Introduction
Phthiriasis palpebrarum is a rare eyelid infestation
caused by Phthiriasis pubis, commonly known as crab lice
(1). Although their primary habitat
is pubic hair, these lice are often found on the hair of the
abdomen, thighs and the axilla, and occasionally they may invade
the eyebrows and eyelashes (2). Lice
may be transferred from one hair-bearing area to another, and any
hair-bearing area may become infested (3). Sexual contact and parent-child
interactions are the most typical routes of infestation and
transfer occurs more often in this manner than through shared
towels, sheets or clothes (4).
Phthiriasis pubis infestation affects 1–2% of the human
population worldwide (5) and is
generally associated with poor hygiene and overcrowding (6). Infestations are most prevalent in
sexually active patients from 15 to 45 years old (7). In the present study, a case of lateral
phthiriasis palpebrarum is reported. The patient provided written
informed consent with regard to her data and images being included
in the present case report.
Case report
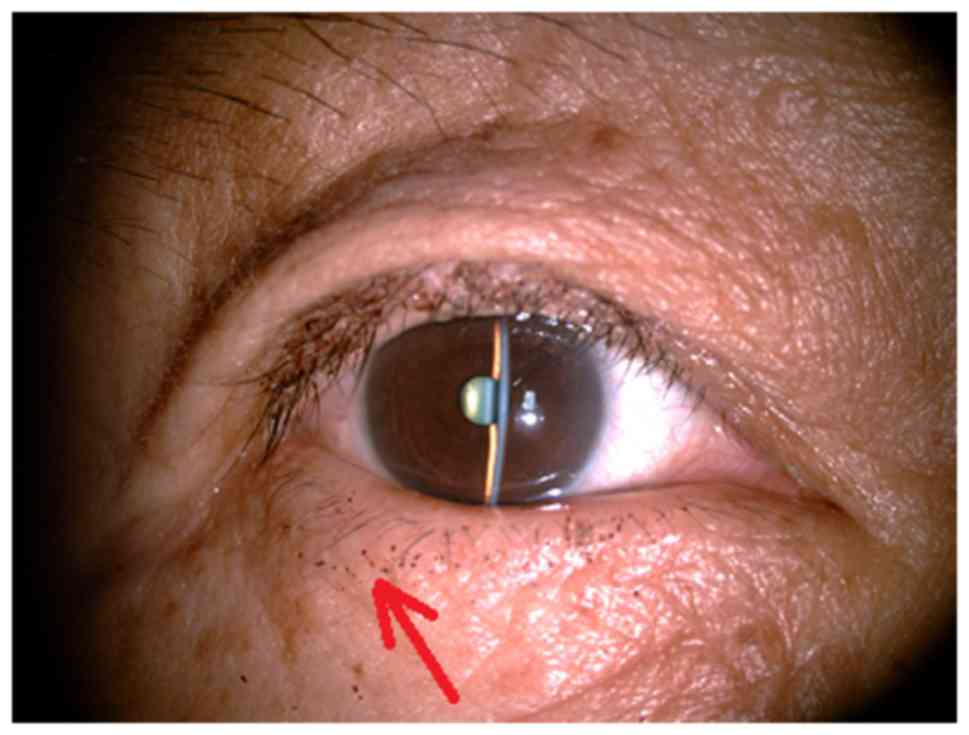
A 63-year-old woman visited the Department of
Ophthalmology, Tianjin First Center Hospital (Tianjin, China) on
June 17, 2015, presenting with a 2-month history of repeated
episodes of itching and burning sensations and moderate pain in
both eyes. The patient had visited another hospital 1 month
previously, where a diagnosis of common anterior blepharitis was
made and she was prescribed a combination of Levofloxacin
antibiotic eye drops and corticosteroid eye drops; however, her
symptoms had not improved. On examination, corrected visual acuity
was observed to be 20/20 in both eyes and intraocular pressure was
14 mmHg in the right eye and 13 mmHg in the left eye. A slit lamp
examination was performed, which revealed >10 adult crab-like
lice, and multiple red pinpoint excretions (Fig. 1). Mild hyperemia and excoriation was
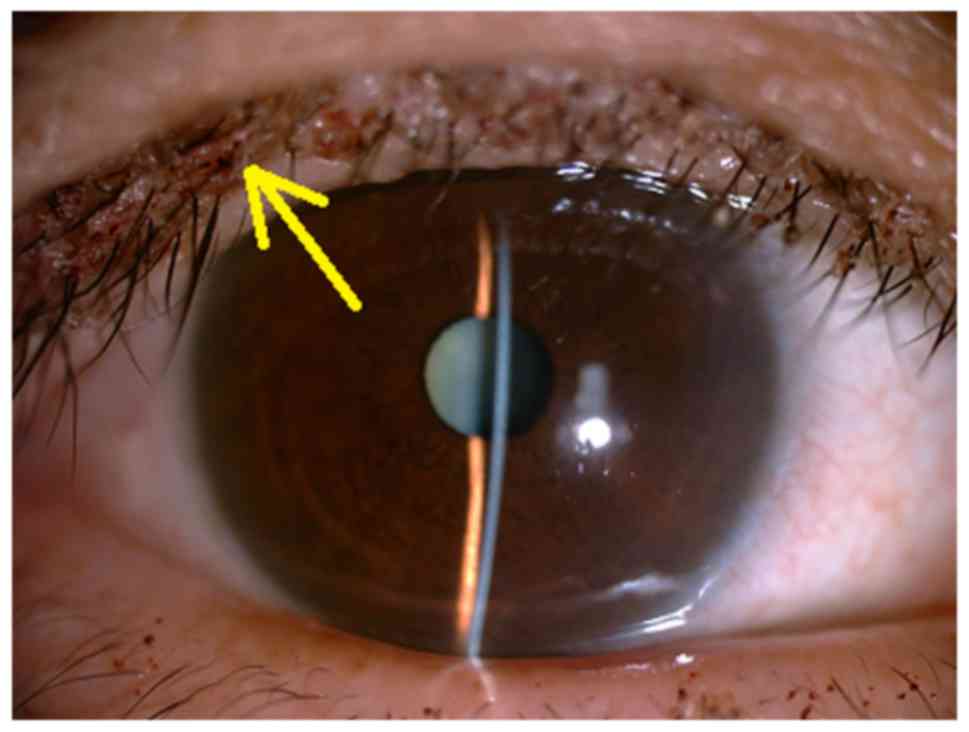
observed at the outer margin of the left upper eyelid, and brownish
scales, which are indicative of louse feces, were present in the
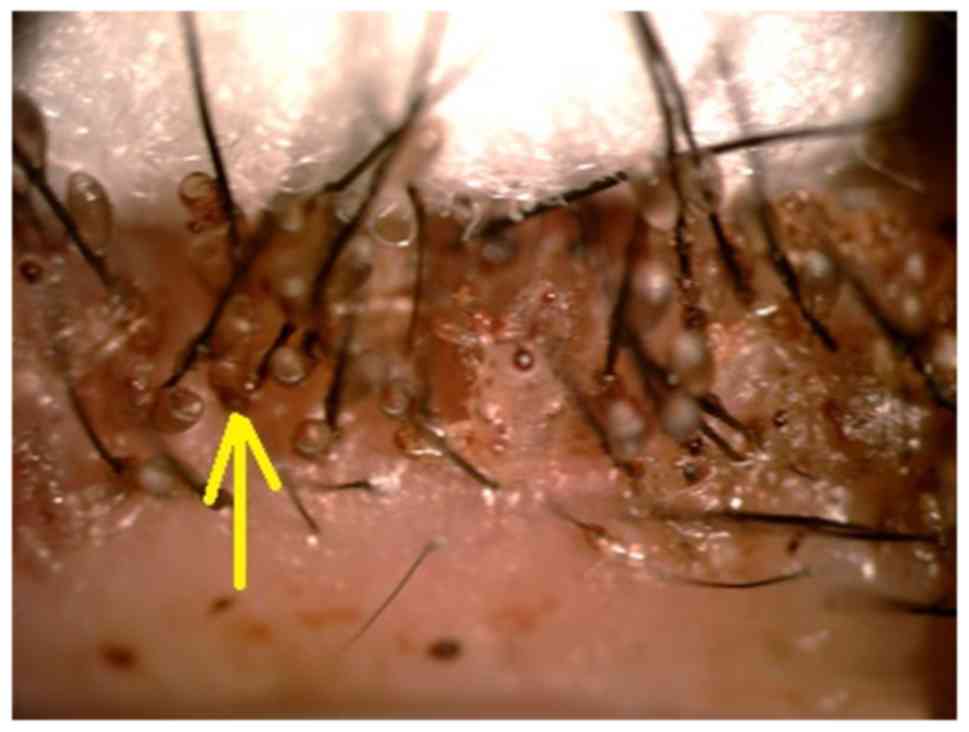
upper eyelashes (Fig. 2). A number
of small, translucent oval eggs (nits) were observed adhering to
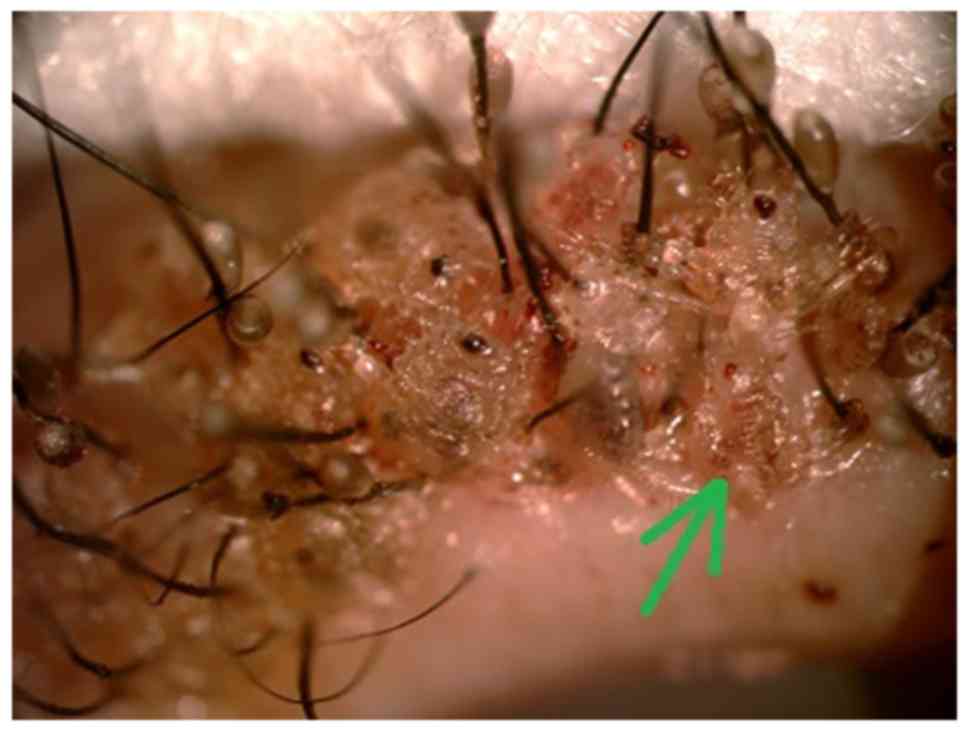
the eyelashes and eyelids of the patient (Fig. 3) and moving lice were hanging from
the eyelashes (Fig. 4). Some
eyelashes, lice and nits were removed mechanically using flat
tweezers. It is very difficult to grip the body of the louse firmly
when using flat tweezers, because its head can be deep within the
hair follicles. Force is required to extract the louse to ensure
that the head is extracted from the follicle, at which time red
dots are observed to appear on the skin of the eyelid. An eye
examination revealed light conjunctival congestion, transparent
cornea, normal transparent lens and no obvious abnormalities in the
fundus. Parasitic bodies were sent for parasitological microscopic
examination, which confirmed the primary diagnosis of
Phthiriasis pubis infestation of the eyelashes. The patient
stated that she had no previous infestations and no history of
sexually transmitted diseases (STDs). She was referred to the
Skin/STD Clinic of the Tianjin First Center Hospital for further
evaluation and returned for a follow-up 2 weeks later. At the
follow-up examination, the patient's symptoms had subsided
completely. The patient was given advice on how to avoid future
infestations, such as personal hygiene improvements and avoidance
of close contact.
Discussion
Phthiriasis palpebrarum is characterized by
infestation of the eyelashes with Pthirus pubis, which is
classed as an STD (8). Approximately
30% of cases are associated with another STD (9,10).
Phthiriasis palpebrarum is uncommon in developed countries and
typically presents in patients with poor personal hygiene (11). It is easily overlooked as the
symptoms are similar to those of blepharoconjunctivitis and
Pthirus pubis is primarily adapted to living in pubic hair
(12). In heavy infestations, lice
are found in the hair of the axilla, chest, eyebrows and eyelashes
(13–15). Phthiriasis palpebrarum is also
occasionally misdiagnosed as common blepharitis (16). Clinically, this disease is typically
not considered, in particular when ocular symptoms are not obvious
(17). To avoid this, it is
recommended that eyelids and eyelashes are carefully examined by
slit lamp to avoid misdiagnosis (18).
Pthirus pubis belongs to the phylum
Arthropoda, the class Insecta and the order Phthiraptera. Two other
subspecies of lice known to infest humans are Pediculus humanus
capitis (head louse) and Pediculus humanus corporis
(body louse) (19). Adult pubic lice
are typically 1–2 mm in size and wingless with a broad, flat
translucent body through which freshly ingested blood may be
observed. The body is crab-like and divided into the head, thorax
and abdomen, with three pairs of short, stout legs and powerful
claws, which enable them to grasp hair shafts tightly (20).
Patients with phthiriasis palpebrarum typically
present with palpebral pruritus, conjunctival inflammation, and
occasionally preauricular lymphadenopathy due to secondary
infection at the site of the louse bites (14). There are multiple treatment options
available, including mechanical removal with forceps, trimming of
the eyelashes, fluorescein eye drops 20%, physostigmine 25%, yellow
mercuric oxide ointment 1%, pilocarpine gel and oral ivermectin
(11,12,14).
Phthiriasis palpebrarum may also be treated via argon laser therapy
or cryotherapy (21). Mechanical
removal has been demonstrated to be effective in treating the
disease and preventing recurrence (22). In the present study, mechanical
removal of lice and eggs was performed successfully. Ngai et
al (23) suggested that
clothing, towels and bedding used by the patient should be washed
at ≥50°C within 2–3 days of treatment and dried on the hot cycle
for 5–10 min. Pthirus pubis are only able to travel short
distances from the point of first contact and die within 24–48 h if
removed from their hosts (24–26). Due
to the ease of transference, if the parasite is detected in one
patient then all members of the household should be examined. In
the present study, all family members were evaluated and did not
require treatment.
In conclusion, the findings of the present study
demonstrate the importance of a correct diagnosis due to the ease
with which phthiriasis palpebrarum may be confused with
blepharitis. As a result, it is suggested that eyelids and
eyelashes should be carefully examined by slit lamp to avoid
misdiagnosis in cases where blepharitis is considered. The present
study also supports systemic treatment and it may be suggested that
patients who present with phthiriasis palpebrarum should undergo
diagnostic tests for other STDs. Mechanical removal is the most
effective treatment option for phthiriasis palpebrarum; however,
follow-up examinations to detect any residual lice or nits are
necessary.
References
|
1
|
Baskan C, Duman R, Balci M and Ozdogan S:
A rare cause of blepharoconjunctivitis: Phthiriasis palpebrarum.
Niger J Clin Pract. 17:817–818. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Turgut B, Kurt J, Catak O and Demir T:
Phthriasis palpebrarum mimicking lid eczema and blepharitis. J
Ophthalmol. 2009:8039512009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lacarrubba F and Micali G: The
not-so-naked eye: Phthiriasis palpebrarum. Am J Med. 126:960–961.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Anane S, Malek I, Kamoun R and Chtourou O:
Phthiriasis palpebrarum: Diagnosis and treatment. J Fr Ophtalmol.
36:815–819. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Anderson AL and Chaney E: Pubic lice
(Pthirus pubis): History, biology and treatment vs. knowledge and
beliefs of US college students. Int J Environ Res Public Health.
6:592–600. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ryan MF: Phthiriasis palpebrarum
infection: A concern for child abuse. J Emerg Med. 46:e159–e162.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yi JW, Li L and da Luo W: Phthiriasis
palpebrarum misdiagnosed as allergic blepharoconjunctivitis in a
6-year-old girl. Niger J Clin Pract. 17:537–539. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Charfi F, Ben Zina Z, Maazoun M, Kharrat
W, Sellami D, Makni F, Ayadi A and Feki J: Phthiriasis pubis
palpebrarum in children. Diagnosis and treatment. J Fr Ophtalmol.
28:765–768. 2005.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Varela JA, Otero L, Espinosa E, Sánchez C,
Junquera ML and Vázquez F: Pthirus pubis in a sexually transmitted
diseases unit: A study of 14 years. Sex Transm Dis. 30:292–296.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Workowski KA and Berman SM: Sexually
transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep.
55:79–80. 2006.
|
|
11
|
Pinckney J II, Cole P, Vadapalli SP and
Rosen T: Phthiriasis palpebrarum: A common culprit with uncommon
presentation. Dermatol Online J. 14:72008.PubMed/NCBI
|
|
12
|
Couch JM, Green WR, Hirst LW and de la
Cruz ZC: Diagnosing and treating Pthirus pubis palpebrarum. Surv
Ophthalmol. 26:219–225. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Manjunatha NP, Jayamanne GR, Desai SP,
Moss TR, Lalik J and Woodland A: Pediculosis pubis: Presentation to
ophthalmologist as pthriasis palpebrarum associated with corneal
epithelial keratitis. Int J STD AIDS. 17:424–426. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rundle PA and Hunghes DS: Pthirus pubis
infestation of the eyelids. Br J Ophthalmol. 77:815–816. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kincaid MC: Pthirus pubis infestation of
the lashes. JAMA. 249:5901983. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Panadero-Fontán R and Otranto D:
Arthropods affecting the human eye. Vet Parasitol. 208:84–93. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
de Pinho Paes Barreto R, Biancardi AL and
Salgueiro MJ: Chronic conjunctivitis related to phthiriasis
palpebrarum. Int Ophthalmol. 32:467–469. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dağdelen S, Aykan U and Cetinkaya K:
Phthriasis palpebrarum can resemble tick larva infestation in an
eyelid. J AAPOS. 17:440–442. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Karabela Y, Yardimci G, Yildirim I, Atalay
E and Karabela SN: Treatment of Phthiriasis Palpebrarum and crab
louse: Petrolatum jelly and 1% Permethrin shampoo. Case Rep Med.
2015:2879062015.PubMed/NCBI
|
|
20
|
Sundu C, Dinç E, Kurtuluş UC and Yıldırım
Ö: Common blepharitis related to Phthiriasis Palpebrarum: Argon
laser phototherapy. Turkiye Parazitol Derg. 39:252–254. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Elston DM: Drugs used in the treatment of
pediculosis. J Drugs Dermatol. 4:207–211. 2005.PubMed/NCBI
|
|
22
|
Jiang J, Shen T and Hong CY: A peculiar
case of eye pruritus: Phthiriasis palpebrarum initially
misdiagnosed as common blepharitis. Int J Ophthalmol. 4:676–677.
2011.PubMed/NCBI
|
|
23
|
Ngai JW, Yuen HK and Li FC: An unusual
case of eye itchiness. Hong Kong Med J. 14:414–415. 2008.PubMed/NCBI
|
|
24
|
Kumar N, Dong B and Jenkins C: Pubic lice
effectively treated with Pilogel. Eye (Lond). 17:538–539. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Thappa DM, Karthikeyan K and Jeevankumar
B: Phthiriasis palpebrarum. Postgrad Med J. 79:1022003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Reddy SC: Phthiriasis palpebrarum. Indian
J Ophthalmol. 28:39–41. 1980.PubMed/NCBI
|