Introduction
Stress urinary incontinence (SUI) is a common pelvic
floor dysfunctional disorder in middle-age women, accounting for
>40% of cases in menopausal women (1). The disease involves leakage of urine
when abdominal pressure due to coughing, laughing and sneezing
occurs. Consequently, when the affected patients walk or lay down,
urine leakage occurs. Since it is difficult to control urinary
incontinence, many patients experience serious psychological
barriers. Therefore, SUI, also known as the ‘social cancer’
constitutes both a health and social issue. The WHO has listed SUI
as one of the five major chronic diseases (2). At present, the pathogensis of SUI
remains to be determined although changes in the female pelvic
floor and lower urethral continence-controlled system during
pregnancy and childbirth constitute the primary risk factors for
SUI (3).
Mobility of ureterovesical junction (UVJ-M),
rotation angle and distance from the bladder neck to lower edge of
pubic bone are largely associated with the occurrence and severity
of SUI (4). Mouritsen and Rasmussen
(5) suggested that an ultrasound
diagnosis should be considered the reference standard. Pregazzi
et al (6) suggested that
UVJ-M >1 cm can be used as an objective indicator for the
ultrasound diagnosis of SUI in non-pregnancy. In view of the
non-invasive, no radiation, and repeatability of ultrasound
diagnosis, the present study was conducted to predict the value of
SUI in late pregnancy and postpartum by transperineal ultrasound.
By using receiver operating characteristic (ROC) curve analysis, we
obtained higher sensitivity and specificity of the threshold as an
early screening of high-risk groups with SUI in late pregnancy and
postpartum. Thus, to reduce the incidence of SUI and improve the
quality of life of women in late pregnancy, early diagnosis,
intervention and treatment are imperative.
Patients and methods
Patients
During the period December 2012-March 2014, 120
primigravidas with single birth were selected for the present study
at the Tangshan Maternal and Child Health Center (Tangshan, China).
Patients who experienced a mid-term induction of labor or maternal
surgery, pre-existing SUI, body mass index >30 kg/m2, combined
pregnancy hypertension, gestational diabetes mellitus, ultrasound
examination of fetal weight >4,000 g in the third trimester, too
much or too little amniotic fluid, long-term constipation, chronic
cough and asthma history were excluded. SUI diagnostic standards
included leakage of urine when abdominal pressure was increased via
coughing, laughing and sneezing, and use of the international
continence inquiring committee's questionnaire short form for
accurate diagnosis.
Methods
Informed consent was obtained from patients and
their families. The study was approved by the ethics committee of
the Tangshan Maternal and Child Health Center (Hebei, China).
Patients were divided into the SUI and non-SUI groups at 34, 36,
and 38 gestational weeks and 6 weeks after delivery, respectively.
The same color ultrasound room was fixed with GE Voluson E8
ultrasound equipment and the GE broadband convex array probe with
frequency 5.0 MHz (Willowick, OH, USA), 15° forward to the
front-end probe with effective visual field of 90°, 250 mm in
length and diameter 17 mm. The front end of the probe was slightly
expanded with a maximum diameter of 27 mm (GE Healthcare,
Piscataway, NJ, USA). An experienced sonographer measured the UVJ-M
value, created the ROC curve and predicted the threshold value.
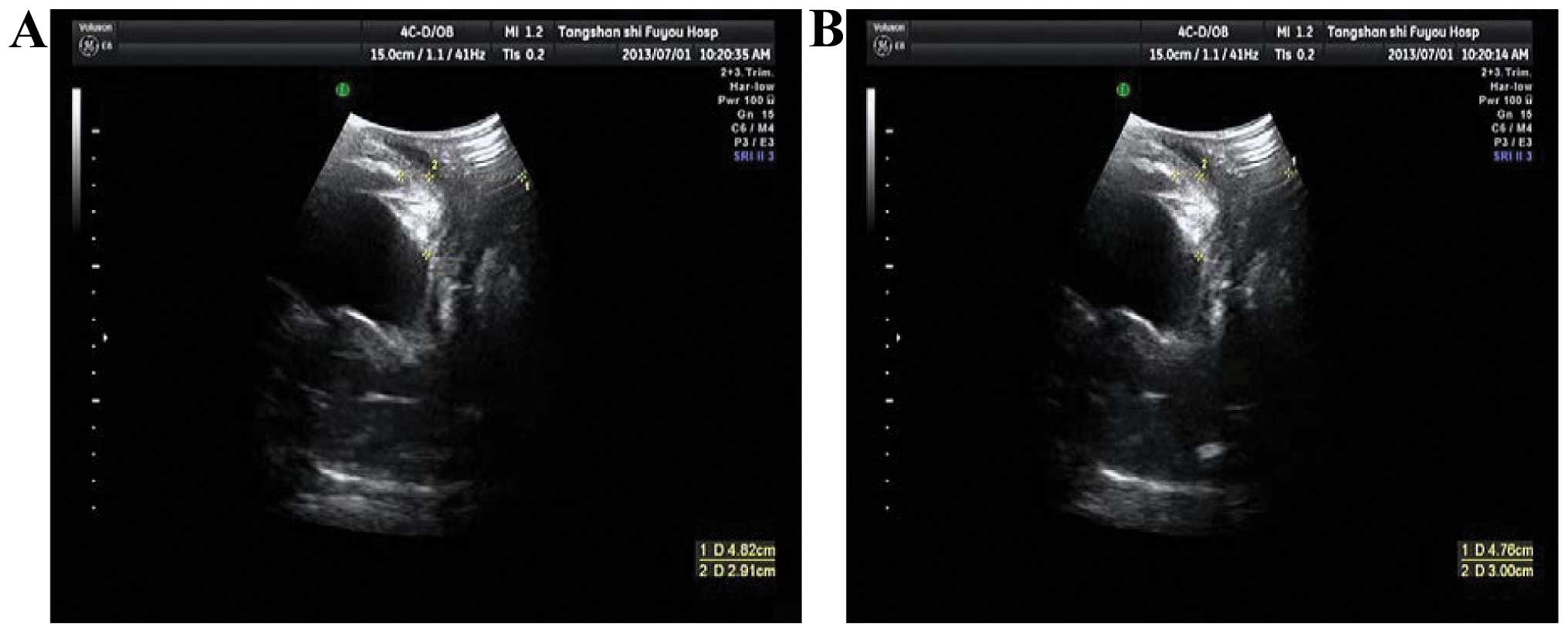
The UVJ-M measurement procedure required the
patients be placed in a supine position. The bladder urine volume
was evaluated as 250–500 ml by regular color ultrasound. Patients
were enjoined to bend knees in the lithotomy position. In addition,
neutrally medical disinfection coupling agent should be smeared
evenly on the surface of probe. Subsequently, the probe was covered
with a condom on which neutrally medical disinfection coupling
agent was applied. To place the probe into the perineum
successfully, the axes of the handle of the probe were parallel to
the vertical axes of the human body to ensure free movement of the
probe. The investigator was required to use sufficient strength to
overcome resistance of the vaginal walls and associated structures.
The probe made longitudinal incisions and the investigator
freeze-framed the images (sonogram), including lower margin of the
pubic bone, base of bladder, UVJ, urethra, vagina and sagittal
image of rectum. A trackball was used to draw up the outline of
base of bladder and UVJ (7). During
the entire procedure, the patient remained in a relaxed state. To
obtain further images, Valsalva manoeuvres were carried out, the
UVJ was observed to slide backward, a procedure also conducted for
soft issues of variants and rectum. When UVJ-M reached its maximum,
sonogram images were obtained again for measurement. By replaying
the ultrasound image and moving the cursor, UVJ-M was measured as
the distance between UVJ in stationary stage and UVJ in tension.
The average of this distance was subsequently calculated. UVJ-M
images of patients with or without SUI at different time points are
shown in Figs. 1–5.
Observing index
To obtain the threshold of UVJ-M in late pregnancy
and after delivery, the ROC curve was analyzed on the basis of SUI
prevalence and UVJ-M value, respectively, in 34, 36, and 38
gestational weeks and 6 weeks after delivery. ROC curve is
dependent on true- and false-positive rates. Any point on the curve
shows the relationship between the specific positive standard and
the sensitivity and specificity in certain screening tests: UVJ-M
value dring late pregnancy and postpartum (8).
Statistical analysis
Data were analyzed using SPSS 20.0 (IBM SPSS,
Armonk, NY, USA) statistical software package. Measurement data
were presented as mean ± standard deviation. Comparisons in
multiple and two groups were assessed using analysis of variance
and independent sample t-test, respectively. Measurement data were
shown as [no. (%)], and comparison between the groups was
determined by the χ2 test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of baseline data
Analysis of baseline data revealed that for 38
gestational weeks, there were 52 cases of SUI (43.3%). No
statistically significant differences were identified (P>0.05)
(Table I).
 | Table I.Comparison of baseline data (mean ±
standard deviation). |
Table I.
Comparison of baseline data (mean ±
standard deviation).
| Group | Case | Age | Height | BMI
(kg/m2), before 34 gestational weeks | Growth in BMI
(kg/m2), during weeks |
|---|
| SUI | 52 | 26.5±2.4 | 159±18.2 | 23.7±3.1 | 6.5±1.1 |
| Non-SUI | 68 | 25.8±2.6 | 158±18.7 | 23.5±3.2 | 6.8±1.2 |
| t-test |
| 0.981 | 1.232 | 1.560 | 0.471 |
| P-value |
| 0.423 | 0.924 | 0.785 | 0.326 |
SUI prevalence and UVJ-M in different
stages of pregnancy
At 34, 36, and 38 gestational weeks, as well as 6
weeks after delivery, the SUI prevalence was 7.5 (9/120), 22.5
(27/12), 43.3 (52/120), and 5.8% (7/120), respectively. The SUI
prevalence was increased with the gestational weeks, with
statistically significant differences (χ2=5.624,
P=0.016) (data not shown). The UVJ-M value was 3.43±1.52,
4.76±1.33, 6.77±0.98 and 2.35±1.04 mm, respectively. The UVJ-M
value increased with the gestational weeks, with a statistically
significant difference (Table
II).
 | Table II.Different UVJ-M values in different
stages of pregnancy. |
Table II.
Different UVJ-M values in different
stages of pregnancy.
| Group | 34 weeks | 36 weeks | 38 weeks | 6 weeks after
delivery |
|---|
| SUI | 3.43±1.52 | 4.76±1.33 | 6.77±0.98 | 2.35±1.04 |
| Non-SUI | 2.56±1.13 | 3.76±1.48 | 6.01±1.85 | 1.41±0.66 |
| t-test | 4.182 | 3.754 | 4.621 | 5.743 |
| P-value | 0.037 | 0.039 | 0.028 | 0.012 |
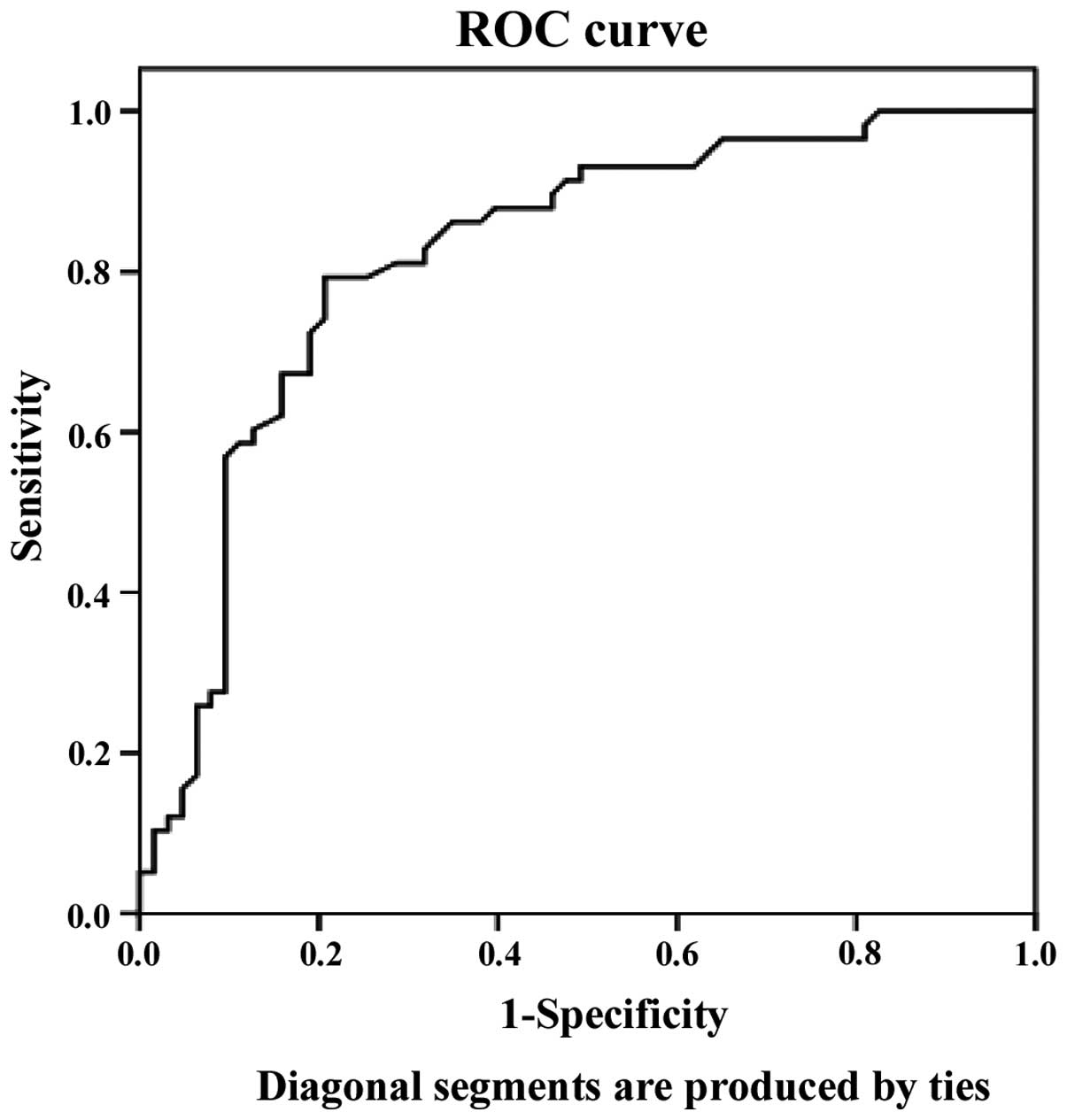
Analysis of ROC curve
ROC curve was constructed on the basis of UVJ-M
whether SUI occurs in late pregnancy. Horizontal axes showed the
specificity, and vertical axes showed the sensitivity. Generally,
the point closest to the top left corner of the curve was
considered the optimal threshold. Fig.
6 shows that the square below the curve was 0.819. The standard
error of the square was 0.039, and the 95% confidence interval of
the square was (0.742–0.896), with the exception of 0.5. The ROC
curve determined that the optimal threshold was 6.59 mm, in
correlation to a sensitivity of 95% and a specificity of 77.8%.
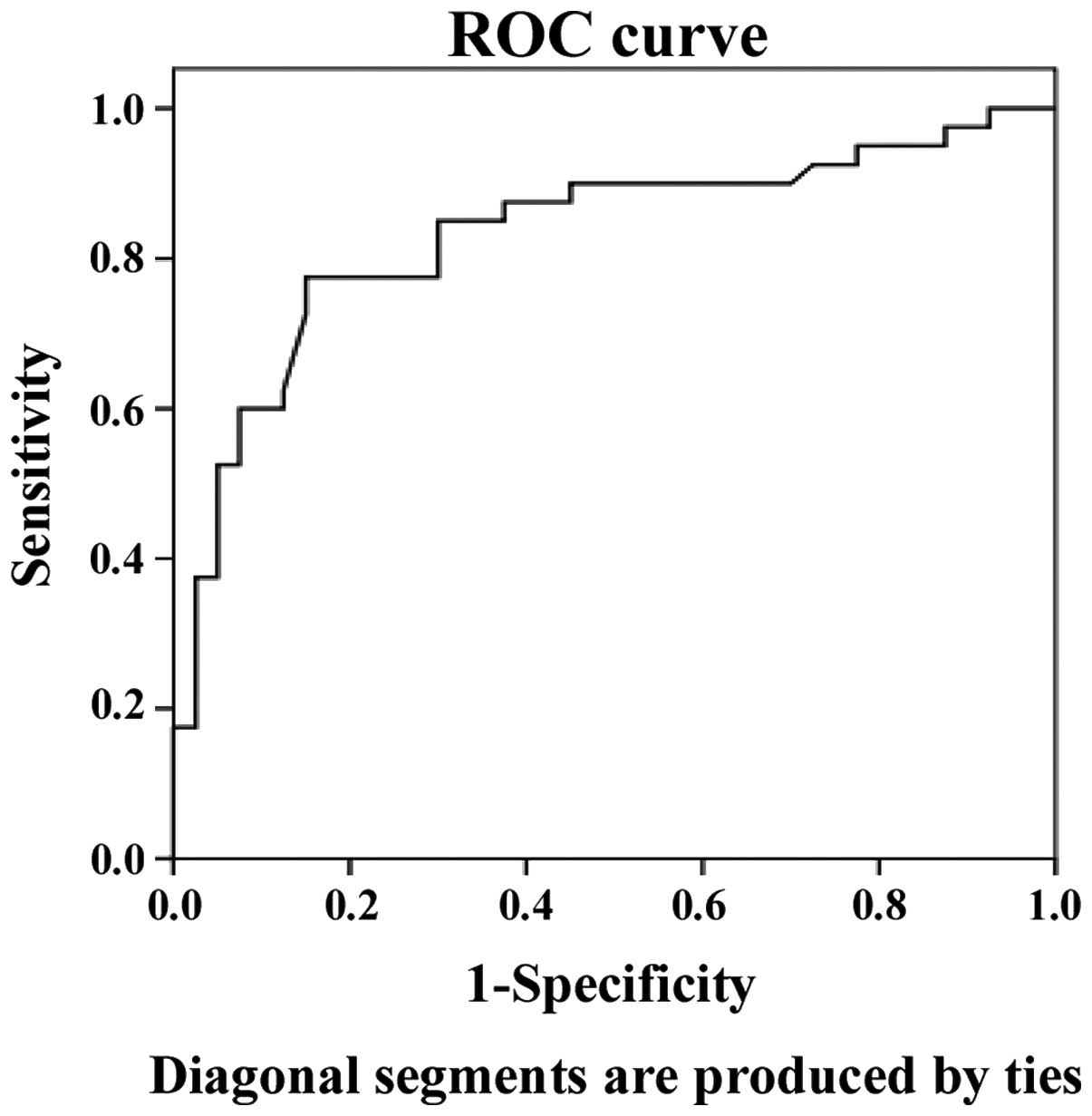
The ROC curve analysis of UVJ-M from the SUI and
non-SUI groups after delivery, revealed the square below the curve
was 0.832. The standard error of the square was 0.047, and the 95%
confidence interval of the square was (0.739–0.925) with the
exception of 0.5. The ROC curve determined the optimal threshold to
be 8.66 mm in correlation to a sensitivity of 89.5% and a
specificity of 66.7% (Fig. 7).
Discussion
The pathogenesis of SUI remains to be determined.
The hammock and integral hypotheses have been posited, with
supporters of the hammock theory advocating that maintaining
closure function of urethra is dependent on the pressure along the
anterior wall of the vagina and the supporting structure of the
bladder neck and the effective conduction between bladder neck and
urethra (4). The pelvic floor
compression of the urethra reduced the intensity and caused the
occurrence of SUI, where the supporting structure of anterior
vaginal wall and the bladder neck were destroyed. The integral
theory of pelvic floor involves focuses on urinary bladder,
urethra, uterus, rectum, anus, other pelvic organs and the related
muscles as a whole (7). Any defects
in part of the pelvic floor may lead to an imbalance of these
interactions, resulting in urethral pressure not being effectively
maintained when abdominal pressure is increased, leading to SUI.
The occurrence of SUI is in affected by the anatomical position of
the pelvic floor in both the hammock and integral hypotheses.
Pelvic floor damage in women is initiated during the
gestational period. The incidence rate of SUI is not high during
the early period of pregnancy. Owing to fetal growth and an
increase in pressure, collagen fiber in the pelvic floor muscles is
compelled to expand and stretch gradually, and tension relaxation
occurs to meet the needs required for childbirth (8). However, 6 weeks after delivery, the
muscles recover to the pre-pregnancy state, with the exception of
breast. The location of pelvic organs is also recovered (9). Therefore, the ultrasound examination
cannot only observe the location and mobility of the bladder neck
change in late pregnancy with gestational weeks, but can evaluate
recovery situations of position and function of pelvic organs. At
present, a number of methods are available to examine SUI such as
endoscopy, urethral pressure measurement, urine dynamics and
magnetic resonance imaging. Of these tecniques, ultrasound,
transperineal ultrasound in particular, allow for a real-time
dynamic observation of the shape and position of the urethra, and
bladder neck. Additionally, this ultrasound clearly identifies
mutual associations between the various structures of the pelvic
floor, thereby providing a morphological and functional basis for
the clinical diagnosis and treatment of SUI. At the same time,
advantages including non-radiation, safety, non-invasive, economic,
single operation and good repeatability render it more suitable for
pregnant women (10).
Parameters for ultrasonic monitoring of urinary
incontinence includes reflecting the retrovesical angle of the
posterior basal part in bladder and proximal urethra (11). It also includes vertical and
horizontal distance in accordance with distance between bladder
neck and symphysis. UVJ-M is an early parameter in the ultrasound
examination of labia, which is considered an important parameter
and significant sign of stability in bladder neck position. It is a
major factor involved in female continence mechanism (12,13).
Furthermore, due to the overactivity of UVJ-M, the bladder neck
junction is extremely low in tension, resulting in obstacles of
abdominal pressure, leading to the occurrence of SUI in women
(14–16). To construct the ROC curve and
identify the threshold value predicted, the present study measured
UVJ-M in 34, 36, and 38 gestational weeks and 6 weeks after
delivery, respectively. SUI prevalence and UVJ-M were increased
with the various gestational weeks. These differences were
statistically significant. The predicted value of SUI in late
pregnancy was UVJ-M ≥6.59 mm, while that after delivery was UVJ-M
≥8.66 mm.
The present study was based on the subjective
symptoms of the patients. It mainly focused on late pregnancy and
early postpartum. As the sample size in the present study was
relatively small, additional samples and an extension of the
follow-up time period to further confirm the reliability and
accuracy of SUI in the diagnosis of particular intervals
corresponding to UVJ-M during pregnancy and childbirth.
Acknowledgements
The study was supported by the Science and
Technology Research and Development Support Program (Tangshan City,
2012). The correlation factors of urinary tract anatomy defects and
postpartum SUI were indicated by no. 131302116z.
References
|
1
|
Abrams P, Andersson KE, Birder L, Brubaker
L, Cardozo L, Chapple C, Cottenden A, Davila W, de Ridder D,
Dmochowski R, et al: Members of Committees; Fourth International
Consultation on Incontinence: Fourth International Consultation on
Incontinence Recommendations of the International Scientific
Committee: Evaluation and treatment of urinary incontinence, pelvic
organ prolapse, and fecal incontinence. Neurourol Urodyn.
29:213–240. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ge J, Lu YX, Zhang Z and Li X: The
prevalence and cognition of urinary incontinence among female
adults in Beijing. Chin J Chin J Clin Obstet Gynecol. 11:15–17.
2010.
|
|
3
|
Rinne KM, Kainulainen S, Aukee S, Heinonen
S and Nilsson CG: Dynamic magnetic resonance imaging of the
behavior of the mid-urethra in healthy and stress incontinent
women. Acta Obstet Gynecol Scand. 89:373–379. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kruger JA, Dietz HP and Murphy BA: Pelvic
floor function in elite nulliparous athletes. Ultrasound Obstet
Gynecol. 30:81–85. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mouritsen L and Rasmussen A: Bladder neck
mobility evaluated by vaginal ultrasonography. Br J Urol.
71:166–171. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pregazzi R, Sartore A, Bortoli P, Grimaldi
E, Troiano L and Guaschino S: Perineal ultrasound evaluation of
urethral angle and bladder neck mobility in women with stress
urinary incontinence. BJOG. 109:821–827. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cosimato C, Cipullo LM, Troisi J, Di
Spiezio SA, Tommaselli GA, Oro RR, Zullo F, Altieri V and Guida M:
Ultrasonographic evaluation of urethrovesical junction mobility:
Correlation with type of delivery and stress urinary incontinence.
Int Urogynecol J. 26:1495–1502. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Masata J, Svabik K, Martan A, Drahoradova
P and Pavlikova M: [What ultrasound parameter is optimal in the
examination of position and mobility of urethrovesical junction?].
Ceska Gynekol. 70:280–285. 2005.PubMed/NCBI
|
|
9
|
Weinstein MM, Jung SA, Pretorius DH, Nager
CW, den Boer DJ and Mittal RK: The reliability of puborectalis
muscle measurements with 3-dimensional ultrasound imaging. Am J
Obstet Gynecol. 197:68.e1–68.e6. 2007. View Article : Google Scholar
|
|
10
|
Minardi D, Piloni V, Amadi A, El Asmar Z,
Milanese G and Muzzonigro G: Correlation between urodynamics and
perineal ultrasound in female patients with urinary incontinence.
Neurourol Urodyn. 26:176–182; discussion 183–184. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
García SL, Ramírez DL, Rey JR, Calvo JF,
Iglesias BR and Calvo AO: Complications of polypropylene mesh for
the treatment of female pelvic floor disorders. Arch Esp Urol.
64:620–628. 2011.PubMed/NCBI
|
|
12
|
Tincello DG, Botha T, Grier D, Jones P,
Subramanian D, Urquhart C, Kirkemo A and Khandwala S: TVT Worldwide
Registry Investigators: The TVT Worldwide Observational Registry
for Long-Term Data: safety and efficacy of suburethral sling
insertion approaches for stress urinary incontinence in women. J
Urol. 186:2310–2315. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen Z, Chen Y, Du GH, Yuan XY, Wu J, Zeng
XY, Hu ZQ, Cai D, Yang WM and Ye: Comparison of three kinds of
mid-urethral slings for surgical treatment of female stress urinary
incontinence. Urologia. 77:37–41; discussion 42. 2010.PubMed/NCBI
|
|
14
|
DuBeau CE, Kuchel GA, Johnson T II, Palmer
MH and Wagg A: Fourth International Consultation on Incontinence:
Incontinence in the frail elderly: report from the 4th
International Consultation on Incontinence. Neurourol Urodyn.
29:165–178. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
McClurg D, Ashe RG and Lowe-Strong AS:
Neuromuscular electrical stimulation and the treatment of lower
urinary tract dysfunction in multiple sclerosis - a double blind,
placebo controlled, randomised clinical trial. Neurourol Urodyn.
27:231–237. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim SO, Na HS, Kwon D, Joo SY, Kim HS and
Ahn Y: Bone-marrow-derived mesenchymal stem cell transplantation
enhances closing pressure and leak point pressure in a female
urinary incontinence rat model. Urol Int. 86:110–116. 2011.
View Article : Google Scholar : PubMed/NCBI
|