Introduction
Germ cell tumors account for 98% of all testicular
malignancies. Testicular cancer represents the most common
malignancy in males aged between 15 and 34 (1). Cryptorchidism remains the best
established risk factor for testicular germ cell tumors. It is
estimated that a cryptorchid testicle is 30–50 times more likely to
develop a malignant neoplasm compared with a normally placed organ.
The incidence is higher even following orchiopexy, if done after 6
years of age. Notably, molecular studies have shown strong evidence
of an association between genetic alterations and testicular germ
cell tumors (2)
It is fortunate that testicular germ cell tumors
represent a highly curable malignant tumor entity, even in the
presence of metastasis. The overall survival rate is ~90%,
considering all stages are reported (3). In the following case report, a
24-year-old man is presented in severe condition with a giant 12×10
cm left stage III cryptorchid seminoma metastasizing to the neck
and liver. Chemotherapy yielded complete remission of the primary
lesion.
Case report
In Sepember 2014, a 24-year-old previously healthy
man accompanied by his parents, was admitted to Department of
Otolaryngology, The First Hospital of Jilin University (Jilin,
China), complaining for a left neck mass that had grown rapidly
during recent months. The patient also complained of a huge mass
located in the left groin. However, it had failed to draw his
attention due to non-tenderness and its hidden nature. He had no
hematuria, no fever, chill or rigors, with the exception of weight
loss during the past year.
Upon examination, the patient was emaciated, nearly
in a state of cachexia, at <45 kg. A 3.0×3.0 cm mass situated in
left supraclavicular fossa extending to the lower cervical region
was palpable. Abdominal examination revealed a left inguinal mass
of 12×10 cm, directly beneath the skin, extending to the left rib,
hard in consistency. Scrotal examination revealed the absence of
the left testicle and normal scrotum. The patient was then
transferred to the Department of Andrology.
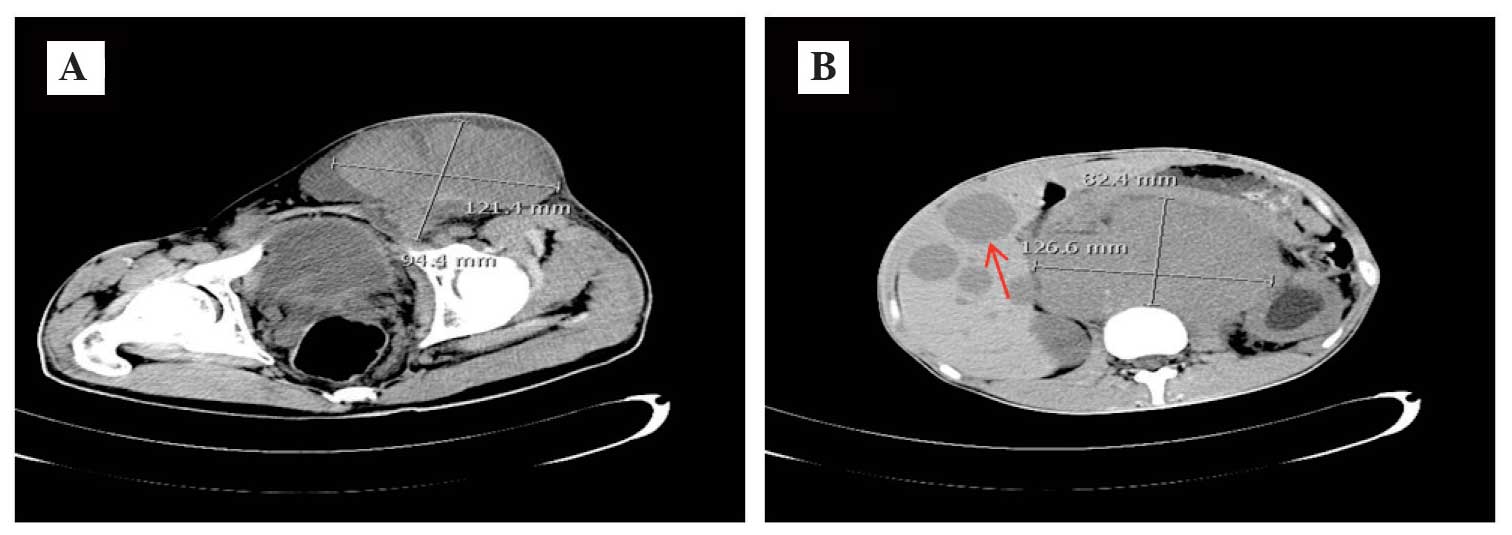
Computed tomography (CT) confirmed that the mass
measuring 12.1×9.4 cm was a left undescended testicle malignancy,
and revealed widespread metastasis to the liver and a large
retroperitoneal mass (12.6×8.2 cm; Fig.
1). The tumor markers α-fetoprotein, the β-subunit of human
chorionic gonadotrophin and lactic dehydrogenase were within normal
limits. All laboratory tests, including complete blood count,
biochemistry and chest X-ray, were normal. The provisional
diagnosis was testicular metastatic tumor, with a suspicion of
lymphoma or germ cell tumor.
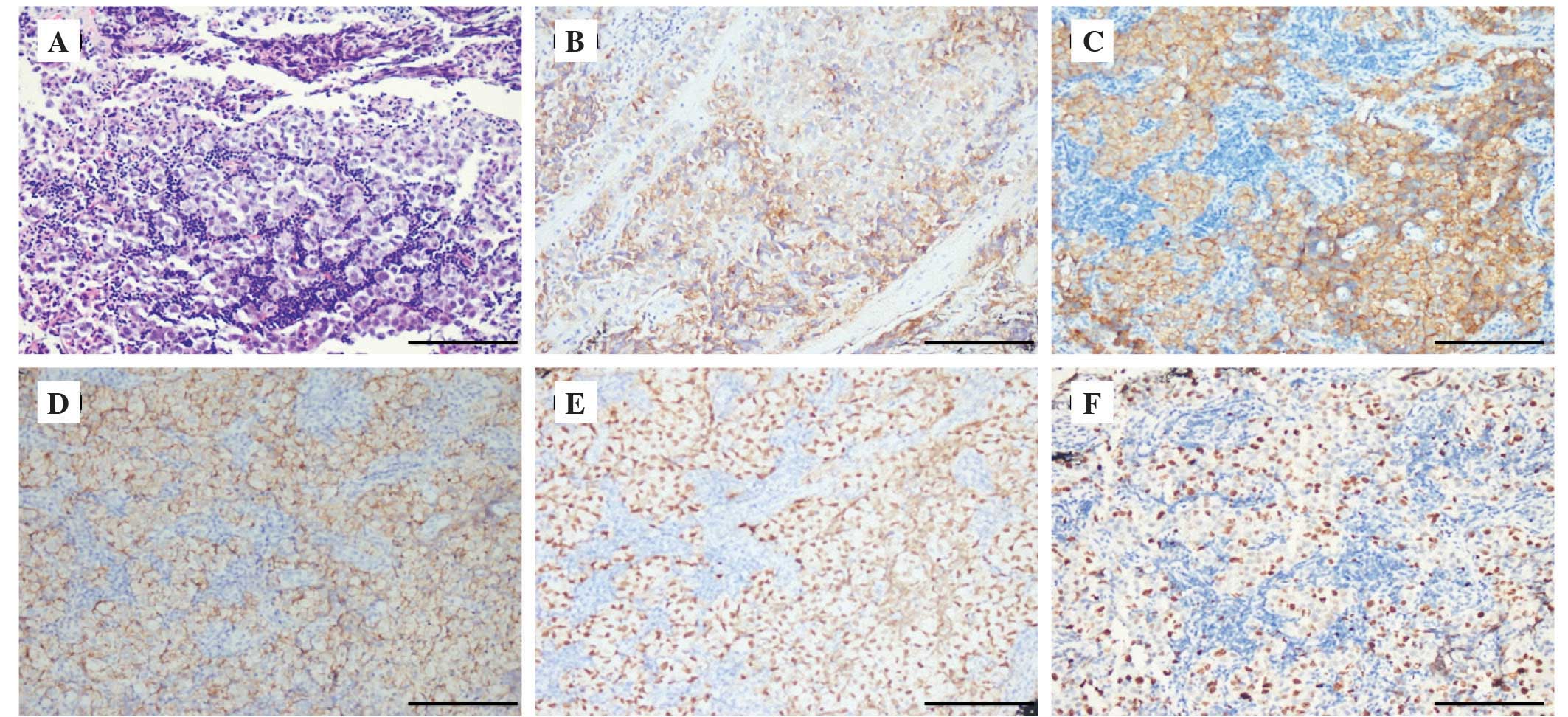
The needle biopsy of the supraclavicular mass was
performed. Pathological examination revealed nodules of metastatic
tumor cells lined in the pattern of nests and cords, divided by
intervening fibrous septa with a moderate lymphocytic infiltrate.
Immunohistochemical stains revealed diffuse expression of placental
alkaline phosphatase and OCT3/4. In addition, the tumor cells
exhibited strong and diffuse positivity for cluster of
differentiation (CD)117 and D2-40, which confirmed the seminoma.
The proliferation marker, Ki-67, revealed a high proliferation
index (>30%; Fig. 2).
Due to the extent of the metastasis, the tumor was
considered inoperable, both oncologically and in view of the
resulting morbidity. At the interdisciplinary tumor board,
chemotherapy with curative intent was indicated. Finally, the
patient was administered the chemotherapy VIP regimen (four cycles
of cisplatin, etoposide and ifosfamide). Six months after this
routine therapy, the patient remained stable and achieved complete
remission. CT revealed a reduction of the inguinal mass by 98%
without changes in the size of the retroperitoneal lymph nodes. The
patient was informed about surgical resection of the left testicle,
however, he refused further surgery due to personal reasons.
Discussion
Testicular cancer is the most common cancer type in
men between the ages of 20- and 35-years old. Seminoma is the most
common of the testicular germ cell tumor types, accounting for ~30%
of all testicular neoplasms. The undescended testicles harbor a
20–48 times higher potential for malignant transformation compared
with the normally descended testicles. The relative risk of
malignancy is highest for the intra-abdominal testis (5%) and is
significantly lower for the inguinal testis (1.25%) (4). Metastases of seminoma are rare, unless
it is associated with sarcoma (5). In
the review by van Vledder et al (6), 4% of patients with seminoma had cervical
metastasis. The peak age for presentation is 30–35 years for
classic seminoma, secondary peaks are noted in infancy (0–10 years)
and in late adulthood (>60 years). More commonly, the diagnosis
may be missed as a result of inadequate physical examination or
laboratory evaluation, which can lead to unnecessary surgical
procedures and delays to diagnosis and appropriate therapy.
The important aspect of the case presentation
concerns the diagnostic delay: Qualitative psycho-oncological
studies have documented that certain patients responded to disease
symptoms by using self-medication or waiting. Problems with access
to healthcare professionals and patients' social responsibilities
served as the predominant barriers to prompt seeking assistance
(7). As with the present case, the
patient failed to pay attention to the groin enlargement until it
grew so quickly that it became a burden. Therefore, it is assumed
that the patient may neglect this important sign if the groin mass
were not large enough. The present case demonstrated the importance
of a thorough physical examination and consideration of testicular
mass in the evaluation of patients presenting with neck nodes.
Furthermore, this case was unusual in another aspect. The hugeness
and massive metastasis of the primary lesion resulted in the
consideration of possible lymphoma. The diagnosis of seminoma was
established by immunohistochemistry.
Notably, once neck nodes are involved, the tumor is
classed as stage 3 and initial treatment is generally chemotherapy.
The majority of patients with this tumor stage are curable since
the introduction of cisplatin-based chemotherapy, a regimen that
has recently been suggested as a less toxic and equally effective
alternative in intermediate prognosis metastatic seminoma (overall
survival of 91% after 3.5 years) (8).
In the present patient, chemotherapy yielded complete clinical
remission. The present study was confused as to why the patient
refused surgical resection of left orchid testis, which may be like
a ‘untimed bomb’. The present case highlighted that cryptorchidism
remains the best established risk factor for testicular germ cell
tumor and medical practitioners must remember to include metastatic
testicular germ cell tumors in their differential diagnosis of
supraclavicular neck mass.
Acknowledgements
The present study was funded by the Jilin Financial
Foundation (no. 20157301051).
References
|
1
|
Aparicio J: SEOM clinical guidelines for
diagnosis and treatment of testicular seminoma. Clin Transl Oncol.
13:560–564. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Winter C and Albers P: Testicular germ
cell tumors: pathogenesis, diagnosis and treatment. Nat Rev
Endocrinol. 7:43–53. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reiter WJ, Brodowicz T, Alavi S, Zielinski
CC, Kozak W, Maier U, Nöst G, Lipsky H, Marberger M and Kratzik C:
Twelve-year experience with two courses of adjuvant single-agent
carboplatin therapy for clinical stage I seminoma. J Clin Oncol.
19:101–104. 2001.PubMed/NCBI
|
|
4
|
Pettersson A, Richiardi L, Nordenskjold A,
Kaijser M and Akre O: Age at surgery for undescended testis and
risk of testicular cancer. N Engl J Med. 356:1835–1841. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carriere P, Baade P and Fritschi L:
Population based incidence and age distribution of spermatocytic
seminoma. J Urol. 178:125–128. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
van Vledder MG, van der Hage JA, Kirkels
WJ, Oosterhuis JW, Verhoef C and de Wilt JH: Cervical lymph node
dissection for metastatic testicular cancer. Ann Surg Oncol.
17:1682–1687. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Malavasi N, Ferrara L, Fiorani C, Saviola
A and Longo G: Diagnostic delay in oncology: A case report of
metastatic seminoma. Case Rep Oncol. 4:216–221. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
ASCO annual meeting proceedings
(Post-Meeting Edition). J Clin Oncol. 27:50312009.PubMed/NCBI
|