Introduction
Radiofrequency catheter ablation (RFCA) has become
the curative treatment of choice for supraventricular tachycardia
(SVT) in patients with Wolff-Parkinson-White (WPW) syndrome
(1). The posteroseptal accessory
pathways (APs) are occasionally located in the epicardial region
and are associated with ablation failure due to their complex
anatomic arrangement. This type of epicardial AP results from a
connection between an extension of the coronary sinus (CS)
myocardial coat along the middle cardiac vein, or the neck of a CS
diverticulum and the left ventricular epicardium (2). In the current study, a case of left
posteroseptal AP showing narrow QRS-complex SVT and atrial flutter
is described that was successfully ablated with radiofrequency
energy applied in the neck of a CS diverticulum.
Case report
A 46-year-old male presented with recurrent SVT
associated with symptoms of palpitations, dizziness and
diaphoresis. The termination of tachycardia with drugs is not
always successful and electrical cardioversion may be required. The
patient in this study used antiarrhythmic drugs prior to
radio-frequency catheter ablation (RFCA) and drugs alone were used
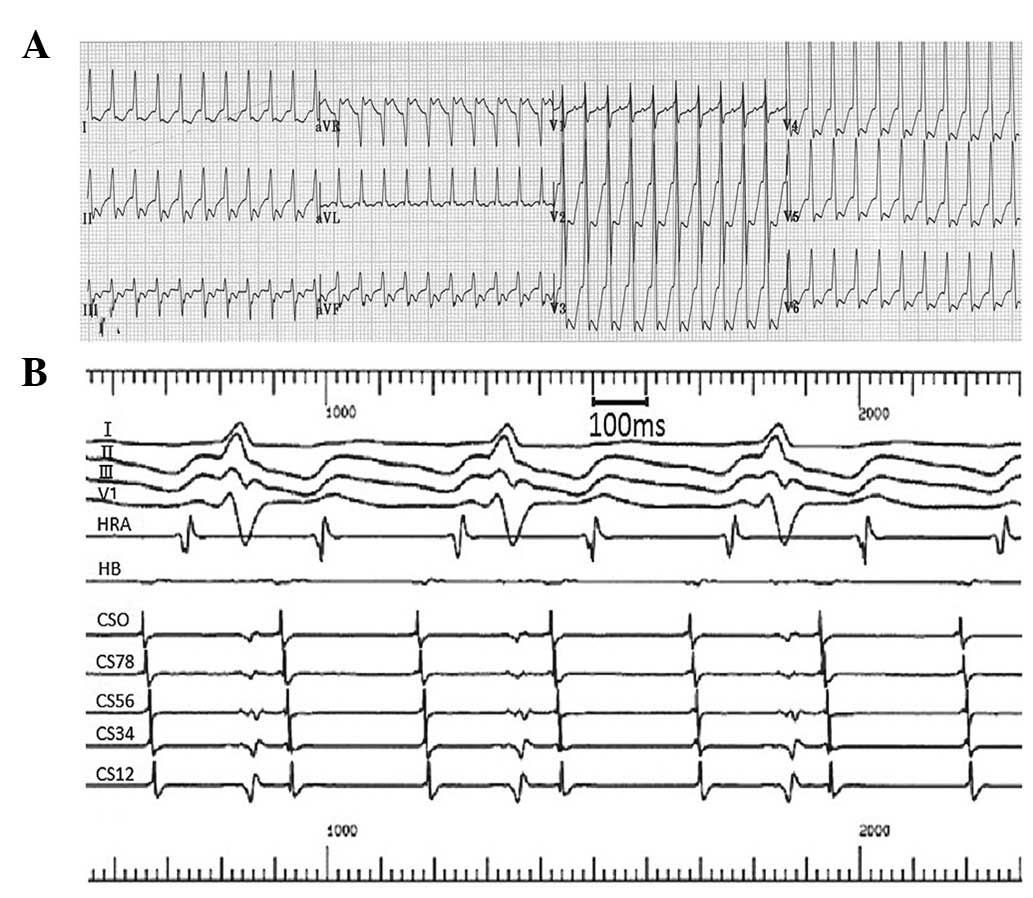
during the attacks. A sinus rhythm electrocardiogram (ECG) showed
ventricular pre-excitation with a positive δ wave in leads I, V1,
V2 and a negative δ wave in leads II, III and aVF (Fig. 1A), indicating a left posteroseptal
AP. SVT at a rate of 230 beats/min was documented by ECG during the
attacks (Fig. 2A). The rhythm was
regular and the waves showed a narrow QRS-complex. The patient also
presented with paroxysmal atrial flutter (2:1) during ablation
(Fig. 2B). The esophagus
electrophysiological study (EPS) confirmed the manifest left AP
accompanied orthodromic atrioventricular reentrant tachycardia
(AVRT). Clinical examination, chest X-ray and echocardiography were
normal.
An EPS was performed to identify the mechanism of
tachycardia and RFCA. A deflectable decapolar catheter (Cordis
Webster, Diamond Bar, CA, USA) was placed in the coronary sinus via
the left subclavian vein. Quadripolar catheters (Cordis-Webster)
were introduced through the right femoral vein and positioned in
the His-bundle region and the right ventricular apex (RVA). The
intracardiac electrogram revealed the earliest atrial activation
was at the CS ostium and RVA pacing initiated orthodromic AVRT. The
AP was located in the left posteroseptal region. An 8-French
ablation catheter with a 4-mm tip electrode (Cordis-Webster) was
introduced via the right femoral artery and placed under the mitral
valve close to the annulus. The ventricular wave could not be
significantly ahead of the atrial wave and the AV wave was not
always merged. The applications of radiofrequency energy (20W, 10
sec) delivered in the posteroseptal region of the mitral valve
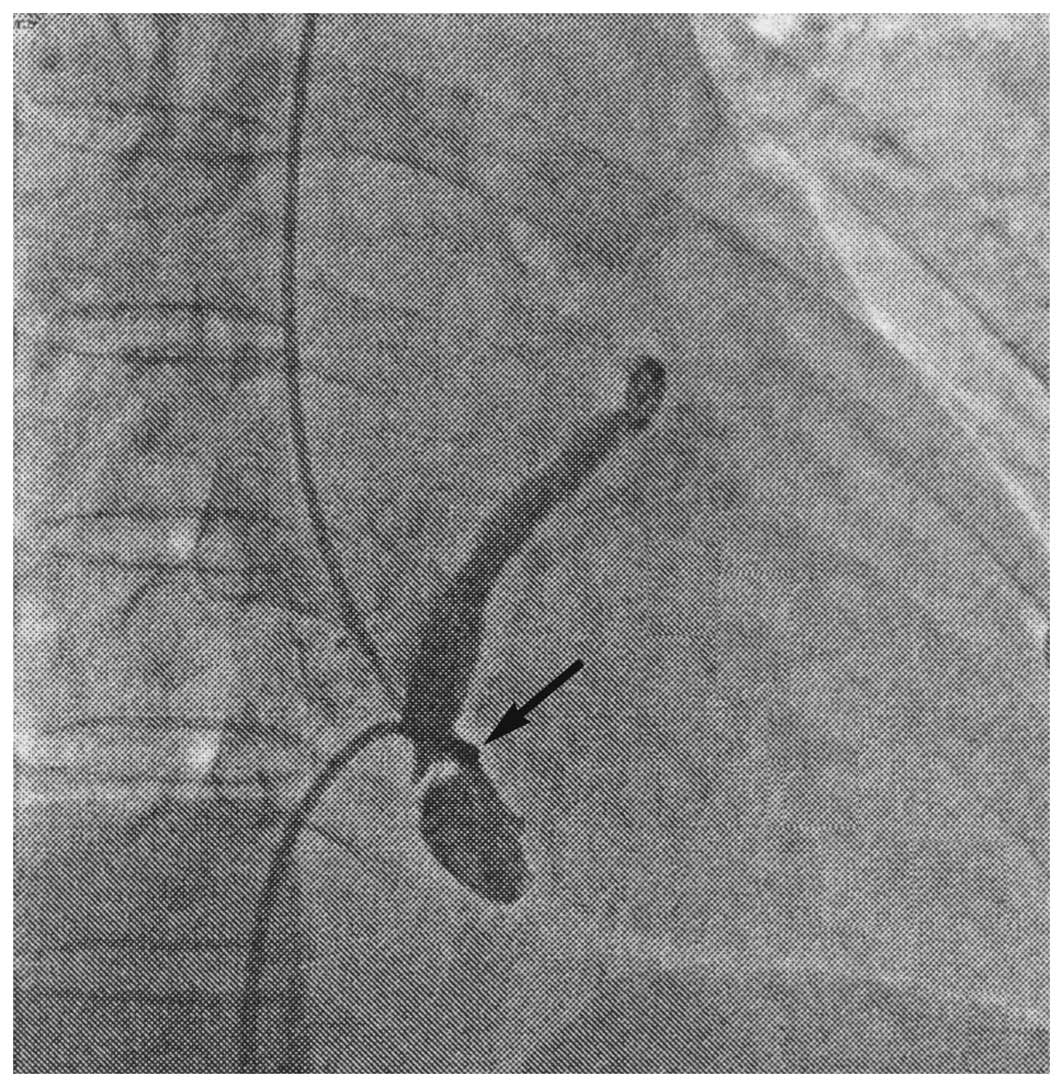
annulus failed to ablate the AP. Due to the consideration that the
AP may have been located at the epicardium, CS angiography was
implemented and a CS diverticulum was identified near the ostium
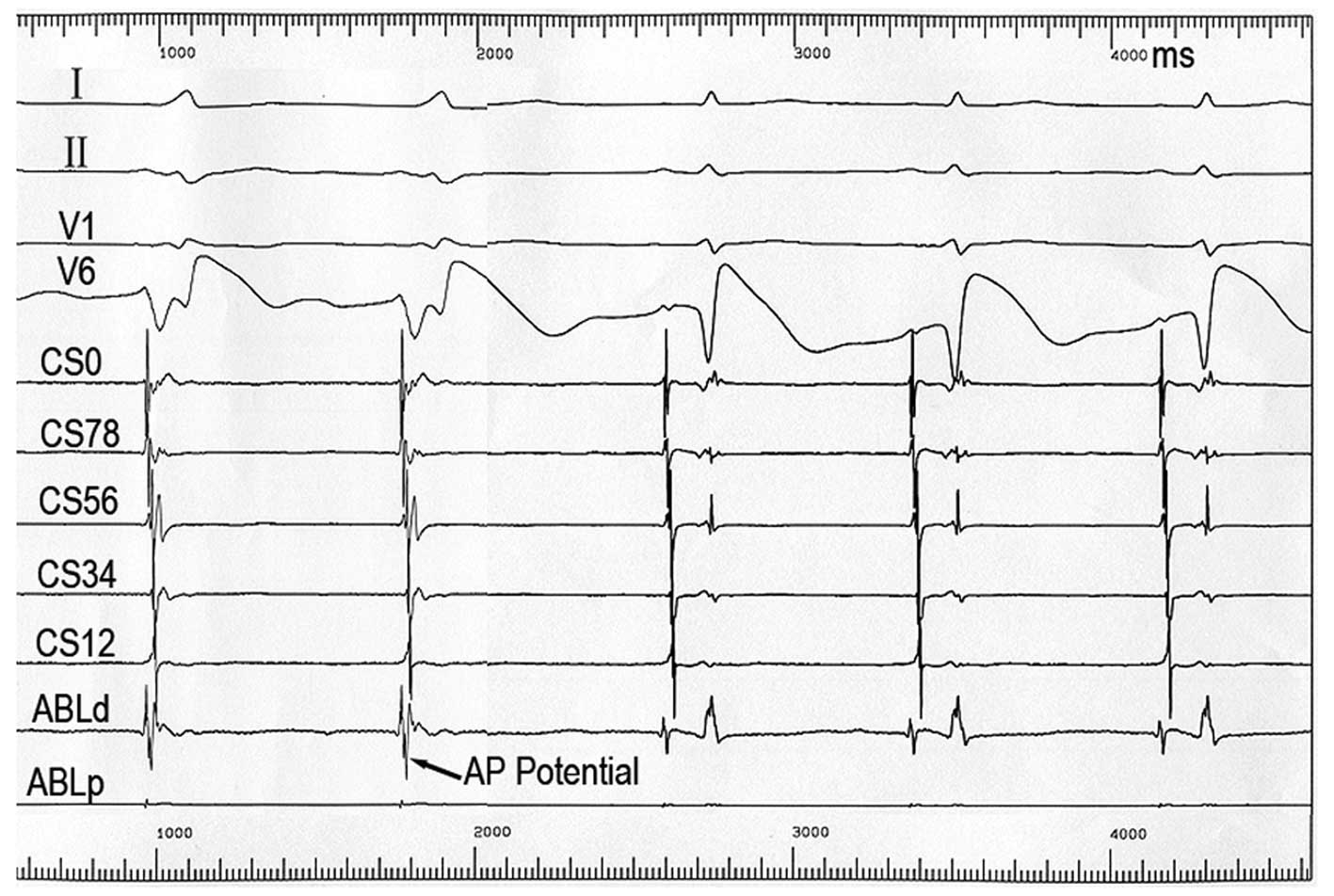
(Fig. 3). The ablation catheter
was placed into the CS via the right femoral vein and the ideal
target in the neck of CS diverticulum was recorded. The ventricular
wave was significantly ahead of the atrial wave and the AV wave was
fusion well (Fig. 4). At this
site, a clear AP potential was recorded by the ablation catheter.
Ablation in this area under temperature control with a
radiofrequency energy of 20 W (AV wave separation after 3 sec then
terminated discharge after 60 sec, Fig. 4) achieved successful abolition of
atrioventricular conduction via the AP. Following ablation, the δ
wave disappeared from the surface ECG and the PR interval was 0.16
sec (Fig. 1B). Programmed atrial
pacing showed the retrograde atrioventricular conduction property
and ventricular pacing displayed AV wave separation. A vigorous
stimulation protocol with isoprenaline failed to induce
tachycardia. The patient did not experience recurring tachycardia
within the one-year follow-up.
Discussion
A CS diverticulum is a rare congenital abnormality
of the intracardiac veins and is shown to contain myocardial fibers
which connect to the ventricle and the CS myocardial coat. The
connections between the CS myocardial coat and the ventricle may
serve as an AP (2,3). CS diverticula are known to be present
in patients with WPW syndrome with APs located in the posteroseptal
region (2,3). Epicardial APs are most commonly
located in the posteroseptal regions. The finding of a steep
negative δ wave in lead II is known to be predictive of an
epicardial AP. It has been reported that the sensitivity of a
negative δ wave in lead II in identifying a CS AP is >70%
(4). The ECG of the present case
showed a positive δ wave in leads I, V1, V2 and negative δ waves in
leads II, III and aVF. The patient was confirmed as having left
posteroseptal epicardial AP accompanied by a CS diverticulum.
A CS diverticulum is usually associated with
manifest posteroseptal APs and the manifest APs have bidirectional
atrioventricular conduction properties (5). These APs are difficult to ablate
endocardially outside the diverticulum and successful ablation is
often performed from within the diverticulum. Diagnosis of CS
diverticulum may be difficult from transthoracic echocardiograms.
CS angiography is suggested, therefore, prior to catheter ablation
of posteroseptal APs, especially when endocardial signals are not
optimal. In patients with a CS diverticulum, an AP potential is
often recorded from the neck of the diverticulum. In the EPS,
orthodromic AVRT was easily inducible and the earliest atrial
activation during sinus rhythm was mapped and identified to be
within the CS diverticulum. A CS diverticulum may contribute to the
reentrant circuit of atrial flutter (6). The present patient presented with
paroxysmal atrial flutter (2:1) during surgery. WPW syndrome with a
CS diverticulum has a high incidence of atrial flutter with short
R-to-R intervals, and a number of sudden mortalities have been
reported. APs in this location tend to have a very rapid
atrioventricular conduction, putting these patients at risk of
sudden mortality during atrial flutter or atrial fibrillation; such
APs, therefore, should be ablated (7,8). Due
to the close proximity of the CS ostium and posterolateral branch
of the right coronary artery, caution should be exercised while
applying radiofrequency energy to the CS. When the optimal ablation
site is near the passage of the right coronary artery,
saline-irrigated ablation or temperature-controlled ablation is
recommended to avoid the complication of coronary artery stenosis
(9). Moreover, the walls of the
coronary veins and the atriums are rather thin so vessel rupture,
hemopericardium and cardiac tamponade may occur when radiofrequency
is delivered within a CS diverticulum. CS angiography was performed
prior to the ablation to define the anatomy around the ablation
site and a temperature-controlled ablation catheter was used to
prevent complications. It is recognized that ablation of a
posteroseptal AP requires CS angiography and careful evaluation of
CS recordings for AP potential.
This case report illustrates a patient who had SVT
and atrial flutter with a left posteroseptal AP associated with a
CS diverticulum. RFCA at the neck of the CS diverticulum
effectively interrupted the AP conduction. The current case
highlights the potential importance of CS angiography and
identification of AP potentials in patients with a posteroseptal AP
which is difficult to ablate by the endocardial approach.
References
|
1.
|
Jackman WM, Wang XZ, Friday KJ, et al:
Catheter ablation of accessory atrioventricular pathways
(Wolff-Parkinson-White syndrome) by radiofrequency current. N Engl
J Med. 324:1605–1611. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Sun Y, Arruda M, Otomo K, et al: Coronary
sinus-ventricular accessory connections producing posteroseptal and
left posterior accessory pathways: incidence and
electrophysiological identification. Circulation. 106:1362–1367.
2002. View Article : Google Scholar
|
|
3.
|
Di Segni E, Siegal A and Katzenstein M:
Congenital diverticulum of the heart arising from the coronary
sinus. Br Heart J. 56:380–384. 1986.PubMed/NCBI
|
|
4.
|
Arruda MS, McClelland JH, Wang X, et al:
Development and validation of an ECG algorithm for identifying
accessory pathway ablation site in Wolff-Parkinson-White syndrome.
J Cardiovasc Electrophysiol. 9:2–12. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Liu S, Yuan S and Olsson SB: Conduction
properties of accessory atrioventricular pathways: importance of
the accessory pathway location and normal atrioventricular
conduction. Scand Cardiovasc J. 37:43–48. 2003. View Article : Google Scholar
|
|
6.
|
Igarashi M, Tada H, Sekiguchi Y and Aonuma
K: Successful radiofrequency catheter ablation of common atrial
flutter at the bottom of a coronary sinus diverticulum. Heart
Vessels. 27:643–647. 2012. View Article : Google Scholar
|
|
7.
|
Funabashi N, Asano M and Komuro I: Giant
coronary sinus diverticulum with persistent left superior vena cava
demonstrated by multislice computed tomography. Int J Cardiol.
111:468–469. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Blank R, Dieterle T, Osswald S and
Sticherling C: Images in cardiovascular medicine.
Wolff-Parkinson-White syndrome and atrial fibrillation in a patient
with a coronary sinus diverticulum. Circulation. 115:e469–e471.
2007. View Article : Google Scholar
|
|
9.
|
Jang SW, Rho TH, Kim DB, et al: Successful
radiofrequency catheter ablation for wolff-Parkinson-white syndrome
within the neck of a coronary sinus diverticulum. Korean Circ J.
39:389–391. 2009. View Article : Google Scholar
|