Introduction
Breast cancer is a major public health problem in
developing countries. The American Cancer Society has estimated
that approximately 1,735,350 new cases of cancer and 609,640
cancer-related fatalities will occur in the United States (US) in
2018, including 266,120 new cases of invasive breast cancer
(1). Furthermore, in the US the
healthcare costs of cancer in 2010 surpassed $124.5 billion (USD),
with this figure estimated to reach $157.8 billion by 2020, of
which the highest costs will be for breast cancer (2). A study by Youlden et al (3) in 2014 revealed that breast cancer was
the most prevalent cancer and fourth leading cause of
cancer-related mortality among women in Asia. In Nepal, according
to the data from seven major cancer service hospitals in 2012,
breast cancer was the second most common cancer among women, after
cancer of the cervix (4,5). The risk of breast cancer increases
exponentially up to the age of menopause, and increases at a slower
rate thereafter (6). Early detection
of breast cancer markedly increases the probability of successful
treatment. Nevertheless, there is a need for culturally
appropriate, targeted intervention to promote preventive strategies
and enhance knowledge and awareness regarding breast cancer. A
similar previous review has been conducted in India by Agarwal and
Ramakant (7), which concluded that
breast cancer was the most prevalent cancer in Indian women living
in urban regions, while awareness of the symptoms, early diagnosis
and screening tests for breast cancer was notably poor. Previous
studies have demonstrated that there are sub-optimal levels of
breast cancer awareness, knowledge of risk factors and screening
among Nepalese women (8,9).
Breast cancer is a substantial social and economic
burden in Nepal. Prevention has been demonstrated to be among the
most effective long-term strategies to lessen the increasing
chronic disease burden (7). However,
due to socioeconomic disparities and insufficient financial
resources, to date, the prevention of breast cancer has not been
well conducted in Nepal (4). As a
developing nation, Nepal is faced with several challenges with
regards to the care of patients with breast cancer with inadequate
funding; the uneven distribution of resources and services;
inadequate numbers, training and distribution of health-care
personnel and equipment; and a lack of adequate care for many
populations based on socioeconomic and geographic factors (4). In the present review, the
epidemiological characteristics, risk factors and current breast
cancer awareness and screening efforts in Nepal are summarized.
Additionally, alternative ways to improve the prevention of breast
cancer in Nepal are discussed.
Burden of breast cancer in Nepal
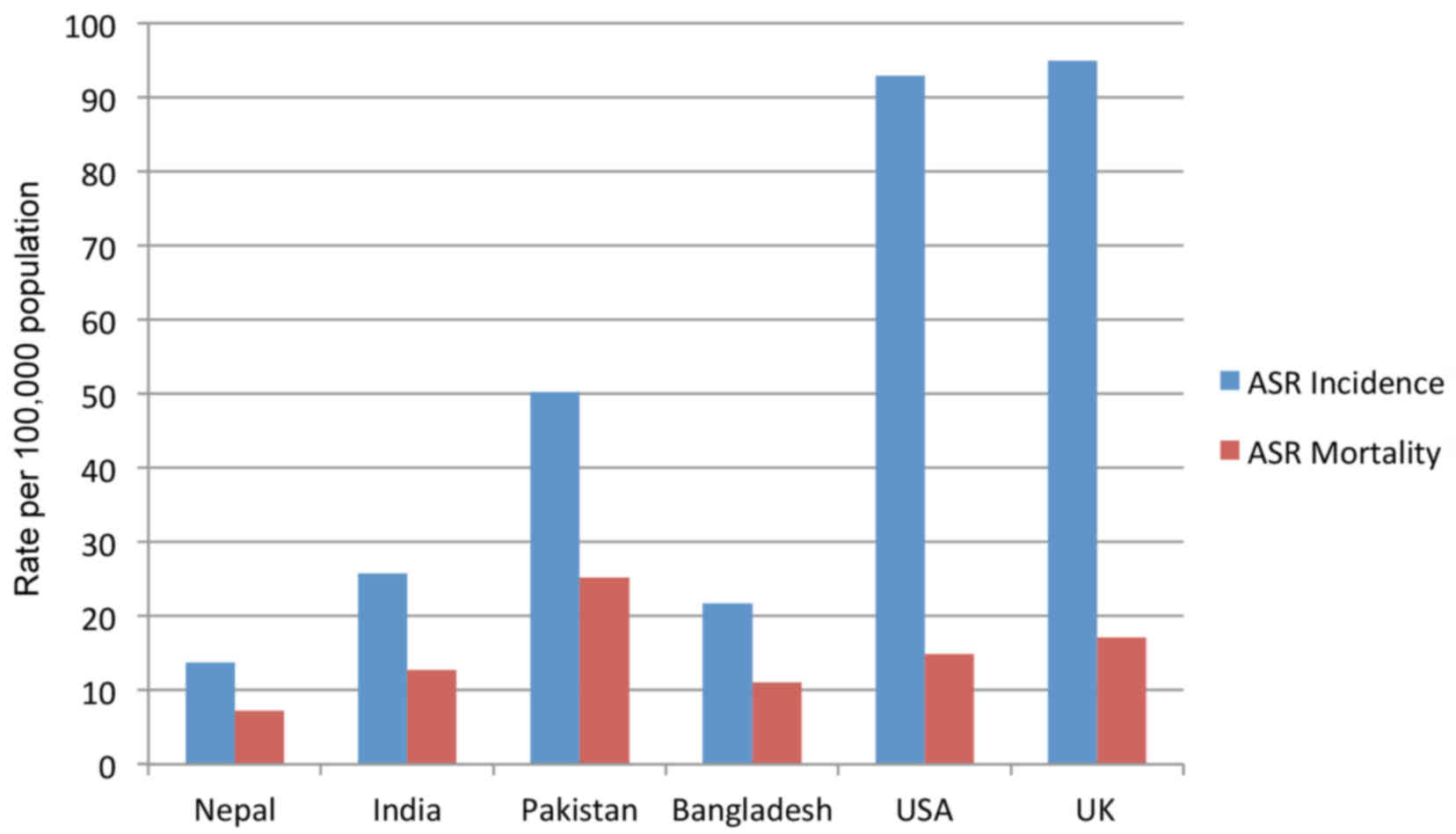
According to GLOBOCAN 2012 (10), an estimated 1,700 new breast cancer
cases were diagnosed in Nepal in 2012, with an age standardized
rate (ASR) of 13.7 new cases per 100,000 omen, while 870 fatalities
in women occurred, with an ASR of 7.2 fatalities per 100,000 women
(Fig. 1). Figure 1 compares these data with those of
other countries (10) including India
(ASR incidence: 25.8, ASR mortality: 12.7), Pakistan (ASR
incidence: 50.3, ASR mortality: 25.2), Bangladesh (ASR incidence:
21.7, ASR mortality: 11.1), the US (ASR incidence: 92.9, ASR
mortality: 14.9) and the United Kingdom (ASR incidence: 95 and ASR
mortality: 17.1). While still noteworthy, the ASRs were markedly
lower in Asian than in Western countries, which may be due to rapid
economic growth and urbanization, and rises in the population's
socioeconomic status in developed countries (10). Population-based cancer registries are
considered the best option for measuring indicators of cancer
(11). Although a population-based
national cancer registry does not exist in Nepal, there is a
multi-institution hospital-based registry. The most common age of
breast cancer patients has been reported to be 40–50 years in
various population-based studies performed in different parts of
Nepal (12,13), among which a marked proportion of
Nepalese breast cancer patients were younger than 50 years of
age.
Risk factors
The risk of breast cancer increases with age. Risk
factors associated with breast cancer (Table I), including early menarche (before
age 12), late menopause (after 55 years of age), nulliparity or
first child birth after the age of 30 years, are similar in Asian
and western populations, except for hormone replacement therapy
(HRT), which is an important risk factor in Caucasians but not in
Asian women (14–17). The adoption of the westernized
lifestyle of delayed childbearing, reduced breastfeeding and other
westernized dietary and lifestyle patterns has a significant impact
on breast cancer risk and prognosis among Asian women (18). Studies have revealed that breast
cancer in premenopausal Nepalese patients was associated with late
menarche (>14 years), early first full-term pregnancy (before 40
weeks of pregnancy) and a longer duration of breastfeeding, when
compared with Japanese subjects (19,20).
Family history is also an important risk factor for breast cancer,
but there is no association between family history of breast cancer
and breast cancer severity or associated mortality (21). A family history of female breast
cancer in first degree relatives is reportedly rare in a Nepalese
context (19). Meanwhile, studies
have identified that high dietary fat, excessive alcohol intake,
hormone replacement therapy, smoking and exposure to radiation may
be associated with an increased risk of breast cancer in Nepalese
women among other nationalities (22,23).
 | Table I.Risk factors of breast cancer in
Nepal. |
Table I.
Risk factors of breast cancer in
Nepal.
| Risk factor | Refs. |
|---|
| Late menarche
(>14 years of age) | (19,20) |
| Nulliparity or late
age at first birth (>35 years of age) | (19,20) |
| Longer duration of
breastfeeding | (19,20) |
| Family history | (19,21) |
| Smoking | (22,23) |
| Excessive alcohol
consumption (>8 units per week) | (22,23) |
| Consumption of fat
(BMI ≥30 kg/m2) | (22,23) |
| Exposure to
radiation | (14,23) |
| Hormone replacement
therapy | (15,22) |
Current screening of breast cancer in
Nepal
Similar to India (7),
no national or regional breast cancer screening program exists in
Nepal. Early detection of breast cancer serves a leading role in
the reduction of breast cancer mortality (7,21). Among
different methods of screening recommended for breast cancer
(Table II), breast self-examination
(BSE) and clinical breast examination are the most effective steps
for detecting breast cancer at an early stage (24). Furthermore, studies have demonstrated
that mammography screening may reduce breast cancer mortality risk
by 20%, and thus screening may be regarded as the optimal method to
prevent breast cancer (24,25). At present, parallel to India,
mammography is not available in a large number of public and
private hospitals in towns as a diagnostic service for women
(7,26). A study in Nepal in 2008 demonstrated
that BSE could be regarded as tool to aid primary prevention
strategies for breast cancer (23).
High-resolution ultrasound may afford improved breast cancer
detection and differentiation; however, ultrasound is generally
only used if a suspicious lesion is detected by mammography
(27). Kelly et al (28) revealed that automated whole breast
ultrasound resulted in significantly improved cancer detection
compared with mammography alone. For BRCA mutation carriers and
their first-degree relatives, the American Cancer Society (ACS)
recommended breast magnetic resonance imaging (MRI) screening as an
adjunct to mammography (29). As a
country with limited resources, in Nepal the number of MR imaging
units is markedly low in proportion to the number of hospitals and
its population. Thus, for early detection of breast cancer in
Nepal, awareness and breast self-examination should be promoted
through newspapers, electronic media, as well as through health
personnel in various settings (7).
 | Table II.Screening methods for breast cancer
in Nepal. |
Table II.
Screening methods for breast cancer
in Nepal.
| Method | Refs. |
|---|
| Breast
self-assessment | (23,24) |
| Mammography | (23–25) |
| Ultrasound | (23–28) |
| Magnetic resonance
imaging | (23,29) |
Treatment modalities of breast cancer in
Nepal
National breast cancer management protocols in Nepal
are at an early stage. To date, the treatment of breast cancers in
Nepal has been decided by factors including financial situation,
accessibility to the appropriate institution and social condition
of the patient (4). There are number
of clinical courses for treating breast cancer (Table III), which depend on its type and
stage. Modified radical mastectomy, simple mastectomy or toilet
mastectomy are frequently practiced surgical techniques for the
management of breast cancer in Nepal (30). Of preference may be breast conserving
surgery (BCS) followed by moderate-dose radiation therapy to
eradicate any microscopic residual disease, which provides the
survival equivalent of mastectomy, reduced cosmetic impact, less
anxiety and depression and improved body image (31). Studies have demonstrated that prior to
2009, trends of BCS in Nepal ranged from 6 to 15%, while the most
common operation performed was modified radical mastectomy
(4,19). Alike Indian populations, few Nepalese
patients are offered post-mastectomy reconstruction, and only a
small proportion of those offered accept to have it performed,
probably due to the reconstructive procedure being seen as an
unnecessary financial burden (7,30). The
presence of axillary lymph node involvement is among the most
important prognostic factors in breast cancer patients (32). Surgical staging of breast cancer by
axillary lymph node dissection remains to be frequently practiced
by many hospitals in Nepal (19);
however, axillary lymph node dissection is increasingly being
replaced by the sentinel node procedure, and sentinel node biopsy
is now regarded as the standard procedure for axillary staging of
breast cancer (33).
 | Table III.Treatment options for breast cancer
in Nepal. |
Table III.
Treatment options for breast cancer
in Nepal.
| Modality | Refs. |
|---|
| Surgery | (31) |
| Total
radical mastectomy |
|
| Simple
mastectomy/toilet mastectomy |
|
|
BCS |
|
| Radiotherapy | (34–36) |
| To the
breast following BCS |
|
| To the
chest wall following radical mastectomy |
|
| Systemic
therapy | (36–39) |
|
Tamoxifen |
|
|
Anthracycline combination |
|
| Palliative
treatment: | (45–48) |
| Opioid
analgesics |
|
| Non
Steroidal Anti Inflammatory Agents |
|
|
Glucocorticoids |
|
|
Systemic administration of
radioisotopes |
|
Radiotherapy reduces local recurrence rates and
increases breast cancer-specific survival in patients with
early-stage breast cancer. Previous data indicates that the
survival of breast cancer patients is improved by post-mastectomy
radiotherapy (34). Radiotherapy is
typically administered to the breast following conservation surgery
and may be administered to the chest wall following mastectomy to
complete local treatment (35). A
study by Sapkota et al (36)
in 2016 identified that radiotherapy was among the most commonly
used modalities for the treatment of breast cancer in Nepal
Systemic treatment of breast cancer includes the use
of cytotoxic, hormonal and immunotherapeutic agents (37). Although metastatic breast cancer is
unlikely to be cured, with the introduction of newer systemic
therapies, notable improvements in survival have been observed in
patients with breast cancer (37).
The main aim of systemic therapies is prolongation of survival,
alleviation of symptoms and improvement of quality of life.
Tamoxifen has been used for more than 30 years to treat hormone
receptor-positive breast cancer. A previous meta-analysis revealed
that adjuvant therapy with tamoxifen resulted in a significant
decrease in breast cancer mortality rate, with an absolute
reduction in mortality of 9.2% at 15 years (38). Tamoxifen is the commonly used hormonal
medicine for the management of breast cancer irrespective of
menopausal status in Nepal (36,39).
However, tamoxifen is associated with serious adverse events (SAEs)
including endometrial cancer and thromboembolic events due to its
estrogen-agonistic activity in selected tissues (40). The patient's health status is vital
when choosing the most appropriate chemotherapy regimen for breast
cancer. An anthracycline-based chemotherapy regimen is also
commonly used in Nepal (41). Ideal
candidates for an anthracycline-containing regimen include women
with chemotherapy naive, stage IV breast cancer and those who have
not previously received an anthracycline (42). Anthracycline should be avoided in
patients was cardiac history, as it may damage the myocardium
through free reactive oxygen radicals and cause direct DNA damage;
such patients treated with anthracycline typically develop cardiac
dysfunction as a result of the treatment (43,44). For
combination chemotherapy, patient preferences aid to individualize
the treatment plan as certain patients may not accept the
additional risks of toxicity associated with combination
chemotherapy.
The primary goal of palliative care for breast
cancer is to prevent and ease suffering and improve the quality of
life of women with metastatic breast disease. Bone metastases are a
common cause of chronic pain, with pain resulting directly from
expanding lesions, pathological fracture or damage to adjacent
structures (45). Opioid analgesics
are widely used to treat pain in patients with breast cancer due to
their safety, multiple routes of administration, ease of titration,
reliability, and effectiveness for all types of pain (46). Glucocorticoids should be considered
for the inflammation or pain related to nerve compression. The
National Comprehensive Cancer Network recommend nonsteroidal
anti-inflammatory drugs (NSAIDs) and acetaminophen in combination
with opioids for bone pain not associated with spinal cord
compression or fracture (47).
Bisphosphonates, glucocorticoids or systemic administration of
radioisotopes should be considered for diffuse bone pain resulting
from metastases (46,47). Such palliative care for breast cancer
in Nepal is still in its infancy (48,49).
Breast cancer awareness and future
directions
Studies have repeatedly demonstrated that
irrespective of their socio-economic and educational backgrounds,
Nepalese women had poor knowledge of the risk factors of breast
cancer (8,9,50).
Although age, education, household income and family history of
breast cancer are reported to be significantly associated with
awareness level, a study on breast cancer literacy among higher
secondary students demonstrated that students had poor knowledge on
breast cancer risk factors, symptoms and curability (50). Furthermore, most of the students
lacked awareness of age, early menarche, delayed menopause and use
of the oral contraceptive pill as being the risk factors for breast
cancer. Sathian et al (8)
identified that among female residents of Pokhara in Nepal, the
level of awareness and understanding of breast cancer, including
knowledge of warning signs and BSE, was sub-optimal. Another
cross-sectional study conducted at KIST medical college in
Kathmandu revealed that 70% of the participants had never heard of
breast cancer (9). This study
demonstrated that awareness and understanding of breast cancer
among Nepalese women was notably poor. Nepalese women need to be
aware of modifiable and non-modifiable risk factors of breast
cancer to adopt appropriate practices for prevention. Cancer
literacy provided by healthcare settings should be increased to
ensure this knowledge becomes more widespread amongst the general
public. The government should also formulate formal policies for
effective nation- and district-wide cancer literacy programmes, as
well as engagements with community-level, national and
international organizations and the healthcare system.
Additionally, breast health education sessions, guidance by nurses
on BSE, regular follow-up by nurses and other healthcare training
institutions should carried out throughout the country. An
awareness campaign could be conducted through advertisements on
breast cancer and screening via radio, internet, television and
poster platforms to promote an attitude change regarding breast
cancer in women. There is also a need to strengthen the
cancer-related curriculum in medical schools, with focus on breast
cancer awareness and screening methods. Furthermore, future
research should continue to focus on the genetic makeup of breast
cancer, to further improve understanding on the early onset of
breast cancer in Nepal and other regions.
Conclusion
In conclusion, the overall perspectives for breast
cancer are notably variable among women in Nepal. Breast cancer has
emerged as the second more prevalent malignancy in women in Nepal.
Factors responsible for the general delayed diagnosis are lack of
knowledge, limited breast cancer screening programs, limited health
care facilities and sociocultural barriers. The government should
foster novel policies to establish effective nationwide cancer
literacy programmes, as well as engagements with community-level,
national and international organizations and the healthcare
system.
Acknowledgements
The authors are thankful to Professor Yang Lü from
the Department of Geriatrics and Professor Shu Liang Guo from the
Department of Respiratory Medicine of Chongqing Medical University
for their help during the preparation of this article.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
MG and MG completed the online database search for
relevant information and designed the concept. MG, MG, RJT, BU and
BP wrote sections of the manuscript. RJT, BU and BP were involved
in revision of the manuscript at all stages. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
American Cancer Society, . Cancer Facts
& Figures 2018. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-andstatistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdfJanuary
25–2018
|
|
2
|
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ
and Brown ML: Projections of the cost of cancer care in the United
States: 2010–2020. J Natl Cancer Inst. 103:117–128. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Youlden DR, Cramb SM, Yip CH and Baade PD:
Incidence and mortality of female breast cancer in the Asia-Pacific
region. Cancer Biol Med. 11:101–115. 2014.PubMed/NCBI
|
|
4
|
Singh YP and Sayami P: Management of
breast cancer in Nepal. JNMA J Nepal Med Assoc. 48:252–257.
2009.PubMed/NCBI
|
|
5
|
Pun CB, Pradhananga KK, Siwakoti B, Subedi
K and Moore MA: Malignant neoplasm burden in Nepal-Data from the
seven major cancer service hospitals for 2012. Asian Pac J Cancer
Prev. 16:8659–8663. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Benz CC: Impact of aging on the biology of
breast cancer. Crit Rev Oncol Hematol. 66:65–74. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Agarwal G and Ramakant P: Breast Cancer
Care in India: The Current Scenario and the Challenges for the
Future. Breast Care (Basel). 3:21–27. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sathian B, Nagaraja SB, Banerjee I,
Sreedharan J, De A, Roy B, Rajesh E, Senthilkumaran S, Hussain SA
and Menezes RG: Awareness of breast cancer warning signs and
screening methods among female residents of Pokhara valley, Nepal.
Asian Pac J Cancer Prev. 15:4723–4726. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shrestha K: Breast cancer knowledge and
screening practice among women visited to KIST medical college.
Nepal Med Coll J. 14:308–311. 2012.PubMed/NCBI
|
|
10
|
GLOBOCAN, . 2012, Estimated Cancer
Incidence, Mortality and Prevalence Worldwide in 2012. http://globocan.iarc.fr/Pages/fact_sheets_population.aspxJanuary
25–2018
|
|
11
|
Forsea AM: Cancer registries in
Europe-going forward is the only option. Ecancermedicalscience.
10:6412016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pradhananga KK, Baral M and Shrestha BM:
Multi-institution hospital-based cancer incidence data for Nepal:
An initial report. Asian Pac J Cancer Prev. 10:259–262.
2009.PubMed/NCBI
|
|
13
|
Binu V, Chandrashekhar T, Subba S, Jacob
S, Kakria A, Gangadharan P and Menezes RG: Cancer pattern in
Western Nepal: A hospital based retrospective study. Asian Pac J
Cancer Prev. 8:183–186. 2007.PubMed/NCBI
|
|
14
|
Moore MA, Ariyaratne Y, Badar F, Bhurgri
Y, Datta K, Mathew A, Gangadharan P, Nandakumar A, Pradhananga KK,
Talukder MH, et al: Cancer epidemiology in South Asia - past,
present and future. Asian Pac J Cancer Prev. 11 Suppl 2:49–66.
2010.PubMed/NCBI
|
|
15
|
Anothaisintawee T, Wiratkapun C,
Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J,
Hirunpat S, Woodtichartpreecha P, Boonlikit S, Teerawattananon Y,
et al: Risk factors of breast cancer: A systematic review and
meta-analysis. Asia Pac J Public Health. 25:368–387. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aich RK, Mondal NK, Chhatui B, Sepai HM,
Aich R, Acharyya A, Manir K and Bhattacharaya J: Relevance of risk
factors of breast cancer in women: An Eastern Indian scenario. J
Cancer Res Ther. 12:302–308. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Collaborative Group on Hormonal Factors in
Breast Cancer, . Menarche, menopause, and breast cancer risk:
Individual participant meta-analysis, including 118 964 women with
breast cancer from 117 epidemiological studies. Lancet Oncol.
13:1141–1151. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Porter P: “Westernizing” women's risks?
Breast cancer in lower-income countries. N Engl J Med. 358:213–216.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bhattacharya S and Adhikary S: Evaluation
of risk factors, diagnosis and treatment in carcinoma breast-a
retrospective study. Kathmandu Univ Med J (KUMJ). 4:54–60.
2006.(KUMJ). PubMed/NCBI
|
|
20
|
Singh Y, Sayami P, Sayami G, Nakagawa H,
Koreeda T, Hatano T and Tsubura A: Nepalese breast cancer in
relation to reproductive factors: Comparison between Nepalese and
Japanese cases. Anticancer Res. 22(1A): 1–323. 2002.PubMed/NCBI
|
|
21
|
Melvin JC, Wulaningsih W, Hana Z,
Purushotham AD, Pinder SE, Fentiman I, Gillett C, Mera A, Holmberg
L and Van Hemelrijck M: Family history of breast cancer and its
association with disease severity and mortality. Cancer Med.
5:942–949. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gram IT, Park SY, Kolonel LN, Maskarinec
G, Wilkens LR, Henderson BE and Le Marchand L: Smoking and Risk of
Breast Cancer in a Racially/Ethnically Diverse Population of Mainly
Women Who Do Not Drink Alcohol: The MEC Study. Am J Epidemiol.
182:917–925. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tara S, Agrawal CS and Agrawal A:
Validating breast self examination as screening modalities for
breast cancer in eastern region of Nepal: A population based study.
Kathmandu Univ Med J (KUMJ). 6:89–93. 2008.PubMed/NCBI
|
|
24
|
Glasziou P and Houssami N: The evidence
base for breast cancer screening. Prev Med. 53:100–102. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Marmot MG, Altman DG, Cameron DA, Dewar
JA, Thompson SG and Wilcox M: The benefits and harms of breast
cancer screening: An independent review. Br J Cancer.
108:2205–2240. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sidhartha TB, Thapa B, Singh Y, Sayami P
and Khanal U: Mammographic diagnosis of breast carcinoma: An
institutional experience. JNMA J Nepal Med Assoc. 47:62–65.
2008.PubMed/NCBI
|
|
27
|
Madjar H: Role of Breast Ultrasound for
the Detection and Differentiation of Breast Lesions. Breast Care
(Basel). 5:109–114. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kelly KM, Dean J, Comulada WS and Lee S-J:
Breast cancer detection using automated whole breast ultrasound and
mammography in radiographically dense breasts. Eur Radiol.
20:734–742. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Saslow D, Boetes C, Burke W, Harms S,
Leach MO, Lehman CD, Morris E, Pisano E, Schnall M, Sener S, Smith
RA, et al: American Cancer Society guidelines for breast screening
with MRI as an adjunct to mammography. CA Cancer J Clin. 5:75–89.
2007. View Article : Google Scholar
|
|
30
|
Pradhan GB, Shrestha R, Shrestha S, Khadka
P, Bhattachan CL, Lehman CD, et al: Outcome analysis of breast
cancer patients treated at Nepal Medical College. Nepal Med Coll J.
14:93–95. 2012.PubMed/NCBI
|
|
31
|
Young OE, Valassiadou K and Dixon M: A
review of current practices in breast conservation surgery in the
UK. Ann R Coll Surg Engl. 89:118–123. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fujii T, Yajima R, Yamaguchi S, Yanagita
Y, Fujisawa T, Hirakata T, Tsutsumi S, Asao T, Iijima M and Kuwano
H: Extracapsular invasion of sentinel lymph nodes is not associated
with disease recurrence in breast cancer. Int Surg. 99:305–308.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kuenen-Boumeester V, Menke-Pluymers M, de
Kanter AY, Obdeijn IM, Urich D and Van Der Kwast TH:
Ultrasound-guided fine needle aspiration cytology of axillary lymph
nodes in breast cancer patients. A preoperative staging procedure.
Eur J Cancer. 39:170–174. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Headon H, Kasem A, Almukbel R and Mokbel
K: Improvement of survival with postmastectomy radiotherapy in
patients with 1–3 positive axillary lymph nodes: A systematic
review and meta-analysis of the current literature. Mol Clin Oncol.
5:429–436. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yang TJ and Ho AY: Radiation therapy in
the management of breast cancer. Surg Clin North Am. 93:455–471.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sapkota A, Shrestha S, Sedhain A, Koirala
S and Kafle P: Problems of Breast Cancer Survivors Living in an
Urban Area of Nepal. Asia Pac J Oncol Nurs. 3:289–296. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gonzalez-Angulo AM, Morales-Vasquez F and
Hortobagyi GN: Overview of resistance to systemic therapy in
patients with breast cancer. Adv Exp Med Biol. 608:1–22. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Early Breast Cancer Trialists'
Collaborative Group (EBCTCG), . Effects of chemotherapy and
hormonal therapy for early breast cancer on recurrence and 15-year
survival: An overview of the randomised trials. Lancet.
365:1687–1717. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Perez EA: Safety profiles of tamoxifen and
the aromatase inhibitors in adjuvant therapy of hormone-responsive
early breast cancer. Ann Oncol. 18 Suppl 8:viii26–35. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Karn A, Jha AK, Shrestha S, Acharya B,
Poudel S and Bhandari RB: Tamoxifen for breast cancer. JNMA J Nepal
Med Assoc. 49:62–67. 2010.PubMed/NCBI
|
|
41
|
Acharya SC, Jha AK and Manandhar T:
Clinical profile of patients presenting with breast cancer in
Nepal. Kathmandu Univ Med J (KUMJ). 10:3–7. 2012.(KUMJ). PubMed/NCBI
|
|
42
|
Sparano JA, Wang M, Martino S, Jones V,
Perez EA, Saphner T, et al: Weekly paclitaxel in the adjuvant
treatment of breast cancer. N Engl J Med. 358:1663–1671. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Romond EH, Perez EA, Bryant J, Suman VJ,
Geyer CE Jr, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman
PA, et al: Trastuzumab plus adjuvant chemotherapy for operable
HER2-positive breast cancer. N Engl J Med. 353:1673–1684. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
FDA, . PLp: doxorubicin HCl intravenous
injection, doxorubicin HCl intravenous injection. New York:
2013
|
|
45
|
Irvin W Jr, Muss HB and Mayer DK: Symptom
management in metastatic breast cancer. Oncologist. 16:1203–1214.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lussier D, Huskey AG and Portenoy RK:
Adjuvant analgesics in cancer pain management. Oncologist.
9:571–591. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
National Comprehensive Cancer Network
(NCCN) Adult Cancer Pain. December 30–2016https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf
|
|
48
|
Braun CM and Itano JK: Cancer care in
Nepal: variables that affect diagnosis, treatment, and prognosis: a
case study. Cancer Nurs. 24:137–142. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Piya MK and Acharya SC: Oncology in Nepal.
South Asian J Cancer. 1:5–8. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bhandari PM, Thapa K, Dhakal S,
Bhochhibhoya S, Deuja R, Acharya P and Mishra SR: Breast cancer
literacy among higher secondary students: Results from a
cross-sectional study in Western Nepal. BMC Cancer. 16:1192016.
View Article : Google Scholar : PubMed/NCBI
|