Introduction
The proximal femur is one of the most common
locations for primary benign bone tumor formation. The majority of
benign tumors, including osteochondromas and fibrous dysplasia,
remain asymptotic and do not require surgical intervention.
However, there are a number of reasons why surgery may be
performed, including pain, inhibited growth, decreased range of
motion, cosmesis, peripheral nerve compression, vessel compression
and to reduce the risk of a malignant transformation, with pain
being the most common (1,2). The recommended surgical intervention in
these instances is the resection of the tumor (3). Numerous studies have focused on
exposing the hip joint capsule or the femur neck, as tumors located
in these areas more commonly lead to clinical symptoms and severe
complications (4,5). By contrast, tumors located in the
lesser trochanter, particularly those outside of the hip joint
capsule, may manifest with clinical symptoms gradually with a long
asymptomatic period, and are seldom encountered in routine clinical
practice. The conventional surgical intervention in these cases is
to approach the lesser trochanter indirectly via the hip joint,
which has various advantages and disadvantages. The conventional
lateral approach is safe, but requires extreme rotation of the limb
in order to expose enough of the region to perform surgery. By
contrast, the medial approach, which provides the shortest approach
to the hip, presents a challenge as it involve navigating
complicated anatomical structure, including the highly variable
obturator nerve, in order to expose the lesser trochanter (6).
Following detailed anatomical dissections, a novel
and direct approach for the treatment of tumors in the lesser
trochanter was developed. This technique involves passing through
the femoral triangle and across the gap between the femoral artery
and femoral nerve. The aim of the present study was to demonstrate
the use of this novel approach, which may be specifically suited to
tumors projecting toward the lateral and anterior of the lesser
trochanter. In addition, follow-up examination was performed to
evaluate the outcome of the surgery in the patients.
Materials and methods
Clinical research
A total of six patients with tumors located in the
lesser trochanter (Fig. 1) were
treated at the First Affiliated Hospital of Xinjiang Medical
University (Ürümqi, China) between March 2007 and March 2013. There
were two male and four female patients, with a median age of 24
years (age range, 13–85 years). Prior to surgery, all the patients
experienced mild to moderate pain, however, their ranges of motion
around the hip joint were not affected. In four cases, the patient
had experienced symptoms for over two years. A biopsy was performed
on the patients (5/6) prior to open surgery. There were two cases
of osteochondroma and one case each of osteoid osteoma,
non-osteogenic fibroma, osteoma and liposarcoma. The patients with
an osteoma and liposarcoma had recurring tumors, and had previously
received treatment in a different hospital. This study was
conducted in accordance with the Declaration of Helsinki, and with
approval from the Ethics Committee of Xinjiang Medical University.
Written informed consent was obtained from all the participants
prior to surgery.
A visual analog scale was used to evaluate the
degree of pain experienced by the patients prior to surgery and at
four weeks following surgery. All six patients underwent follow-up
observation, which varied between 6 and 34 months after surgery;
the median follow-up time was 25 months. Images were collected at
1, 3, 6, 12 and 24 months after surgery in order to evaluate local
recurrence, femur head necrosis and the occurrence of degeneration
disease. Radiographic images were obtained using a DirectView DR
3000 (Kodak, Rochester, NY, USA). All patients were subjected to
hip magnetic resonance imaging (MRI) using a MAGNETOM Avanto 1.5T
MRI scanner (Siemens AG, Munich, Germany). MRI examination was
conducted at approximately the time of the patients
hospitalization. A conventional MRI sequence protocol was applied
in all of the participants and fat saturation was applied in the
patient with liposarcoma. Scanning parameters were as follows:
T1-weighted images had a repetition time of 600 msec and an echo
time of 10 msec; T2-weighted image repetition time was 4,000 msec
and the echo time was 110 msec. These materials were analyzed by
two bone tumor specialists and one radiologist.
Cadaveric dissections
A total of 20 adult lower limb specimens without
organic disease, including 5 unilateral and 4 bilateral male
specimens, and 3 unilateral and 2 bilateral female specimens, were
provided by the Department of Human Anatomy of Xinjiang Medical
University. The virtual area of our approach was the formal
triangle, where the formal artery and vein are located. The formal
artery and vein are wrapped and limited by the surrounding tunica
vaginalis, thus we focused on the gap between the lateral and
medial margins of the femoral nerve. This gap is located by the
innermost branch among the branches of femoral nerve. In order to
determine the space available for the surgical procedure, the
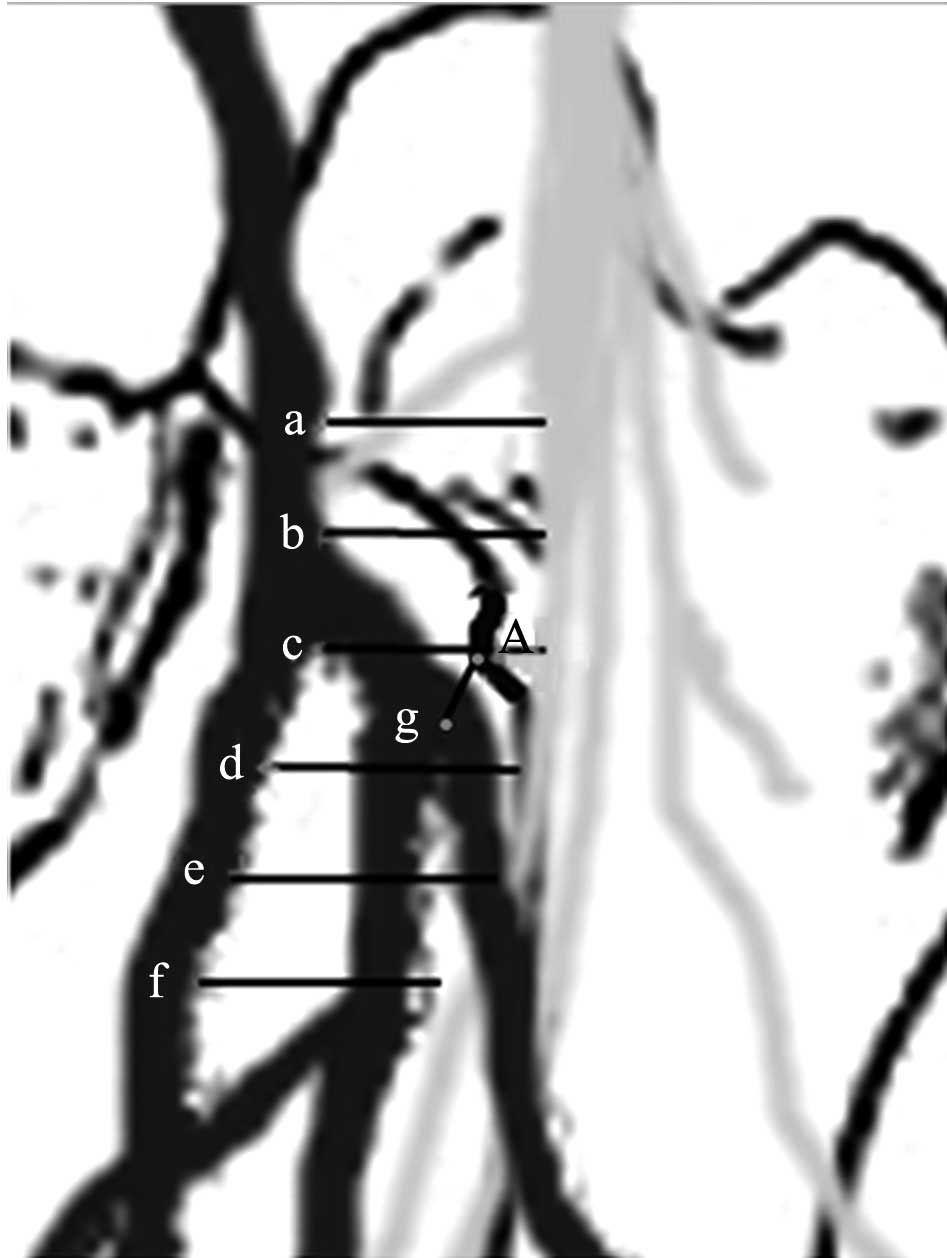
distance of the gap described was measured. The proximal (4, 2 and
0 cm) and distal (2, 4 and 6 cm) distances were measured from the
highest point of the lesser trochanter. In addition, the distance
between the highest point of the lesser trochanter to the start of
the lateral circumflex femoral artery was measured (Fig. 2). Measurements were calculated with
vernier calipers (accuracy of 0.02 mm) and were recorded twice.
Surgical technique
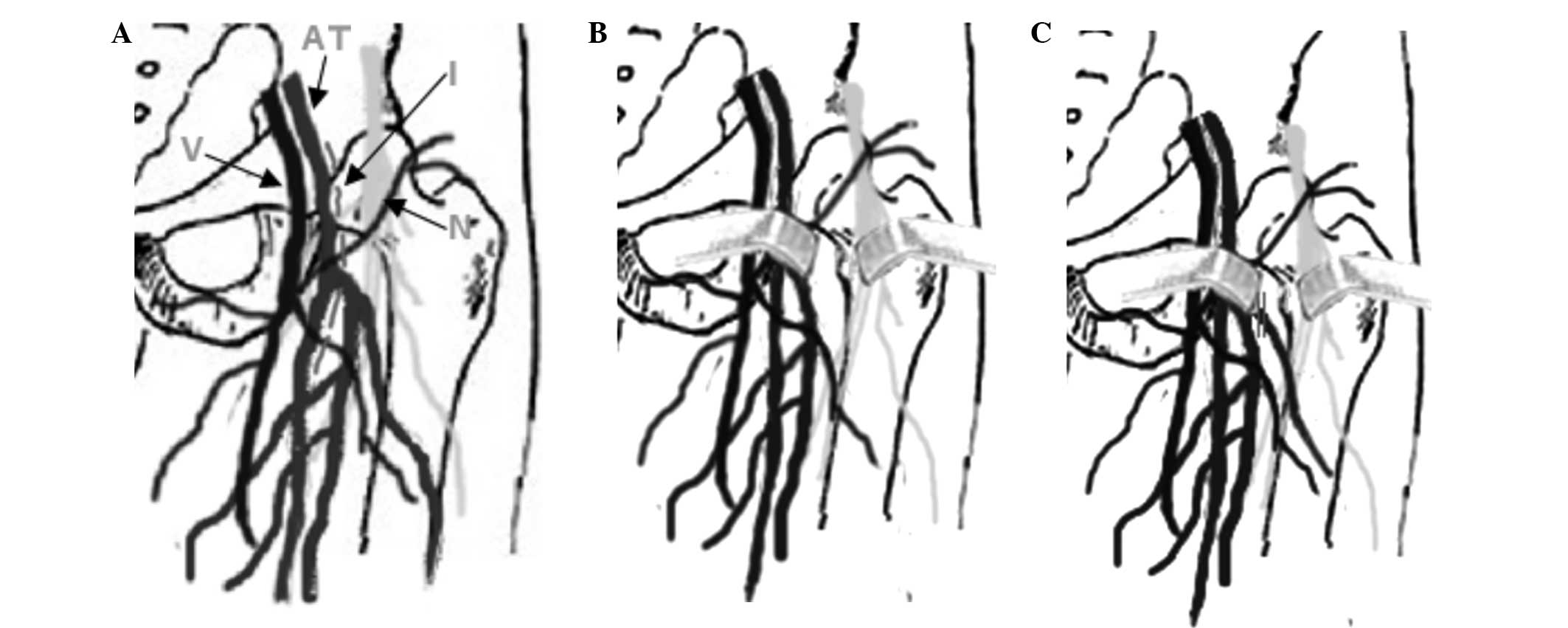
Preoperative assessment included identifying the
position and extent of the tumors using imaging techniques. The
first stage of the surgical procedure was to place the patient in
the supine position, with the hip joint of the affected side facing
outward in order to limit rotation. The pulse of the arteria
femoralis was clearly identifiable in the femoral triangle region,
near the tumor site. The incision was centered over the tumor, by
the outside of the arteria femoralis, and the incision length could
be adjusted (Fig. 3A). The
superficial fascia incision was performed in the same manner as the
standard surgical procedure. The deep fascia incision was made with
caution, as a number of vital blood vessels and nerves associated
with the femur ran through the area. The incision separated the
tissue, with the blood vessels, nerves and surrounding adipose
tissue separated to either side of the incision. Adipose tissue
between the vessels and nerves was appropriately separated.
Vessels, including arteries and veins, were trapped and protected
away from the incision area towards the medial, while nerves were
pulled laterally (Fig. 3B). Further
separation was performed through the adipose tissue. Small branches
of the blood vessels and the femoral nerves were removed if they
prevented further separation. In addition, the lateral femoral
circumflex artery and its branches may prevent further exposure of
the lesser trochanter and should be removed if this is the case
(Fig. 3C). Intramuscular separation
was performed between the iliopsoas and pectineal muscles.
Subsequently, the lesser trochanter and tumor were clearly exposed
through this channel, and were further exposed by outward rotation
of the hip joint. If required, the end of the iliopsoas and
pectineal muscles may be removed.
Condition of the patients following
surgery
Patients who had received reconstruction of the
iliopsoas and pectineal muscle ends had their hip kept in flexor
and adductor positions for four to six weeks after surgery.
However, patients who did not undergo reconstruction of the muscle
ends were able to walk three or four days after surgery.
Statistical analysis
Cadaver measurement data are presented as the mean ±
standard deviation. Statistical analysis was performed using SPSS
software, version 19.0 (IBM SPSS, Armonk, NY, USA).
Results
Surgical outcomes
In the six patients that underwent the novel
surgical procedure, the incision lengths ranged between 8 and 12
cm, and the total operative time varied between 60 and 100 min.
Continuous epidural anesthesia was used with four patients, while
two patients received general anesthesia. The esthetic outcomes
were judged to be acceptable, and blood loss ranged between 30 and
200 ml (Table I). The lateral
femoral circumflex artery was removed in five patients. In
addition, the ends of the iliopsoas and pectineal muscles were
resected in one patient and their hip was kept in the flexor and
adductor position for five weeks after surgery. The five patients
who did not undergo reconstruction of the muscle ends were able to
walk three or four days after surgery.
 | Table I.Patient data. |
Table I.
Patient data.
| Patient | Age (years) | Gender | Anesthesia | Incision size
(cm) | Time (min) | Blood loss (ml) | Diagnosis |
|---|
| 1 | 21 | Male | CEA | 10 | 75 | 50 | Osteoid osteoma |
| 2 | 40 | Female | CEA | 11 | 60 | 30 | Osteochondroama |
| 3 | 13 | Female | GA | 8 | 100 | 200 | Osteochondroma |
| 4 | 23 | Male | CEA | 12 | 80 | 100 | Osteoid osteoma |
| 5 | 25 | Female | CEA | 12 | 60 | 100 | Non-osteogenic
fibroma |
| 6 | 85 | Male | GA | 12 | 90 | 200 | Liposarcoma |
Follow-up and pain
All diagnoses were the same as had been indicated by
the biopsies. There were no wound complications and the hip ranges
of motion and length were the same as those prior to surgery. No
deep vein thrombosis was identified in any of the patients;
however, one patient suffered from sensory dysfunction, with
persistent numbness and paresthesia in the distribution of the
femur nerve after surgery. These symptoms gradually decreased after
three weeks of symptomatic treatment. All six patients were fully
satisfied with the extent of pain relief following surgery.
Sensations of pain were eliminated entirely in five of the patients
following surgery, although a single patient continued to report
mild pain (VAS, 18 mm) (Table II),
while the remaining patient experienced mild pain for six months,
which ceased eight to nine months after surgery. No evidence of
local tumor recurrence, femur head necrosis or hip joint
degeneration disease was identified in any of the patients.
 | Table II.VAS for patient pain prior to and
following surgery. |
Table II.
VAS for patient pain prior to and
following surgery.
|
| VAS (mm) |
|---|
|
|
|
|---|
| Patient | Pre-surgery | Post-surgery |
|---|
| 1 | 55 | 0 |
| 2 | 68 | 0 |
| 3 | 57 | 0 |
| 4 | 62 | 18 |
| 5 | 60 | 0 |
| 6 | 43 | 0 |
Samples and gap measurement
In total, there were 11 small nerve branches in six
of the specimens, three in one specimen and two in three specimens,
while the remaining specimens contained just one nerve. Two small
arteries and one lymphatic vessel were identified in three separate
specimens, respectively. The lateral femoral circumflex artery
encounter to femoral nerves in our investigated area in all
specimens. The saphenous nerve was the most internal nerve in the
selected region; however, in two cases, the nerve was in front of
the femoral artery in the proximal region. As two saphenous nerves
front the femoral artery in the proximal of our region, in fact,
our measurement measured distance from femoral artery trunk lateral
margin to medial margin of saphenous nerves in 18 cases, to vastus
medialis muscle branches of femoral nerve in two cases. The space
in 4 cm proximal of lesser trochanter was 8.01±2.71 mm, 2 cm was
9.65±2.60 mm, 0 cm was 10.12±2.91 mm, and 2 cm distal of lesser
trochanter was 9.89±2.74 mm, 4 cm was 9.58±2.86 mm, 6 cm was
8.39±2.99 mm (Table III). The
distance from the highest point of lesser trochanter to the start
of the lateral circumflex femoral artery was 12.56±9.74 mm.
 | Table III.Measurements of the space between the
femoral artery and femoral nerve. |
Table III.
Measurements of the space between the
femoral artery and femoral nerve.
| Specimen | Min (mm) | Max (mm) | Mean ± SD (mm) |
|---|
| a | 0.00 | 12.72 |
8.01±2.71 |
| b | 4.86 | 13.48 |
9.65±2.60 |
| c | 5.24 | 14.52 |
10.12±2.91 |
| d | 4.84 | 13.00 |
9.89±2.74 |
| e | 4.26 | 12.32 |
9.58±2.86 |
| f | 0.00 | 11.50 |
8.39±2.99 |
Discussion
The proximal femur is a common location for benign
tumor formation. Current treatment options concentrate on tumors
that may lead to hip disfunction, recurring tumors (7) or pediatric cases (4). These procedures typically open the
capsule of the hip joint and surgeons select an approach based on
the orientation of the tumor (3).
Due to the proximity of the lesser trochanter to the capsule of the
hip, there is currently no surgical approach aimed specifically at
the lesser trochanter. Hip-specific surgical protocols are
typically used as the standard approach. Each hip-specific surgical
protocol exhibits advantages and disadvantages for performing tumor
resection or curettage in the lesser trochanter. A surgical
procedure for treating the lesser trochanter more directly may have
the advantages of allowing improved exposure to the area, resulting
in reduced surgical trauma compared with the conventional hip
approach.
The femoral triangle was selected as the operating
area due to its location above the lesser trochanter, which offered
the shortest distance. The femoral triangle contains a number of
vital blood vessels and nerves; thus, conventional surgical
approaches have typically avoided this region. However, these vital
blood vessels and nerves are usually thick, such as the femoral
nerve, artery and vein, and can be easily distinguished to avoid
injury. When the vital nerves and vessels were crossed, vital
nerves and blood vessels were not found in the gap between the
trunk of the femoral artery and innermost branch of the femoral
nerve. A limited number of small nerve branches and few small
artery and lymphatic vessels were observed in the cadaver research.
Therefore, following protection of the femoral artery and nerve in
the operating region, surgery may be safe and simple.
In the groin, the femoral artery and nerve are
separated by the arcus iliopectineus, suggesting that a certain
distance should exist in the proximal area of the femoral triangle.
Muhly and Orebaugh (8) and Hsu et
al (9) used ultrasound to
identify a space between the femoral nerve and femoral artery, the
size of which is proportional to the rotational angle of the lower
limb. The distance is widest at the level of the lesser trochanter
(10 samples among 20 specimens) and narrows towards both ends. The
spindle region, which has the widest distance in the lesser
trochanter, is suitable for the novel surgical procedure. Nerves
and vessels are able to be separated appropriately. In addition,
enclosed adipose tissue had a cushioning function (10). Thus, it was inferred that an
appropriate space could be separated in order to perform surgery,
without significant damage to the nerves and blood vessels.
The incision location was easily identified by
finding the pulse of the femoral artery. The incision, which
followed the outsight of the femoral artery, took advantage of the
position of the artery truck to avoid damaging the femoral nerve.
The abundance of adipose and muscle tissue was found to protect
important nerves and blood vessels, as well as facilitate blunt
separation. Adipose tissue between the vessels and nerves was
appropriately separated. It was ensured that the femoral nerve and
femoral vessels were separated to either side of the channel.
Vessels, including arteries and veins, should be trapped and
protected towards the medial, while nerves should be pulled
laterally. The iliopsoas and pectineal muscles were located deep in
the adipose tissue. The lesser trochanter was located at the end of
these two muscles, resulting in thinner muscle fiber in this
region, which made the lesser trochanter easier to access. In
addition, rotation of the hip joint permitted greater exposure.
These two muscles are often already separated or pulled to one side
by the tumor, typically toward the adipose tissue. The tumors were
resected from the adipose tissue. The lateral femoral circumflex
artery, which is a main branch of the profunda femoral artery and
also a division of the main vessel of the femoral artery, required
consideration during surgery. As shown in the cadaveric research,
the beginning position of the lateral femoral circumflex artery is
varied, and the vessel goes outward so that all the arteries cross
the femoral nerve. In the novel surgical approach, the region is
further exposed and susceptible to injury. Thus, ligaturing the
artery first may be a suitable and safe surgical approach.
The traditional approaches to accessing the lesser
trochanter, such as the lateral and anterior, involve extreme
rotation of the hip joint. Furthermore, a number of muscles are
typically removed, and reconstruction is required. These factors
contribute to increased surgical trauma and an increased frequency
of complications following surgery. The medial approach is closely
compared with other traditional approaches; however, the muscles
and vessels in that region are even more complex (11). A number of nerves and blood vessels
are present around the adductor brevis, including the obturator
nerve, artery and vein, which innervate and supply muscles, such as
the adductor longus, adductor magnus and gracilis. Moreover, high
anatomical variations in these nerves, blood vessels and their
branches increase the risk of injury (6). Medial approaches are often used to
treat dysplasia or hip dislocation; however, this approach has been
shown to have an avascular necrosis rate of 12–54.3% (12–16).
Furthermore, the incision is close to the perineum, which increases
the risk of infection.
Due to the decreased distance between the point of
incision and destination and careful separation in the novel
surgical approach, the surgery time, trauma and blood loss were
minimal. In addition, the complications caused by long periods of
immobility following surgery may be limited since patients can
exercise earlier following the procedure. The follow-up assessment
revealed evident pain relief and no evidence of lesion recurrence,
indicating that the surgical resections performed in the present
study were successful. The results of the VAS revealed that the
majority of patients experienced complete pain relief, with only
one patient continuing to report mild pain. However, the cause of
this remaining pain is not clear. We hypothesize that the nerve or
vessel was trapped for an extended period of time. Full exposure of
the tumor site is a basic condition for resective surgery. Due to
the absence of lesion recurrence, the exposed area was considered
to be sufficient. The separation process was relatively simple,
which was reflected by the short surgical time and decreased blood
loss. The extent of blood loss was associated with the lesion size
and the degree of adhesion of the surrounding tissue. A longer
surgical duration may lead to greater blood loss.
Two potential complications were identified prior to
surgery. Firstly, femur head necrosis and hip joint degeneration
disease may occur as a result of removing the lateral femoral
circumflex artery or its branches (5/6 patients), since it is one
of the main supply arteries of the femur head. However, no such
problem was identified during follow-up. It was inferred that the
blood supply was compensated by the numerous anastomotic vessels
near the greater trochanter, whose branches supply 65–80% of blood
to the femoral head (17–21). However, the long-term risk of femoral
head degeneration is not known. The other possible complication may
result from the blood vessels and nerves having been separated for
an extended period of time. Separating blood vessels increases the
risk of thrombus development; however, no evidence of a blood
vessel thrombus was identified following surgery, which may be a
result of the limited sample size. The femoral nerve was also kept
tense during surgery, and a number of its small branches may be
removed. This may cause sensory dysfunction, with persistent
numbness and paresthesia. Only one patient suffered from these
symptoms, which decreased three weeks after surgery. Irreversible
nerve damage requires further study, as the sample size was small
in the present study. Although small branches of the femoral nerve
were removed, knee strength was not decreased. Thus, it was
hypothesized that the flexor muscle group may not be impaired.
In conclusion, the novel approach described in the
present study may be a feasible protocol for the resection of
benign tumors, and also the preoperative palliative resection of
malignant tumors. The technique is particularly suited to tumors
extending toward the lateral and anterior of the lesser
trochanter.
References
|
1
|
Barros Filho TE, Oliveira RP, Taricco MA
and Gonzalez CH: Hereditary multiple exostoses and cervical ventral
protuberance causing dysphagia. A case report. Spine (Phila Pa
1976). 20:1640–1642. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cardelia JM, Dormans JP, Drummond DS,
Davidson RS, Duhaime C and Sutton L: Proximal fibular
osteochondroma with associated peroneal nerve palsy: A review of
six cases. J Pediatr Orthop. 15:574–577. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bottner F, Rodi R, Kordish I, Winklemann
W, Gosheger G and Lindner N: Surgical treatment of symptomatic
osteochondroma. A three- to eight-year follow-up study. J Bone
Joint Surg Br. 85:1161–1165. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Learmonth DJ and Raymakers R:
Osteochondroma of the femoral neck secondary to a slipped upper
femoral epiphysis. Arch Orthop Trauma Surg. 112:106–107. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li M, Luettringhaus T, Walker KR and Cole
PA: Operative treatment of femoral neck osteochondroma through a
digastric approach in a pediatric patient: a case report and review
of the literature. J Pediatr Orthop B. 21:230–234. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Anagnostopoulou S, Kostopanagiotou G,
Paraskeuopoulos T, Chantzi C, Lolis E and Saranteas T: Anatomic
variations of the obturator nerve in the inguinal region:
Implications in conventional and ultrasound regional anesthesia
techniques. Reg Anesth Pain Med. 34:33–39. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hsieh PC, Ondra SL, Grande AW, et al:
Posterior vertebral column subtraction osteotomy: a novel surgical
approach for the treatment of multiple recurrences of tethered cord
syndrome. J Neurosurg Spine. 10:278–286. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Muhly WT and Orebaugh SL: Ultrasound
evaluation of the anatomy of the vessels in relation to the femoral
nerve at the femoral crease. Surg Radiol Anat. 33:491–494. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hsu HT, Lu IC, Chang YL, Wang FY, Kuo YW,
Chiu SL and Chu KS: Lateral rotation of the lower extremity
increases the distance between the femoral nerve and femoral
artery: An ultrasonographic study. Kaohsiung J Med Sci. 23:618–623.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Norgan NG: The beneficial effects of body
fat and adipose tissue in humans. Int J Obes Relat Metab Disord.
21:738–746. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Moore AE and Stringer MD: Iatrogenic
femoral nerve injury: A systematic review. Surg Radiol Anat.
33:649–658. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Szöke G, Staheli LT, Jaffe K and Hall JG:
Medial-approach open reduction of hip dislocation in
amyoplasia-type arthrogryposis. J Pediatr Orthop. 16:127–130. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tumer Y, Ward WT and Grudziak J: Medial
open reduction in the treatment of developmental dislocation of the
hip. J Pediatr Orthop. 17:176–180. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tarassoli P, Gargan MF, Atherton WG and
Thomas SR: The medial approach for the treatment of children with
developmental dysplasia of the hip. Bone Joint J. 96-B:406–413.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Koizumi W, Moriya H, Tsuchiya K, Takeuchi
T, Kamegaya M and Akita T: Ludloffs medial approach for open
reduction of congenital dislocation of the hip. A 20-year
follow-up. J Bone Joint Surg Br. 78:924–929. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Okano K, Yamada K, Takahashi K, Enomoto H,
Osaki M and Shindo H: Long-term outcome of Ludloffs medial approach
for open reduction of developmental dislocation of the hip in
relation to the age at operation. Int Orthop. 33:1391–1396. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kalhor M, Horowitz K, Gharehdaghi J, Beck
M and Ganz R: Anatomic variations in femoral head circulation. Hip
Int. 22:307–312. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ichikawa T, Haradome H, Hachiya J,
Nitatori T and Araki T: Diffusion-weighted MR imaging with a
single-shot echoplanar sequence: detection and characterization of
focal hepatic lesions. AJR Am J Roentgenol. 170:397–402. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Grose AW, Gardner MJ, Sussmann PS, Helfet
DL and Lorich DG: The surgical anatomy of the blood supply to the
femoral head: description of the anastomosis between the medial
femoral circumflex and inferior gluteal arteries at the hip. J Bone
Joint Surg Br. 90:1298–1303. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Boraiah S, Dyke JP, Hettrich C, Parker RJ,
Miller A, Helfet D and Lorich D: Assessment of vascularity of the
femoral head using gadolinium (Gd-DTPA)-enhanced magnetic resonance
imaging: a cadaver study. J Bone Joint Surg Br. 91:131–137. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gautier E, Ganz K, Krügel N, Gill T and
Ganz R: Anatomy of the medial femoral circumflex artery and its
surgical implications. J Bone Joint Surg Br. 82:679–683. 2000.
View Article : Google Scholar : PubMed/NCBI
|