Introduction
The prevalence of chronic degenerative diseases has
increased in the adult Mexican population (1,2). In
Mexico, cardiovascular disease (CVD) was a leading cause of death
in 2015 (3), while
hypercholesterolemia, a major risk factor for CVD, was the most
prevalent type of dyslipidemia in the Mexican population between
2003 and 2005 (4). Statins are
cholesterol-lowering drugs, and in 2012, atorvastatin (ATV) was the
most frequently prescribed statin in Mexico (5). Within liver cells, ATV disrupts
cholesterol biosynthesis by blocking
3-hydroxy-3-methylglutaryl-coenzyme A reductase, which reduces the
amount of cholesterol released into the blood. As a consequence,
low-density lipoprotein cholesterol uptake by liver cells increases
and blood cholesterol levels diminish (6). However, in clinical trials of ATV,
pharmacokinetic parameters including maximum plasma concentration
(Cmax), time to reach Cmax (Tmax),
area under the plasma concentration-time curve (AUC) from time 0 to
the time of last measurement (AUC0-t), AUC from time 0
extrapolated to infinity (AUC0-∞), apparent clearance of
the fraction dose absorbed (Cl/F), elimination rate constant in the
terminal drug phase (Ke) and the half-life in the terminal drug
phase (T1/2) are variable (7). This reflects the underlying variability
in the absorption, distribution, metabolism and excretion (ADME)
processes of ATV, which may affect the pharmacological response
(8). Although in general, genetic
factors influence ~30% of variation in drug disposition and
response (9,10), recent results have indicated that
genetic variability may contribute to >90% of the variance in
ATV plasma concentrations (11).
These differences in the ADME characteristics of ATV have been
attributed to polymorphisms in genes associated with drug
pharmacokinetics, particularly those encoding enzymes and
transporters (7,10,11).
The anti-inflammatory effect of statins has been
investigated (12). The angiotensin
II type 1 receptor (AGTR1) blocks the angiotensin II pathway and
has been associated with the development of atherosclerosis
(12). In addition, polymorphisms in
AGTR1 have been associated with muscle toxicity in patients
treated with statins (13). In
addition to AGTR1, angiotensinogen (AGT) is part of the
renin-angiotensin-aldosterone system (14). An improved response to diuretics has
been observed in the presence of the AGTR1 A1166C and
AGT G-6A polymorphisms in African-American women and a
Chinese population (15,16).
The kallikrein-kinin system is also involved in
multiple cardiovascular events; it modulates the
renin-angiotensin-aldosterone system, promotes vasodilation,
modulates neovascularization and stimulates the inflammatory
response (17). Genetic variants in
the bradykinin B2 receptor (BDKRB2) and endothelial nitric
oxide synthase (eNOS) genes have been associated with CVD
risk (18,19). Notably, the BDKRB2 C(−58)T
polymorphism has been associated with hypertension in an Asian
population; carriers of the C/C genotype had an increased risk,
whereas carriers of the T/T genotype had a decreased risk. However,
in Asian heterozygous carriers, Americans and Europeans, no
association has been identified (20), though an improved response to
enalapril for the treatment of hypertension has been observed in
individuals with the C/C genotype (21).
Although polymorphisms in the AGTR1,
AGT and BDKRB2 genes have been described, there is a
lack of studies on their frequency and effect on ATV
pharmacokinetics. Therefore, the present study aimed to: i)
Identify novel polymorphic variants influencing the pharmacokinetic
parameters of ATV; and ii) associate genotypes with metabolizing
phenotypes.
Materials and methods
Design
A randomized clinical study was conducted in 60
healthy volunteers of Mexican origin to assess the bioequivalence
of a single oral dose (80 mg) of ATV (coated tablets; Pfizer, Inc.,
New York, NY, USA) (7). The study was
performed according to the guidelines of the Declaration of
Helsinki (22), of Tokyo for Good
Clinical Practice Standards (23),
and to Mexican regulations for studies of bioavailability and
bioequivalence (24). The clinical
protocol was approved by the Research and Ethics Committee of the
Clinical and Experimental Pharmacology Center, Ipharma S.A.
(Monterrey, Mexico), and the pharmacogenetic procedure was approved
by the Ethics, Research and Biosecurity Committees of the
University of Monterrey (Monterrey, Mexico). The study was
registered with the Federal Commission for Protection Against
Health Risks under code Atorvastatina/A95-10Bis and in the Register
of Clinical Trials of Australia and New Zealand (registration no.
ACTRN12614000851662). Written informed consent was obtained from
all subjects.
Study population
As described in our preliminary pilot study
(7), a total of 60 healthy male
volunteers of Mexican origin were included in the study from
January 2011 to February 2011, with a mean age of 24.01±4.35 years.
The inclusion criteria were as follows: Non-smoker; 18–45 years
old; weight, ≥50 kg; body mass index, 20–26 kg/m2; availability to
complete the study and normal health status (free from disease).
Health status was assessed based on physical examination, medical
history and clinical and biochemical tests. Insufficiency in any
requirement (abnormal laboratory results, drug abuse, ingestion of
alcohol 1 week prior to the study, prescription or over-the-counter
medication prior to enrollment and reluctance to complete the
study) was reason for exclusion from the study. Women were excluded
as ATV is classified as a pregnancy category X drug (25). All subjects were informed of the aims
of the study.
Sampling
ATV administration and blood sampling were performed
as described in the pilot study (7).
Briefly, peripheral blood (4 ml) was collected in
K2EDTA-coated BD Vacutainers® (BD
Diagnostics, Franklin Lakes, NJ, USA) at different time points:
Prior to drug administration (time 0) and at 17 time points (0.25,
0.5, 0.75, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 12, 24, 36 and 48 h)
after drug administration. The plasma was used for pharmacokinetic
analysis and DNA was isolated from blood cells using an alkaline
lysis method (26). Genomic DNA was
quantified by UV absorbance using a Nanodrop 1000 Spectrophotometer
(Thermo Fisher Scientific, Inc., Waltham, MA, USA). An absorbance
260/280 ratio between 1.8 and 2 was considered of adequate quality
for subsequent use. The DNA concentration was adjusted to 10 ng/µl
and stored at −20°C until analysis.
Pharmacokinetic analysis
ATV plasma concentrations were measured by
high-performance liquid chromatography tandem mass spectrometry
with an Agilent 1100 system (Agilent Technologies, Inc., Santa
Clara, CA, USA) using a method validated by Ipharma S.A. (7,27,28). The Cmax and Tmax parameters
were obtained from the concentration-time data of the plasma.
Pharmacokinetic parameters including AUC0-t,
AUC0-∞, Cl/F, Ke, and T1/2, were calculated
with a non-compartmental method (29)
using WinNonlin® software v5.3 (Pharsight Corp.,
Mountain View, CA, USA) as described in the pilot study (7).
Metabolic phenotype
classification
The metabolizer phenotypes were determined according
to the results of a multivariate analysis of the combined
pharmacokinetic parameters Cmax and AUC0-t
(7). First, Cmax and
AUC0-t were standardized to minimize the effect of scale
differences, and a distance matrix was made from the combined
standardized Cmax and AUC0-t values.
Subsequently, hierarchical cluster analysis (HCA) using the Ward
linkage method (30) was performed on
individual Cmax and AUC0-t values. Finally,
the interindividual Manhattan distances were computed. Minitab 16
software (Minitab Inc., State College, PA, USA) was used for
standardization and HCA.
Pharmacogenetic tests
DNA samples were genotyped for the polymorphisms
AGT-rs699, AGTR1-rs5186 and BDKRB2-rs1799722
using real-time polymerase chain reaction and Taqman®
probes (Applied Biosystems; Thermo Fisher Scientific, Inc.)
according to the manufacturer's protocol. Three quality controls
thresholds were applied: A genotype call rate equal to 1.0, a
Hardy-Weinberg equilibrium (HWE) test with P>0.05, and a minor
allele frequency of >0.01.
Statistical analysis
The HWE was determined by comparing the genotype
frequencies with the expected values using the maximum likelihood
method (31). All statistical
analysis was performed with SPSS v20 software (IBM Corp., Armonk,
NY, USA). To assess the effects of polymorphisms on the ATV
pharmacokinetic parameters, comparisons between two and three
groups were made. The Student's t-test and one-way analysis of
variance were used for parametric distributions, while Mann-Whitney
U and Kruskal-Wallis H tests were used for nonparametric
distributions. To confirm the contribution of genetic factors to
the variability of pharmacokinetic parameters, linear regression
analysis was performed. Possible associations of genotypes or
combinations of genotypes with phenotypes were evaluated using χ2
and Fisher's exact tests. Linear regression and associations were
assessed under three different models (dominant, over-dominant and
recessive) (32). The odds ratio (OR)
was estimated with a 95% confidence interval (95% CI). All P-values
were two-tailed. Corrected P-values (Pc) were obtained using the
Bonferroni correction for exclusion of spurious associations.
P<0.05 was considered to indicate statistical significance.
Results
Metabolic phenotype
classification
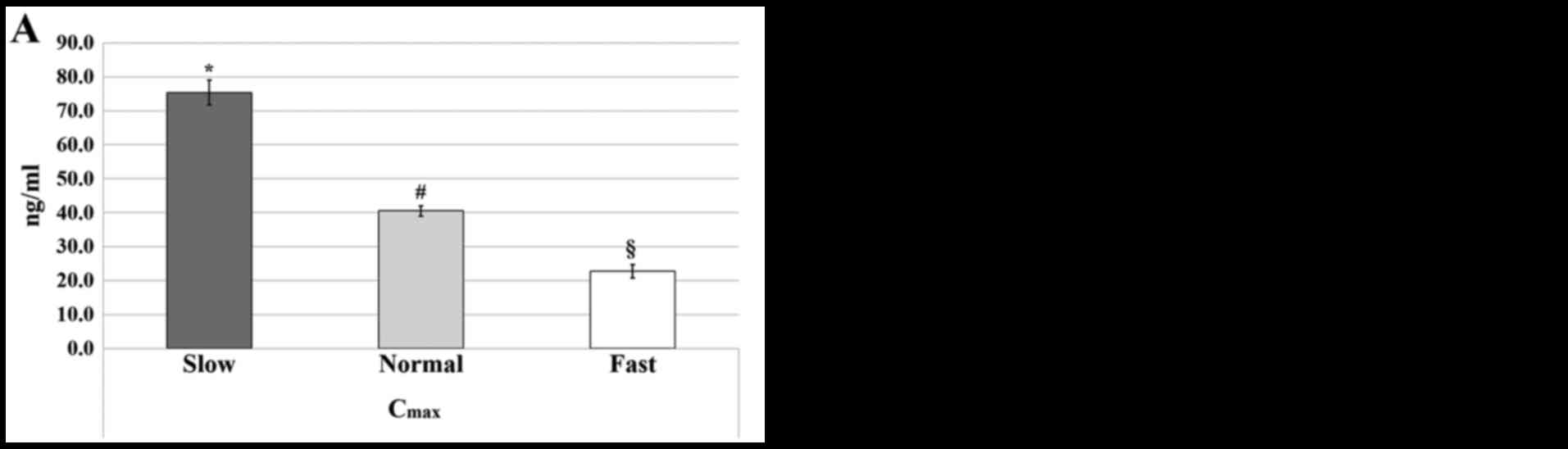
As reported in our previous study (7), the classification of metabolizer
phenotypes, based on the combination of the Cmax and
AUC0-t parameters, identified three ATV metabolizer
phenotypes: Slow metabolizers (30.00%), normal metabolizers
(41.66%) and fast metabolizers (28.33%). The Cmax and
AUC0-t parameters used for the classification were
significantly different between the three phenotypes (7); the parameters were significantly higher
for the slow phenotype compared with the normal and fast
phenotypes, and significantly higher for the normal phenotype
compared with the fast phenotype (P<0.05; Fig. 1). None of the subjects reported any
side effects (7).
Pharmacogenetic tests
Allele frequencies of the genetic polymorphisms were
consistent with HWE (P>0.05). All genetic polymorphisms
satisfied the quality control tests.
Association between genotypes and ATV
pharmacokinetics
There was no significant effect of the
AGT-rs699 polymorphism on ATV pharmacokinetic parameters
(Table I). Conversely,
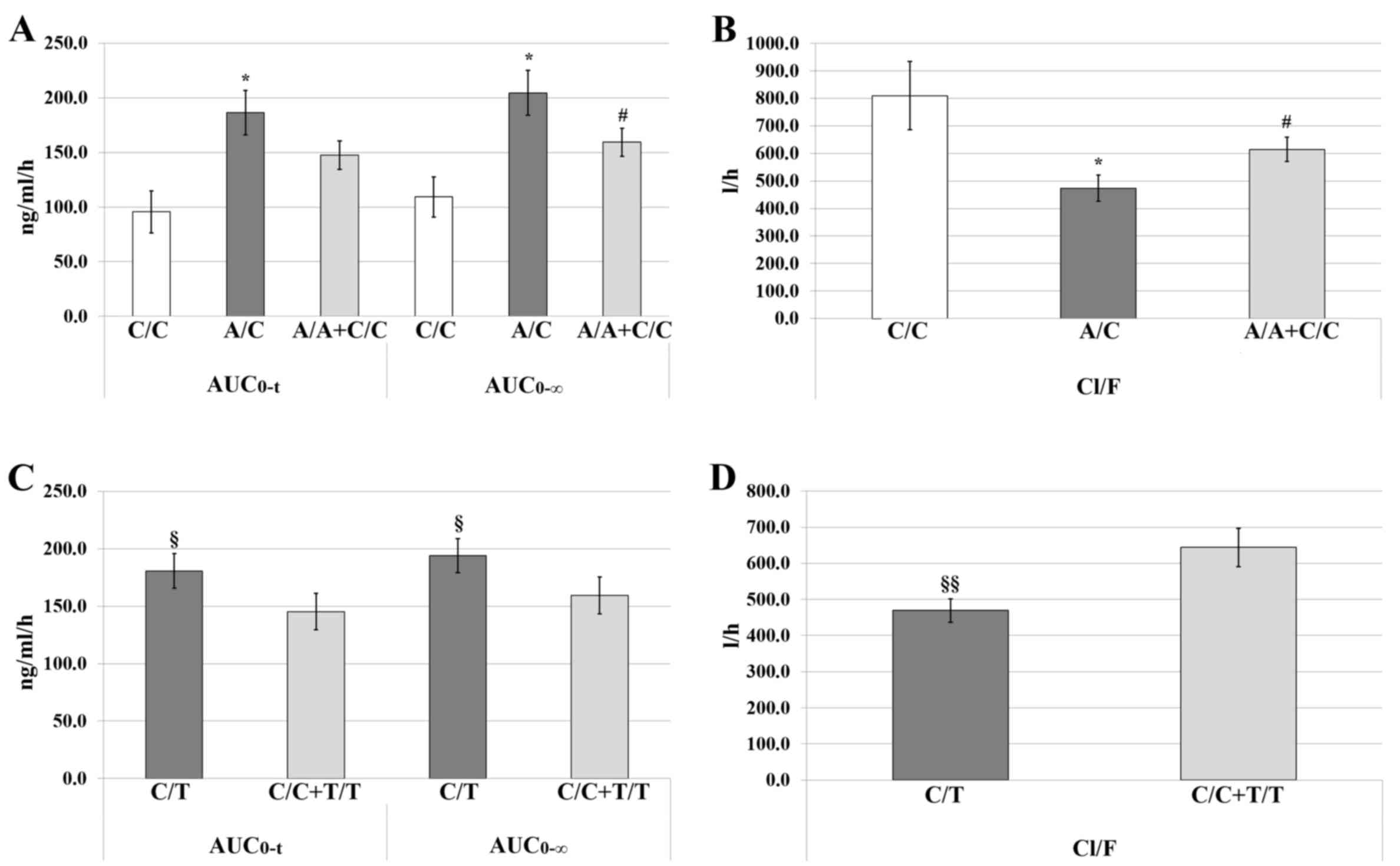
AUC0-t and AUC0-∞ values were significantly
higher in individuals with the heterozygous genotype (A/C) of the
AGTR1-rs5186 polymorphism when compared with the C/C
genotype (P<0.05). In addition, the AUC0-∞ of the A/C
genotype was increased compared with that observed for the
combination of the homozygous wild-type and homozygous variant
alleles (A/A+C/C; P<0.05). In heterozygous carriers, Cl/F values
were significantly lower than those observed for homozygous variant
allele carriers (C/C) and for the combination of homozygous alleles
(A/A+C/C; P<0.05; Table I and
Fig. 2A and B).
 | Table I.Effect of polymorphisms on the
pharmacokinetic parameters of atorvastatin. |
Table I.
Effect of polymorphisms on the
pharmacokinetic parameters of atorvastatin.
|
| Genotypes | N | Cmax
(ng/ml) | AUC0-t
(ng/ml/h) | AUC0-∞
(ng/ml/h) | Cl/F (l/h) | Ke | T1/2
(h) |
|---|
|
AGT-rs699 | A/A | 4 |
45.72±11.03 |
109.72±38.89 |
121.44±43.81 |
729.06±266.90 |
0.05±0.02 |
14.97±9.68 |
|
| A/G | 29 |
43.21±21.06 |
141.98±51.00 |
159.05±56.37 |
588.08±279.10 |
0.07±0.04 |
12.43±7.99 |
|
| G/G | 27 |
51.20±26.65 |
189.40±11.65 |
200.34±110.61 |
516.63±246.52 |
0.08±0.02 |
9.22±3.25 |
|
| A/A+A/G | 33 |
43.51±20.00 |
138.07±50.32 |
154.49±55.82 |
605.17±277.53 |
0.07±0.04 |
12.74±8.09 |
|
AGTR1-rs5186 | A/A | 34 |
44.14±22.86 |
155.21±83.44 |
166.63±81.73 |
585.92±269.36 |
0.08±0.03 |
9.78±5.53 |
|
| A/C | 21 |
54.80±23.47 |
186.44±92.45a |
204.55±94.76a |
473.67±220.44a |
0.06±0.03 |
13.49±8.12 |
|
| C/C | 5 |
33.36±18.79 |
95.57±43.10 |
109.28±40.84 |
810.19±275.81 |
0.07±0.02 |
10.72±3.30 |
|
| A/A+C/C | 39 |
42.76±22.46 |
147.56±81.54 |
159.28±79.71b |
614.68±277.11b |
0.08±0.03 |
9.90±5.27 |
|
BDKRB2-rs1799722 | C/C | 24 |
44.00±27.21 |
151.53±103.77 |
163.00±102.00 |
649.67±316.78 |
0.09±0.02 |
8.78±3.27 |
|
| C/T | 27 |
51.80±20.93 |
180.66±78.48c |
194.17±77.38d |
469.55±168.36e |
0.07±0.04 |
12.64±7.21 |
|
| T/T | 9 |
40.40±17.73 |
128.38±42.26 |
150.31±66.35 |
627.71±287.80 |
0.06±0.02 |
13.05±9.53 |
|
| C/C+T/T | 33 |
43.02±24.76 |
145.22±91.08 |
159.54±92.80 |
643.68±304.85 |
0.08±0.02 |
9.94±5.84 |
For BDKRB2-rs1799722, carriers of the
heterozygous genotype (C/T) were identified to have significantly
higher values of AUC0-t (P=0.021) and AUC0-∞
(P=0.023) and lower values of Cl/F (P=0.007) compared with those
obtained for the combination of homozygous alleles (C/C+T/T;
Table I and Fig. 2C and D).
The linear regression analysis under the
over-dominant genetic model indicated that the AGTR1-rs5186
polymorphism significantly affected the values of T1/2
(adjusted R2=0.053, P=0.043); however, on comparison of
the means by genotype, no significant differences were observed.
Similarly, the BDKRB2-rs1799722 polymorphism significantly
affected the Cl/F values (adjusted R2=0.093, P=0.01;
data not shown).
Association between genotypes and
metabolizer phenotypes
Of the two polymorphisms with an effect on ATV
pharmacokinetics, BDKRB2-rs1799722 was associated with fast
metabolism when considering genetic models; association analysis
using the dominant model identified that the C/C genotype of
BDKRB2-rs1799722 was associated with the fast metabolizer
phenotype (OR, 0.47; 95% CI, 0.26–0.83), whereas the C/T+T/T
combination was associated with the normal and slow phenotypes (OR,
1.98; 95% CI, 1.01–3.88; P=0.014). When using the over-dominant
model, the C/C+T/T combination was associated with the fast
metabolizer phenotype (OR, 0.68; 95% CI, 0.40–0.92) and C/T was
associated with the normal and slow phenotypes (OR, 2.27; 95% CI,
0.92–5.60; P=0.036). However, following Bonferroni's correction,
only the associations under the dominant model remained
statistically significant (Pc=0.03; Table II).
 | Table II.Association between genotypes and
metabolizer phenotypes. |
Table II.
Association between genotypes and
metabolizer phenotypes.
| Gene | Polymorphism | Model | OR (95% CI) | P-value | Pc-value |
|---|
| BDKRB2 | rs1799722 | Dominant (C/C vs.
C/T+T/T) | C/C: Fast
metabolizers | 0.014 | 0.03 |
|
|
|
| 0.47
(0.26–0.83) |
|
|
|
|
|
| C/T+T/T:
Normal/slow metabolizers |
|
|
|
|
|
| 1.98
(1.01–3.88) |
|
|
| BDKRB2 | rs1799722 | Over-dominant
(C/C+T/T vs. C/T) | C/C+T/T: Fast
metabolizers | 0.036 | 0.07 |
|
|
|
| 0.68
(0.40–0.92) |
|
|
|
|
|
| C/T: Normal/slow
metabolizers |
|
|
|
|
|
| 2.27
(0.92–5.60) |
|
|
Discussion
The pharmacokinetic parameters of ATV, namely
Cmax and AUC, may vary by >10-fold (7,33).
Following analysis of pharmacokinetic discrepancies, three major
metabolizer phenotypes of ATV have been identified in Chinese and
Mexican populations (7,33). This variation has been associated with
polymorphisms in genes encoding drug metabolizing enzymes and
transporters (34). However,
differences in allele frequencies and their effect on quantitative
parameters including cholesterol levels, arterial pressure and
pharmacokinetic parameters, and associations of genotypes with drug
metabolism and response have been documented across various
populations (7,33,35,36).
In the current study, the effect on ATV
pharmacokinetics of three polymorphic variants in genes related to
drug metabolism and response were evaluated. AGT-rs699 had
no significant effect on pharmacokinetic parameters. However, to
the best of our knowledge, the study is the first to identify an
effect of AGTR1-rs5186 and BDKRB2-rs1799722 on ATV
pharmacokinetics.
Heterozygous carriers of rs5186 (A/C) exhibited
higher AUC0-t and AUC0-∞ values, while having
lower Cl/F values, than homozygous carriers (C/C), which thus
indicates a diminished clearance activity and longer permanence of
ATV in heterozygous carriers. The effect of the AGTR1
polymorphism on T1/2 was consistent with this
interpretation. This decreased clearance and longer exposure to ATV
may lead to an improved response to drug therapy, or to an adverse
effect. By contrast, carriers of homozygous genotypes (A/A or C/C)
had increased clearance, and thus may have a poorer response to
treatment. However, there was no association between the A/A or C/C
genotypes with the fast metabolizer phenotype. To the best of our
knowledge, this is the first report on the influence of rs5186 on
ATV pharmacokinetics, though the rs5186 polymorphism has previously
been associated with lipid levels (37), and ATV, as a statin, has
lipid-lowering effects (38).
Consistent with the present results, the C/C genotype has been
related to higher levels of triglycerides in a healthy Malayan
population (37). Additionally, in a
case-control study conducted in a Northern Indian population, the
C/C genotype was associated with essential hypertension and higher
gene expression of AGTR1 (39). Regarding the anti-inflammatory effect
of statins, ATV may affect activation of the angiotensin pathway
through AGTR1 by attenuating the activity of angiotensin II
(ANG II), as observed in rats, whereby ATV modulated ANG II-induced
expression of inflammatory and fibrogenic genes in the liver
(40); however there is a lack of
data regarding the association of AGTR1-rs5186 with the
anti-inflammatory response.
Regarding BDKRB2-rs1799722, significant
differences in the AUC0-t, AUC0-∞ and Cl/F
parameters were identified between heterozygous carriers (C/T) and
homozygous carriers (C/C or T/T). The current results suggest that
the BDKRB2-rs1799722 polymorphism affects ATV clearance
activity. This effect was demonstrated by linear regression and
association analyses under over-dominant and dominant models.
Notably, it was indicated that the C allele promotes fast
metabolism, while accumulation of the T allele leads to a shift
towards slower metabolism. However, the pharmacokinetic parameters
of the T/T homozygous carriers did not differ significantly
compared with heterozygous carriers. To the best of our knowledge,
BDKRB2-rs1799722 has not previously been associated with
statin metabolism. However, a meta-analysis identified that the C
allele of rs1799722 increased the risk of hypertension in Asian and
African-American populations (20). A
pharmacogenetic study conducted in a Brazilian population revealed
that carriers of the C allele responded to Enalapril, an
antihypertensive drug that serves as an inhibitor of
angiotensin-converting enzyme (21).
The statins are also established for their antihypertensive effects
in hypercholesterolemic patients (41). Nonetheless, there is a lack of studies
into the effect of BDKRB2-rs1799722 on the metabolism or
response of patients to statins.
Although a number of polymorphisms have been
suggested as candidate responsible for the pharmacokinetic
variability of ATV, the present study is the first to indicate the
involvement of AGTR1-rs5186 and BDKRB2-rs1799722. The
inclusion of these biomarkers in future studies may improve the
prediction of the pharmacokinetic variability of ATV or decrease
the number of variants required for prediction (7,11). While
the current study demonstrated the contribution of genetic
polymorphisms to ATV pharmacokinetics, there were a number of
limitations. Firstly, there was a lack of data, such as cholesterol
levels at one month post-treatment, for complete analysis of
polymorphism effect on response. Secondly, in some cases the number
of subjects per genotype was small, and thus associations may have
been lost following correction. To validate the results, further
studies should be performed in a larger population. In addition,
the influence of other genes may explain the lack of association
with the slow metabolizer phenotype.
In conclusion, a significant effect of
AGTR1-rs5186 and BDKRB2-rs1799722 on ATV
pharmacokinetics was detected. The present findings suggest that
the A/C genotype of AGTR1-rs5186 is associated with slow ATV
metabolism, while the C/C or A/A+C/C genotypes are associated with
fast metabolism. Additionally, the C/T genotype of
BDKRB2-rs1799722 may be associated with the slow metabolizer
phenotype, while the homozygous genotypes may be associated with
the fast metabolizer phenotype. These novel findings increase the
panel of potential genetic biomarkers associated with ATV
metabolism, and should be verified in future pharmacogenetic
studies in larger populations with different genetic
backgrounds.
Acknowledgements
The authors would like to thank the University of
Monterrey, Italy, for funding the current study (grant no.
UIN15009) and Dr Irene Meester from the University of Monterrey for
reviewing and improving the manuscript.
References
|
1
|
Valdez Morales M, Medina Godoy S, Chacón
López MA and Espinosa Alonso LG: Comprehensive approach of diet
importance on health status of the Mexican population. Biotecnia.
18:102016. View Article : Google Scholar
|
|
2
|
Kuri-Morales PA: La transición en salud y
su impacto en la demanda de servicios. Gac Med Mex. 147:451–454.
2011.(In Spanish). PubMed/NCBI
|
|
3
|
National Institute of Statistics and
Geography (INEGI), . Mortality Statistics. INEGI, Mexico City.
2015.http://www.beta.inegi.org.mx/contenidos/proyectos/registros/vitales/mortalidad/doc/presentacion.pdfJune
15–2016(In Spanish).
|
|
4
|
Escobedo-de la Peña J, de Jesús-Pérez R,
Schargrodsky H and Champagne B: Prevalence of dyslipidemias in
Mexico city and Its relation to other cardiovascular risk factors.
Results from the CARMELA study. Gac Med Mex. 150:128–136. 2014.(In
Spanish).
|
|
5
|
Canalizo-Miranda E, Favela-Pérez EA,
Salas-Anaya JA, Gómez-Díaz R, Jara-Espino R, Del Pilar
Torres-Arreola L and Viniegra-Osorio A: Clinical practice
guideline. Diagnosis and treatment of dyslipidemia. Rev Med Inst
Mex Seguro Soc. 51:700–709. 2013.(In Spanish).
|
|
6
|
McFarland AJ, Anoopkumar-Dukie S, Arora
DS, Grant GD, McDermott CM, Perkins AV and Davey AK: Molecular
mechanisms underlying the effects of statins in the central nervous
system. Int J Mol Sci. 15:20607–20637. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
León-Cachón RBR, Ascacio-Martínez JA,
Gamino-Peña ME, Cerda-Flores RM, Meester I, Gallardo-Blanco HL,
Gómez-Silva M, Piñeyro-Garza E and Barrera-Saldaña HA: A
pharmacogenetic pilot study reveals MTHFR, DRD3, and MDR1
polymorphisms as biomarker candidates for slow atorvastatin
metabolizers. BMC Cancer. 16:742016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
León-Cachón RBR, Ascacio-Martínez JAI,
Gómez-Silva M, Piñeyro-Garza E, González-González JG, Pogue G,
Simón-Buela L and Barrera-Saldaña HA: Application of genomic
technologies in clinical pharmacology research. Rev Inves Clin.
67:212–218. 2015.
|
|
9
|
US Food and Drug Administration, . Draft
guidance on atorvastatin calcium and ezetimibe. US Department of
Health and Human Services; Silver Spring, MD: 2014
|
|
10
|
León-Cachón RB1, Ascacio-Martínez JA and
Barrera-Saldaña HA: Individual response to drug therapy: Bases and
study approaches. Rev Invest Clin. 64:364–376. 2012.PubMed/NCBI
|
|
11
|
Cruz-Correa OF, León-Cachón RB,
Barrera-Saldaña HA and Soberón X: Prediction of atorvastatin
plasmatic concentrations in healthy volunteers using integrated
pharmacogenetics sequencing. Pharmacogenomics. 18:121–131. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ma Y, Chen Z, Zou Y and Ge J: Atorvastatin
represses the angiotensin 2-induced oxidative stress and
inflammatory response in dendritic cells via the PI3K/Akt/Nrf 2
pathway. Oxid Med Cell Longev. 2014:1487982014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ruaño G, Thompson PD, Windemuth A, Smith
A, Kocherla M, Holford TR, Seip R and Wu AH: Physiogenomic analysis
links serum creatine kinase activities during statin therapy to
vascular smooth muscle homeostasis. Pharmacogenomics. 6:865–872.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Peters BJ, Klungel OH, de Boer A, Ch
Stricker BH and Maitland-van der Zee AH: Pharmacogenetics of
cardiovascular drug therapy. Clin Cases Miner Bone Metab. 6:55–65.
2009.PubMed/NCBI
|
|
15
|
Frazier L, Turner ST, Schwartz GL, Chapman
AB and Boerwinkle E: Multilocus effects of the
renin-angiotensin-aldosterone system genes on blood pressure
response to a thiazide diuretic. Pharmacogenomics J. 4:17–23. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jiang X, Sheng HH, Lin G, Li J, Lu XZ,
Cheng YL, Huang J, Xiao HS and Zhan YY: Effect of
renin-angiotensin-aldosterone system gene polymorphisms on blood
pressure response to antihypertensive treatment. Chin Med J (Engl).
120:782–786. 2007.PubMed/NCBI
|
|
17
|
Bryant JW and Shariat-Madar Z: Human
plasma kallikrein-kinin system: Physiological and biochemical
parameters. Cardiovasc Hematol Agents Med Chem. 7:234–250. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bentley JP, Asselbergs FW, Coffey CS,
Hebert PR, Moore JH, Hillege HL and van Gilst WH: Cardiovascular
risk associated with interactions among polymorphisms in genes from
the renin-angiotensin, bradykinin, and fibrinolytic systems. PLoS
One. 5:e127572010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pal GK, Adithan C, Umamaheswaran G, Pal P,
Nanda N, Indumathy J and Syamsunder AN: Endothelial nitric oxide
synthase gene polymorphisms are associated with cardiovascular
risks in prehypertensives. J Am Soc Hypertens. 10:865–872. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Luo K, Kang W and Xu G: The risk of
bradykinin B2 receptor-58T/C gene polymorphism on hypertension: A
meta-analysis. Int J Clin Exp Med. 8:19917–19927. 2015.PubMed/NCBI
|
|
21
|
Silva PS, Fontana V, Luizon MR, Lacchini
R, Silva WA Jr, Biagi C and Tanus-Santos JE: eNOS and BDKRB2
genotypes affect the antihypertensive responses to enalapril. Eur J
Clin Pharmacol. 69:167–177. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
World Medical Association, . World Medical
Association Declaration of Helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
World Medical Association, . WMA
Declaration of Tokyo - Guidelines for physicians concerning torture
and other cruel, inhuman or degrading treatment or punishment in
relation to detention and imprisonment. 29th WMA General Assembly.
Tokyo, Japan. 1975;
|
|
24
|
Solorzano-Flores LI: Official Mexican
Standard NOM-177-SSA1-1998, establishing tests and procedures to
demonstrate that a drug is interchangeable. Requirements must be
subject to third party authorized to perform the tests. Secretaria
de Salud, Mexico. 1999.
|
|
25
|
Briggs GG, Freeman RK, Towers CV and
Forinash AB: Drugs in Pregnancy and Lactation. 11th. Williams &
Wilkins; Philadelphia, PA: 2017
|
|
26
|
Sambrook J and Russell DW: Preparation and
analysis of eukaryotic genomic DNAMolecular Cloning: A Laboratory
Manual. 3rd. Cold Spring Harbor Laboratory Press; New York, NY:
2001
|
|
27
|
Ahmed T, Kollipara S, Gautam A, Gigras R,
Kothari M, Saha N, Batra V and Paliwal J: Bioavailability and
interaction potential of atorvastatin and losartan on
co-administration in healthy human subjects. J Bioequiv Availab.
1:18–27. 2009.
|
|
28
|
Stanisz B and Kania L: Validation of HPLC
method for determination of atorvastatin in tablets and for
monitoring stability in solid phase. Acta Pol Pharm. 63:471–476.
2006.PubMed/NCBI
|
|
29
|
Rowland M and Tozer TN: Clinical
Pharmacokinetics and Pharmacodynamics: Concepts and Applications.
4th. Williams & Willkins; Philadelphia, PA: 2017
|
|
30
|
Ward JH Jr: Hierarchical grouping to
optimize an objective function. J Am Stat Assoc. 58:236–244. 1963.
View Article : Google Scholar
|
|
31
|
Reed TE and Schull WJ: A general maximum
likelihood estimation program. Am J Hum Genet. 20:579–580.
1968.PubMed/NCBI
|
|
32
|
Horita N and Kaneko T: Genetic model
selection for a case-control study and a meta-analysis. Meta Gene.
5:1–8. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Huang Q, Aa J, Jia H, Xin X, Tao C, Liu L,
Zou B, Song Q, Shi J, Cao B, et al: A Pharmacometabonomic approach
to predicting metabolic phenotypes and pharmacokinetic parameters
of atorvastatin in healthy volunteers. J Proteome Res.
14:3970–3981. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Niemi M: Transporter pharmacogenetics and
statin toxicity. Clin Pharmacol Ther. 87:130–133. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kadam P, Ashavaid TF, Ponde CK and Rajani
RM: Genetic determinants of lipid-lowering response to atorvastatin
therapy in an Indian population. J Clin Pharm Ther. 41:329–333.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Prado Y, Zambrano T and Salazar LA:
Transporter genes ABCG2 rs2231142 and ABCB1 rs1128503 polymorphisms
and atorvastatin response in Chilean subjects. J Clin Pharm Ther.
Aug 19–2017.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yap RWK, Shidoji Y, Yap WS and Masaki M:
Association and interaction effect of AGTR1 and AGTR2 gene
polymorphisms with dietary pattern on metabolic risk factors of
cardiovascular disease in Malaysian adults. Nutrients. 9:E8532017.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Isley WL, Miles JM, Patterson BW and
Harris WS: The effect of high-dose simvastatin on triglyceride-rich
lipoprotein metabolism in patients with type 2 diabetes mellitus. J
Lipid Res. 47:193–200. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Chandra S, Narang R, Sreenivas V, Bhatia
J, Saluja D and Srivastava K: Association of angiotensin II type 1
receptor (A1166C) gene polymorphism and its increased expression in
essential hypertension: A case-control study. PLoS One.
9:e1015022014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Moreno M, Ramalho LN, Sancho-Bru P,
Ruiz-Ortega M, Ramalho F, Abraldes JG, Colmenero J, Dominguez M,
Egido J, Arroyo V, et al: Atorvastatin attenuates angiotensin
II-induced inflammatory actions in the liver. Am J Physiol
Gastrointest Liver Physiol. 296:G147–G156. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Morgado M, Rolo S, Macedo AF and
Castelo-Branco M: Association of statin therapy with blood pressure
control in hypertensive hypercholesterolemic outpatients in
clinical practice. J Cardiovasc Dis Res. 2:44–49. 2011. View Article : Google Scholar : PubMed/NCBI
|