Introduction
Patients with small bowel diseases usually present
with abdominal pain, diarrhea, hematochezia, fever as well as
weight loss. However, due to the length, tortuosity and location of
the small bowel, its examination is technically difficult in
previous times. Furthermore, conventional methods, such as X-ray
analysis with barium enteroclysis, angiography, radioisotope
scanning, computed tomography (CT) and magnetic resonance imaging
are usually poorly tolerated or indirect, and have low diagnostic
efficacy (1–3).
Since its implementation ~10 years ago, capsule
endoscopy has become one of the most important tools for small
bowel investigation (4). This
non-invasive technology allows for direct and complete examination
of the entire small bowel, and has been particularly used in
patients with obscure gastrointestinal bleeding, mucosal lesions,
chronic abdominal pain, chronic diarrhea and Crohn's disease
(3,5–7).
However, >50,000 images are reproduced during this endoscopy
procedure and physicians are required to spend 50–120 min to
completely review these images (8).
It is undoubtedly difficult for physicians to concentrate for such
a long time and misdiagnosis may occur. Thus, software-aided
reading is urgently required to solve the time-consuming problem of
traditional capsule endoscopy.
OMOM capsule endoscopy, developed by Jinshan Science
& Technology Co. (Chongqing, China), has an added automatic
mode and quickview mode, which functions through elimination of
similar images as well as analyzing colors and patterns (9). This workstation is proved to be
valuable for small bowel evaluation with a good overall diagnostic
yield and to date, it has been widely used in >60 countries and
regions, particularly in Asia and Europe (10). While previous studies have indicated
the superiority of this innovative technique over conventional
modalities, few published studies have reported on the experience
of its clinical application (1,11,12).
Therefore, the present study evaluated the feasibility and validity
of OMOM capsule endoscopy for the diagnosis of small bowel diseases
and reported on its rational application in practice.
Materials and methods
Patients
A total of 89 consecutive patients aged >20 years
who underwent OMOM capsule endoscopy at the People's Hospital of
Xinghua (Jiangsu, China) from March 2012 to September 2014 were
recruited for the present study. These patients had small bowel
diseases, including obscure abdominal pain, chronic diarrhea,
gastrointestinal bleeding and anemia. Capsule endoscopy was not
performed in patients who were unable to swallow, suffering from
digestive tract stenosis or obstruction, acute ulcerative colitis,
ischemic bowel diseases or radioactive colitis, suspected to have
digestive tract stenosis and fistula and/or those with a cardiac
pacemaker or other electro-medical device implanted.
The present study was approved by the Ethics
Committee of Xinghua People's Hospital (Jiangsu, China). Written
informed consent to undergo the entire procedure of capsule
endoscopy and for the use of images/data for publication in the
present study was obtained from each of the included patients.
Device description
The OMOM endoscopy capsule was purchased from
Jinshan Science & Technology (Chongqing, China). This
diagnostic system consisted of an OMOM capsule (13.0×27.9 mm), an
image recorder and a workstation. Image features included a
resolution of 0.1 mm and a 140° field of view. Images were first
captured at a rate of two per second and the acquired images were
then transmitted to the image recorder, which was later connected
to the workstation. Images were finally processed in the
workstation by a specifically designed software package.
Capsule endoscopy
Patients were instructed to follow a 1-day
minimum-residue diet with an overnight fast prior to undergoing the
procedure. At 3–4 h following dinner, each of them took
polyethylene glycol electrolyte powder orally with 3–4 l drinking
water for small-bowel cleansing and then took 100 mg simethicone to
prevent bubbles in the small bowel half an hour prior to undergoing
OMOM capsule endoscopy.
The procedure of capsule endoscopy was performed as
previously described (13). The
course was monitored through a computer station. If the OMOM
capsule did not reach the duodenum within 2 h, a snare under
gastroscopy was used to facilitate propulsion of the capsule. After
8-h ingestion, the recorded data were downloaded to the OMOM
workstation and the capsule endoscopy video was reviewed by two
physicians independently. The average transit time of the endoscopy
capsule in the esophagus, stomach and small intestine was
calculated, as well as the percentage of each type of small bowel
disease.
Statistical analysis
Continuous and categorical variables were
respectively presented as the mean ± standard deviation and
frequency (%). All calculations and analyses were performed by SPSS
19.0 software (IBM Corp., Armonk, NY, USA). P<0.05 was
considered to indicate a statistically significant difference.
Results
Demographic and clinical data of
patients
A total of 89 patients, including 43 males and 46
females, were included in the present study. The age of the
included patients ranged from 20 to 80 years and the median age was
53.41 years. Among these patients, 45 presented with obscure
abdominal pain, 22 with chronic diarrhea, 18 with obscure
gastrointestinal bleeding and 4 with anemia.
Transit time of capsule endoscopy in
the digestive tract
As presented in Table
I, the transit time of the capsules in the stomach was >90
min in 29 of the 89 patients. For 8 of the 29 patients, a snare
under gastroscopy was used, as the endoscopy capsule was retained
in the stomach for >120 min. However, capsule retention for
>7 h occurred in 4 patients (4.49%), among which the capsules
did not reach the colon in 2 of these patients. A further 2
patients presented with capsule retention in their small
intestines. One of the capsule retention patients complained of
abdominal pain and the other one developed diarrhea, the latter of
which was diagnosed with Crohn's disease. Finally, all of the
retention capsules were successfully removed. The completion rate
of capsule endoscopy was 85/89 (95.51%). The average transit time
of the endoscopy capsule in esophagus, stomach and small intestine
was 62.18±64.23 sec, 67.46±63.13 min and 346.53±102.81 min,
respectively.
 | Table I.Transit time of capsule endoscopy in
the digestive tract of patients. |
Table I.
Transit time of capsule endoscopy in
the digestive tract of patients.
|
|
| Transit in stomach
(min) | Transit in small
intestine (min) |
|---|
|
| Transit in esophagus
(sec) | <90 | 90–120 | >120 | 120–240 | 240–360 | 360–420 | 420–480 |
|---|
| Cases (n) | 89 | 60 | 21 | 8 | 10 | 58 | 17 | 4 |
| Transit time | 62.18±64.23 |
| 67.46±63.13 |
|
| 346.53±102.81 |
|
Capsule endoscopy findings
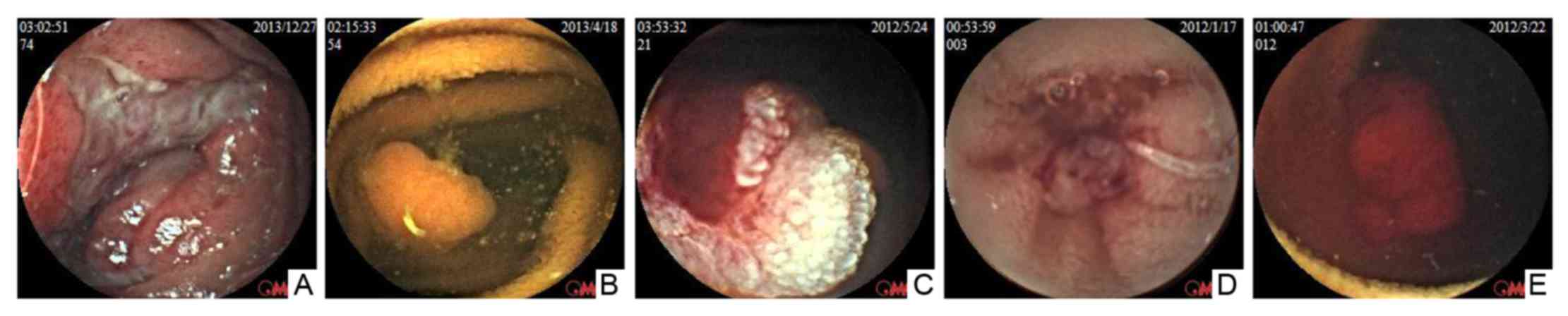
On capsule endoscopy examination, small intestinal
lesions were identified in 54 of 89 patients (60.67%), among which
19 (21.35%), 15 (16.85%), 9 (10.11%), 5 (5.62%), 5 (5.62%) and 1
(1.12%) were diagnosed with mucosal erosion, anabrosis, polypus,
angiodysplasia, tumor and ancylostomiasis (Fig. 1 and Table
II).
 | Table II.Capsule endoscopy results depending on
different symptoms within the cohort (n=89). |
Table II.
Capsule endoscopy results depending on
different symptoms within the cohort (n=89).
| Diagnosis | Abdominal pain | Diarrhea | Gastrointestinal
bleeding | Anemia | Total, n (%) |
|---|
| Mucosal erosion | 10 | 5 | 4 | 0 | 19 (21.35) |
| Anabrosis | 5 | 5 | 2 | 3 | 15 (16.85) |
| Polypus | 5 | 2 | 2 | 0 | 9
(10.11) |
| Angiodysplasia | 0 | 0 | 5 | 0 | 5 (5.62) |
| Tumor | 3 | 1 | 1 | 0 | 5 (5.62) |
| Ancylostomiasis | 0 | 0 | 0 | 1 | 1 (1.12) |
| Total | 23 | 13 | 14 | 4 | 54 (60.67) |
Specifically, of the 45 patients with obscure
abdominal pain, 10 (22.22%) were diagnosed with mucosal erosion, 5
(11.11%) with anabrosis, 5 (11.11%) with polypus and 3 (6.67%) with
tumors. Among the 22 chronic diarrhea patients, 5 (22.73%) had
mucosal erosion, 5 (22.73%) had ulcers, 2 (9.09%) had polypus and 1
(4.55%) had one tumor. Of the 18 subjects with obscure
gastrointestinal bleeding, 4 (22.22%) were diagnosed with mucosal
erosion, 3 (16.67%) with anabrosis, 2 (11.11%) with polypus, 5
(27.78%) with angiodysplasia (3 (16.67%) with active bleeding and 2
(11.11%) with bleeding) and 1 (5.56%) with one tumor. Of the 4
anemia patients, 3 (75.00%) had anabrosis and 1 (25.00%) had
ancylostomiasis.
Discussion
OMOM capsule endoscopy, a promising and innovative
technique, has been widely used in China, Africa and Europe since
its marketing from 2005 onwards. The present prospective study
presented the diagnostic value of OMOM capsule endoscopy in
practice. The results demonstrated that the average transit time of
the endoscopy capsule in the esophagus, stomach and small intestine
was 62.18±64.23 sec, 67.46±63.13 min and 346.53±102.81 min,
respectively. In addition, OMOM capsule endoscopy identified 54 out
of 89 patients (60.67%) with various types of small intestinal
lesion, among which 19 (21.35%), 15 (16.85%), 9 (10.11%), 5
(5.62%), 5 (5.62%) and 1 (1.12%) were diagnosed with mucosal
erosion, anabrosis, polypus, angiodysplasia, tumor and
ancylostomiasis.
The small bowel is characterized by its considerable
length, tortuosity and inaccessibility, which makes small bowel
examinations a challenge for physicians. Conventional modalities
for diagnosing suspected small bowel lesions have been reported to
be low in sensitivity or invasive and difficult to tolerate for
patients (14–16). Of note, the advent of capsule
endoscopy has facilitated small bowel examination with high
diagnostic efficiency and non-invasiveness with no pain. Several
different types of capsule endoscopy system have emerged and the
PillCam capsule endoscope, developed by Given Imaging (Yokne'am
Illit, Israel), is the first and most widely used wireless
endoscopy system worldwide. Although less well-known than the
PillCam capsule endoscope, the diagnostic yield of OMOM capsule
endoscopy has been proved to be similar (11). In the present study, visualization of
the entire small bowel by OMOM capsule endoscopy was achieved in 85
of 89 patients (95.51%) and various distinct types of lesion were
identified, including mucosal erosion, anabrosis, polypus,
angiodysplasia, tumor and ancylostomiasis. Thus, OMOM capsule
endoscopy is effective in diagnosing patients with suspected small
bowel disease, particularly for those with pathologies that are
difficult to detect by traditional methods.
The transit time in the digestive tract is a key
parameter for successful completion of capsule endoscopy. A
retrospective study demonstrated that a transit time of >45 min
in the stomach is an independent risk factor for incomplete capsule
endoscopy in the small bowel (17).
The prolonged transfer may be associated with the positioning of
patients and insufficient gastrointestinal motility in the resting
state. In order to resolve limitations regarding incomplete small
bowel capsule endoscopy, drugs such as domperidone have been used
to improve the gastric dynamics and improve the diagnostic yield of
endoscopy (18). In the present
study, the first real-time observation was performed during the
initial 90 min of capsule action. The second real-time observation
was performed at 90–120 min. In 8 of the patients, gastroscopy
intervention was performed, as the capsule retention in their
stomach was >120 min. Finally, the capsules did not reach the
colon in only 2 of the patients.
The diagnostic yield of capsule endoscopy varies
among different studies. Mohan et al (1) reported that 36 out of 42 patients
(85.71%) had abnormal findings on OMOM capsule endoscopy in their
study, among which 26 patients exhibited obscure gastrointestinal
bleeding and a further 10 patients exhibited abdominal pain and/or
diarrhea. However, the diagnostic yield in another study using the
PillCam patency capsule was 77.78% (14/18) (19). In the present study, various types of
lesion were detected in 54 out of 89 patients (60.67%), which was
lower than the rates in previous studies. This may be explained by
the relatively small number of samples included in these studies.
Although capsule endoscopy has the capacity of providing endoscopic
imaging data of the entire small bowel, a miss rate of 10% has been
reported for this method (20). In
the present study, capsule retention occurred in four patients
(4.49%); the capsules did not enter their small bowel at all and no
detection was performed. Thus, endoscopy capsule retention may also
be an explanation for the discrepancy in diagnostic yield.
As other capsules, the OMOM endoscopy capsule has
several limitations. First, the diagnostic value for esophagus and
colon lesions is limited due to the short transit time and battery
life. Furthermore, there are blind areas and the capsule cannot
accurately identify all lesions due to the small bowel residue,
bleeding or peristalsis. Therefore, studies focusing on these
limitations as well as those aiming to improve the diagnostic
accuracy are required to realize the full potential of capsule
endoscopy.
In conclusion, the present 2-year retrospective
study confirmed the feasibility and validity of OMOM capsule
endoscopy as a diagnostic tool for small bowel disease in adults.
In China, OMOM capsule endoscopy may be a better choice for
investigating the cause of obscure chronic abdominal pain, diarrhea
and gastrointestinal bleeding, as it is relatively low-cost and
while having an acceptable diagnostic value.
References
|
1
|
Mohan K, Xiaohong T, Dao-Rong C, Shun-Wen
W and Sai G: One year experience of OMOM capsule endoscopy for
suspected small intestine lesions. J Nobel Med Coll. 1:27–29.
2011.
|
|
2
|
Masselli G, Casciani E, Polettini E and
Gualdi G: Comparison of MR enteroclysis with MR enterography and
conventional enteroclysis in patients with Crohn's disease. Eur
Radiol. 18:438–447. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Marmo R, Rotondano G, Piscopo R, Bianco MA
and Cipolletta L: Meta-analysis: Capsule enteroscopy vs.
conventional modalities in diagnosis of small bowel diseases.
Aliment Pharmacol Ther. 22:595–604. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Iddan G, Meron G, Glukhovsky A and Swain
P: Wireless capsule endoscopy. Nature. 405:4172000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pennazio M, Santucci R, Rondonotti E,
Abbiati C, Beccari G, Rossini FP and De Franchis R: Outcome of
patients with obscure gastrointestinal bleeding after capsule
endoscopy: Report of 100 consecutive cases. Gastroenterology.
126:643–653. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jensen MD, Nathan T, Rafaelsen SR and
Kjeldsen J: Diagnostic accuracy of capsule endoscopy for small
bowel Crohn's disease is superior to that of MR enterography or CT
enterography. Clin Gastroenterol Hepatol. 9:124–129. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Triester SL, Leighton JA, Leontiadis GI,
Fleischer DE, Hara AK, Heigh RI, Shiff AD and Sharma VK: A
meta-analysis of the yield of capsule endoscopy compared to other
diagnostic modalities in patients with obscure gastrointestinal
bleeding. Am J Gastroenterol. 100:2407–2418. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Delvaux M and Gay G: Capsule endoscopy:
Technique and indications. Best Pract Res Clin Gastroenterol.
22:813–837. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xu Y, Zhang W, Ye S, Han Z, Bai Y, Li A,
Chen Z, Wan T and Liu S: The evaluation of the OMOM capsule
endoscopy with similar pictures elimination mode. Clin Res Hepatol
Gastroenterol. 38:757–762. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liao Z, Gao R, Li F, Xu C, Zhou Y, Wang JS
and Li ZS: Fields of applications, diagnostic yields and findings
of OMOM capsule endoscopy in 2400 Chinese patients. World J
Gastroenterol. 16:2669–2676. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li CY, Zhang BL, Chen CX and Li YM: OMOM
capsule endoscopy in diagnosis of small bowel disease. J Zhejiang
Univ Sci B. 9:857–862. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xue M, Chen X, Shi L, Si J, Wang L and
Chen S: Small-bowel capsule endoscopy in patients with unexplained
chronic abdominal pain: A systematic review. Gastrointest Endosc.
81:186–193. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Geng Y, Wang AM, Gao WY, Zhang ZW, Xiong Y
and Yuan-Ping LI: Diagnostic value of OMOM capsule endoscopy in
gastrointestinal diseases. Chin J Clin Gastroenterol. 2010.
|
|
14
|
Costamagna G, Shah SK, Riccioni ME,
Foschia F, Mutignani M, Perri V, Vecchioli A, Brizi MG, Picciocchi
A and Marano P: A prospective trial comparing small bowel
radiographs and video capsule endoscopy for suspected small bowel
disease. Gastroenterology. 123:999–1005. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ell C, Remke S, May A, Helou L, Henrich R
and Mayer G: The first prospective controlled trial comparing
wireless capsule endoscopy with push enteroscopy in chronic
gastrointestinal bleeding. Endoscopy. 34:685–689. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hara AK, Leighton JA, Sharma VK and
Fleischer DE: Small bowel: Preliminary comparison of capsule
endoscopy with barium study and CT. Radiology. 230:260–265. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Eliakim R: Video capsule endoscopy of the
small bowel. Curr Opin Gastroenterol. 26:129–133. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cotter J, de Castro FD, Magalhães J,
Moreira MJ and Rosa B: Finding the solution for incomplete small
bowel capsule endoscopy. World J Gastrointest Endosc. 5:595–599.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gralnek IM, Cohen SA, Ephrath H, Napier A,
Gobin T, Sherrod O and Lewis J: Small bowel capsule endoscopy
impacts diagnosis and management of pediatric inflammatory bowel
disease: A prospective study. Dig Dis Sci. 57:465–471. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lewis BS, Eisen GM and Friedman S: A
pooled analysis to evaluate results of capsule endoscopy trials.
Endoscopy. 39:303–308. 2007. View Article : Google Scholar
|