Lung cancer is the leading cause of cancer-related
death throughout the whole world. More than half (57%) of all
patients with lung cancer have metastasis at the time of diagnosis,
and the 5-year survival rate is only 5% (1). Non-small cell lung cancer (NSCLC)
constitutes 85% of all lung cancer cases (2). Epidermal growth factor receptor
(EGFR) is one of the most common driver genes in NSCLC.
Female patients have higher mutation rates than male patients.
Adenocarcinomas and non-smoking are also associated with
EGFR mutations (3). The
EGFR belongs to the HER/ErbB family; it locates on the cell
surface, and binds to its ligands, such as EGF and transforming
growth factor. Upon ligand binding, EGFR undergoes dimer formation
and auto-phosphorylation at the tyrosine residues, and activates
downstream signaling through MAPK and PI3K pathways, leading to
cancer cell proliferation, differentiation and migration (4). Approximately 20% of NSCLC patients
bear activating mutations in EGFR. The deletions in exon 19
(Ex19del) and the L858R point mutation within exon 21 constitute
~90% of EGFR activating mutations (5). The activating mutations of
EGFR are the targets of EGFR tyrosine kinase inhibitors
(EGFR-TKIs). Current treatment guidelines recommend EGFR-TKIs as
the 1st-line treatment for patients with advanced NSCLC with
EGFR activating mutations.
The 1st-generation EGFR-TKIs, including gefitinib,
erlotinib and icotinib, are reversible inhibitors that can inhibit
the EGFR tyrosine kinase domain in an ATP-competitive and
-reversible manner (Fig. 1)
(6). The Iressa Pan-Asia study is
a phase III and open-label study comparing gefitinib with
carboplatin-paclitaxel as the 1st-line treatment for patients with
advanced NSCLC in East Asia. The results showed that in the
patients with EGFR-activating mutations, the gefitinib group
experienced longer progression-free survival (PFS) than the
carboplatin/paclitaxel group, while in patients without EGFR
mutations, there was no PFS benefit in the gefitinib group
(7). In 2015, gefitinib was
approved by the U.S. Food and Drug Administration (FDA) for the
1st-line treatment of advanced NSCLC with EGFR-activating
mutations (8). The European
Tarceva versus Chemotherapy study is a multicenter, open-label and
randomized phase III trial, which aimed to compare erlotinib with
platinum-based chemotherapy as the 1st-line treatment for European
patients with advanced NSCLC. In this study, erlotinib
significantly improved PFS time compared with platinum-based
chemotherapy in the patients with EGFR-activating mutations
(9.7 vs. 5.2 months; HR, 0.37; 95% CI, 0.25-0.54; P<0.0001)
(9). Icotinib is independently
developed in China, and the CONVINCE study was designed to compare
the efficacy and safety of 1st-line icotinib versus
cisplatin/pemetrexed plus pemetrexed maintenance in patients with
advanced lung adenocarcinoma. The results have demonstrated
superior efficacy in that the PFS time of the icotinib group was
significantly longer than that of the pemetrexed plus cisplatin
chemotherapy group following the 1st-line treatment of
EGFR-mutated NSCLC (11.2 vs. 7.9 months; HR, 0.61; 95% CI,
0.43-0.87; P=0.006) (10).
The 2nd-generation EGFR-TKIs, such as afatinib and
dacomitinib, were originally designed to overcome the resistance to
the 1st-generation EGFR-TKIs (Fig.
1). Afatinib is an irreversible dual specificity EGFR/human
epidermal growth factor receptor 2 (HER2) inhibitor that is
designed to covalently bind to EGFR and HER2, while dacomitinib is
an irreversible pan-HER inhibitor. The broad spectrum of activity
enables them to improve inhibition of EGFR-dependent tumor growth
compared with the 1st-generation EGFR-TKIs. In the LUX-Lung7 and
ARCHER studies, afatinib and dacomitinib significantly prolonged
PFS and overall survival (OS) times compared with gefitinib in the
1st-line treatment of patients with NSCLC and EGFR
activating mutations (11,12).
However, afatinib and dacomitinib exhibited low maximum tolerated
doses in the patients. Compared to gefitinib, they were associated
with a higher incidence of adverse events, including increased skin
and gastrointestinal toxicity. The 2nd-generation EGFR-TKIs
therefore have limited roles in patients with developed resistance
to the 1st-generation EGFR-TKIs (13-15). Most patients inevitably develop
acquired resistance through various mechanisms after 9-13 months of
treatment with the 1st- and 2nd-generation EGFR-TKIs. The T790M
mutation in EGFR exon 20 is the predominant cause, occurring
in 50-60% of patients (15-17).
The so-called 'gatekeeper' T790M mutation increases
the competition between ATP and the reversible EGFR-TKIs by
exerting effects on both steric hindrance and increased ATP
affinity to mutant EGFR receptor, thereby decreasing the efficacy
of 1st- and 2nd-generation EGFR-TKIs (15). The 3rd-generation EGFR-TKIs,
represented by osimertinib, have satisfactory efficacy in
overcoming acquired resistance to the 1st- and 2nd-generation
EGFR-TKIs mediated by T790M mutation (Fig. 1). Osimertinib selectively targets
the EGFR T790M mutation, forming covalent bonds with the
C797 residue in the ATP-binding site of mutant EGFR. Since their
binding is irreversible, this agent overcomes the enhanced ATP
affinity conferred by the T790M mutation; it exhibits ~200 times
greater potency against L858R/T790M mutant EGFR than wild-type EGFR
(18). The 3rd-generation
EGFR-TKIs have promising clinical activity and tolerability. For
patients who progressed on the 1st-generation EGFR-TKI treatment
and have a T790M mutation, osimertinib has significantly improved
their PFS and OS times compared with chemotherapy (17). Furthermore, osimertinib has shown
better efficacy than gefitinib or erlotinib in untreated NSCLC with
EGFR mutations (19).
Patients receiving osimertinib have a lower incidence of serious
adverse events than those treated with the 1st- or 2nd-generation
EGFR-TKIs (12,19). However, patients with
EGFR-activating mutations administered osimertinib as the
1st-line treatment have also been found to inevitably develop
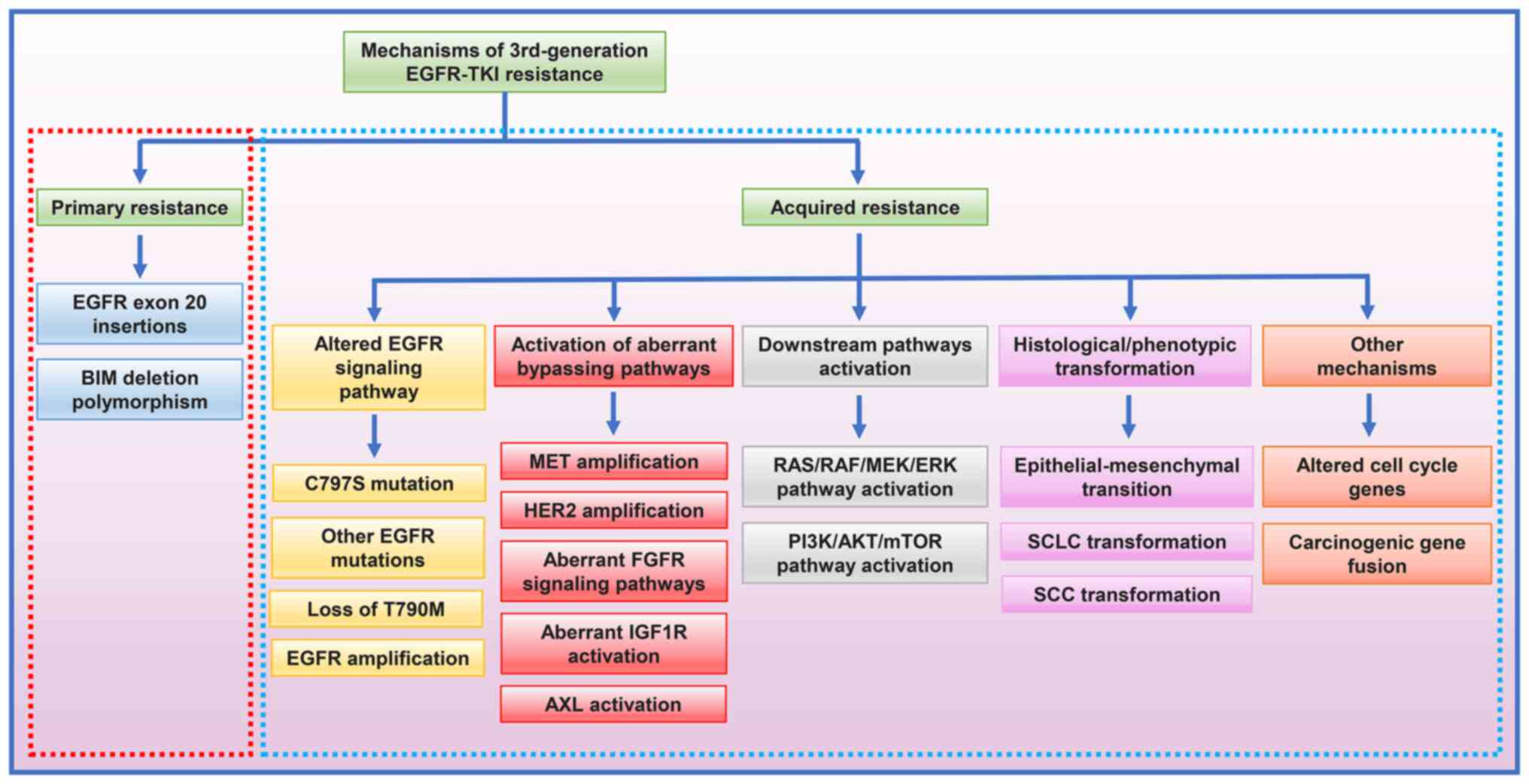
resistance after 18.9 months (19). Previous studies on the mechanisms
of 3rd-generation EGFR-TKI resistance have revealed both primary
and acquired resistance (Fig. 2).
For patients with NSCLC progression after the 3rd-generation
EGFR-TKI treatments, the use of next-generation sequencing (NGS) of
plasma or tissue samples to clarify the resistance mechanism is
important to guide further treatment. The molecular targets and
resistance mechanisms of different generations of EGFR-TKIs are
shown in Table I. Comprehensive
and in-depth studies on the resistance to the 3rd-generation
EGFR-TKIs are urgently required to provide better therapeutic
strategies.
The present review summarizes the emerging evidence
on mechanisms of 3rd-generation EGFR-TKI resistance in advanced
NSCLC, and outlines the latest clinical strategies used to overcome
this problem.
In addition to osimertinib, several other
3rd-generation EGFR-TKIs targeting the T790M mutation (Fig. 1), such as rociletinib (CO1686),
lazertinib (YH25448), abivertinib (AC0010), nazartinib (EGF816),
naquotinib (ASP8273) and olmutinib (HM61713), are at various stages
of development (Table I)
(17,20-33). Osimertinib, rociletinib and
olmutinib are currently approved for clinical use by the U.S. FDA.
Osimertinib has dominated the global landscape of treatment of
EGFR-positive NSCLC, since it is the current standard of
care for the 1st-line treatment of advanced EGFR-mutated
NSCLC and for EGFR T790M-positive NSCLC after 1st- or
2nd-generation EGFR-TKIs (17,19).
In 2015, the FDA approved osimertinib for the
treatment of patients with metastatic EGFR-mutant NSCLC who
have acquired the EGFR T790M resistance mutation. The drug
was then approved as the 1st-line therapy for advanced EGFR-mutated
NSCLC in 2018 (34). Osimertinib
is an oral, irreversible EGFR-TKI that is selective for both
EGFR and T790M mutations and has activity in the central
nervous system (CNS). AURA3 is a randomized, open-label, phase 3
trial that has been conducted to show the superiority of
osimertinib over platinum therapy plus pemetrexed in patients with
T790M-positive advanced NSCLC after 1st-generation EGFR-TKI
therapy. The results showed that the median PFS time was
significantly longer with osimertinib than that with platinum
therapy plus pemetrexed (10.1 vs. 4.4 months; HR, 0.30; 95% CI,
0.23-0.41; P<0.001), which establish a standard protocol for the
treatment of EGFR T790M-positive patients after failure of
1st-generation EGFR-TKI therapy, as well as targeted therapy for
brain metastasis (17). The
double-blind, phase 3 FLAURA trial compared the efficacy and safety
of osimertinib with the standard EGFR-TKIs (gefitinib or erlotinib)
in patients with untreated EGFR mutation-positive advanced
NSCLC. It demonstrated that the median PFS time of untreated
patients with EGFR mutation was significantly longer
following osimertinib administration compared with that following
gefitinib or erlotinib administration (18.9 vs. 10.2 months; HR,
0.80; 95% CI, 0.37-0.57; P<0.001) (19), as was the median OS time (38.6 vs.
31.8 months; HR, 0.46; 95% CI, 0.64-1.00; P=0.046) (35). In patients with measurable brain
metastases, the objective response rate (ORR) was 91% with
osimertinib versus 68% with the 1st-generation EGFR-TKIs (odds
ratio, 4.6; 95% CI, 0.9-34.9; P=0.066) (36). Several studies have investigated
the safety and efficacy of EGFR-TKIs in combination with other
targeted therapies (37-39). The phase Ib TATTON study assessed
the safety and tolerability of osimertinib in combination with
selumetinib (MEK inhibitor), savolitinib [hepatocyte growth factor
receptor (MET) inhibitor] or durvalumab, a human anti-programmed
cell death-ligand-1 (PD-L1) antibody. The ORR in the selumetinib,
savolitinib and durvalumab arms was 42, 44 and 43%, respectively
(39).
Overall, osimertinib is a promising 3rd-generation
EGFR-TKI in current lung cancer treatment regimens, and
osimertinib-based combination therapy deserves broad investigations
to improve outcomes in patients with advanced EGFR-mutated
NSCLC.
Rociletinib (CO1686) is a small-molecule, orally
administered and irreversibly selective EGFR-TKI that inhibits
EGFR mutations, including Ex19del, L858R and T790M, but not
exon 20 insertion (e20ins) (26).
The TIGER-X trial (phase I/II study) and the TIGER-2 trial (phase
II, open-label, multi-center study) evaluated the safety and
efficacy of rociletinib in previously treated patients with
EGFR-mutated NSCLC. A total of 130 patients were enrolled in
the TIGER-X study. Of the 46 evaluable T790M patients, the ORR was
59% (95% CI, 45-73), and the estimated median PFS time was 13.1
months (95% CI, 5.4-13.1) (26).
However, results of the TIGER-X and TIGER-2 trials using a pooled
cohort of patients found that the rate of confirmed response was
28-34% for rociletinib, which significantly differed from the
result of the TIGER-X trial. After independent analysis, the
maturation confirmation response rate was updated to 45% and the
median PFS time to 6.1 months (20). Sequist et al (40) reported that 9 patients with
progression on rociletinib were subsequently treated with
osimertinib. Among them, 2 patients exhibited a partial response, 3
presented with stable disease and 4 developed progressive disease.
The 3 patients with brain metastasis after rociletinib treatment
also showed improvement in CNS disease response to osimertinib. The
development of rociletinib was terminated on May 6, 2016, due to a
lower efficacy than osimertinib and incidences of adverse events
such as high-grade hyperglycemia and corrected QT interval
prolongation (41).
Abivertinib (AC0010) is one of the 3rd-generation
EGFR-TKIs developed in China; it is a pyrrolopyrimidine compound,
which is highly selective, irreversible and potent (42). A phase I study of abivertinib
presented significant clinical benefits and a good safety profile
in patients with NSCLC and acquired resistance to the
1st-generation EGFR-TKIs. The ORR in patients with T790M mutation
was 42%, and the median PFS time estimated by Kaplan-Meier ranged
between 14.0 and 35.6 weeks in those patients receiving a daily
dose of 350-600 mg (42). A phase
I, open, multicenter study explored the efficacy of abivertinib in
patients with NSCLC and CNS metastasis. The median intracranial PFS
time was 142 days (95% CI, 31.1-252.9) in 7 patients with brain
metastasis, suggesting that abivertinib had good control of
asymptomatic brain metastasis (43). A recent study reported that 9
patients received osimertinib treatment after progression on
abiverinib, with a median total treatment duration of 15.9 months
(95% CI, 12.5-19.3) (27). These
results have demonstrated that osimertinib might be an option for
subsequent therapy in patients with disease progression after
abivertinib treatment. Further studies on abivertinib are required
to investigate its interaction with osimertinib.
Several other 3rd-generation EGFR-TKIs are also
under development. Nazartinib (EGF816) is a covalent and
irreversible EGFR-TKI. Preliminary results from an open-label,
multicenter, phase I/II study of 180 patients at 9 academic medical
centers in Europe, Asia and North America demonstrated that
nazartinib had an excellent safety profile, with low dermal
toxicity and a primary adverse event of maculopapular rash (40%)
(28). Olmutinib (HM61713),
approved by the FDA in December 2015 for the treatment of NSCLC,
has potent inhibitory activity against L858R/T790M mutant NSCLC
cells (44). In a recently
published single-arm, open-label, phase I/II trial, EGFR
T790M-positive patients receiving olmutinib (800 mg/day) had an ORR
of 55% (38/69 evaluable patients; 95% CI, 42.6-67.1) and an
estimated median PFS time of 6.9 months (95% CI, 5.6-9.7). The
common adverse events included diarrhea (59%), pruritus (42%), rash
(41%) and nausea (40%) (29). On
September 30, 2016, two cases of toxic epidermal
necrolysis/Stevens-Johnson syndrome, one of which was fatal, were
reported in a phase II trial of olmutinib in South Korea. On April
13, 2018, the development of olmutinib was terminated (41). Alflutinib (AST2818) is a newly
developed 3rd-generation EGFR-TKI; its ORR was 77% (89 out of 116
patients), and 9% of patients (11 out of 130 patients) experienced
grade 3 or higher drug-related adverse events (30). Almonertinib, a 3rd-generation
EGFR-TKI developed in China, has also shown good efficacy in the
treatment of T790M-positive NSCLC after EGFR-TKI resistance. In a
phase II trial, it exhibited a median PFS time of 12.3 months, an
ORR of 69% and acceptable toxicity. On March 19, 2020, almonertinib
was approved by the Center for Drug Evaluation of the China
National Medical Products Administration (31). Phase I/II clinical studies on
lazertinib showed that lazertinib had a favorable safety profile
and exhibited promising antitumor activity in patients with
EGFR T790M-positive NSCLC, with a median PFS time of 11.0
months and an ORR of 58%. Lazertinib was approved for EGFR
T790M-positive NSCLC in South Korea in 2021 (21,32). Naquotinib has anti-tumor activity
in preclinical models of EGFR-mutant NSCLC that targets
mutant EGFR, including EGFR T790M. In phase I trials,
it had an ORR of 31% against T790M-positive NSCLC. However, the
phase III clinical trial of naquotinib was terminated due to
toxicity and limited predicted efficacy (24,33). Further investigations on
3rd-generation EGFR-TKIs are still ongoing.
Similar to chemotherapy-associated resistance,
resistance to EGFR-TKIs includes both primary (intrinsic) and
acquired (secondary) types. The primary type is generally defined
as resistance that is present prior to the EGFR-TKI treatment.
There are few studies related to primary resistance, and the
mechanisms are unclear. Possible causes include EGFR e20ins
and B-cell lymphoma-2 (BCL-2)-like 11 (BIM) deletion
polymorphism.
EGFR e20ins occur in ~3% of lung adenocarcinoma
patients and 9% of EGFR-mutated tumors. EGFR e20ins block EGFR-TKI
binding to EGFR target sites, leading to primary resistance
(45). For patients with EGFR
e20ins, the overall effectiveness of 1st-line treatment with 1st-
and 2nd-generation EGFR-TKIs is 3-8%, with a median PFS time of
only 2 months. An in vitro study showed that NSCLC cells
stably expressing EGFR e20ins were resistant to the 3rd-generation
EGFR-TKIs, suggesting that EGFR e20ins might be primary mechanisms
of 3rd-generation EGFR-TKI resistance (46). Qin et al (47) demonstrated that p.A767_V769dup
(25%) and p.S768_D770dup (18%) were the 2 most common EGFR e20ins,
accounting for 44% of cases and serving as primary targets for
future drug development. In addition, different EGFR e20ins might
be associated with different outcomes in patients with advanced
NSCLC. p.A763_Y764insFQEA conferred better PFS times than the other
e20ins when patients were treated with various EGFR-TKIs, while
p.S768_D770dup showed a limited response and p.D770delinsGY
patients experienced a short PFS time. Therefore, it is important
to select the appropriate EGFR-TKIs according to the specific EGFR
e20in type (47). van Veggel
et al (48) reported that
osimertinib (80 or 160 mg/day) treatment had an ORR of 5% and a
median PFS time of 3.6 months (95% CI, 2.6-4.5) in 21 patients with
advanced NSCLC and EGFR e20ins (48). Phase II clinical studies on
osimertinib for EGFR e20ins in NSCLC are currently underway
(NCT03414814 and NCT03191149).
Acquired resistance refers to the evading effects of
EGFR-TKIs in tumor cells via alteration of their metabolic pathways
after exposure to the drugs. With the application of NGS-based
genomic profiling, the mechanisms of 3rd-generation EGFR-TKI
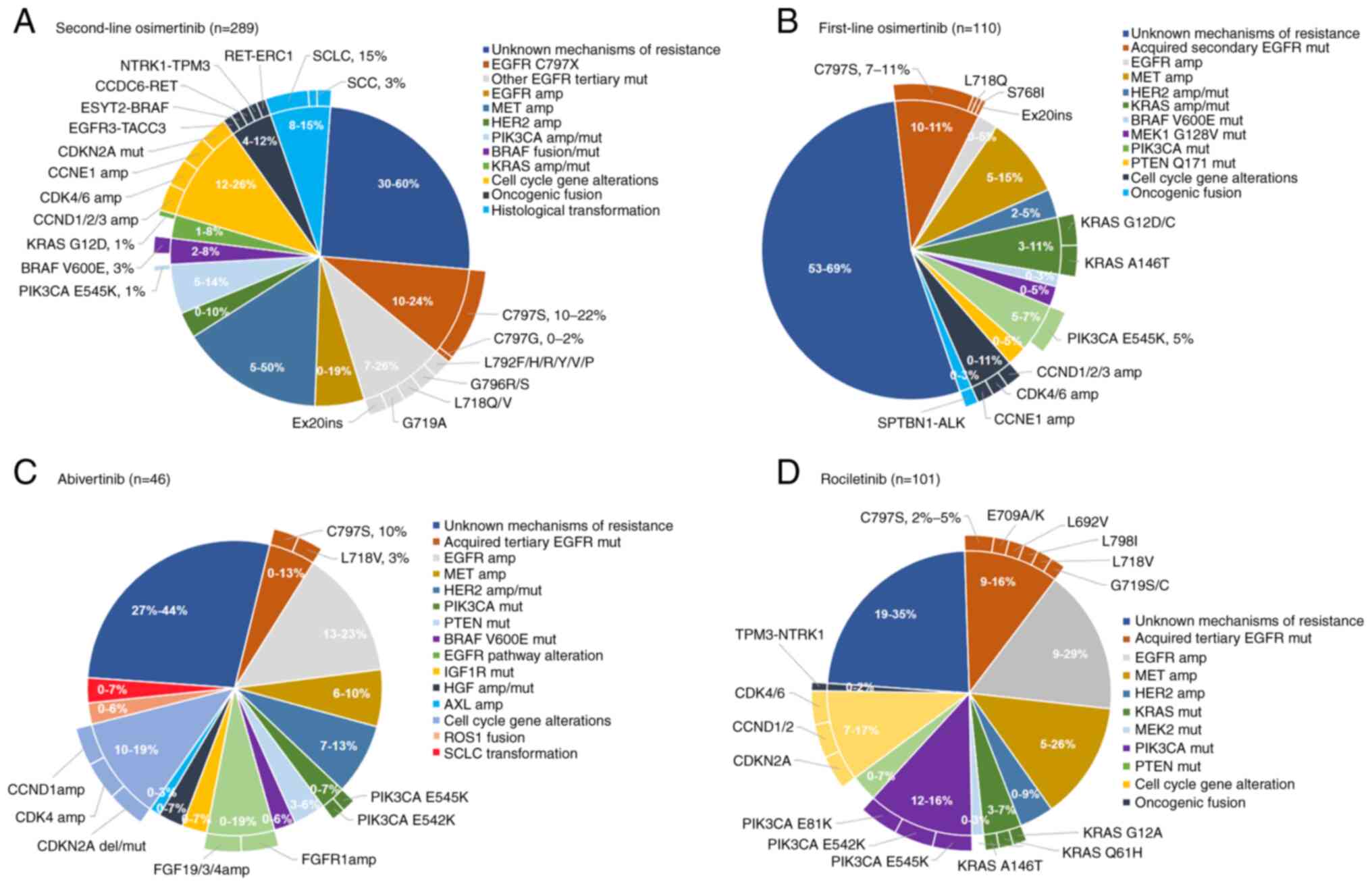
resistance have been extensively studied. The acquired resistance
of osimertinib as the 2nd- and 1st-line therapy (54-60), as well as rociletinib and
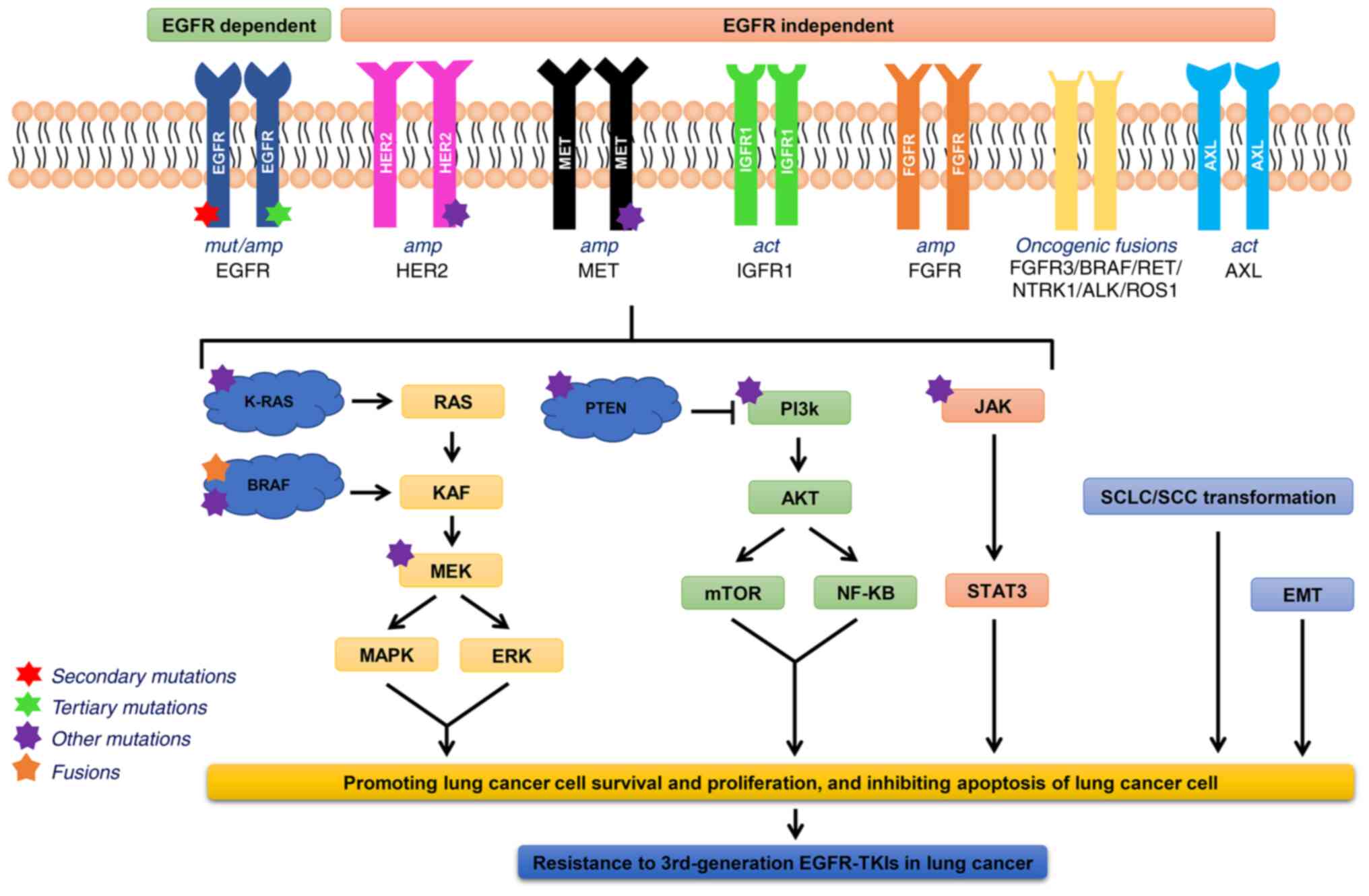
abivertinib (42,61-63), is summarized in Fig. 3. The mechanisms of acquired
resistance to 3rd-generation EGFR-TKIs include an altered EGFR
signaling pathway, aberrant activation of bypass and downstream
signaling pathways, and histological transformation. The molecular
mechanisms are depicted in Fig.
4.
Patients enrolled in the AURA3 study all developed
the T790M mutation after the 1st-line treatment with 1st- or
2nd-generation EGFR-TKIs, and 49% (36/73) of them had loss of T790M
after osimertinib resistance (54). The frequency of T790M mutation
loss in osimertinib-resistant patients in the studies by Le et
al (56) and Oxnard et
al (57) was 53% (21/40) and
68% (28/41), respectively. Oxnard et al (57) conducted tumor biopsies for genomic
analysis in 41 patients, and suggested that the loss of T790M was
associated with a small decrease in EGFR-activating
mutations after 1-3 weeks of treatment. Another recent study
demonstrated a markedly shorter median PFS time in the T790M-loss
group than that in the T790M group (5.93 vs. 11.87 months,
P=0.0004). Loss of T790M mutation was correlated with earlier
disease progression and worse survival in the osimertinib-resistant
patients (70). In addition, the
loss of T790M was present in 50% (6/12) of patients resistant to
rociletinib (71). In T790M
cases, the resistant mechanism is mostly related to C797S mutation
or bypass pathway activation, while patients without T790M often
show EGFR-independent mechanisms (56,71).
Amplification of c-Met plays an important role in
1st- and 3rd-generation EGFR-TKI resistance; it functions as a
transmembrane receptor tyrosine kinase. When hepatocyte growth
factor ligands bind to c-Met, c-Met is activated, inducing
homodimerization and phosphorylation of intracellular tyrosine
residues, which activates the downstream RAS/ERK/MAPK and PI3K-AKT
signaling pathways (73,74). These pathways can drive cell
survival, proliferation, motility, migration, invasion,
angiogenesis and epithelial-mesenchymal transition (EMT), providing
a bypass pathway in the presence of an EGFR inhibitor (73,74). The AURA3 study showed that 19%
(14/73) of patients developed MET gene amplification after
the 2nd-line treatment with osimertinib, which is the second most
common cause of resistance following the C797S mutation (54). Moreover, the incidence of
MET amplification was 14% (6/42) in the study by Le et
al (56). In the FLAURA
study, 15% (14/91) of patients resistant to osimertinib developed
MET amplification, exceeding the 7% (6/91) of the C797S
mutation (59). MET
amplification might be the most common cause of resistance when
osimertinib is used as 1st-line treatment. It is also one of the
most common resistance mechanisms to rociletinib, occurring in
8-26% of rociletinib-resistant patients (62,63). In the abivertinib-resistant
cohort, MET amplification was detected in 3 (10%) patients
(61).
FGFR signaling pathways regulate cell
proliferation, migration, cycle progression, metabolism and
survival (76). Kim et al
(77) found that FGFR1
amplification and FGF2 expression were upregulated in patients
resistant to osimertinib, suggesting that the FGF2-FGFR1 autocrine
loop might be associated with osimertinib resistance (77). The plasma-based circulating tumor
DNA (ctDNA) assay revealed that the FGFR3-TACC3 fusion
mutation was present in patients with the T790M mutation, and
disease progression occurred upon osimertinib and naquotinib
treatment (78). These results
suggested that abnormalities of the FGFR signaling pathway might
contribute to 3rd-generation EGFR-TKI resistance.
IGF1R is present in numerous cell types in various
tissues, such as muscle, cartilage, bone and brain; it is a
tyrosine kinases receptor that is involved in the pathogenesis and
progression of various malignancies, including lung cancer
(79). Abnormalities of IGF1R
confer resistance to 3rd-generation EGFR-TKIs by activating the
EGFR bypass signaling pathway (79). Manabe et al (80) demonstrated for the first time that
IGF2 autocrine-mediated activation of the IGF1R pathway in lung
cancer cells was involved in osimertinib resistance.
Immunohistochemistry confirmed the increased IGF2 expression in
lung cancer patients with acquired osimertinib resistance (80). Phosphate-receptor tyrosine kinase
array analysis of osimertinib-resistant cells showed that IGF1R was
activated in PC9/T790M/AZDR and H1975/AZDR cells. Inhibition of
IGF1R activation by small interfering RNA or linstinib (IGF1R
inhibitor) significantly restored osimertinib sensitivity,
suggesting that aberrant IGF1R activation might be one of the
causes of 3rd-generation EGFR-TKI resistance (79).
AXL is a member of the receptor tyrosine kinases,
which are involved in the regulation of cell survival,
proliferation, migration and metabolism. A study by Taniguchi et
al (81) demonstrated that
the overexpression of AXL was associated with a poor response to
osimertinib. This study showed that osimertinib stimulated AXL by
inhibiting the feedback inhibition of SPRY4. Activated AXL
interacted with EGFR and HER3 to maintain cell survival and induced
osimertinib resistance, which could be delayed by AXL inhibitors
(81). Another study demonstrated
that AXL was upregulated in osimertinib-resistant lung
adenocarcinoma cells. Osimertinib combined with cabozantinib (AXL
inhibitor) inhibited the growth of these cells both in vitro
and in vivo (82). In
addition, AXL amplification was also detected in
abivertinib-resistant patients (61). Therefore, AXL activation and
AXL amplification might also contribute to the primary and
acquired resistance to 3rd-generation EGFR-TKIs.
Acquired resistance to the 3rd-generation EGFR-TKIs
is associated with the activation of the RAS-MAPK pathway. BRAF is
a serine/threonine protein kinase, which regulates cell survival,
proliferation, differentiation and apoptosis, and plays a crucial
role in RAS/RAF/MEK/ERK pathways. Nakatani et al (83) observed KRAS overexpression in
osimertinib-resistant cells. One case (1%) in the AURA3 study had a
KRAS (G12D) mutation after resistance and 2 cases (3%) had
BRAF V600E mutations (54). KRAS Q61K mutation,
BRAF mutations and ESYT2-BRAF gene fusion have also
been detected in patients with acquired osimertinib resistance
(57). KRAS mutations in
the FLAURA study included A146T (1%), G12C (1%) and G12D (1%), and
the incidence of the BRAF V600E mutation was 3% (3/91)
(59).
The AURA3 and FLAURA studies demonstrated that the
frequency of cell cycle gene alterations was 11 and 12%,
respectively, in patients with disease progression after
osimertinib treatment as the 1st- or 2nd-line therapy (54,59). Both CCNE1 and CDK6
amplification occurred at a frequency of 7% (5/73) as the most
common cell cycle gene alterations in the AURA3 study (54). The most common cell cycle gene
alteration in the FLAURA study was CDK6 amplification (3%)
(59). In the study by Le et
al (56), CCND1,
CCNE1 and CDKN2A deletions were also found.
Alterations in cell cycle genes may be involved in the development
of osimertinib resistance.
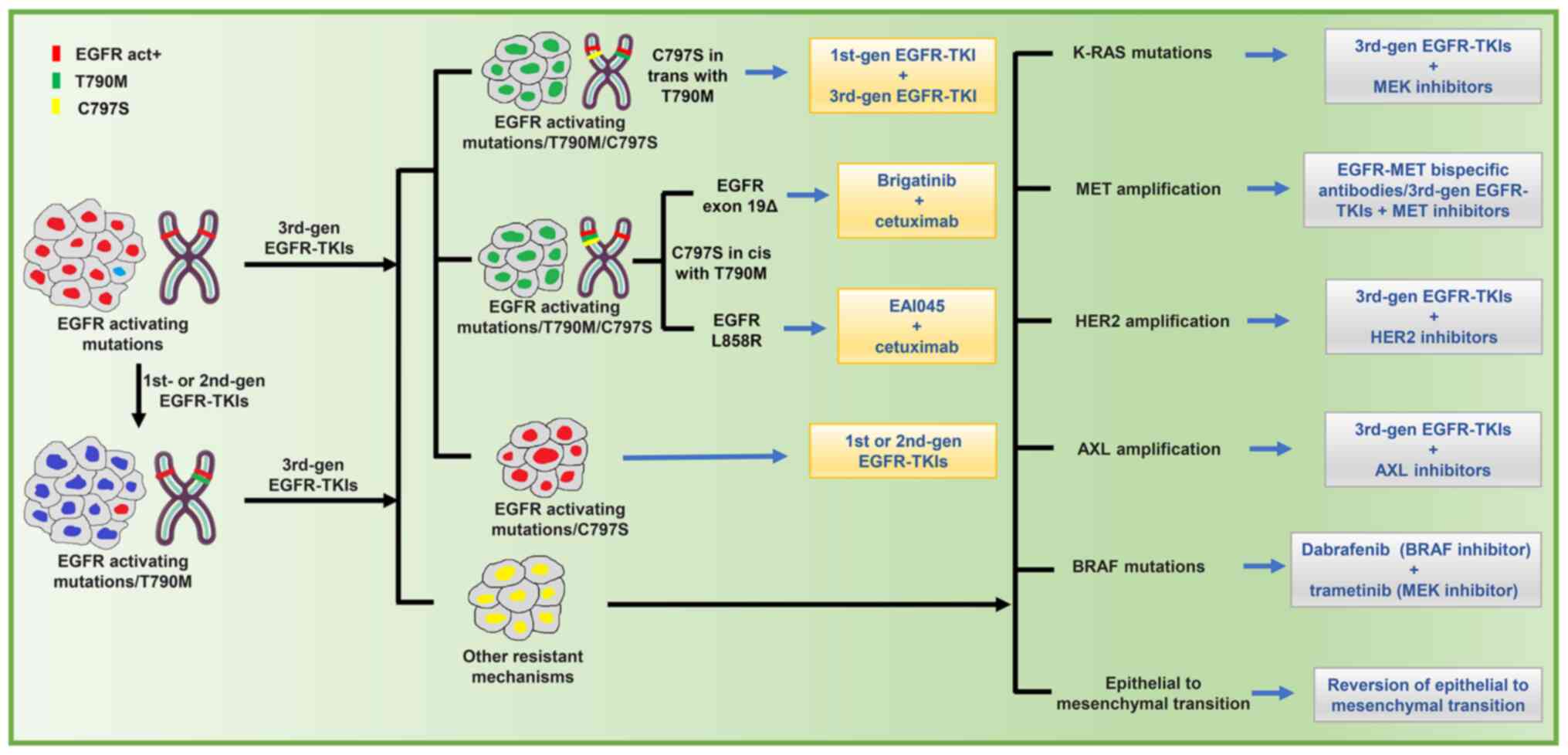
Scientists are exploring approaches to overcome the
different mechanisms of 3rd-generation EGFR-TKI resistance.
Combination of targeted therapies is a promising strategy. For the
reversion of 3rd-generation EGFR-TKI resistance, possible
strategies to overcome different mechanisms are shown in Fig. 5. Some representative
4th-generation EGFR-TKIs are summarized in Table I (91-95). Case reports and ongoing clinical
trials exploring the emerging combination are shown in Table II (84,89,96-104).
If the C797S and T790M mutations are cis-structured
(located in the same allele; 85%), patients are resistant to 1st-,
2nd- and 3rd-generation EGFR-TKIs (105). The 4th-generation EGFR-TKI,
EAI045, is the first selective, non-ATP-competitive allosteric TKI
targeting the L858R, T790M and C797S mutations (Fig. 1). However, EGFR dimerization
affects the efficacy of allosteric EGFR inhibitors. EAI045 is
ineffective when used alone. Cetuximab is a chimeric monoclonal
antibody that inhibits EGFR dimerization (91). EAI045 in combination with
cetuximab was demonstrated to significantly inhibit the
proliferation of lung cancer cells with EGFR
L858R/T790M/C797S mutations both in vitro and in
vivo. However, it was ineffective against drug resistance
caused by EGFR Ex19del/C797S/T790M mutation (91). Brigatinib, an ALK and EGFR
inhibitor, was effective against both EGFR
Ex19del/C797S/T790M and L858R/C797S/T790M mutant cells in
vitro and in vivo (96). Uchibori et al (92) demonstrated that brigatinib fits
into the ATP-binding pocket of triple-mutant EGFR. The
structure-activity relationship analysis revealed that the chloro,
phosphine oxide group and the methoxy group of brigatinib worked as
key components to inhibit the triple-mutant EGFR. The efficacy of
brigatinib was significantly enhanced when used in combination with
anti-EGFR antibody due to the reduction of surface and total EGFR
expression (92). A recent study
reported the cases of 15 osimertinib-resistant patients with
EGFR T790M-cis-C797S mutation, 5 of whom were treated with a
combination of brigatinib and cetuximab, and the remainder of whom
received cisplatin-based doublet chemotherapy. The median PFS time
was 14 and 3 months, respectively, with an ORR of 60 and 10%,
respectively (96). Blu-945 is a
4th-generation EGFR-TKI designed to target EGFR T790M/C797S
and T790M-resistant mutations. A recent study reported that BLU-945
alone or in combination with osimertinib significantly inhibited
osimertinib-resistant lung cancer cell growth both in vitro
and in vivo (93). TQB3804
is a 4th-generation EGFR-TKI developed in China (Fig. 1). A preclinical study showed that
TQB3804 exhibits a prominent inhibitory effect on the
Ex19del/T790M/C797S and L858R/T790M/C797S triple mutations
(94). A phase I clinical trial
of TQB3804 is currently recruiting (NCT04128085). More clinical
trials are required to validate the efficacy of the novel EGFR-TKIs
in patients with advanced NSCLC.
Currently, the studies on AXL inhibitors are mainly
at the preclinical stages, and there are few clinical trials. Okura
et al (114) demonstrated
that the novel AXL inhibitor ONO-7475 increased the sensitivity of
AXL-overexpressing NSCLC cells to osimertinib and suppressed the
emergence of osimertinib-resistant cells in vitro (114). Kim et al (115) found that promoting AXL
degradation in combination with osimertinib delayed or overcame
osimertinib resistance in EGFR-mutant patient-derived
xenograft models (115). In
addition, the newly developed drug CB469 inhibited both AXL and
c-Met activation and phosphorylation, thereby overcoming acquired
resistance to EGFR-TKIs mediated by AXL and c-Met activation both
in vitro and in vivo (116).
For drug resistance caused by RAS/RAF/MEK/ERK
signaling pathway activation, 3rd-generation EGFR-TKIs combined
with MEK inhibitors are potential therapeutic strategies.
Preclinical studies demonstrated that the combination of
osimertinib and selumetinib overcame the resistance caused by
KRAS amplification and overexpression (83). In another in vitro study,
MEK inhibitors restored the sensitivity of EGFR
ex19del/T790M/C797S-mutated PC9 cells to osimertinib by modulating
MEK/ERK-dependent degradation of BIM and MCL-1 (117). Osimertinib and MEK/ERK
inhibitors synergistically promoted apoptosis and inhibited
survival in osimertinib-resistant cells, and this combination could
delay the emergence of osimertinib resistance both in vitro
and in vivo (118). In
2017, the FDA approved the combination of dabrafenib (BRAF
V600E inhibitor) plus trametinib (MEK inhibitor) for the treatment
of patients with BRAF V600E mutations, with an ORR of 63 and
61%, respectively, for the 1st- and 2nd-line treatments (101). Xie et al (119) demonstrated that osimertinib
combined with vemurafenib was effective to overcome BRAF
V600E-mediated osimertinib resistance (119). More clinical trials are required
to validate the roles of RAS/RAF/MEK/ERK signaling pathway
inhibitors in osimertinib-resistant patients.
In a recent study, the 3rd-generation EGFR
inhibitor WZ-4002 and the FGFR inhibitor dovitinib synergistically
inhibited EMT-mediated resistant cell survival and prevented the
generation of resistant clones. It was shown that FGFR signaling is
critical for the emergence of mesenchymal-like drug tolerant
clones. Dual EGFR plus FGFR inhibition might be a promising
strategy to avoid resistance (120). Yochum et al (121) reported that the transcription
factor TWIST1 inhibitor harmine and the Bcl-2/BclXL inhibitor
ABT737 were able to target the EMT transcription factor TWIST1 in
EGFR-mutant NSCLC. The study demonstrated that downregulated
TWIST1 and upregulated BIM could overcome EMT- and BIM-mediated
drug resistance (121). Another
recent study demonstrated that combined treatment with osimertinib
and aspirin promoted BIM-dependent apoptosis in
osimertinib-resistant lung cancer cells. A retrospective analysis
of 45 patients with NSCLC also confirmed that the median PFS time
of the osimertinib plus aspirin group was significantly longer than
that of the osimertinib alone group (104).
VEGFR inhibitors have synergistic antitumor effects
with EGFR inhibitors. Phase I/II clinical trials of osimertinib in
combination with ramucirumab (128) or bevacizumab (129) in patients with advanced NSCLC
and EGFR mutations are ongoing. In addition, an open-label,
phase II, multicenter, single-arm trial is exploring the efficacy
of afatinib plus bevacizumab in patients with EGFR-mutant
NSCLC and osimertinib resistance (130).
A retrospective analysis showed that
anti-programmed cell death-1 (PD-1) monotherapy was poorly
effective in EGFR-mutated patients, even for patients with
PD-L1 expression ≥50% (131). In
phase Ib TATTON study, osimertinib in combination with durvalumab
had an ORR of 67% in patients with EGFR T790M mutation.
However, the incidence of interstitial lung disease was 38%
(132). The osimertinib plus
durvalumab combination arm of the TATTON study was suspended due to
severe adverse events. Immunotherapy combined with chemotherapy may
provide new hope for patients resistant to the 3rd-generation
EGFR-TKIs. A recent study reported that combined therapy of
toripalimab (anti-PD-1 anti-body) and pemetrexed/carboplatin
achieved a partial response for >8 months in a
osimertinib-resistant patient. A phase II clinical trial of
toripalimab combined with chemotherapy in patients without
EGFR T790M mutation achieved an ORR of 50% and a median PFS
time of 7.0 months (133).
Clinical trials of nivolumab (anti-PD-1 antibody) in combination
with chemotherapy or ipilimumab (anti-cytotoxic T
lymphocyte-associated antigen-4 antibody) (NCT02864251) and
pembrolizumab (anti-PD-1 antibody) in combination with chemotherapy
(NCT03515837) in patients who were resistant to the 1st- or
2nd-line treatment of osimertinib are currently underway.
For patients who developed SCLC transformation,
chemotherapy after osimertinib resistance is an option. Marcoux
et al (84) demonstrated
that patients with SCLC transformation had higher response rates to
etoposide, cisplatin and paclitaxel. For patients with unknown
resistant mechanisms, chemotherapy is still an option. If the
patient is asymptomatic or has symptomatic local progression,
osimertinib can be combined with local treatment according to
National Comprehensive Cancer Network (NCCN) guidelines (134). Furthermore,
carboplatin/paclitaxel/bevacizumab/atezolizumab (anti-PD-L1
antibody) are also options for patients who experience systemic
progression after osimertinib treatment (135). Whether chemotherapy can delay
resistance to the 3rd-generation EGFR-TKIs remains unknown. A study
on osimertinib with or without chemotherapy as the 1st-line
treatment in patients with EGFR-mutated NSCLC is currently
recruiting (NCT04035486).
The resistance mechanism of 3rd-generation
EGFR-TKIs for advanced NSCLC is very complex. The mechanism of
3rd-generation EGFR-TKI resistance in EGFR-mutated tumors is
different between patients, and heterogeneous among different tumor
sites. Therefore, NGS of blood-based ctDNA or tissue samples to
clarify the resistance mechanism is of importance to guide the next
treatment, which will be conducive to the clinical research of
novel combined therapy to overcome drug resistance. According to
the NCCN guidelines (version 4. 2021) (136), radical local therapy combined
with osimertinib continuation should be considered for patients who
progressed on osimertinib, except those who developed extensive
progression after resistance, for whom platinum-based two-drug
chemotherapy with or without bevacizumab is recommended. To improve
survival in patients with EGFR mutations, a range of new therapies
targeting different resistance mechanisms are being developed.
4th-generation EGFR-TKIs have emerged, such as EAI045, TQB3804 and
BLU-945, and the multi-target TKI brigatinib, showing high
potential and being worthy of attention with regard to targeting
EGFR T790M/C797S mutation. EAI045 is a representative of
allosteric EGFR-mutant selective compounds. A number of
other allosteric EGFR inhibitors, including JBJ-04-125-02 and
DDC-01-163, are currently in development. Studies have suggested
that EGFR dimerization affects the efficacy of allosteric EGFR
inhibitors, so it is more effective when allosteric EGFR inhibitors
are combined with osimertinib or EGFR-targeted monoclonal
antibodies (cetuximab), than when used as single agents.
Furthermore, the allogeneic EGFR inhibitors have potential to
improve the clinical efficacy of osimertinib and delay the
emergence of mutant EGFR-mediated resistance in NSCLC
(91,137,138). Receptor structure-based drug
design and library screening provides novel allogeneic EGFR
inhibitors. Combined therapy of allogeneic EGFR inhibitors with
conventional EGFR-TKIs, EGFR-targeted monoclonal antibodies,
chemotherapy or immunotherapy offers an effective treatment option
for patients with 3rd-generation EGFR-TKI-resistant NSCLC. More
preclinical and clinical studies are required to validate the
efficacy of combined therapies. The combinations of EGFR-TKIs with
agents targeting aberrant EGFR bypassing pathways, as well as
downstream pathways, are also promising to overcome EGFR-TKI
resistance. Mutations in some EGFR loci are insensitive to
conventional EGFR-TKIs, and the emergence of new agents such as
mobocertinib, amivantamab and poziotinib have shown promising
efficacy against EGFR e20ins. Recent studies have shown that
chemotherapy plus EGFR-TKIs or bevacizumab is superior to
chemotherapy alone in SCLC-transformed EGFR-mutant lung
adenocarcinoma. In addition, the rapid development of immunotherapy
has brought new hope for EGFR-TKI resistant patients. The
combination of immune checkpoint inhibitors, anti-angiogenic agents
and chemotherapy may be a promising research direction in future.
Although the combination of immunotherapy and EGFR-TKIs has
achieved satisfactory efficacy, serious adverse events have
hindered further promotion of clinical trials. The manner in which
the occurrence of adverse reactions can be reduced in the process
of combination therapy is an important concern. Most combined
therapies are still under development, several of which have shown
satisfactory results at the preclinical stage, but failed in
clinical trials. Therefore, more studies should be conducted in the
future to improve our understanding of the complex signaling
pathways involved in the resistance to 3rd-generation EGFR-TKIs and
to find the best combination treatments modality to overcome the
3rd-generation EGFR-TKI resistance under the guidance of NGS.
Not applicable.
JH, YG and CX were responsible for the study
conception and design. Administrative support was provided by YG
and CX. JH and ZH contributed to the provision of study materials
or patients. JH, ZH and LH collected and assembled the data, and
JH, ZH and LH were responsible for data analysis and
interpretation. All authors helped to write the manuscript and have
read and approved the final manuscript. Data authentication is not
applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Testa U, Castelli G and Pelosi E: Lung
cancers: Molecular characterization, clonal heterogeneity and
evolution, and cancer stem cells. Cancers (Basel). 10:2482018.
View Article : Google Scholar
|
|
3
|
Rosell R, Moran T, Queralt C, Porta R,
Cardenal F, Camps C, Majem M, Lopez-Vivanco G, Isla D, Provencio M,
et al: Screening for epidermal growth factor receptor mutations in
lung cancer. New Engl J Med. 361:958–967. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
da Cunha Santos G, Shepherd FA and Tsao
MS: EGFR mutations and lung cancer. Annu Rev Pathol. 6:49–69. 2011.
View Article : Google Scholar
|
|
5
|
Roskoski R Jr: Small molecule inhibitors
targeting the EGFR/ErbB family of protein-tyrosine kinases in human
cancers. Pharmacol Res. 139:395–411. 2019. View Article : Google Scholar
|
|
6
|
Huang L and Fu L: Mechanisms of resistance
to EGFR tyrosine kinase inhibitors. Acta Pharm Sin B. 5:390–401.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mok TS, Wu YL, Thongprasert S, Yang CH,
Chu DT, Saijo N, Sunpaweravong P, Han B, Margono B, Ichinose Y, et
al: Gefitinib or carboplatin-paclitaxel in pulmonary
adenocarcinoma. N Engl J Med. 361:947–957. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kazandjian D, Blumenthal GM, Yuan W, He K,
Keegan P and Pazdur R: FDA approval of gefitinib for the treatment
of patients with metastatic EGFR mutation-positive non-small cell
lung cancer. Clin Cancer Res. 22:1307–1312. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rosell R, Carcereny E, Gervais R,
Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R,
Pallares C, Sanchez JM, et al: Erlotinib versus standard
chemotherapy as first-line treatment for European patients with
advanced EGFR mutation-positive non-small-cell lung cancer
(EURTAC): A multicentre, open-label, randomised phase 3 trial.
Lancet Oncol. 13:239–246. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shi YK, Wang L, Han BH, Li W, Yu P, Liu
YP, Ding CM, Song X, Ma ZY, Ren XL, et al: First-line icotinib
versus cisplatin/pemetrexed plus pemetrexed maintenance therapy for
patients with advanced EGFR mutation-positive lung adenocarcinoma
(CONVINCE): A phase 3, open-label, randomized study. Ann Oncol.
28:2443–2450. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Park K, Tan EH, O'Byrne K, Zhang L, Boyer
M, Mok T, Hirsh V, Yang JC, Lee KH, Lu S, et al: Afatinib versus
gefitinib as first-line treatment of patients with EGFR
mutation-positive non-small-cell lung cancer (LUX-Lung 7): A phase
2B, open-label, randomised controlled trial. Lancet Oncol.
17:577–589. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wu YL, Cheng Y, Zhou X, Lee KH, Nakagawa
K, Niho S, Tsuji F, Linke R, Rosell R, Corral J, et al: Dacomitinib
versus gefitinib as first-line treatment for patients with
EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): A
randomised, open-label, phase 3 trial. Lancet Oncol. 18:1454–1466.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Miller VA, Hirsh V, Cadranel J, Chen YM,
Park K, Kim SW, Zhou C, Su WC, Wang M, Sun Y, et al: Afatinib
versus placebo for patients with advanced, metastatic
non-small-cell lung cancer after failure of erlotinib, gefitinib,
or both, and one or two lines of chemotherapy (LUX-Lung 1): A phase
2b/3 randomised trial. Lancet Oncol. 13:528–538. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ellis PM, Shepherd FA, Millward M, Perrone
F, Seymour L, Liu G, Sun S, Cho BC, Morabito A, Leighl NB, et al:
Dacomitinib compared with placebo in pretreated patients with
advanced or metastatic non-small-cell lung cancer (NCIC CTG BR.26):
A double-blind, randomised, phase 3 trial. Lancet Oncol.
15:1379–1388. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Westover D, Zugazagoitia J, Cho BC, Lovly
CM and Paz-Ares L: Mechanisms of acquired resistance to first- and
second-generation EGFR tyrosine kinase inhibitors. Ann Oncol.
29(Suppl-1): i10–i19. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Passaro A, Guerini-Rocco E, Pochesci A,
Vacirca D, Spitaleri G, Catania CM, Rappa A, Barberis M and de
Marinis F: Targeting EGFR T790M mutation in NSCLC: From biology to
evaluation and treatment. Pharmacol Res. 117:406–415. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim
HR, Ramalingam SS, Shepherd FA, He Y, Akamatsu H, Theelen WS, et
al: Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung
cancer. New Engl J Med. 376:629–640. 2017. View Article : Google Scholar
|
|
18
|
Cross DA, Ashton SE, Ghiorghiu S, Eberlein
C, Nebhan CA, Spitzler PJ, Orme JP, Finlay MR, Ward RA, Mellor MJ,
et al: AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated
resistance to EGFR inhibitors in lung cancer. Cancer Discov.
4:1046–1061. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Soria JC, Ohe Y, Vansteenkiste J,
Reungwetwattana T, Chewaskulyong B, Lee KH, Dechaphunkul A, Imamura
F, Nogami N, Kurata T, et al: Osimertinib in untreated EGFR-mutated
advanced non-small-cell lung cancer. New Engl J Med. 378:113–125.
2018. View Article : Google Scholar
|
|
20
|
Sequist LV, Soria JC and Camidge DR:
Update to rociletinib data with the RECIST confirmed response rate.
New Engl J Med. 374:2296–2297. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yun J, Hong MH, Kim SY, Park CW, Kim S,
Yun MR, Kang HN, Pyo KH, Lee SS, Koh JS, et al: YH25448, an
irreversible EGFR-TKI with potent intracranial activity in EGFR
mutant non-small cell lung cancer. Clin Cancer Res. 25:2575–2587.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xu X, Mao L, Xu W, Tang W, Zhang X, Xi B,
Xu R, Fang X, Liu J, Fang C, et al: AC0010, an irreversible EGFR
inhibitor selectively targeting mutated EGFR and overcoming
T790M-induced resistance in animal models and lung cancer patients.
Mol Cancer Ther. 15:2586–2597. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jia Y, Juarez J, Li J, Manuia M, Niederst
MJ, Tompkins C, Timple N, Vaillancourt MT, Pferdekamper AC,
Lockerman EL, et al: EGF816 exerts anticancer effects in non-small
cell lung cancer by irreversibly and selectively targeting primary
and acquired activating mutations in the EGF receptor. Cancer Res.
76:1591–1602. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yu HA, Spira A, Horn L, Weiss J, West H,
Giaccone G, Evans T, Kelly RJ, Desai B, Krivoshik A, et al: A phase
I, dose escalation study of oral ASP8273 in patients with non-small
cell lung cancers with epidermal growth factor receptor mutations.
Clin Cancer Res. 23:7467–7473. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Park K, Lee JS, Lee KH, Kim JH, Min YJ,
Cho JY, Han JY, Kim BS, Kim JS, Lee DH, et al: Updated safety and
efficacy results from phase I/II study of HM61713 in patients (pts)
with EGFR mutation positive non-small cell lung cancer (NSCLC) who
failed previous EGFR-tyrosine kinase inhibitor (TKI). J Clin Oncol.
33(Suppl 15): S80842015. View Article : Google Scholar
|
|
26
|
Sequist LV, Rolfe L and Allen AR:
Rociletinib in EGFR-mutated non-small-cell lung cancer. New Engl J
Med. 373:578–579. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang H, Pan R, Zhang X, Si X, Wang M and
Zhang L: Abivertinib in patients with T790M-positive advanced NSCLC
and its subsequent treatment with osimertinib. Thorac Cancer.
11:594–602. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tan DS, Leighl NB, Riely GJ, Yang JC,
Sequist LV, Wolf J, Seto T, Felip E, Aix SP, Jonnaert M, et al:
Safety and efficacy of nazartinib (EGF816) in adults with
EGFR-mutant non-small-cell lung carcinoma: A multicentre,
open-label, phase 1 study. Lancet Resp Med. 8:561–572. 2020.
View Article : Google Scholar
|
|
29
|
Kim DW, Lee DH, Han JY, Lee J, Cho BC,
Kang JH, Lee KH, Cho EK, Kim JS, Min YJ, et al: Safety,
tolerability, and anti-tumor activity of olmutinib in non-small
cell lung cancer with T790M mutation: A single arm, open label,
phase 1/2 trial. Lung Cancer. 135:66–72. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shi Y, Zhang S, Hu X, Feng J, Ma Z, Zhou
J, Yang N, Wu L, Liao W, Zhong D, et al: Safety, clinical activity,
and pharmacokinetics of alflutinib (AST2818) in patients with
advanced NSCLC With EGFR T790M mutation. J Thorac Oncol.
15:1015–1026. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yang JC, Camidge DR, Yang CT, Zhou J, Guo
R, Chiu CH, Chang GC, Shiah HS, Chen Y, Wang CC, et al: Safety,
efficacy, and pharmacokinetics of almonertinib (HS-10296) in
pretreated patients with EGFR-mutated advanced NSCLC: A
multicenter, open-label, phase 1 Trial. J Thorac Oncol.
15:1907–1918. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ahn MJ, Han JY, Lee KH, Kim SW, Kim DW,
Lee YG, Cho EK, Kim JH, Lee GW, Lee JS, et al: Lazertinib in
patients with EGFR mutation-positive advanced non-small-cell lung
cancer: Results from the dose escalation and dose expansion parts
of a first-in-human, open-label, multicentre, phase 1-2 study.
Lancet Oncol. 20:1681–1690. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kelly RJ, Shepherd FA, Krivoshik A, Jie F
and Horn L: A phase III, randomized, open-label study of ASP8273
versus erlotinib or gefitinib in patients with advanced stage
IIIB/IV non-small-cell lung cancer. Ann Oncol. 30:1127–1133. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Mezquita L, Varga A and Planchard D:
Safety of osimertinib in EGFR-mutated non-small cell lung cancer.
Expert Opin Drug Saf. 17:1239–1248. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ramalingam SS, Vansteenkiste J, Planchard
D, Cho BC, Gray JE, Ohe Y, Zhou C, Reungwetwattana T, Cheng Y,
Chewaskulyong B, et al: Overall Survival with Osimertinib in
Untreated, -Mutated Advanced NSCLC. New Engl J Med. 382:41–50.
2020. View Article : Google Scholar
|
|
36
|
Reungwetwattana T, Nakagawa K, Cho BC,
Cobo M, Cho EK, Bertolini A, Bohnet S, Zhou C, Lee KH, Nogami N, et
al: CNS response to osimertinib versus standard epidermal growth
factor receptor tyrosine kinase inhibitors in patients with
untreated EGFR-mutated advanced non-small-cell lung cancer. J Clin
Oncol. Aug 28–2018.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Saito H, Fukuhara T, Furuya N, Watanabe K,
Sugawara S, Iwasawa S, Tsunezuka Y, Yamaguchi O, Okada M, Yoshimori
K, et al: Erlotinib plus bevacizumab versus erlotinib alone in
patients with EGFR-positive advanced non-squamous non-small-cell
lung cancer (NEJ026): Interim analysis of an open-label,
randomised, multicentre, phase 3 trial. Lancet Oncol. 20:625–635.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Goldberg SB, Redman MW, Lilenbaum R,
Politi K, Stinchcombe TE, Horn L, Chen EH, Mashru SH, Gettinger SN,
Melnick MA, et al: Randomized trial of afatinib plus cetuximab
versus afatinib alone for first-line treatment of -mutant
non-small-cell lung cancer: Final results from SWOG S1403. J Clin
Oncol. 38:4076–4085. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Oxnard GR, Yang JC, Yu H, Kim SW, Saka H,
Horn L, Goto K, Ohe Y, Mann H, Thress KS, et al: TATTON: A
multi-arm, phase Ib trial of osimertinib combined with selumetinib,
savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann Oncol.
31:507–516. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Sequist LV, Piotrowska Z, Niederst MJ,
Heist RS, Digumarthy S, Shaw AT and Engelman JA: Osimertinib
responses after disease progression in patients who had been
receiving rociletinib. JAMA Oncol. 2:541–543. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nagasaka M, Zhu VW, Lim SM, Greco M, Wu F
and Ou SI: Beyond osimertinib: The development of third-generation
EGFR tyrosine kinase inhibitors for advanced EGFR+
NSCLC. J Thorac Oncol. 16:740–763. 2021. View Article : Google Scholar
|
|
42
|
Ma Y, Zheng X, Zhao H, Fang W, Zhang Y, Ge
J, Wang L, Wang W, Jiang J, Chuai S, et al: First-in-human phase I
study of AC0010, a mutant-selective EGFR inhibitor in non-small
cell lung cancer: Safety, efficacy, and potential mechanism of
resistance. J Thorac Oncol. 13:968–977. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang H, Zhang L, Hu P, Zheng X, Si X,
Zhang X and Wang M: Penetration of the blood-brain barrier by
avitinib and its control of intra/extra-cranial disease in
non-small cell lung cancer harboring the T790M mutation. Lung
Cancer. 122:1–6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kim ES: Olmutinib: First global approval.
Drugs. 76:1153–1157. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Arcila ME, Nafa K, Chaft JE, Rekhtman N,
Lau C, Reva BA, Zakowski MF, Kris MG and Ladanyi M: EGFR exon 20
insertion mutations in lung adenocarcinomas: Prevalence, molecular
heterogeneity, and clinicopathologic characteristics. Mol Cancer
Ther. 12:220–229. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Robichaux JP, Elamin YY, Tan Z, Carter BW,
Zhang S, Liu S, Li S, Chen T, Poteete A, Estrada-Bernal A, et al:
Mechanisms and clinical activity of an EGFR and HER2 exon
20-selective kinase inhibitor in non-small cell lung cancer. Nat
Med. 24:638–646. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Qin Y, Jian H, Tong X, Wu X, Wang F, Shao
YW and Zhao X: Variability of EGFR exon 20 insertions in 24 468
Chinese lung cancer patients and their divergent responses to EGFR
inhibitors. Mol Oncol. 14:1695–1704. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
van Veggel B, Madeira R, Santos JFV,
Hashemi SMS, Paats MS, Monkhorst K, Heideman DAM, Groves M, Radonic
T, Smit EF, et al: Osimertinib treatment for patients with EGFR
exon 20 mutation positive non-small cell lung cancer. Lung Cancer.
141:9–13. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Li X, Wang S, Li B, Wang Z, Shang S, Shao
Y, Sun X and Wang L: BIM deletion polymorphism confers resistance
to osimertinib in EGFR T790M lung cancer: A case report and
literature review. Target Oncol. 13:517–523. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhao M, Zhang Y, Cai W, Li J, Zhou F,
Cheng N, Ren R, Zhao C, Li X, Ren S, et al: The Bim deletion
polymorphism clinical profile and its relation with tyrosine kinase
inhibitor resistance in Chinese patients with non-small cell lung
cancer. Cancer. 120:2299–2307. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Tanimoto A, Takeuchi S, Arai S, Fukuda K,
Yamada T, Roca X, Ong ST and Yano S: Histone deacetylase 3
inhibition overcomes BIM deletion polymorphism-mediated osimertinib
resistance in EGFR-mutant lung cancer. Clin Cancer Res.
23:3139–3149. 2017. View Article : Google Scholar
|
|
52
|
Isobe K, Hata Y, Tochigi N, Kaburaki K,
Kobayashi H, Makino T, Otsuka H, Sato F, Ishida F, Kikuchi N, et
al: Clinical significance of BIM deletion polymorphism in
non-small-cell lung cancer with epidermal growth factor receptor
mutation. J Thorac Oncol. 9:483–487. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Liu SY, Zhou JY, Li WF, Sun H, Zhang YC,
Yan HH, Chen ZH, Chen CX, Ye JY, Yang JJ, et al: Concomitant
genetic alterations having greater impact on the clinical benefit
of EGFR-TKIs in EGFR-mutant advanced NSCLC than BIM deletion
polymorphism. Clin Transl Med. 10:337–345. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Papadimitrakopoulou VA, Wu YL, Han JY, Ahn
MJ, Ramalingam SS, John T, Okamoto I, Yang JCH, Bulusu KC, Laus G,
et al: Analysis of resistance mechanisms to osimertinib in patients
with EGFR T790M advanced NSCLC from the AURA3 study. Ann Oncol.
29(Suppl 8): VIII7412018. View Article : Google Scholar
|
|
55
|
Yang Z, Yang N, Ou Q, Xiang Y, Jiang T, Wu
X, Bao H, Tong X, Wang X, Shao YW, et al: Investigating novel
resistance mechanisms to third-generation EGFR tyrosine kinase
inhibitor osimertinib in non-small cell lung cancer patients. Clin
Cancer Res. 24:3097–3107. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Le X, Puri S, Negrao MV, Nilsson MB,
Robichaux J, Boyle T, Hicks JK, Lovinger KL, Roarty E,
Rinsurongkawong W, et al: Landscape of EGFR-dependent and
-independent resistance mechanisms to osimertinib and continuation
therapy beyond progression in -mutant NSCLC. Clin Cancer Res.
24:6195–6203. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Oxnard GR, Hu Y, Mileham KF, Husain H,
Costa DB, Tracy P, Feeney N, Sholl LM, Dahlberg SE, Redig AJ, et
al: Assessment of resistance mechanisms and clinical implications
in patients with EGFR T790M-positive lung cancer and acquired
resistance to osimertinib. JAMA Oncol. 4:1527–1534. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lin CC, Shih JY, Yu CJ, Ho CC, Liao WY,
Lee JH, Tsai TH, Su KY, Hsieh MS, Chang YL, et al: Outcomes in
patients with non-small-cell lung cancer and acquired Thr790Met
mutation treated with osimertinib: A genomic study. Lancet Resp
Med. 6:107–116. 2018. View Article : Google Scholar
|
|
59
|
Ramalingam SS, Cheng Y, Zhou C, Ohe Y,
Imamura F, Cho BC, Lin MC, Majem M, Shah R, Rukazenkov Y, et al:
Mechanisms of acquired resistance to first-line osimertinib:
Preliminary data from the phase III FLAURA study. Ann Oncol.
29(Suppl 8): viii7402018. View Article : Google Scholar
|
|
60
|
Ramalingam SS, Yang JC, Lee CK, Kurata T,
Kim DW, John T, Nogami N, Ohe Y, Mann H, Rukazenkov Y, et al:
Osimertinib as first-line treatment of EGFR mutation-positive
advanced non-small-cell lung cancer. J Clin Oncol. 36:841–849.
2018. View Article : Google Scholar
|
|
61
|
Zhang YC, Chen ZH, Zhang XC, Xu CR, Yan
HH, Xie Z, Chuai SK, Ye JY, Han-Zhang H, Zhang Z, et al: Analysis
of resistance mechanisms to abivertinib, a third-generation EGFR
tyrosine kinase inhibitor, in patients with EGFR T790M-positive
non-small cell lung cancer from a phase I trial. EBioMedicine.
43:180–187. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Chabon JJ, Simmons AD, Lovejoy AF,
Esfahani MS, Newman AM, Haringsma HJ, Kurtz DM, Stehr H, Scherer F,
Karlovich CA, et al: Circulating tumour DNA profiling reveals
heterogeneity of EGFR inhibitor resistance mechanisms in lung
cancer patients. Nat Commun. 7:118152016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Helman E, Nguyen M, Karlovich CA, Despain
D, Choquette AK, Spira AI, Yu HA, Camidge DR, Harding TC, Lanman RB
and Simmons AD: Cell-Free DNA next-generation sequencing prediction
of response and resistance to third-generation EGFR inhibitor. Clin
Lung Cancer. 19:530.e72018. View Article : Google Scholar
|
|
64
|
Ercan D, Choi HG, Yun CH, Capelletti M,
Xie T, Eck MJ, Gray NS and Jänne PA: EGFR mutations and resistance
to irreversible pyrimidine-based EGFR inhibitors. Clin Cancer Res.
21:3913–3923. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Song HN, Jung KS, Yoo KH, Cho J, Lee JY,
Lim SH, Kim HS, Sun JM, Lee SH, Ahn JS, et al: Acquired C797S
mutation upon treatment with a T790M-specific third-generation EGFR
inhibitor (HM61713) in non-small cell lung cancer. J Thorac Oncol.
11:e45–e47. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Park S, Ku BM, Jung HA, Sun JM, Ahn JS,
Lee SH, Park K and Ahn MJ: EGFR C797S as a resistance mechanism of
lazertinib in non-small cell lung cancer with EGFR T790M mutation.
Cancer Res Treat. 52:1288–1290. 2020.PubMed/NCBI
|
|
67
|
Oztan A, Fischer S, Schrock AB, Erlich RL,
Lovly CM, Stephens PJ, Ross JS, Miller V, Ali SM, Ou SI and Raez
LE: Emergence of EGFR G724S mutation in EGFR-mutant lung
adenocarcinoma post progression on osimertinib. Lung Cancer.
111:84–87. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Fassunke J, Muller F, Keul M, Michels S,
Dammert MA, Schmitt A, Plenker D, Lategahn J, Heydt C, Bragelmann
J, et al: Overcoming EGFRG724S-mediated osimertinib
resistance through unique binding characteristics of
second-generation EGFR inhibitors. Nat Commun. 9:46552018.
View Article : Google Scholar
|
|
69
|
Bersanelli M, Minari R, Bordi P, Gnetti L,
Bozzetti C, Squadrilli A, Lagrasta CA, Bottarelli L, Osipova G,
Capelletto E, et al: L718Q mutation as new mechanism of acquired
resistance to AZD9291 in EGFR-Mutated NSCLC. J Thorac Oncol 11:
e121-e123,. 2016.
|
|
70
|
Zhao S, Li X, Zhao C, Jiang T, Jia Y, Shi
J, He Y, Li J, Zhou F, Gao G, et al: Loss of T790M mutation is
associated with early progression to osimertinib in Chinese
patients with advanced NSCLC who are harboring EGFR T790M. Lung
Cancer. 128:33–39. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Piotrowska Z, Niederst MJ, Karlovich CA,
Wakelee HA, Neal JW, Mino-Kenudson M, Fulton L, Hata AN, Lockerman
EL, Kalsy A, et al: Heterogeneity underlies the emergence of
EGFRT790 wild-type clones following treatment of T790M-positive
cancers with a third-generation EGFR inhibitor. Cancer Discov.
5:713–722. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Knebel FH, Bettoni F, Shimada AK, Cruz M,
Alessi JV, Negrão MV, Reis LFL, Katz A and Camargo AA: Sequential
liquid biopsies reveal dynamic alterations of EGFR driver mutations
and indicate EGFR amplification as a new mechanism of resistance to
osimertinib in NSCLC. Lung Cancer. 108:238–241. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Wang Q, Yang S, Wang K and Sun SY: MET
inhibitors for targeted therapy of EGFR TKI-resistant lung cancer.
J Hematol Oncol. 12:632019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Drilon A, Cappuzzo F, Ou SI and Camidge
DR: Targeting MET in lung cancer: Will expectations finally Be MET?
J Thorac Oncol. 12:15–26. 2017. View Article : Google Scholar :
|
|
75
|
Hsu CC, Liao BC, Liao WY, Markovets A,
Stetson D, Thress K and Yang JC: Exon 16-Skipping HER2 as a Novel
Mechanism of Osimertinib Resistance in EGFR L858R/T790M-positive
non-small cell lung cancer. J Thorac Oncol. 15:50–61. 2020.
View Article : Google Scholar
|
|
76
|
Desai A and Adjei AA: FGFR signaling as a
target for lung cancer therapy. J Thorac Oncol. 11:9–20. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Kim TM, Song A, Kim DW, Kim S, Ahn YO,
Keam B, Jeon YK, Lee SH, Chung DH and Heo DS: Mechanisms of
acquired resistance to AZD9291: A mutation-selective, irreversible
EGFR inhibitor. J Thorac Oncol. 10:1736–1744. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Ou SI, Horn L, Cruz M, Vafai D, Lovly CM,
Spradlin A, Williamson MJ, Dagogo-Jack I, Johnson A, Miller VA, et
al: Emergence of FGFR3-TACC3 fusions as a potential by-pass
resistance mechanism to EGFR tyrosine kinase inhibitors in EGFR
mutated NSCLC patients. Lung Cancer. 111:61–64. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Hayakawa D, Takahashi F, Mitsuishi Y,
Tajima K, Hidayat M, Winardi W, Ihara H, Kanamori K, Matsumoto N,
Asao T, et al: Activation of insulin-like growth factor-1 receptor
confers acquired resistance to osimertinib in non-small cell lung
cancer with EGFR T790M mutation. Thorac Cancer. 11:140–149. 2020.
View Article : Google Scholar
|
|
80
|
Manabe T, Yasuda H, Terai H, Kagiwada H,
Hamamoto J, Ebisudani T, Kobayashi K, Masuzawa K, Ikemura S, Kawada
I, et al: IGF2 Autocrine-Mediated IGF1R activation is a clinically
relevant mechanism of osimertinib resistance in lung cancer. Mol
Cancer Res. 18:549–559. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Taniguchi H, Yamada T, Wang R, Tanimura K,
Adachi Y, Nishiyama A, Tanimoto A, Takeuchi S, Araujo LH, Boroni M,
et al: AXL confers intrinsic resistance to osimertinib and advances
the emergence of tolerant cells. Nat Commun. 10:2592019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Namba K, Shien K, Takahashi Y, Torigoe H,
Sato H, Yoshioka T, Takeda T, Kurihara E, Ogoshi Y, Yamamoto H, et
al: Activation of AXL as a preclinical acquired resistance
mechanism against osimertinib treatment in EGFR-mutant non-small
cell lung cancer cells. Mol Cancer Res. 17:499–507. 2019.
View Article : Google Scholar
|
|
83
|
Nakatani K, Yamaoka T, Ohba M, Fujita KI,
Arata S, Kusumoto S, Taki-Takemoto I, Kamei D, Iwai S, Tsurutani J
and Ohmori T: KRAS and EGFR amplifications mediate resistance to
rociletinib and osimertinib in acquired afatinib-resistant NSCLC
harboring exon 19 deletion/T790M in. Mol Cancer Ther. 18:112–126.
2019. View Article : Google Scholar
|
|
84
|
Marcoux N, Gettinger SN, O'Kane G, Arbour
KC, Neal JW, Husain H, Evans TL, Brahmer JR, Muzikansky A, Bonomi
PD, et al: EGFR-mutant adenocarcinomas that transform to small-cell
lung cancer and other neuroendocrine carcinomas: Clinical outcomes.
J Clin Oncol. 37:278–285. 2019. View Article : Google Scholar
|
|
85
|
Schoenfeld AJ, Chan JM, Kubota D, Sato H,
Rizvi H, Daneshbod Y, Chang JC, Paik PK, Offin M, Arcila ME, et al:
Tumor analyses reveal squamous transformation and off-target
alterations as early resistance mechanisms to first-line
osimertinib in EGFR-mutant lung cancer. Clin Cancer Res.
26:2654–2663. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Dongre A and Weinberg RA: New insights
into the mechanisms of epithelial-mesenchymal transition and
implications for cancer. Nat Rev Mol Cell Biol. 20:69–84. 2019.
View Article : Google Scholar
|
|
87
|
Nukaga S, Yasuda H, Tsuchihara K, Hamamoto
J, Masuzawa K, Kawada I, Naoki K, Matsumoto S, Mimaki S, Ikemura S,
et al: Amplification of EGFR wild-type alleles in non-small cell
lung cancer cells confers acquired resistance to mutation-selective
EGFR tyrosine kinase inhibitors. Cancer Res. 77:2078–2089. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Weng CH, Chen LY, Lin YC, Shih JY, Lin YC,
Tseng RY, Chiu AC, Yeh YH, Liu C, Lin YT, et al:
Epithelial-mesenchymal transition (EMT) beyond EGFR mutations per
se is a common mechanism for acquired resistance to EGFR TKI.
Oncogene. 38:455–468. 2019. View Article : Google Scholar
|
|
89
|
Schrock AB, Zhu VW, Hsieh WS, Madison R,
Creelan B, Silberberg J, Costin D, Bharne A, Bonta I, Bosemani T,
et al: Receptor tyrosine kinase fusions and BRAF kinase fusions are
rare but actionable resistance mechanisms to EGFR tyrosine kinase
inhibitors. J Thorac Oncol. 13:1312–1323. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Batra U, Sharma M, Amrith BP, Mehta A and
Jain P: EML4-ALK fusion as a resistance mechanism to osimertinib
and its successful management with osimertinib and alectinib: Case
report and review of the literature. Clin Lung Cancer.
21:e597–e600. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Jia Y, Yun CH, Park E, Ercan D, Manuia M,
Juarez J, Xu C, Rhee K, Chen T, Zhang H, et al: Overcoming
EGFR(T790M) and EGFR(C797S) resistance with mutant-selective
allosteric inhibitors. Nature. 534:129–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Uchibori K, Inase N, Araki M, Kamada M,
Sato S, Okuno Y, Fujita N and Katayama R: Brigatinib combined with
anti-EGFR antibody overcomes osimertinib resistance in EGFR-mutated
non-small-cell lung cancer. Nat Commun. 8:147682017. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Schalm SS, Dineen T, Lim SM, Park CW,
Hsieh J, Woessner R, Zhang Z, Wilson K, Eno M, Wilson D, et al:
1296P BLU-945, a highly potent and selective 4th generation EGFR
TKI for the treatment of EGFR T790M/C797S resistant NSCLC. Ann
Oncol. 31(Suppl 6): S1386–S1406. 2020.
|
|
94
|
Liu X, Zhang X, Yang L, Tian X, Dong T,
Ding CZ, Hu L, Wu L, Zhao L, Mao J, et al: Abstract 1320:
Preclinical evaluation of TQB3804, a potent EGFR C797S inhibitor.
79(Suppl 13): S13202019.
|
|
95
|
Kim DW, Tiseo M, Ahn MJ, Reckamp KL,
Hansen KH, Kim SW, Huber RM, West HL, Groen HJ, Hochmair MJ, et al:
Brigatinib in patients with crizotinib-refractory anaplastic
lymphoma kinase-positive non-small-cell lung cancer: A randomized,
multicenter phase II trial. J Clin Oncol. 35:2490–2498. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Wang Y, Yang N, Zhang Y, Li L, Han R, Zhu
M, Feng M, Chen H, Lizaso A, Qin T, et al: Effective treatment of
lung adenocarcinoma harboring EGFR-activating mutation, T790M, and
cis-C797S triple mutations by brigatinib and cetuximab combination
therapy. J Thorac Oncol. 15:1369–1375. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Zhao J, Zou M, Lv J, Han Y and Wang G and
Wang G: Effective treatment of pulmonary adenocarcinoma harboring
triple EGFR mutations of L858R, T790M, and -C797S by osimertinib,
bevacizumab, and brigatinib combination therapy: A case report.
Onco Targets Ther. 11:5545–5550. 2018. View Article : Google Scholar :
|
|
98
|
Arulananda S, Do H, Musafer A, Mitchell P,
Dobrovic A and John T: Combination osimertinib and gefitinib in
C797S and T790M EGFR-mutated non-small cell lung cancer. J Thorac
Oncol. 12:1728–1732. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Giroux-Leprieur E, Dumenil C and Chinet T:
Combination of crizotinib and osimertinib or erlotinib might
overcome MET-mediated resistance to EGFR Tyrosine kinase inhibitor
in EGFR-mutated adenocarcinoma. J Thorac Oncol. 13:e232–e234. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Sequist LV, Han JY, Ahn MJ, Cho BC, Yu H,
Kim SW, Yang JC, Lee JS, Su WC, Kowalski D, et al: Osimertinib plus
savolitinib in patients with EGFR mutation-positive, MET-amplified,
non-small-cell lung cancer after progression on EGFR tyrosine
kinase inhibitors: Interim results from a multicentre, open-label,
phase 1b study. Lancet Oncol. 21:373–386. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Odogwu L, Mathieu L, Blumenthal G, Larkins
E, Goldberg KB, Griffin N, Bijwaard K, Lee EY, Philip R, Jiang X,
et al: FDA approval summary: Dabrafenib and trametinib for the
treatment of metastatic non-small cell lung cancers harboring BRAF
V600E mutations. Oncologist. 23:740–745. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Oh DK, Ji WJ, Kim WS, Choi CM, Yoon SK,
Rho JK and Lee JC: Efficacy, safety, and resistance profile of
osimertinib in T790M mutation-positive non-small cell lung cancer
in real-world practice. PLoS One. 14:e02102252019. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Piotrowska Z, Isozaki H, Lennerz JK,
Gainor JF, Lennes IT, Zhu VW, Marcoux N, Banwait MK, Digumarthy SR,
Su W, et al: Landscape of acquired resistance to osimertinib in
EGFR-Mutant NSCLC and clinical validation of combined EGFR and RET
inhibition with osimertinib and BLU-667 for acquired fusion. Cancer
Discov. 8:1529–1539. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Han R, Hao S, Lu C, Zhang C, Lin C, Li L,
Wang Y, Hu C and He Y: Aspirin sensitizes osimertinib-resistant
NSCLC cells in vitro and in vivo via Bim-dependent apoptosis
induction. Mol Oncol. 14:1152–1169. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Niederst MJ, Hu H, Mulvey HE, Lockerman
EL, Garcia AR, Piotrowska Z, Sequist LV and Engelman JA: The
allelic context of the C797S mutation acquired upon treatment with
third-generation EGFR inhibitors impacts sensitivity to subsequent
treatment strategies. Clin Cancer Res. 21:3924–3933. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Wang Z, Yang JJ, Huang J, Ye JY, Zhang XC,
Tu HY, Han-Zhang H and Wu YL: Lung Adenocarcinoma Harboring EGFR
T790M and in trans C797S responds to combination therapy of first-
and third-generation EGFR TKIs and shifts allelic configuration at
resistance. J Thorac Oncol. 12:1723–1727. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Rotow JK, Costa DB, Paweletz CP, Awad MM,
Marcoux P, Rangachari D, Barbie DA, Sands J, Cheng ML, Johnson BE,
et al: Concurrent osimertinib plus gefitinib for first-line
treatment of EGFR-mutated non-small cell lung cancer (NSCLC). J
Clin Oncol. 38:95072020. View Article : Google Scholar
|
|
108
|
Chic N, Mayo-de-Las-Casas C and Reguart N:
Successful treatment with gefitinib in advanced non-small cell lung
cancer after acquired resistance to osimertinib. J Thorac Oncol.
12:e78–e80. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Rangachari D, To C, Shpilsky JE,
VanderLaan PA, Kobayashi SS, Mushajiang M, Lau CJ, Paweletz CP,
Oxnard GR, Jänne PA and Costa DB: EGFR-mutated lung cancers
resistant to osimertinib through EGFR C797S respond to
first-generation reversible EGFR inhibitors but eventually acquire
EGFR T790M/C797S in preclinical models and clinical samples. J
Thorac Oncol. 14:1995–2002. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Yang X, Huang C, Chen R and Zhao J:
Resolving resistance to osimertinib therapy with afatinib in an
NSCLC patient with EGFR L718Q mutation. Clin Lung Cancer.
21:e258–e260. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Romaniello D, Mazzeo L, Mancini M,
Marrocco I, Noronha A, Kreitman M, Srivastava S, Ghosh S, Lindzen
M, Salame TM, et al: A combination of approved antibodies overcomes
resistance of lung cancer to osimertinib by blocking bypass
pathways. Clin Cancer Res. 24:5610–5621. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Yu HA, Baik CS, Gold K, Hayashi H, Johnson
M, Koczywas M, Murakami H, Nishio M, Steuer C, Su WC, et al: LBA62
Efficacy and safety of patritumab deruxtecan (U3-1402), a novel
HER3 directed antibody drug conjugate, in patients (pts) with
EGFR-mutated (EGFRm) NSCLC. Ann Oncol. 31:S1189–S1190. 2020.
View Article : Google Scholar
|
|
113
|
Cho BC, Lee KH, Cho EK, Kim DW, Lee JS,
Han JY, Kim SW, Spira A, Haura EB, Sabari JK, et al: 1258O
Amivantamab (JNJ-61186372), an EGFR-MET bispecific antibody, in
combination with lazertinib, a 3rd-generation tyrosine kinase
inhibitor (TKI), in advanced EGFR NSCLC. Ann Oncol. 31(Suppl 4):
S8132020. View Article : Google Scholar
|
|
114
|
Okura N, Nishioka N, Yamada T, Taniguchi
H, Tanimura K, Katayama Y, Yoshimura A, Watanabe S, Kikuchi T,
Shiotsu S, et al: ONO-7475, a Novel AXL inhibitor, suppresses the
adaptive resistance to initial EGFR-TKI treatment in -mutated
non-small cell lung cancer. Clin Cancer Res. 26:2244–2256. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kim D, Bach DH, Fan YH, Luu TT, Hong JY,
Park HJ and Lee SK: AXL degradation in combination with EGFR-TKI
can delay and overcome acquired resistance in human non-small cell
lung cancer cells. Cell Death Dis. 10:3612019. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Yang YM, Jang Y, Lee SH, Kang B and Lim
SM: AXL/MET dual inhibitor, CB469, has activity in non-small cell
lung cancer with acquired resistance to EGFR TKI with AXL or MET
activation. Lung Cancer. 46:70–77. 2020. View Article : Google Scholar
|
|
117
|
Shi P, Oh YT, Deng L, Zhang G, Qian G,
Zhang S, Ren H, Wu G, Legendre B Jr, Anderson E, et al: Overcoming
acquired resistance to AZD9291, A third-generation EGFR inhibitor,
through modulation of MEK/ERK-dependent Bim and Mcl-1 Degradation.
Clin Cancer Res. 23:6567–6579. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Gu J, Yao W, Shi P, Zhang G, Owonikoko TK,
Ramalingam SS and Sun SY: MEK or ERK inhibition effectively
abrogates emergence of acquired osimertinib resistance in the
treatment of epidermal growth factor receptor-mutant lung cancers.
Cancer. 126:3788–3799. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Xie Z, Gu Y, Xie X, Lin X, Ouyang M, Qin
Y, Zhang J, Lizaso A, Chen S and Zhou C: Lung adenocarcinoma
harboring concomitant EGFR mutations and BRAF V600E responds to a
combination of osimertinib and vemurafenib to overcome osimertinib
resistance. Clin Lung Cancer. 22:e390–e394. 2021. View Article : Google Scholar
|
|
120
|
Raoof S, Mulford IJ, Frisco-Cabanos H,
Nangia V, Timonina D, Labrot E, Hafeez N, Bilton SJ, Drier Y, Ji F,
et al: Targeting FGFR overcomes EMT-mediated resistance in EGFR
mutant non-small cell lung cancer. Oncogene. 38:6399–6413. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Yochum ZA, Cades J, Wang H, Chatterjee S,
Simons BW, O'Brien JP, Khetarpal SK, Lemtiri-Chlieh G, Myers KV,
Huang EH, et al: Targeting the EMT transcription factor TWIST1
overcomes resistance to EGFR inhibitors in EGFR-mutant
non-small-cell lung cancer. Oncogene. 38:656–670. 2019. View Article : Google Scholar
|
|
122
|
Yang JC, Schuler M, Popat S, Miura S,
Heeke S, Park K, Märten A and Kim ES: Afatinib for the treatment of
NSCLC harboring uncommon EGFR mutations: A database of 693 cases. J
Thorac Oncol. 15:803–815. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Fang W, Huang Y, Gan J, Shao YW and Zhang
L: Durable response of low-dose afatinib plus cetuximab in an
adenocarcinoma patient with a novel EGFR exon 20 insertion
mutation. J Thorac Oncol. 14:e220–e221. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Hasegawa H, Yasuda H, Hamamoto J, Masuzawa
K, Tani T, Nukaga S, Hirano T, Kobayashi K, Manabe T, Terai H, et
al: Efficacy of afatinib or osimertinib plus cetuximab combination
therapy for non-small-cell lung cancer with EGFR exon 20 insertion
mutations. Lung Cancer. 127:146–152. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
van Veggel B, de Langen AJ, Hashemi SMS,
Monkhorst K, Heideman DAM, Thunnissen E and Smit EF: Afatinib and
cetuximab in four patients with EGFR exon 20 insertion-positive
advanced NSCLC. J Thorac Oncol. 13:1222–1226. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Yun J, Lee SH, Kim SY, Jeong SY, Kim JH,
Pyo KH, Park CW, Heo SG, Yun MR, Lim S, et al: Antitumor activity
of amivantamab (JNJ-61186372), an EGFR-MET bispecific antibody, in
diverse models of exon 20 insertion-driven NSCLC. Cancer Discov.
10:1194–1209. 2020.PubMed/NCBI
|
|
127
|
Riely GJ, Neal JW, Camidge DR, Spira A,
Piotrowska Z, Horn L, Costa DB, Tsao A, Patel J, Gadgeel S, et al:
1261MO Updated results from a phase I/II study of mobocertinib
(TAK-788) in NSCLC with EGFR exon 20 insertions (exon20ins). Ann
Oncol. 31:S815–S816. 2020. View Article : Google Scholar
|
|
128
|
Nakahara Y, Kato T, Isomura R, Seki N,
Furuya N, Naoki K, Yamanaka T and Okamoto H: A multicenter, open
label, randomized phase II study of osimertinib plus ramucirumab
versus osimertinib alone as initial chemotherapy for EGFR
mutation-positive non-squamous non-small cell lung cancer:
TORG1833. J Clin Oncol. 37:TPS91202019. View Article : Google Scholar
|
|
129
|
Yu HA, Schoenfeld AJ, Makhnin A, Kim R,
Rizvi H, Tsui D, Falcon C, Houck-Loomis B, Meng F, Yang JL, et al:
Effect of osimertinib and bevacizumab on progression-free survival
for patients with metastatic EGFR-mutant lung cancers: A Phase 1/2
single-group open-label trial. JAMA Oncol. 6:1048–1054. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Kobayashi N, Hashimoto H, Kamimaki C,
Nagasawa R, Tanaka K, Kubo S, Katakura S, Chen H, Hirama N, Ushio
R, et al: Afatinib + bevacizumab combination therapy in EGFR-mutant
NSCLC patients with osimertinib resistance: Protocol of an
open-label, phase II, multicenter, single-arm trial. Thorac Cancer.
11:2125–2129. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Lisberg A, Cummings A, Goldman JW,
Bornazyan K, Reese N, Wang T, Coluzzi P, Ledezma B, Mendenhall M,
Hunt J, et al: A phase II study of pembrolizumab in EGFR-Mutant,
PD-L1+, tyrosine kinase inhibitor naïve patients with
advanced NSCLC. J Thorac Oncol. 13:1138–1145. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Ahn MJ, Yang J, Yu H, Saka H, Ramalingam
S, Goto K, Kim SW, Yang L, Walding A and Oxnard GR: 136O:
Osimertinib combined with durvalumab in EGFR-mutant non-small cell
lung cancer: Results from the TATTON phase Ib trial. J Thorac
Oncol. 11:S1152016. View Article : Google Scholar
|
|
133
|
Zhou J, Zhou F, Xie H, Wu Y, Zhao J and Su
C: An advanced non-small cell lung cancer patient with epidermal
growth factor receptor sensitizing mutation responded to
toripalimab in combination with chemotherapy after resistance to
osimertinib: A case report. Transl Lung Cancer Res. 9:354–359.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Zhang YC, Zhou Q and Wu YL: Clinical
management of third-generation EGFR inhibitor-resistant patients
with advanced non-small cell lung cancer: Current status and future
perspectives. Cancer Lett. 459:240–247. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Wu YL, Planchard D, Lu S, Sun H, Yamamoto
N, Kim DW, Tan DSW, Yang JC, Azrif M, Mitsudomi T, et al: Pan-Asian
adapted clinical practice guidelines for the management of patients
with metastatic non-small-cell lung cancer: A CSCO-ESMO initiative
endorsed by JSMO, KSMO, MOS, SSO and TOS. Ann Oncol. 30:171–210.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Non-Small Cell Lung Cancer Version 4. NCCN
Clinical Practice Guidelines in Oncology. 2021, https://www.nccn.org. Accessed at 25 Jun 2021.
|
|
137
|
Jang J, To C, De Clercq DJH, Park E,
Ponthier CM, Shin BH, Mushajiang M, Nowak RP, Fischer ES, Eck MJ,
et al: Mutant-selective allosteric EGFR degraders are effective
against a broad range of drug-resistant mutations. Angew Chem Int
Ed Engl. 59:14481–14489. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
To C, Jang J, Chen T, Park E, Mushajiang
M, De Clercq DJH, Xu M, Wang S, Cameron MD, Heppner DE, et al:
Single and dual targeting of mutant EGFR with an allosteric
inhibitor. Cancer Discov. 9:926–943. 2019. View Article : Google Scholar : PubMed/NCBI
|