Introduction
Gastroscopy is a well-established, highly effective
diagnostic and therapeutic procedure. The frequency of this
procedure in the elderly is increasing rapidly as the general
population ages (1,2). Although it is a non-traumatic invasive
procedure, it often causes significant discomfort in the majority
of patients. With the collaboration of the anesthesia and digestive
system departments, gastroscopy under anesthesia minimizes the risk
of physical injury occurring during examination, and provides the
endoscopist with a suitable environment for a thorough examination.
This has been reported to be safe in high risk patients, including
elderly, frail and seriously ill patients (3,4). Despite
the benefits of using anesthesia for gastroscopy, it has
significant drawbacks. Anesthesia can delay patient recovery and
discharge time, and increases the risk of cardiopulmonary
complications, which are understood to account for ~50% mortality
and ~60% morbidity associated with upper gastrointestinal endoscopy
(5,6). This risk is increased in elderly
patients or those with cardiovascular diseases and upper
gastrointestinal bleeding (7).
Arterial hypoxemia, arrhythmias and myocardial ischemia have been
reported following gastroscopy with anesthesia (7).
Anesthesia strategies for gastroscopy have been
explored for decades. There are numerous reports on the safety
profile of propofol used for anesthesia during gastrointestinal
endoscopy (8–10). Propofol is currently the most
frequently used intravenous anesthetic, due to its rapid recovery
profile, and is widely used in outpatient surgeries and
examinations (4,10). The most prominent undesirable effect
of propofol is its marked depression on cardiovascular and
respiratory parameters, particularly in elderly patients (9–10). The
distinct pharmacological characteristics of etomidate include
improved hemodynamic stability and minimal respiratory depression
(11). This results in a wider
margin of safety for patients with significant risk factors,
including patients with valvular heart disease and myocardial
ischemia, and elderly patients. However, due to side effects,
including myoclonus and post-operative nausea and vomiting (PONV),
etomidate is rarely used in patients undergoing gastroscopy.
The aim of the present prospective study is to
determine the safety, efficacy, cost effectiveness, side effect
profile and recovery time of a combination of propofol and
etomidate, compared with propofol and etomidate alone, as
anesthetic regimens for gastroscopy.
Materials and methods
Patients and study design
The current study is a double-blinded, randomized,
parallel-group study, performed in accordance with the
International Conference on Harmonization Good Clinical Practice
guidelines (8). The study was
approved by the Ethics Committee of Renmin Hospital of Wuhan
University (Wuhan, China), and informed consent was obtained from
all patients. A total of 200 healthy, American Society of
Anesthesiologists grade I–II patients, consisting of 97 males and
103 females, aged between 65 and 79 years, who were scheduled for
gastroscopy with anesthesia, were included in the study. Patients
had normal serum chemistry, and normal liver and renal function
test results. No patients were experiencing cardiac or respiratory
disease. Exclusion criteria included the following: Severe
dysfunction of heart; lung, liver, kidney and adrenal
insufficiency; sleep apnea syndrome; gastric retention; history of
an allergic reaction to the study drugs; history of previous
experience with endoscopy; patients receiving analgesics, such as
nonsteroidal anti-inflammatory drugs; patients administered
α-methyldopa, clonidine or a β-blocker; patients with psychiatric,
neurological or neuromuscular disorders; or patients who had used
drugs, drank alcohol or smoked tobacco two weeks prior to the
study. Demographic data obtained included age, weight, gender and
primary diagnosis. Propofol and etomidate doses, administered by
bolus and continuous infusion, were recorded.
Medicine preparation, anesthesia
monitoring and gastroscopy procedure
Drugs used in the study included 200 mg/20 ml
propofol (AstraZeneca, London, UK), 20 mg/10 ml etomidate (Nhwa
Pharmaceutical Group, Jiangsu, China) and 100 mg/2 ml fentanyl
(Yichang Humanwell Pharmaceutical Co., Ltd., Yichang, China).
Etomidate and propofol were diluted to 20 ml prior to
administration. All dugs were prepared by an anesthesiologist who
was blinded to the study. An investigator, who was blinded to group
assignment, assessed and recorded all observed parameters.
In accordance with hospital policies regarding
procedural anesthesia, fasting status was confirmed, and a 20-gauge
peripheral IV catheter was placed in the right forearm without
subcutaneous local anesthesia following the arrival of patients to
the Digestive Endoscopy Center of Renmin Hospital of Wuhan
University. Lactated Ringer's solution (Baxter International Inc.,
Deerfield, IL, USA) was infused, and routine monitoring consisting
of a 5-lead electrocardiography (ECG), non-invasive blood pressure,
pulse oxygen saturation (SpO2) and bispectral index
(BIS; Monitor Model A-2000; Aspect Medical Systems, Inc., Norwood,
MA, USA). The mean of the final 3 vital signs obtained prior to the
injection of anesthetics was recorded as the baseline in all
patients. After lying on the examination table in the left lateral
position, each patient was provided oxygen (5 l/min) via a face
mask and instructed to take deep breathes to increase their oxygen
reserves.
All patients received intravenous (i.v.) 1 µg/kg
fentanyl at 5–10 sec prior to gastroscopy. Prior to endoscopy,
patients were randomized to one of four groups using a
computer-generated random numbers table, which allocated 50
patients to each group. Patients in the propofol group (P) received
i.v. propofol at an induction dose of 1.5–2.0 mg.kg−1
over a 1 min period using a computer controlled infusion pump
(Syringe Infusion Pump Model compact; B. Braun Melsungen AG,
Melsungen, Germany), followed by a maintenance infusion of 4
mg.kg−1.h−1 during the gastroscopy procedure.
Patients in the etomidate group (E) received i.v. etomidate at an
induction dose of 0.15-0.2 mg/kg over 1 min using the same infusion
pump, followed by a maintenance infusion of 0.4
µg.kg−1.h−1 during the gastroscopy procedure.
Patients in the propofol and etomidate group (P+E) received
propofol (0.75–1 mg/kg) over a 30 sec period and subsequently
etomidate (0.075-0.1 mg/kg) over a 30 sec period using the same
infusion pump, followed by a maintenance infusion of 2
mg.kg−1.h−1 propofol and 0.2
µg.kg−1.h−1 etomidate simultaneously during
the gastroscopy procedure via a three-way joint. Patients in the
etomidate and propofol group (E+P) received etomidate (0.075-0.01
mg/kg) over a 30-sec period and subsequently propofol (0.75-1
mg/kg) over a 30 sec period via the same infusion pump, followed by
a maintenance infusion of 2 mg.kg−1.h−1
propofol and 0.2 µg.kg−1.h−1 etomidate during
the gastroscopy procedure via a three-way joint.
Gastroscopy was performed when eyelash reflexes
disappeared. The gastroscopy was performed with patients in a left
lateral position, using a side-viewing video duodenoscope (Olympus
Optical Co., Ltd., Tokyo, Japan). An anesthetist was in attendance
during all procedures. Spontaneous respiration was maintained
during the course of gastroscopy.
Observed parameters
A 5-lead ECG was performed throughout the
gastroscopy. In addition, reductions in SpO2, changes in
heart rate (HR) and blood pressure (BP), ST segment deviations,
arrhythmias and conduction defects were recorded throughout the
procedure. Vital signs were recorded at T0 (baseline, prior to
induction of anesthesia), T1 (2 min after induction of anesthesia),
T2 (4 min after induction of anesthesia), T3 (6 min after induction
of anesthesia), T4 (8 min after induction of anesthesia), T5 (10
min after induction of anesthesia), T6 (15 min after induction of
anesthesia) and T7 (20 min after induction of anesthesia).
Patients were assessed at the following time points
for various complications: i) Start of anesthesia (first drug
bolus); ii) start of examination (gastroscopy placement); iii)
completion of the examination (removal of the gastroscopy); iv)
‘induction time’ (start of anesthesia to start of examination); v)
‘inspection time’ (gastroscopy insertion to gastroscopy removal);
vi) ‘recovery time’ (the time between the gastroscopy removal and
the start of the final psychometric assessment); and vii)
‘discharge time’ (the time between gastroscopy removal and
departure from the endoscopy unit). The criteria for discharge from
the endoscopy unit were as follows: Fully awake with stable
hemodynamics; no evidence of respiratory depression; no nausea or
vomiting; and ability to drink water safely.
Rate pressure product (RPP) and pressure-rate
quotient (PRQ) (12), which are two
indices that reflect myocardial oxygen consumption, were calculated
following the examination as follows: RPP = systolic blood pressure
(SBP) × heart rate (HR) / 1,000; PRQ = mean arterial pressure /
HR.
Adverse events, the use of ventilator support,
including support of the oral or nasopharyngeal airways, and the
administration of pressors and chronotropic agents were recorded.
Bradycardia was defined as a heart rate <50 beats per minute
(bpm). Hypotension was defined as a systolic pressure <70%
baseline or <80 mmHg. Side effects, including PONV, swallowing,
body movement (limb locomotor activity with no influence on
gastroscopy), serious body movements (resulting in suspension of
the examination), apnea (interval time of respiration, >30 sec),
hypoxemia (SpO2,<90%), myoclonus (involuntary and
brief twitching of a group of muscles) and injection pain, were
recorded.
At the end of the procedure, the satisfaction of the
anesthetist and gastroenterologist were evaluated according to the
visual analogue scale (13) (VAS
scores; 0 = no satisfaction and 10 = most satisfaction). A
questionnaire, which inquired about i) overall satisfaction with
the anesthesia, ii) difficulty of anesthesia, iii) patient
cooperation, and iv) overall satisfaction with the gastroscopy
procedure, was used.
Prior to discharge, patient satisfaction was
evaluated by completing an anonymous and confidential Patient
Satisfaction Questionnaire, modified from Sipe (14), to evaluate the endoscopy
experience.
Safety equipment
Vital signs were monitored for 2 h after the
completion of the examination. The incidence of the following
cardiorespiratory events were recorded: Bradycardia; respiratory
depression (RR; <9 breaths/min); apnea; hypertension (BP >30%
baseline); and hypotension (BP <30% baseline). Intervention,
including the administration of fluid, pressors, or the use of an
anticholinergic agents, was applied for any adverse events.
Mask-assisted ventilation was performed if SpO2 <90%
remained for 30 sec. Additionally, any events resulting in
mortality, permanent impairment, hospitalization and/or medical or
surgical intervention were recorded.
Statistical analysis
Data are presented as the mean ± standard deviation,
and medians. GraphPad Prism version 5.0 (GraphPad Software, Inc.,
San Diego, CA, USA) was used to analyze the results. One-way
analysis of variance was performed to examine differences among the
four groups with respect to parametric variables, followed by
Tukey's post hoc test. Incidences of complications were analyzed
using the χ2 or Fisher's exact test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Combined use of propofol and etomidate
reduces recovery and discharge times, as compared with etomidate
alone
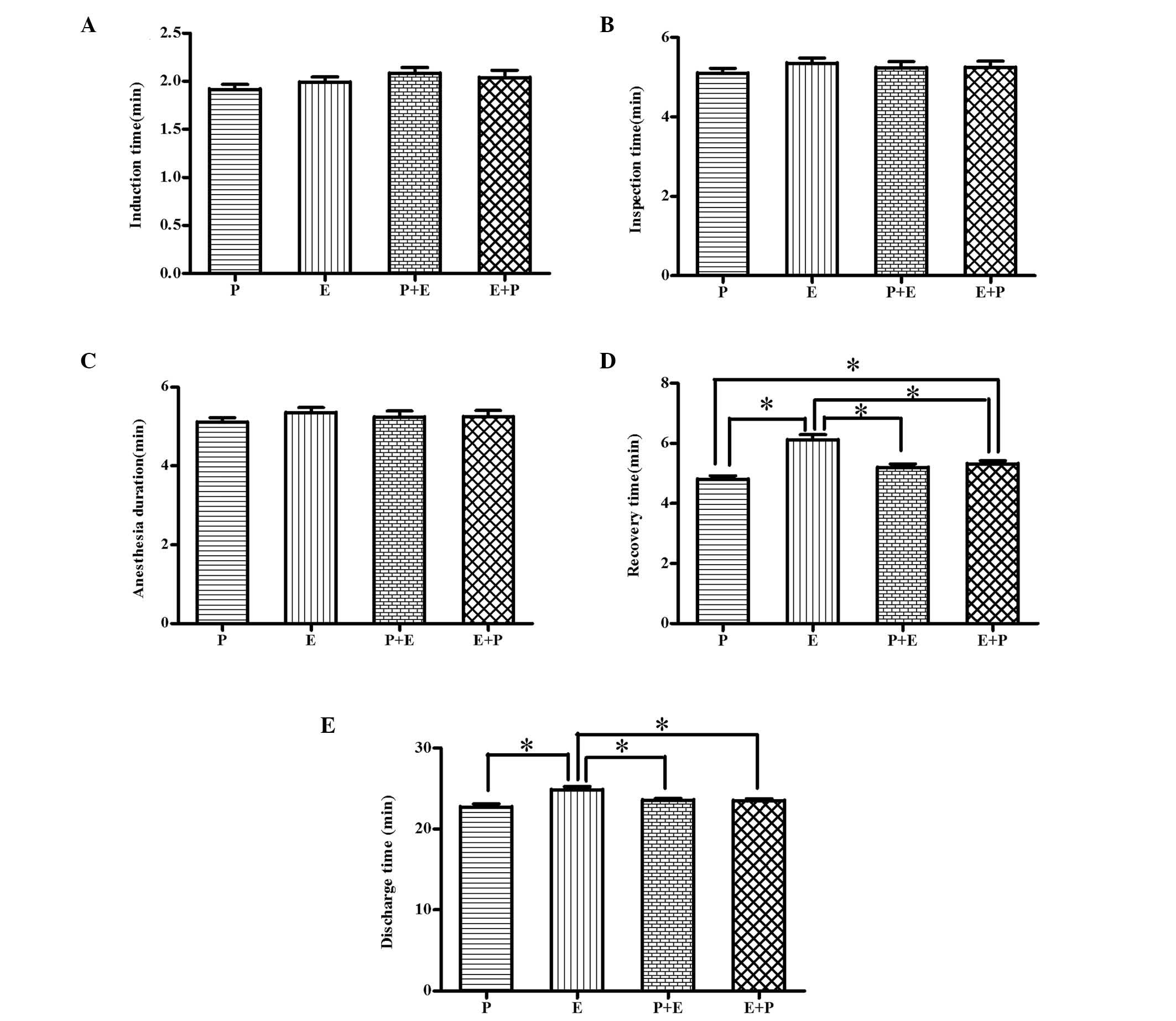
A total of 253 patients were assessed for study
eligibility; 35 patients did not meet the inclusion criteria, 15
patients declined to participate and 3 patients were excluded for
other reasons (Fig. 1). In total,
200 patients were included in the study (97 males and 103 females;
age range, 65–82 years). The four groups had similar demographic
data (P>0.05; Table I) and BIS
(P>0.05; Table I). The induction
time, inspection time and anesthesia duration were not different
between the four groups (P>0.05; Fig.
2). The recovery (6.1±1.2 h) and discharge times (24.8±2.8 h)
in group E were longer compared with group P (4.8±0.9 h and
22.7±2.8 h, respectively), group P+E (5.2±0.9 h and 23.6±1.4 h,
respectively) and group E+P (5.3±0.8 h and 23.5±1.8 h,
respectively) (P<0.05; Fig. 2).
No gastroscopy procedure was terminated because of inadequate
patient anesthesia.
 | Table I.Patient demographics. |
Table I.
Patient demographics.
|
| Group |
|---|
|
|
|
|---|
| Parameter | P | E | P+E | E+P |
|---|
| Median age (range),
years | 68.4 (65–78) | 69.7 (65–80) | 72.3 (65–79) | 71.8 (65–82) |
| Gender,
male/female | 24/26 | 25/25 | 24/26 | 24/26 |
| Median weight
(range), kg | 60.7 (50–84) | 62.4 (52–82) | 62.6 (47–85) | 61.8 (49–84) |
Etomidate improves hemodynamic
stability, as compared with propofol
A decrease in BP >30% from the baseline occurred
in 62 patients across all groups (Table
II). There was a decrease in SBP from the baseline in all
patients at T1, and there was a significant difference in the
incidence of hypotension in group P, as compared with the other
three groups (88%; P<0.05; Fig.
3). In addition, there were statistically significant
differences in SBP in group P at T1, as compared with the other
three groups (P<0.05; Fig. 3),
and there were significant differences in SBP at T0 compared with
T1, T2, T3, T4, T5 and T6 in group P (P<0.05; Fig. 3). Furthermore, there was a
significant difference in SBP at T0 compared with T1, T2, T3, T4
and T5 in groups E, P+E and E+P (P<0.05; Fig. 3). Moreover, in groups E, P+E and E+P,
there was a significant difference in SBP at T1 (132.08±6.56,
129.56±6.58 and 131.20±5.93 mmHg, respectively) compared with T6
(151.28±5.73, 150.72±5.79 and 152.16±6.65 mmHg, respectively) and
T7 (157.44±5.36, 154.36±8.04 and 158.68±5.71 mmHg, respectively)
(P<0.05; Fig. 3). The results for
the other three groups showed improved hemodynamic stability
compared with group P (P<0.05, Fig.
3). There were no significant differences in the mean and
maximum HR during gastroscopy in different groups (P>0.05,
Fig. 3). It has been suggested that
RPP ≥12 indicates myocardial ischemia (12), and that RPP ≥20 is a threshold for
angina pectoris; PRQ <1.0 is considered to be an accurate
measure of myocardial ischemia. In the present study, 1 patient had
a very high RPP (>20), and 2 patients had PRQ <1.0, in group
P.
 | Figure 3.Mean (A) SBP, (B) DBP and (C) HR
levels of the four study groups (n=50) during gastroscopy. Data are
presented as the mean ± standard deviation. There was a significant
difference between SBP in group P at T1 compared with T0
(P<0.05), and there were significant differences in SBP at T0
compared with SBP at T1, T2, T3, T4, T5 and T6 in group P
(P<0.05). In addition, there were significant differences in SBP
at T0 compared with T1, T2, T3, T4 and T5 in groups E, P+E and E+P
(P<0.05). Furthermore, there were significant differences in SBP
at T1 compared with T6 and T7 in groups E, P+E and E+P (P<0.05).
However, there were no significant differences in HR in any groups
(P>0.05). SBP, systolic blood pressure; DBP, diastolic blood
pressure; HR, heart rate; P, propofol (1.5–2.0 mg/kg); E, etomidate
(0.15-0.2 mg/kg); P+E, propofol (0.75–1 mg/kg) followed by
etomidate (0.075-0.1 mg/kg); E+P, etomidate (0.075-0.01 mg/kg)
followed by propofol (0.75–1 mg/kg). |
 | Table II.Complications of the four study
groups (n=50). |
Table II.
Complications of the four study
groups (n=50).
|
| Group |
|---|
|
|
|
|---|
| Parameter | P | E | P+E | E+P |
|---|
| Hypotension | 44 (88) | 6
(12)a | 6
(12)a | 6
(12)a |
| ST segment
depression | 10 (20) | 3 (6)a | 4 (8)a | 3 (6)a |
| Transient atrial
fibrillation | 2 (4) | 0 (0) | 0 (0) | 1 (2) |
| Sinus
bradycardia | 5
(10) | 6
(12) | 5
(10) | 4 (8) |
| Ventricular
premature complexes | 1 (2) | 0 (0) | 0 (0) | 1 (2) |
| SpO2
<95% | 12 (24) | 2 (4)a | 3 (6)a | 3 (6)a |
| SpO2
<90% | 4 (8) | 0 (0)a | 0 (0)a | 0 (0)a |
| Apnea | 21 (42) | 7
(14)a | 3 (6)a | 3 (6)a |
| Mask assisted
ventilation | 4 (8) | 1 (2)a | 1 (2)a | 1 (2)a |
| Body movements | 13 (26) | 18 (36) | 5
(10)b | 6
(12)b |
| Body movements,
general | 12 (24) | 18 (36) | 5
(10) | 6
(12) |
| Body movements,
serious | 1 (2) | 0 (0) | 0 (0) | 0 (0) |
| Myoclonus | 1 (2) | 15
(30)a | 2 (4) | 3 (6) |
| Injection pain | 32 (64) | 3 (6)a | 10
(20)a,b | 3 (6)a |
| PONV | 4 (8) | 7
(14)a | 5
(10) | 6
(12) |
Combined use of propofol and etomidate
causes minimal respiratory depression and few side effects
The incidences of complications resulting from
gastroscopy are presented in Table
II. No serious complication occurred during the study.
Transient hypoxia (SpO2, <90% for >30 sec)
requiring supplemental oxygen by mask-assisted ventilation occurred
in 7 patients across all groups (Table
II). All episodes of hypotension and bradycardia were
transient, and the administration of a pharmacologic agent or other
therapeutic intervention was not required to treat any of the
patients. No perforations or mortality occurred, and following the
procedure, no patient required assisted ventilation or was admitted
to hospital.
The occurrence of apnea during and following
gastroscopy was 17% (34); 2% of these patients had SpO2
<90%, and 2.5% of the patients reported accessing mask-assisted
ventilation in the endoscopy unit. The occurrence of
SpO2 <95% (24%), SpO2 <90% (8%), apnea
(42%) and mask-assisted ventilation (8%) in group P were
significant higher compared with groups E (4, 0, 14 and 2%,
respectively), P+E (6, 0, 6 and 2%, respectively) and E+P (6, 0, 6
and 2%, respectively) (P<0.05; Table
II). There were no significant differences in the occurrence of
SpO2 <95%, SpO2 <90%, apnea, and
mask-assisted ventilation when comparing groups E, P+E and E+P
(P>0.05; Table II).
ECG changes during and following gastroscopy
occurred in 22.5% of all procedures. In group P, related transient
ECG changes included ST segment depression (20%), transient atrial
fibrillation (4%), sinus bradycardia (10%) and ventricular
premature complexes (2%). In group E, sinus bradycardia occurred in
12% of procedures and ST segment changes occurred in 6% of
patients. In group P+E, the occurrence of bradycardia was 10%, and
ST segment changes occurred in 8% of patients. In the E+P group,
sinus bradycardia occurred in 8% and ST changes occurred in 6% of
patients. The difference in the incidence of arrhythmia and
ischemic changes between the four groups was not significant
(P>0.05; Table II).
The occurrence of myoclonus during and following
gastroscopy with anesthesia in group E (30%) was significantly
higher compared with groups P (2%), P+E (4%) and E+P (6%)
(P<0.05). The occurrence of injection pain during and following
gastroscopy in group P (64%) was significantly higher compared with
groups E (6%), P+E (20%) and E+P (6%) (P<0.05). The occurrence
of injection pain in group P+E was significant higher compared with
groups E and E+P (P<0.05). There were no statistical differences
between groups P and E with regards to the occurrence of body
movements (P>0.05; Table II).
One patient moved significantly enough to require suspension of the
gastroscopy while additional propofol was given. The occurrence of
body movements significantly decreased using propofol and etomidate
together, regardless of which drug was administered first
(P<0.05; Table II). Body
movements occurred in 42 patients (21%), the majority of which were
general body movements (97.6%). The incidence of PONV in group E
(14%) was significantly higher compared with group P (8%)
(P<0.05; Table II). There was no
statistical difference in the incidence of PONV between groups P,
P+E and E+P.
Combination of propofol and etomidate
increases patient satisfaction following a gastroscopy, as compared
with using either agent alone
Patient evaluation of the gastroscopy is presented
in Table III. The immediate
post-procedure questionnaire was completed by all patients. In
group P, 90% of patients described their overall satisfaction with
the anesthesia as ‘excellent’ and 10% rated it ‘good’ when asked to
rate the degree of pain or discomfort experienced during the
endoscopy. Meanwhile, in group E, 80% of patients described overall
satisfaction as ‘excellent’, 12% described it as ‘good’ and 8% of
patients described it as ‘fair’. In the P+E and E+P groups, overall
satisfaction was rated as excellent in 90 and 92% of patients,
respectively, which is significantly increased compared with groups
P and E (P>0.05; Table
III).
 | Table III.Patient satisfaction surveys of four
study groups (n=50). |
Table III.
Patient satisfaction surveys of four
study groups (n=50).
| Question and
response (n=50) | P | E | P+E | E+P |
|---|
| How much discomfort
or pain did you feel? |
|
|
|
|
|
None | 40 (80) | 36 (72) | 40 (80) | 39 (78) |
|
Mild | 8 (16) | 12 (24) | 9 (18) | 10 (20) |
|
Moderate | 2 (4) | 2 (4) | 1 (2) | 1 (2) |
|
Severe | 0 | 0 | 0 | 0 |
| Rate the level of
sedation received during the endoscopic exam |
|
|
|
|
|
Adequate | 45 (90) | 46 (92) | 50 (100) | 50 (100) |
| Too
little | 4 (8) | 3 (6) | 0 | 0 |
| Too
much | 1 (2) | 1 (2) | 0 | 0 |
| Rate your overall
satisfaction with the endoscopic sedation |
|
|
|
|
|
Excellent | 45 (90) | 40 (80) | 45 (90) | 46 (92) |
|
Good | 5 (10) | 6 (12) | 4 (8) | 3 (6) |
|
Fair | 0 | 4 (8) | 1 (2) | 1 (2) |
|
Poor | 0 | 0 | 0 | 0 |
| Did you require
additional sleep during the day after your procedure? |
|
|
|
|
|
Yes | 14 (28) | 16 (32) | 12 (24) | 11 (22) |
| No | 36 (72) | 34 (68) | 38 (76) | 39 (78) |
| How much sleep did
you require? |
|
|
|
|
|
None | 36 (72) | 34 (68) | 38 (76) | 39 (78) |
| <2
h | 9 (18) | 11 (22) | 9 (18) | 8 (18) |
| 2–4
h | 4 (8) | 4 (8) | 3 (8) | 3 (8) |
| 4–6
h | 1 (2) | 1 (2) | 0 (0) | 0 (0) |
| When did you resume
your normal daily activities? |
|
|
|
|
| <2
h | 35 (70) | 36 (72) | 40 (80) | 41 (82) |
| 2–4
h | 9 (18) | 8 (16) | 5 (10) | 4 (8) |
| 4–6
h | 3 (6) | 3 (6) | 2 (4) | 2 (4) |
| >6
h | 3 (6) | 2 (4) | 3 (6) | 3 (6) |
In group P, 80% of patients reported no discomfort,
16% described discomfort as mild, and 4% described discomfort as
moderate; 90% of patients rated the level of anesthesia as
‘adequate’, 8% believed that they received ‘too little’, and 2%
stated that they were given ‘too much’. In group E, 72% of patients
reported no discomfort, 24% described discomfort as mild and 4%
described discomfort as moderate; 92% of patients rated the level
of anesthesia as ‘adequate’, 6% believed that they received ‘too
little’ and 2% stated that they were given ‘too much’. In groups
P+E and E+P, 80 and 78% reported no discomfort, respectively, 18
and 20% described discomfort as mild, respectively, and 2% in both
groups described discomfort as moderate. All patients rated the
level of anesthesia as ‘adequate’ when asked to rate the level of
anesthesia during the endoscopy following co-administration of
propofol and etomidate (P>0.05; Table III).
Combination of propofol and etomidate provides
Although the survey was conducted 24 h after discharge, it was
shown that different proportions of patients in the four groups
returned to normal activities within 2 h of discharge. Group P
patients required ≥4 h before resumption of activities, although
the majority of patients did not require additional sleep following
discharge from the endoscopy unit. There were no statistical
differences between group P and the other three groups with regard
to the patients' immediate and post-procedure satisfaction
(P>0.05; Table III). Finally,
in the present study, a combination of propofol and etomidate
provided better satisfaction of endoscopists (P<0.05) and
anesthetists (P<0.01) compared with using propofol alone
(Fig. 4).
Discussion
The results of the present study demonstrate that
there is improved hemodynamic stability and minimal respiratory
depression in elderly patients when propofol is used in combination
with etomidate, instead of either agent used alone, for anesthesia
during gastroscopy. Co-administration of propofol and etomidate has
a favorable side effect profile, allows rapid recovery to full
activity and provides high levels of satisfaction.
Gastroscopy is a non-traumatic invasive procedure
used for the diagnosis of gastrointestinal pathology and for
treatment for gastrointestinal hemorrhage, polypus and corpus
alienum (3). Elderly patients
experience specific physiological changes of organs and cell
functions (15,16), and it is important to understand how
to maintain hemodynamic stability and adequate spontaneous
respiration during gastroscopy procedures in such patients.
Gastroscopy is frequently performed with anesthesia for the comfort
of the patient. Elderly patients requiring gastroscopy frequently
have cardiovascular disease and other co-morbidities, which results
in difficulties in safely administering anesthesia while
maintaining stable hemodynamics. The features of gastroscopy
examination require that the anesthetic regimen provides rapid
induction, sufficient anesthesia, hemodynamic stability, quick
recovery and minimal side effects.
Propofol is the most frequently used i.v. anesthetic
to date due to its rapid recovery profile, and it has been widely
used for anesthesia in outpatients (8,9).
However, propofol causes marked depression on hemodynamic and
respiratory parameters. Hypotension is a common side effect
associated with propofol due to vasodilatation and negative
inotropic effects (11). An
induction dose of propofol results in a 25–30% incidence of apnea
and a 25–40% reduction in systolic blood pressure (9,10). The
high incidence of apnea, lasting longer than 30 sec, exposes
patients to the potential risks of brain damage, which is the
leading cause of morbidity in anesthesia-related events (17). In the present study, elderly patients
induced with propofol experienced a 42% incidence of apnea, and 88%
of patients experienced a significant (>30%) reduction in
systolic blood pressure. This may be related to diminished
myocardial contractility, decreased cardiac output, reduced ability
of the cardiovascular system to respond to stress and preoperative
routine fasting. In contrast, etomidate is associated with
hemodynamic stability and minimal respiratory depression, which are
unique characteristics among rapid-onset induction agents (11,18).
These properties differentiate etomidate from other rapid-onset
induction agents, as it has a wider margin of safety than propofol,
particularly in patients with valvular heart disease, myocardial
ischemia and elderly patients. The results in the current study
demonstrated that there was a 14% incidence of apnea and a 12%
incidence of hypotension following the use of etomidate. It is
important to note that there is a significantly decrease in the
incidence of apnea (6%), and a 12% incidence of hypotension, when
using propofol and etomidate together.
Cardiopulmonary complications in elderly patients
have been evaluated during gastroscopy. Elderly patients who
undergo gastroscopy may be at risk of developing cardiopulmonary
complications resulting from preexisting cardiovascular diseases,
the sympathetic response when the gastroscope is inserted through
the throat, and prolonged procedure time (5,6,19,20). In
addition, elderly patients may be more susceptible to silent
myocardial ischemia. The high incidence of ST segment depression in
group P (20%) in the present study may be related to the reduction
in blood pressure resulting from an induction dose of propofol.
Although 1 patient developed a very high RPP (>20), and 2
patients experienced PRQ <1.0, it is not sufficient to conclude
that standard-dose propofol monotherapy exposes patients to a high
risk of myocardial ischemia. In the current study, there were no
differences in the incidence of transient atrial fibrillation,
sinus bradycardia and ventricular premature complexes, which
indicate that temporary short periods of fluctuations in blood
pressure have little effect on the cardiac conduction system.
Propofol is a potent hypnotic agent that can cause life-threatening
side effects, including the loss of protective airway reflexes and
respiratory depression (17,21). In the present study, it was observed
that 8% of elderly patients in group P required short-term positive
pressure ventilation, while 2% of elderly patients in the other
three groups required this intervention. This result demonstrates
that etomidate has unique characteristics which allow it to be used
alone or in combination with propofol for anesthesia. In addition,
the results show that a combination of etomidate and propofol can
result in favorable hemodynamic stability and preserve spontaneous
respirations during anesthesia for gastroscopy.
Etomidate has rarely been used in outpatient
operations and during examination due to side effects, such as
myoclonus and PONV. Etomidate has been observed to be associated
with a high (30–40%) incidence of PONV, and the incidence of
myoclonus following etomidate use is highly variable (0–70%)
(22,23), which is higher than propofol
(22). In the present study, the
incidence of myoclonus, PONV and injection pain when etomidate
combined with propofol was used and injected in different
sequences, was investigated. The results demonstrate that the
incidences of PONV and myoclonus in group E (14 and 30%,
respectively) are higher compared with group P (8 and 2%), and are
reduced by combined use with propofol (10 and 12% PONV in groups
P+E and E+P, respectively; 4 and 6% myoclonus in groups P+E and
E+P, respectively). In addition, the current study observed a
decreased incidence of injection pain following the combined use of
propofol and etomidate. All of the results demonstrate that the
combined use of propofol and etomidate results in reducedside
effects, including myoclonus, injection pain and PONV, in elderly
patients undergoing gastroscopy. Furthermore, the present study
demonstrated that the combined use of propofol and etomidate for
endoscopic anesthesia, alone or in combination, results in high
levels of patient satisfaction.
In the present study, it was anticipated that a
short recovery time would be accompanied by a rapid recovery to
full activity. In telephone surveys conducted 24 h after discharge
in the current study, it was reported that 72% of patients did not
require additional sleep following discharge, and that 70% resumed
normal activities within 2 h of departure from the endoscopy unit
when propofol monotherapy was used, which is in agreement with the
other results (8). The novel finding
of the present study revealed that 76 and 78% of patients in groups
P+E and E+P, respectively, did not require additional sleep
following discharge, and that 80 and 82% of patients in groups P+E
and E+P, respectively, resumed normal activities within 2 h of
departure from the endoscopy unit. This demonstrates that the
combined use of propofol and etomidate can result in a rapid return
to full activity for elderly patients following gastroscopy.
The present study is subject to a number of
limitations. Firstly, the current study is not a multi-center
study; further research should be conducted at multiple sites.
Although the study supports the hypothesis that the combined use of
etomidate and propofol reduces the side effects of etomidate and
propofol with minimal effects on safety and recovery, a larger
trial that is sufficient to detect differences is needed to confirm
these findings before a change in clinical practice is recommended.
Secondly, although plasma corticosteroid concentrations were not
recorded in the current study, a number of studies have
demonstrated that the induction dose of etomidate can decrease
plasma corticosteroid concentrations, and that this can be
sustained for 6–8 h, leading to adrenocortical dysfunction
(24–26). Thirdly, only the short-term
hemodynamic effects on elderly patients were investigated. Although
no significant difference was identified in the mortality and
hospitalization among patients who received propofol or etomidate,
it can not determine whether there is any effect on mortality or
other aspects of clinical outcome.
In conclusion, the present study demonstrates that
anesthesia for gastroscopy in elderly patients can be safely and
effectively accomplished when propofol combined with etomidate is
used. It is understood that these anesthetic regimens have unique
characteristics, including improved hemodynamic stability, minimal
respiratory depression, reduced side effects, a rapid return to
full activity and high levels of satisfaction.
Acknowledgements
The authors thank patients and their families for
their inclusion in the present study.
References
|
1
|
Cao H, Wang B, Zhang Z, Zhang H and Qu R:
Distribution trends of gastric polyps: An endoscopy database
analysis of 24 121 northern Chinese patients. J Gastroenterol
Hepatol. 27:1175–1180. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Travis AC, Pievsky D and Saltzman JR:
Endoscopy in the elderly. Am J Gastroenterol. 107:1495–1501. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ristikankare M, Julkunen R, Heikkinen M,
Mattila M, Laitinen T, Wang SX and Hartikainen J: Sedation, topical
pharyngeal anesthesia and cardiorespiratory safety during
gastroscopy. J Clin Gastroenterol. 40:899–905. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fanti L, Agostoni M, Arcidiacono PG,
Albertin A, Strini G, Carrara S, Guslandi M, Torri G and Testoni
PA: Target-controlled infusion during monitored anesthesia care in
patients undergoing EUS: Propofol alone versus midazolam plus
propofol. A prospective double-blind randomised controlled trial.
Dig Liver Dis. 39:81–86. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seinelä L, Reinikainen P and Ahvenainen J:
Effect of upper gastrointestinal endoscopy on cardiopulmonary
changes in very old patients. Arch Gerontol Geriatr. 37:25–32.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cha JM, Jeun JW, Pack KM, Lee JI, Joo KR,
Shin HP and Shin WC: Risk of sedation for diagnostic
esophagogastroduodenoscopy in obstructive sleep apnea patients.
World J Gastroenterol. 19:4745–4751. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yetkin G, Oba S, Uludag M, Paksoy I, Akgün
I and Eren N: Effects of sedation during upper gastrointestinal
endoscopy on endocrine response and cardiorespiratory function.
Braz J Med Biol Res. 40:1647–1652. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cohen LB, Delegge MH, Aisenberg J, Brill
JV, Inadomi JM, Kochman ML and Piorkowski JD Jr: AGA Institute: AGA
institute review of endoscopic sedation. Gastroenterology.
133:675–701. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kitagawa N, Katoku M, Kasahara T, Tsuruta
T, Oda M and Totoki T: Does atropine reduce the risk of
propofol-induced cardiovascular depression? Anesth Analg.
103:1606–1608. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Olofsen E, Boom M, Nieuwenhuijs D, Sarton
E, Teppema L, Aarts L and Dahan A: Modeling the non-steady state
respiratory effects of remifentanil in awake and propofol-sedated
healthy volunteers. Anesthesiology. 112:1382–1395. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Morel J, Salard M, Castelain C, Bayon MC,
Lambert P, Vola M, Auboyer C and Molliex S: Haemodynamic
consequences of etomidate administration in elective cardiac
surgery: A randomized double-blinded study. Br J Anaesth.
107:503–509. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fisher L, Fisher A and Thomson A:
Cardiopulmonary complications of ERCP in older patients.
Gastrointest Endosc. 63:948–955. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Berzin TM, Sanaka S, Barnett SR, Sundar E,
Sepe PS, Jakubowski M, Pleskow DK, Chuttani R and Sawhney MS: A
prospective assessment of sedation-related adverse events and
patient and endoscopist satisfaction in ERCP with
anesthesiologist-administered sedation. Gastrointest Endosc.
73:710–717. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sipe BW, Rex DK, Latinovich D, Overley C,
Kinser K, Bratcher L and Kareken D: Propofol versus
midazolam/meperidine for outpatient colonoscopy: Administration by
nurses supervised by endoscopists. Gastrointest Endosc. 55:815–825.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Klotz U: Pharmacokinetics and drug
metabolism in the elderly. Drug Metab Rev. 41:67–76. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Triantafillidis JK, Merikas E, Nikolakis D
and Papalois AE: Sedation in gastrointestinal endoscopy: Current
issues. World J Gastroenterol. 19:463–481. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang D, Chen C, Chen J, Xu Y, Wang L, Zhu
Z, Deng D, Chen J, Long A, Tang D and Liu J: The use of propofol as
a sedative agent in gastrointestinal endoscopy: A meta-analysis.
PLoS One. 8:e533112013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Morel J, Salard M, Castelain C, Bayon MC,
Lambert P, Vola M, Auboyer C and Molliex S: Haemodynamic
consequences of etomidate administration in elective cardiac
surgery: A randomized double-blinded study. Br J Anaesth.
107:503–509. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ross R and Newton JL: Heart rate and blood
pressure changes during gastroscopy in healthy older subjects.
Gerontology. 50:182–186. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gangi S, Saidi F, Patel K, Johnstone B,
Jaeger J and Shine D: Cardiovascular complications after GI
endoscopy: Occurrence and risks in a large hospital system.
Gastrointest Endosc. 60:679–685. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Oberer C, von Ungern-Sternberg BS, Frei FJ
and Erb TO: Respiratory reflex responses of the larynx differ
between sevoflurane and propofol in pediatric patients.
Anesthesiology. 103:1142–1148. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu J, Yao S, Wu Z, Wu Z, Chu S, Xia G and
Deng F: A comparison of anesthetic regimens using etomidate and
propofol in patients undergoing first-trimester abortions:
Double-blind, randomized clinical trial of safety and efficacy.
Contraception. 87:55–62. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mizrak A, Koruk S, Bilgi M, Kocamer B,
Erkutlu I, Ganidagli S and Oner U: Pretreatment with
dexmedetomidine or thiopental decreases myoclonus after etomidate:
A randomized, double-blind controlled trial. J Surg Res.
159:e11–e16. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Schenarts CL, Burton JH and Riker RR:
Adrenocortical dysfunction following etomidate induction in
emergency department patients. Acad Emerg Med. 8:1–7. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Absalom A, Pledger D and Kong A:
Adrenocortical function in critically ill patients 24 h after a
single dose of etomidate. Anaesthesia. 54:861–867. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang N, Wang XH, Lu J and Zhang JY: The
effect of repeated etomidate anesthesia on adrenocortical function
during a course of electroconvulsive therapy. J ECT. 27:281–285.
2011. View Article : Google Scholar : PubMed/NCBI
|