Introduction
Breast infarction occurs as a sequela of benign
breast lesions, such as fibroadenomas, or as a spontaneous change
in healthy breast tissue typically during pregnancy and lactation
(1). Spontaneous solitary infarction
is very rare. Infarction of the breast tissue with hyperplasia
related to pregnancy and/or lactation was first reported by Hasson
and Pope in 1961 (2). Infarction
typically presents as a palpable mass that may be painful and
varies between soft and hard in consistency. It can be mistaken for
a carcinoma due to the hard consistency of the lesion. Infarcts
usually occur as a single lesion, localized to a fibroadenoma, or
hyperplastic lactating breast tissue during the peripartum period;
however, extensive, multifocal, bilateral mammary infarction is
very rare (3). Localized infarction
is most frequently observed in the third trimester of pregnancy or
early postpartum period. In this report, a rare case of breast
infarction occurring during pregnancy and lactation in a
20-year-old woman is presented.
Case report
A 20-year-old woman first noticed a painless lump
(~5×4 cm in size) in her right breast at 2 months of gestation.
However, she did not seek medical attention for the lump. The lump
gradually increased in size but remained painless. At term, she
delivered a healthy, normal baby boy by cesarean section. During
lactation, the patient noted that milk production in the right
breast was less than that in the left one. Over a period of 1 month
after delivery, the lump grew rapidly in size with marked
discoloration of the overlying skin. The patient also had
irregular, high-grade fever, with the body temperature rising to
39°C. The patient was then admitted to hospital at 1 month
postpartum. The patient had no history of taking any special
medication. Clinical examination revealed a soft lump of size 18×16
cm in her right breast with pigmentation and induration of the
overlying skin (Fig. 1). A palpable
lymph node (~2×1.5 cm) was identified in the right axilla of the
patient. The patient had no history of trauma or use of oral
contraceptives.
Color Doppler ultrasonography of the right breast
revealed a well-circumscribed area of mixed echogenicity, with an
approximate size of 199.7×56.7 mm; the heterogeneous echogenicity
of the internal region of the mass suggested fluid content. Some
lymph nodes with abnormal appearance were noted in the right
axilla, with the maximum size of the lymph nodes being 19.0×12.1 mm
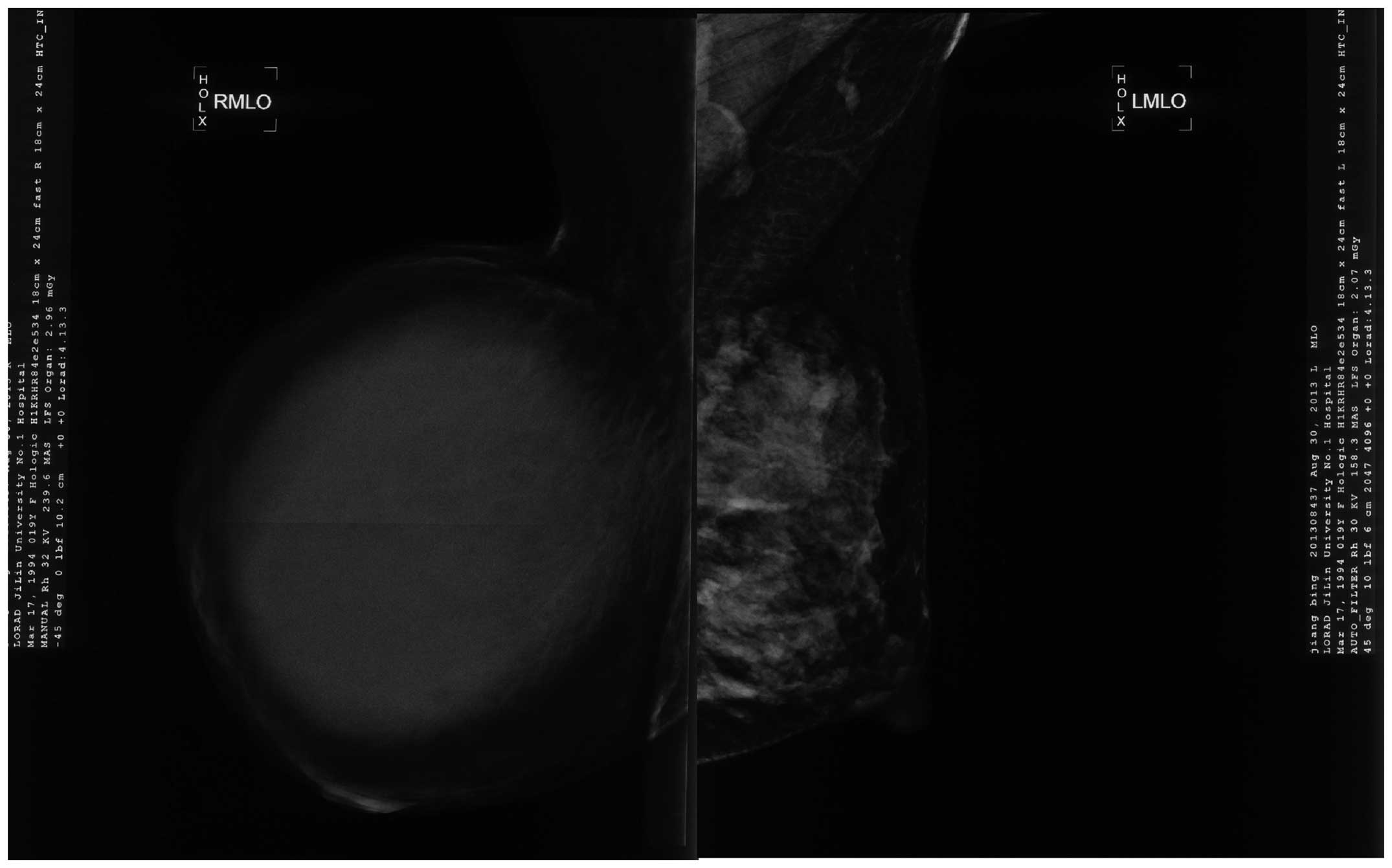
(Fig. 2). Mammography of the right
breast showed a regular, high-density mass shadow, with an
approximate size of 11.0×13.0 cm (Fig.
3). Normal mammary gland tissue could not be identified on the
mammogram. No clear calcification was found within and around the
lesion.
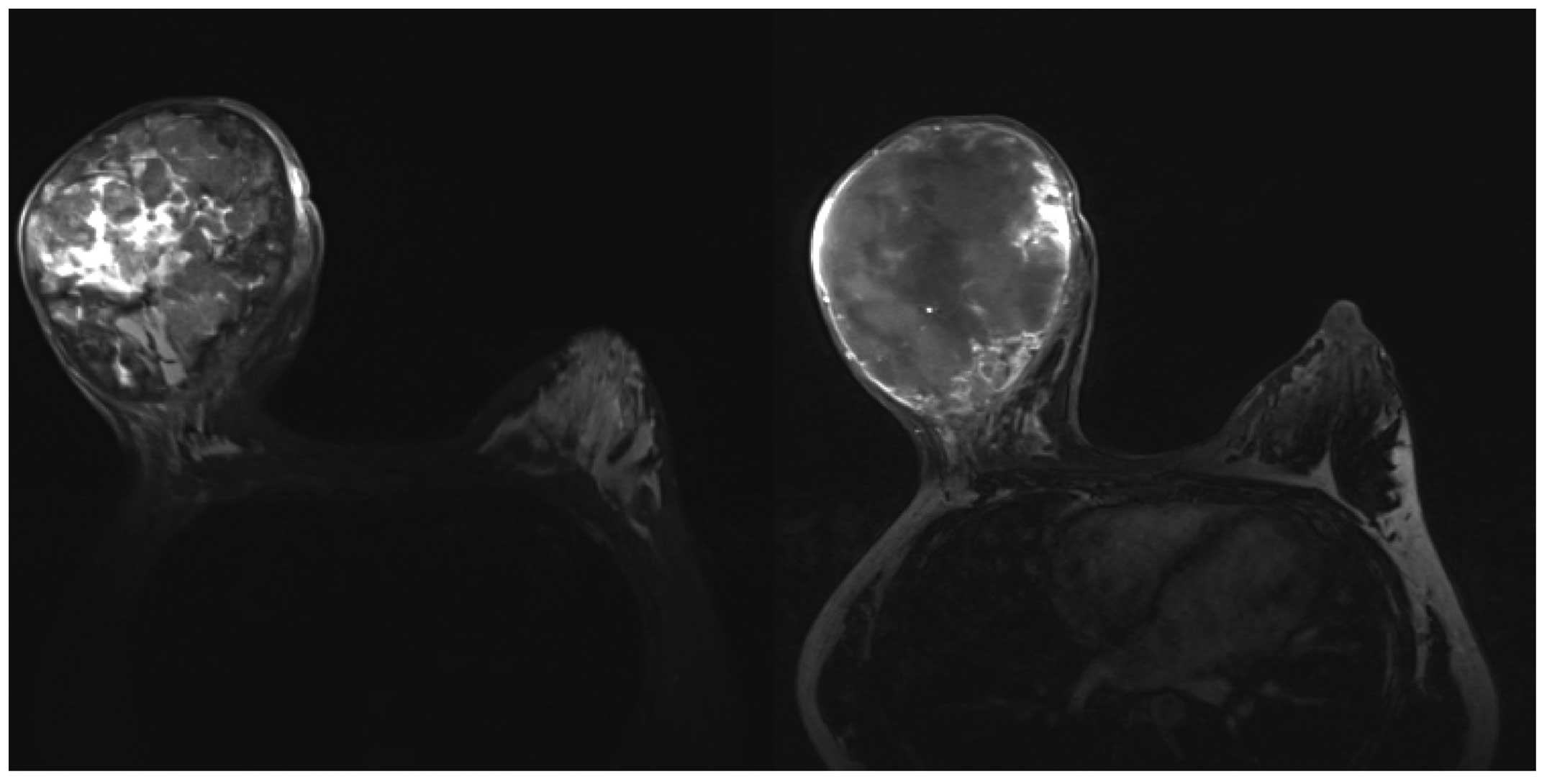
T1-weighted nuclear magnetic resonance imaging
(NMRI) of the right breast revealed the presence of a mass of size
13.4×10.9 cm showing heterogeneous signal intensity, with areas of
isointensity, slight hyperintensity and hypointensity. A scan with
edge enhancement showed a significant increase in heterogeneity. No
abnormality in signal intensity was identified in the pectoralis.
Soft tissue masses, with visible enhancement and diameter 0.4–1.4
cm, were also detected in the right axilla (Fig. 4).
The patient had unexplained, irregular high-grade
fever, but no post-cesarean wound infection. Gynecological
ultrasonography revealed that the depth of ascitic fluid posterior
to the uterus was 11 mm, which suggested that the possibility of
postoperative infection was minimal. The results of blood culture
tests were negative. Urine culture revealed the presence of
Corynebacterium species at a concentration of <10,000
cfu/ml. The fever (temperature, 38°C) persisted.
Core-needle biopsy was performed to establish the
pathological diagnosis and revealed that the lump was composed of
necrotic and unorganized material. No clear tumor lesions were
found within and around the lump. At 5 days after admission,
minimally invasive Mammotome™ biopsy was performed to further
confirm the diagnosis; examination of the biopsied sample revealed
fibroadenosis in the right breast, with lobular hyperplasia, tissue
infarction and unorganized structure. Therefore, surgical treatment
was considered.
Since there was no evidence of normal breast tissue
in the right breast, we advised the patient to undergo mastectomy
and prosthetic reconstruction. The patient underwent mastectomy but
refused prosthetic reconstruction for financial reasons.
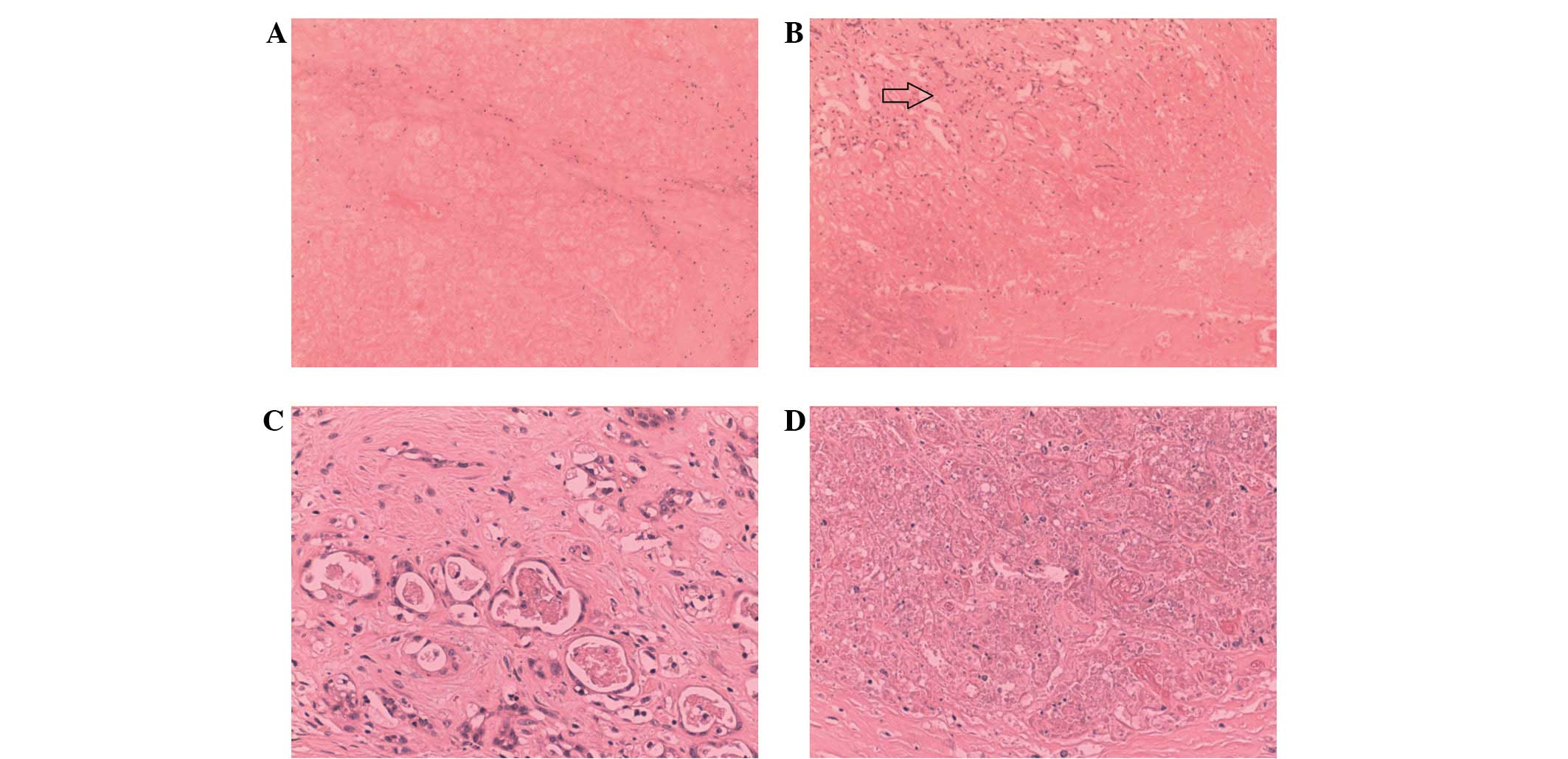
Histopathological study of the resected breast tissue revealed that
90% of the breast tissue had undergone infarction and that the
infarct was located centrally, under the areola. The breast tissue
also exhibited tissue involution and small focal hemorrhages. The
interstitial tissue showed infiltration of acute and chronic
inflammatory cells. Some of the breast ducts showed cystic
dilatation, and the formation of cysts with galactostasia. The
nipple and milk ducts did not show any evident lesions, and the
basal tissue of the breast did not show any evidence of infarction,
with the exception of dilatation and congestion of small blood
vessels to a certain extent. Postoperative recovery of the patient
was good and uneventful, and the fever subsided following the
surgical resection (Figs. 5 and
6). This study was approved by the
ethics committee of the Bethune First Hospital, Jilin University
(Jilin, China) and written informed consent was provided by the
patient.
Discussion
Spontaneous breast infarction is a rare entity.
Infarction of the breast tissue with hyperplasia associated with
pregnancy and/or lactation was first reported by Hasson and Pope in
1961 (2). Infarction typically
presents as a palpable mass that is sometimes painful and soft or
hard in consistency. It can be mistaken for a carcinoma due to the
hard consistency of the lesion. Infarcts usually occur as a single
lesion, localized to a fibroadenoma, or hyperplastic lactating
breast tissue during the peripartum period; however, extensive,
multifocal, bilateral mammary infarction is very rare (3). Localized infarction is most frequently
observed in the third trimester of pregnancy or early postpartum
period. Breast infarction during pregnancy or lactation may also be
mistaken for fibroadenoma (4).
Clinically, fibroadenoma typically occurs in young women during
pregnancy or lactation and presents as a firm, smooth, painless and
easily palpable lump with a well-defined shape. These features are
very similar to those of spontaneous infarction of the breast;
therefore, it is very difficult to distinguish between the two
lesions on the basis of clinical examination alone. Other terms
used to describe breast infarction in the published literature are
adenoma associated with pregnancy or lactation adenoma,
drug-induced breast necrosis (5),
and ischemic fat necrosis of the mammary region (6). In the present case, the results of
pathologic examination revealed the presence of hyperplastic breast
lobules and ischemic necrosis rather than adenomatous features.
Thus, the distinction between infarction and lesions such as
fibroadenoma may not be very difficult. However, during the
diagnostic evaluation in this case, Bard-needle aspiration biopsy
revealed that most tissues were necrotic, with loss of organized
structure. The diagnosis of the lesions could not be definitively
established by core-needle biopsy alone because the sample size
collected was small; this highlights the importance of performing
Mammotome™ biopsy or surgery to confirm the diagnosis of breast
infarction.
On admission, the patient had high-grade, irregular
fever. No case of breast infarction accompanied by fever has been
reported thus far in the literature (7). The fever could have been related to
urinary tract infection, heat absorption of necrotic tissue, or
infection associated with the lump. After the surgery, the
patient's body temperature was restored to normal, and no signs of
infection were noted in the lump tissue. This implies that the
patient's fever was most probably caused by heat absorption from
the necrotic tissue.
The etiology of breast infarction is yet to be
conclusively established; however, proposed theories implicate
vascular insufficiency and localized thrombosis. None of the cases
of breast infarction reported thus far have shown any evidence of
vascular disease or trauma. Another factor associated with the
occurrence of breast infarction is the use of oral contraceptives
(4). Certain medications are known
to exacerbate fibrocystic disease or compromise breast vascularity,
which in turn results in mass formation and necrosis; however, none
of the patient's medications have been shown to lead to breast
complications (3). In the present
case, the pathological examination showed hyperplastic breast
lobules and ischemic necrosis, but no evidence of malignancy.
Therefore, a diagnosis of ischemic infarct was made. The
pathological examination did not reveal any clear signs of venous
thrombosis or vascular endothelial lesions. One of the possible
explanations for the occurrence of breast infarction in this case
is that a local artery may have been compressed during the
lactation period, during which a rich blood supply is necessary.
This compression could have led to ischemic infarction of the
glandular tissue distant from the base of the breast. However, no
signs of infarction were noted in the breast, skin and subcutaneous
tissue because of their intact inherent blood circulation system.
The functions of the mammary glands are controlled by the
neuroendocrine system. Therefore, neuroendocrine disorders may lead
to partial arterial spasm, insufficient blood supply, and tissue
ischemia in the mammary glands. In the present case, the patient
should have been in the lactation stage, but the resected breast
tissue showed involution of the remaining breast tissue on
histopathological examination, thereby indicating dysfunction of
the lactation system. The results of the pathological examination
showed that 90% of the infarct was located centrally, under the
areola, and no evidence of infarction was noted in the peripheral
areas of the breast, including the subcutaneous tissue and
glandular tissue at the base of breast. This finding supports the
possibility that the hyperplastic breast tissue underwent necrotic
changes secondary to ischemia. However, these considerations are
inadequate to explain why the infarction was unilateral rather than
bilateral.
NMRI revealed linearly distributed areas of low
signal intensity surrounding the mass. Enhanced edge scanning
showed a significant enhancement of heterogeneity. The lesion was
observed to be composed of mixed elements, including necrotic
tissues and lactation-associated components. Non-enhanced NMRI
revealed heterogeneous signals in the lesions; however,
contrast-enhanced NMRI revealed pronounced heterogeneous signals in
long and wedge-shaped regions that extended to the center of the
lesions, which may represent granulation tissue growing into the
infarcted area. Increases in the number and thickening of the
arterial shadows were also observed around the lesion, which most
probably reflects the compensatory dilatation and congestion of the
collateral circulation around the lesion. It is possible that the
surface of the lesion was covered in fibrous tissue that formed a
capsule.
The majority of patients with breast infarction are
treated with widespread local excision, which is often performed
after pregnancy (7). In such cases,
the period of hyperplasia of breast tissue ends at the time of the
surgery, and therefore, no case of breast tissue remaining after
local excision has been reported thus far. However, it remains to
be determined whether widespread local excision is safe in patients
with hyperplastic breast tissue. In the present case, the lump was
too big (occupying the entire right breast) for wide local excision
to be performed; therefore, mastectomy and prosthetic
reconstruction was recommended. However, the patient refused
prosthetic reconstruction because of financial constraints.
In conclusion, the present study describes a rare
case of breast infarction associated with pregnancy and lactation
presenting with irregular, high-grade fever. From experience in
this case, it is suggested that in cases of breast infarction, the
findings of core-needle biopsy should be cautiously interpreted
when the sample size is small and that Mammotome™ biopsy or
surgical excision should be performed to confirm the diagnosis.
Widespread local excision is the treatment of choice for this
condition.
References
|
1
|
Kavdia R and Kini U: WCAFTI: Worrisome
cytologic alterations following tissue infarction; a mimicker of
malignancy in breast cytology. Diagn Cytopathol. 36:586–588. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hasson J and Pope CH: Mammary infarcts
associated with pregnancy presenting as breast tumors. Surgery.
49:313–316. 1961.PubMed/NCBI
|
|
3
|
Aggon AA, Eakin LO, Desimone N and Snyder
JA: Extensive multifocal mammary infarction - a case report. Breast
Care (Basel). 8:143–145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Skenderi F, Krakonja F and Vranic S:
Infarcted fibroadenoma of the breast: Report of two new cases with
review of the literature. Diagn Pathol. 8:382013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Davis CE Jr, Wiley WB and Faulconer RJ:
Necrosis of the female breast complicating oral anticoagulant
treatment. Ann Surg. 175:647–656. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Robitaille Y, Seemayer TA, Thelmo WL and
Cumberlidge MC: Infarction of the mammary region mimicking
carcinoma of the breast. Cancer. 33:1183–1189. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Behrndt VS, Barbakoff D, Askin FB and Brem
RF: Infarcted lactating adenoma presenting as a rapidly enlarging
breast mass. AJR Am J Roentgenol. 173:933–935. 1999. View Article : Google Scholar : PubMed/NCBI
|