from carotid
endarterectomy and carotid stenting: A meta-analysis of pooled
patient data from four randomised trials. Lancet. 387:1305–1311.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sorkin GC, Dumont TM, Eller JL, Mokin M,
Hopkins LN, Snyder KV, Siddiqui AH and Levy EI: Instent restenosis
after carotid stenting: Treatment using an off-label cardiac
scoring balloon. J Vasc Interv Neurol. 7:29–34. 2014.PubMed/NCBI
|
|
11
|
Alparslan B, Nas OF, Eritmen UT, Duran S,
Ozkaya G and Hakyemez B: The Effect of Stent Cell Geometry on
Carotid Stenting Outcomes. Cardiovasc Intervent Radiol. 39:507–513.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tendera M, Aboyans V, Bartelink ML,
Baumgartner I, Clément D, Collet JP, Cremonesi A, de Carlo M, Erbel
R, Fowkes FG, et al: European Stroke Organisation; ESC Committee
for Practice Guidelines: ESC Guidelines on the diagnosis and
treatment of peripheral artery diseases: Document covering
atherosclerotic disease of extracranial carotid and vertebral,
mesenteric, renal, upper and lower extremity arteries: the Task
Force on the Diagnosis and Treatment of Peripheral Artery Diseases
of the European Society of Cardiology (ESC). Eur Heart J.
32:2851–2906. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bekelis K, Moses Z, Missios S, Desai A and
Labropoulos N: Indications for treatment of recurrent carotid
stenosis. Br J Surg. 100:440–447. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamagami H, Sakai N, Matsumaru Y, Sakai C,
Kai Y, Sugiu K, Fujinaka T, Matsumoto Y, Miyachi S, Yoshimura S, et
al: Periprocedural cilostazol treatment and restenosis after
carotid artery stenting: The Retrospective Study of In-Stent
Restenosis after Carotid Artery Stenting (ReSISteR-CAS). J Stroke
Cerebrovasc Dis. 21:193–199. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gandini R, Del Giudice C, Da Ros V,
Sallustio F, Altobelli S, D'Onofrio A, Abrignani S, Vasili E,
Stanzione P and Simonetti G: Long-term results of drug-eluting
balloon angioplasty for treatment of refractory recurrent carotid
in-stent restenosis. J Endovasc Ther. 21:671–677. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nishihori M, Ohshima T, Yamamoto T, Goto
S, Nishizawa T, Shimato S, Izumi T and Kato K: Overlap stenting for
in-stent restenosis after carotid artery stenting. Nagoya J Med
Sci. 78:143–149. 2016.PubMed/NCBI
|
|
17
|
Zheng J, Liu L, Cao Y, Zhang D, Wang R and
Zhao J: Carotid endarterectomy with stent removal in management of
in-stent restenosis: A safe, feasible, and effective technique. Eur
J Vasc Endovasc Surg. 47:8–12. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Setacci C, de Donato G, Setacci F,
Pieraccini M, Cappelli A, Trovato RA and Benevento D: In-stent
restenosis after carotid angioplasty and stenting: A challenge for
the vascular surgeon. Eur J Vasc Endovasc Surg. 29:601–607. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vale FL, Fisher WS III, Jordan WD Jr,
Palmer CA and Vitek J: Carotid endarterectomy performed after
progressive carotid stenosis following angioplasty and stent
placement. Case report. J Neurosurg. 87:940–943. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Reedy FM, Colonna M, Genovese V, Mancuso
M, Napoleone M, Notari P and Di Cintio V: Successful surgical
treatment of two patients with restenosis after previous stenting
of the carotid artery. Eur J Vasc Endovasc Surg. 20:99–101. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Reichmann BL, van Laanen JH, de Vries JP,
Hendriks JM, Verhagen HJ, Moll FL and de Borst GJ: Carotid
endarterectomy for treatment of in-stent restenosis after carotid
angioplasty and stenting. J Vasc Surg. 54:87–92. 2011. View Article : Google Scholar : PubMed/NCBI
|