Introduction
Acute colorectal obstruction is an emergency
condition that requires early identification and intervention. In
addition to recognizing the common etiological factors responsible
for the obstruction, physicians must maintain a high index of
suspicion for complete obstruction, gangrenous or perforated bowel,
which should be referred for surgical consultation. For partial
colorectal obstruction, a less invasive approach is desirable to
reduce the risk of adverse outcomes associated with emergency
surgery. Applying urgent colonoscopy allows for direct evaluation
of the site of obstruction and subsequent determination of the
cause of obstruction and provision of treatment (1,2). For
example, although foreign body impaction in the colon is not common
in everyday emergency practice compared with upper gastrointestinal
(GI) foreign body ingestion, the value of urgent colonoscopy for
identifying a foreign body appears to be more efficient compared
with imaging studies, such as plain abdominal X-ray or computed
tomography (3,4). Fecal impaction is a common GI disorder
that may lead to acute complications and it presents with symptoms
similar to those observed in colon obstruction, such as abdominal
pain and distention, nausea, vomiting and anorexia (5). Congenital and acquired conditions of
the colon and rectum, including Hirschsprung's disease and Chagas'
disease, may cause fecal impaction. Anatomic and functional
abnormalities of the anorectum should also be considered and
excluded (5). Therefore, direct
visualization by colonoscopy may also be a useful tool for
diagnosing and treating fecal impaction.
Acute malignant colonic obstruction is common in the
hospital setting. Up to 29% of patients with advanced colorectal
cancer present with acute colonic obstruction from intraluminal
tumor growth. By contrast, metastatic or invasive non-colorectal
cancer may lead to acute obstruction by extrinsic compression
(6). Treatment options include
transanal colonoscopic decompression tubes and placement of a
self-expanding metallic stent (SEMS), which is primarily used for
malignant obstruction, while endoscopic balloon dilation is used
for benign indications, such as strictures resulting from surgical
anastomosis and inflammatory bowel disease (1). The application of SEMS has recently
become more frequent for the palliation of metastatic colorectal
cancer and as a bridge to surgery for obstructing tumors, despite
the concerns regarding safety and efficacy in recent systematic
reviews and meta-analyses (6,7).
Additional considerable variations in practice may exist due to the
lack of expertise and technical difficulties (8,9).
SEMS placement involves passing a guidewire through
the obstruction. The wire is manipulated with either fluoroscopy
alone, as in the over-the-wire (OTW) method, or combined with
endoscopic visualization, as in the through-the-scope (TTS)
technique (8,10). In the literature, it appears that
experienced operators using TTS achieved better technical and
clinical outcomes (8,9,11,12). The
present study demonstrated that TTS is a practical tool for
effectively resolving bowel obstruction in our unit. In addition,
in a case with near complete obstruction, in which the slim
endoscope could not be passed through the lesion, delivery of SEMS
was guided by real-time radiography and CO2 gas was used
as a contrast agent, allowing assessment of the morphology and
length of the obstruction.
Patients and methods
Single endoscopy unit study
A database of all patients treated between February
1, 2011 and January 31, 2016 at the the Endoscopy Unit of Tongji
Hospital (Wuhan, China) was accessed. Tongji Hospital is a
state-owned teaching hospital. The Department of Internal Medicine
and its Endoscopy Unit is a referral center for Gastroenterology
and Hepatology and has availability of all endoscopic facilities
and treatment modalities for diagnostic, therapeutic and palliative
endoscopy. During the study period, ~43,732
esophagogastroduodenoscopies were performed annually at this
Unit.
Retrospective analysis
For the purposes of this study, the Endoscopy Unit
records were retrospectively reviewed, as were hospital medical
records. Approval for the study was granted by the Institutional
Ethics Committee. A total of 61 patients from the inpatient care
who underwent emergency colonoscopy management were evaluated by
both the surgeons and endoscopists prior to the procedure. All the
patients exhibited clinical characteristics of colorectal
obstruction, such as obstipation or constipation for >48 h,
abdominal distension, nausea, vomiting, or cramping abdominal pain.
The abdominal X-rays revealed colon dilation proximal to the
obstruction site, and large-bowel obstruction was confirmed by
means of either computed tomography (CT), barium enema, or
colonoscopy.
Technique
The primary indication of SEMS insertion is intended
to be a bridge to surgery for obstructive colorectal cancer
(1). For elderly patients with
unresectable malignancies who have severe medical comorbidities and
are in a poor overall condition, a transanal colonoscopic
decompression tube may be placed. The indication for endoscopic
balloon dilation is treatment of strictures associated with
surgical anastomoses.
Procedure for SEMS placement
All the SEMS placement procedures were performed by
one of four experienced endoscopists using the TTS technique. The
authors used the following procedures for stenting: First, a thin
gastroscope (GIF XP260; Olympus, Tokyo, Japan) was passed through
the stricture. The stricture length was estimated while monitoring
the endoscope advancing through the stenosis site. Second, a
biliary guidewire (Jagwire; diameter 0.035 inches, length 450 cm;
Boston Scientific, Hemel Hempstead, UK) was inserted into the
working channel (2.0 mm in diameter) of the endoscope (GIF XP260;
Olympus) to pass through the obstruction for ~20 cm or more, to
prevent it from slipping back through the obstruction. Third, the
guidewire was secured by an assistant as the endoscope was
retracted. During retraction, the endoscopist measured the tumor
length and the proximal and distal extension, which was crucial for
subsequent correct stent placement. Fourth, the stent length was
then selected according to the length of the tumor, with a deployed
length of ≥2 cm longer compared with that of the stricture. The
SEMS delivery system was placed over the guidewire followed by
re-intubating with the endoscope proximal to the stricture,
allowing accurate SEMS positioning under direct vision by aligning
the upper end of the stent beyond the tumor margin for ~1 cm. The
stent was then slowly deployed from its distal to its proximal end,
maintaining proximal traction on the stent introducer to prevent
distal migration.
In a case with near complete obstruction, in which
the slim endoscope could not pass through, delivery of SEMS was
guided by real-time radiography and CO2 gas was used as
a contrast agent, allowing assessment of the morphology and length
of the obstruction. Radiographic visualization and an immediate
stool flush were used to assess the patency after completion of
stent placement.
All SEMSs used were uncovered metal mesh devices
from MicroTech (diameter, 20 mm; length, 60–100 mm; MicroTech Co.,
Nanjing, China). The median procedure time was 30 min (range, 20–60
min).
Results
Etiology
Urgent endoscopic management of acute colorectal
obstruction is a rapidly developing field at the Tongji Endoscopy
Unit. In this retrospective study, 61 patients with acute
colorectal obstruction were identified between February, 2011 and
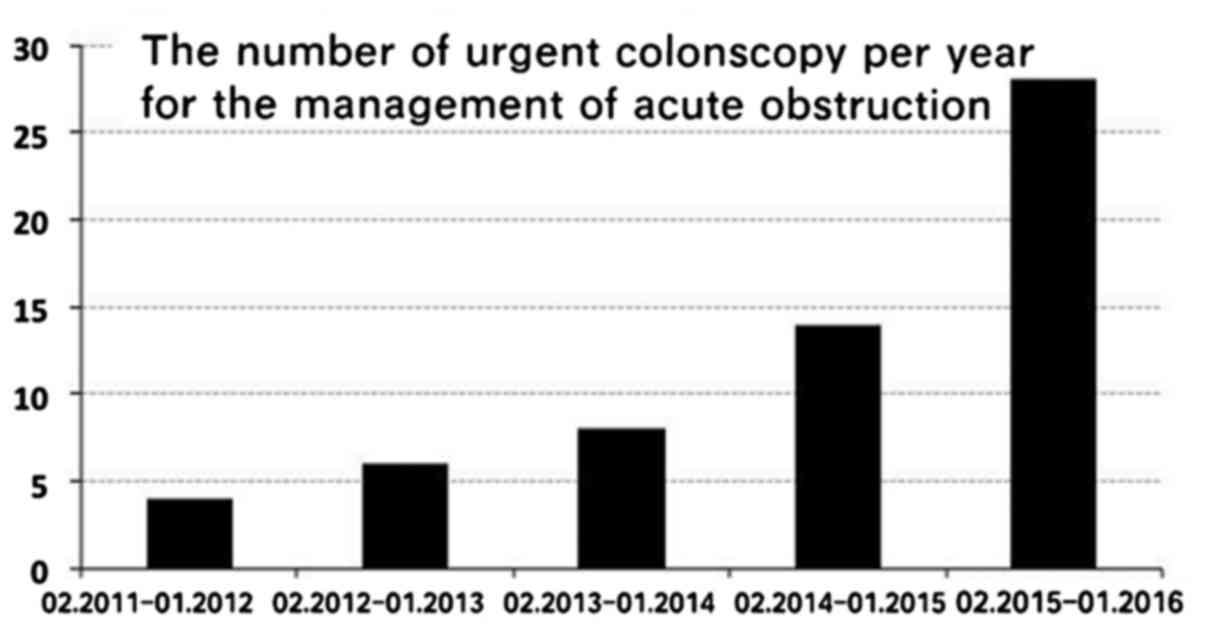
January, 2016. As shown in Fig. 1,
the number of cases increased each year, with only 4 cases in the
first year and 28 cases in the fifth year (Fig. 1). The etiological factors of
obstruction included colorectal cancer (53/61), extracolonic
malignancy, namely advanced peritoneal serous carcinoma (1/61),
foreign bodies (3/61), fecal impaction (2/61) and anastomotic
strictures (2/61; Table I).
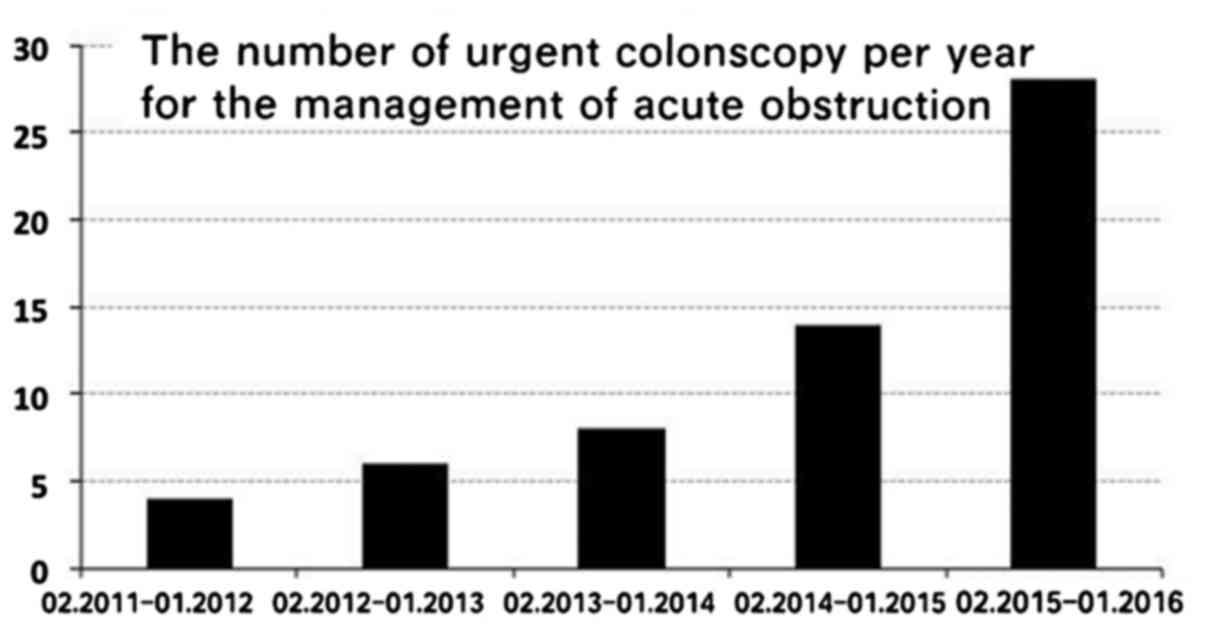 | Figure 1.Number of urgent colonoscopies per
year for the management of acute colorectal obstruction at the
Endoscopy Unit of Tongji Hospital. A total of 61 patients with
acute obstruction underwent the procedure. There were 4 cases
between February, 2011 and January, 2012, 6 between February, 2012
and January, 2013, 8 between February, 2013 and January, 2014, 14
between February, 2013 and January, 2014, and 28 cases between
February, 2015 and January, 2016. |
 | Table I.Etiology and techniques used for acute
colorectal obstruction. |
Table I.
Etiology and techniques used for acute
colorectal obstruction.
| Etiology | No. of patients | Techniques |
|---|
| Malignant
conditions |
|
|
|
Colorectal cancer | 53 | SEMS |
| Advanced
peritoneal serous cancer | 1 | Transanal colonic
decompression |
| Benign
conditions |
|
|
| Foreign
bodies (food, cotton tissue and surgical gauze) | 3 | Forceps method |
| Fecal
impaction (chronic constipation, anatomic anorectal
abnormalities) | 2 | Snare method |
|
Anastomotic strictures
(post-rectal cancer) | 2 | Balloon dilation |
Benign colorectal obstruction
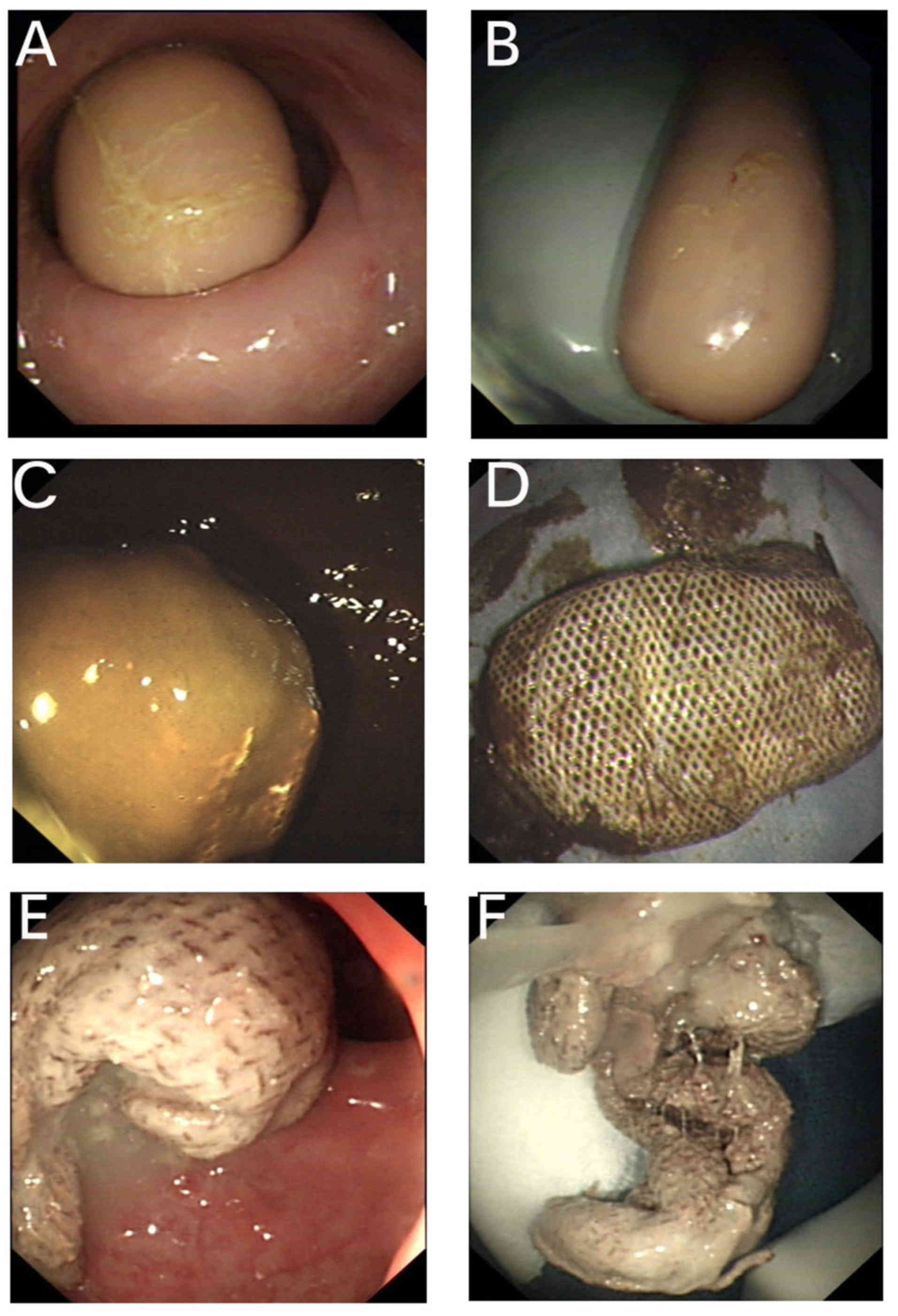
Three cases were caused by foreign body obstruction.
The average age was 39.7 years and all the patients were male. In
two cases the foreign objects had been intentionally inserted into
the rectum. The objects recovered from the rectum included a
sausage and cotton tissue (Fig. 2),
whereas 1 patient had previously undergone sigmoid colectomy and a
piece of surgical gauze was retained in the distal loop. A
retrieval device (alligator forceps) was successfully used to
extract the foreign bodies.
Two cases were caused by fecal impaction: One was a
48-year-old female patient who had chronic constipation and the
hardened stool was impacted in her descending colon close to the
splenic fixture, with subsequent obstruction. The other case was a
28-year-old female patient who suffered from congenital vaginal
obstruction and had undergone vaginal reconstruction with a sigmoid
colon segment when she was 23 years old. The patient subsequently
developed chronic constipation, and colonoscopy revealed fecal
impaction in the sigmoid colon. In both cases, the snare method was
used to break up the stone-like mass, which was then fragmentarily
removed.
Malignant colorectal obstruction
In our unit, SEMS placement is emergently applied as
a bridge to surgery. A total of 53 such patients were identified,
34 men (64.2%) and 19 women (35.8%), aged 19–82 years, with a mean
age of 56 years at the time of the procedure. The most frequent
stricture location was the sigmoid in 21 patients, followed by the
rectosigmoid junction (11 patients), the rectum (10 patients), the
descending colon (5 patients), the splenic fixture (5 patients) and
the transverse colon (1 patient) (Table
II).
 | Table II.SEMS patient demographics, method of
stenting and experience of the operator. |
Table II.
SEMS patient demographics, method of
stenting and experience of the operator.
| Variables | Ν (%) |
|---|
| Age, years [mean
(range)] | 56 (19–82) |
| Gender |
|
| Male | 34 (64.2) |
|
Female | 19 (35.8) |
| Reason for
stenting |
|
| Bridge to
CRC surgery | 8 (15.4) |
|
Palliative for CRC | 44 (84.6) |
| Site |
|
|
Rectum | 10 (18.9) |
|
Sigmoid | 21 (39.6) |
|
Rectosigmoid junction | 11 (20.8) |
|
Descending colon | 5 (9.4) |
| Splenic
fixture | 5 (9.4) |
|
Transverse colon | 1 (1.9) |
| SEMS used |
|
| 1 | 52 (98.1) |
|
0a | 1 (2.9) |
| SEMS length, cm |
|
| 6 | 2 (3.8) |
| 8 | 30 (56.6) |
| 10 | 21 (39.6) |
| SEMS diameter,
mm |
|
| 20 | 53 (100) |
| Deployment
technique |
|
| TTS | 52 (98.1) |
| TTS under
radiographic guidance | 1 (2.9) |
| Total operators
(n=4) |
|
| <10
procedures | 0 |
| ≥10
procedures | 3 |
| ≥10
procedures with ERCP experience | 1 |
| Training, n
(%) |
|
| Trainee
involved | 10 (18.9) |
| No
trainee | 43 (81.1) |
Initial technical success (defined as the ability to
adequately place a stent across the site of obstruction) was
achieved in 52 of the 53 cases (98%). In 1 patient with sigmoid
colon cancer, the stent could not be passed through the stricture
after delivering the guidewire under direct vision; the patient
subsequently underwent palliative surgery, with complete relief of
the obstruction. Clinical success (defined as relief of obstruction
with the passage of stool and gas) was achieved in all 52 patients
(100%) within 24 h, although in ~95% patients bowel decompression
started immediately after stent deployment. There were no
procedure-related complications, such as perforation or stent
dislocation. All the patients underwent surgery at 3–7 days
following SEMS placement. Importantly, stenting gained time for
staging, treatment planning, neoadjuvant therapies and patient
optimization. Of these patients, 8 (15.3%) were found to have
distant organ metastases at staging and, hence, avoided unnecessary
major surgery.
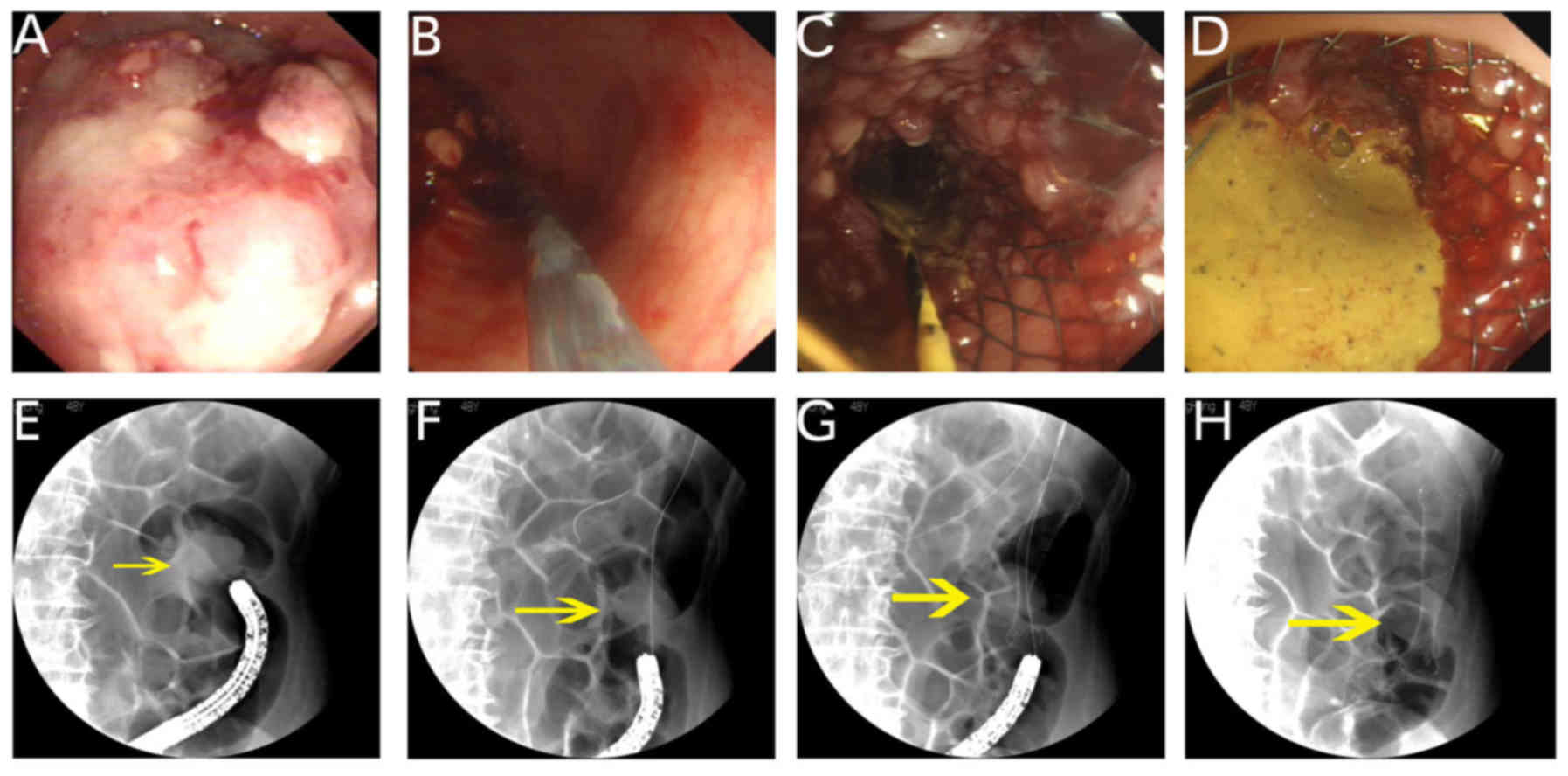
In a 64-year-old female patient with near complete
obstruction of the descending colon due to malignancy, passing a
guidewire and subsequently placing a stent were performed by an
endoscopist experienced in endoscopic retrograde
cholangiopancreatography (ERCP; 264 procedures annually).
Radiography was used at the time of procedure to monitor traversing
the stricture and to ensure complete patency of the prosthesis
following stent placement (Fig. 3).
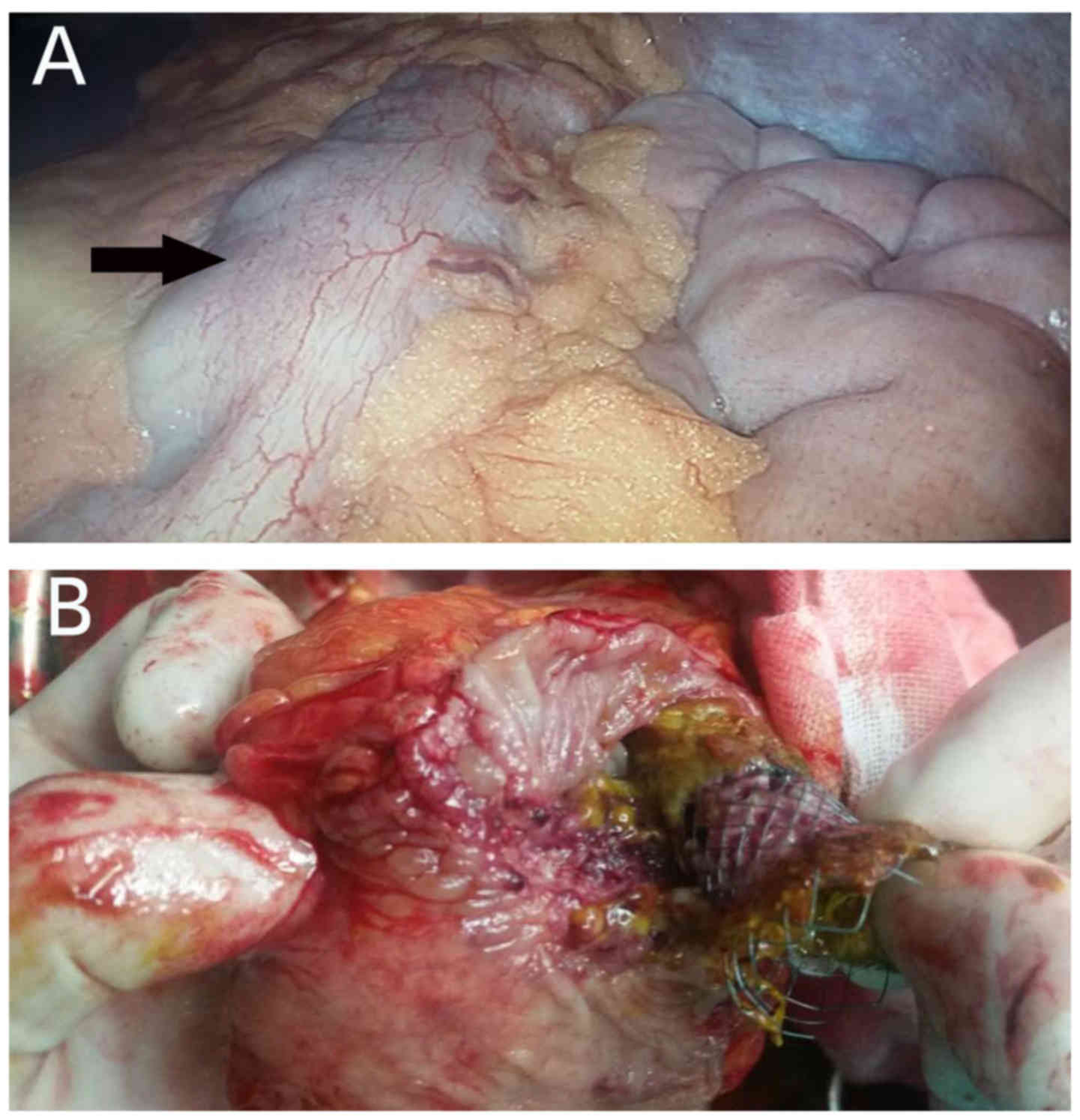
The patient underwent laparotomic surgery 3 days later and the SEMS
was removed (Fig. 4). A one-stage
operation was achieved.
In an 85-year-old female patient who had
extraluminal compression resulting from advanced peritoneal serous
carcinoma, a transanal colonic decompression tube was placed in the
sigmoid colon as palliative therapy. For benign obstructions
resulting from surgical anastomoses, endoscopic balloon dilation of
the strictures was successfully applied in 2 patients, without
complications.
Discussion
Patients admitted to Tongji Hospital with acute
colon obstruction were readily examined by the general/trauma
surgeons. Patients with severe unremitting pain or peritoneal signs
suspected to have complete obstruction, are generally referred for
surgical consultation. The decision to perform urgent colonoscopy
is based on the patient's condition, in addition to excluding the
potential risk of perforation. Following further evaluation by
endoscopists, these patients are immediately prepared for
endoscopy. The incidence in our population of patients requiring an
urgent colonoscopic procedure was 0.56%.
Urgent colonoscopy is widely used to relieve
obstruction resulting from benign conditions, such as volvulus,
inflammatory bowel disease, diverticulitis, anastomotic strictures,
radiation injury, ischemia, foreign bodies and intussusception 1).
Balloon dilation is a well-established technique for treating
strictures resulting from surgical anastomoses and inflammatory
bowel disease (13–15). However, our experience is limited,
compared with our experience with dilating esophageal strictures.
One reason is that the majority of patients with strictures have
already undergone repeated dilations at local smaller-sized
hospitals, but without improvement. Thus, searching for an
alternative treatment option, surgery at our hospital was favored.
Recent studies also highlighted the fact that electrocautery
dilation is a safe and effective treatment for relieving
obstruction caused by postsurgical strictures. Several studies
reported promising results from a long-term follow-up (median, 35.5
months), suggesting that one session of electrocautery treatment
appears to be sufficient and there are no reported recurrences and
procedure-related complications (16,17).
Given that this technique is easy to perform, does not require a
dedicated device and is cost-effective, additional studies are
required to determine whether this technique may serve as an
alternative method for relieving acute obstruction caused by benign
colonic strictures.
Patients with rectal foreign bodies have usually
inserted them intentionally and request their removal. Radiological
examinations, such as plain abdominal X-ray or abdominal CT scan,
are routinely obtained at Tongji Hospital, which may reveal the
cause of the obstruction. However, the value of imaging studies for
an impacted foreign body and fecal obstruction appears to be
questionable based on our experience, since they are often
negative. Regardless, the role of imaging studies is crucial for
determining the inflammatory reaction in and around the bowel wall
and for excluding conditions requiring surgical intervention.
Following complete work-up, the patients are examined by
colonoscopy. Conventional instruments were used for endoscopic
foreign body extraction, such as polypectomy snare, alligator and
rat tooth forceps. Endoscopy revealed no underlying pathology in
the 3 patients with foreign body impaction, apart from 1 patient
who had previously undergone sigmoid colectomy and a piece of
surgical gauze was retained in the distal loop.
The outcome of stenting for managing colorectal
obstruction from extrinsic invasive tumors has been previously
investigated, although its safety and efficiency are controversial
(11,18). These patients often present with a
complex stricture of the lumen, potentially at more than one
locations, with complex adhesions, which result in bowel
immobilization and altogether may contribute to the low success and
high complication rate of SEMS placement. Therefore, in an elderly
patient who had advanced peritoneal cancer leading to the extrinsic
compression and obstruction of the lumen, a transanal colonic
decompression tube was placed in the sigmoid colon as palliative
therapy.
In the recent guidelines (6,7), the use
of SEMS as a bridge to elective surgery is not recommended for
patients with curable left-sided colorectal malignant obstruction.
One reason is that stent appears to adversely affect the
oncological safety, without a reduction in postoperative mortality,
whereas the technical and clinical success rates for stenting were
lower than expected. It is suggested that the procedure may be
considered to be an acceptable alternative treatment option in
patients aged >70 years and/or with an American Society of
Anesthesiologists (ASA) score of ≥III (6,7).
However, as recognized by several other studies through comparing
preoperative SEMS with emergency surgery, the use of SEMS in the
acute phase has the definite advantage: It allows for rapid
decompression of the colon, gaining valuable time to stabilize the
patient's clinical condition and design an optimal treatment plan,
overall resulting in higher successful primary anastomosis and
lower stoma rates, without a significant difference in terms of
complications or mortality (8,19–23).
In practice, it appears that the decision to place a
SEMS or operate should be made by joint consultation between
patients, gastroenterologists and surgeons, with the risks and
benefits weighed carefully. At our Unit, SEMS placement mainly
serves as a bridge to colorectal cancer surgery (Table II). There was an interval of 3–7
days following stenting, which allowed for staging and systemic
evaluation of the candidates' fitness for surgical resection. A
total of 8 patients were found to have extensive multiple
metastases; thus, stenting was used as permanent palliative
therapy. The remaining 44 patients achieved one-stage surgery.
To achieve a better surgical outcome, it is crucial
to improve the safety and efficiency of the stenting procedure. The
main reason for technical failure of stenting is the inability to
pass through the stenosis with a guidewire or the deployment system
due to the severity of the obstruction or its angularity (8,15). It
has been suggested that SEMS should be placed by an experienced
gastroenterologist, such as one who has independently placed at
least 10–20 stents (7–9,24). In
our Institution, four skilled operators meet that standard for
performing SEMS, including an ERCP-specialized endoscopist. The
technical and clinical success rates were 98 and 100%,
respectively. SEMS was also successfully implanted in the
transverse colon in 1 case (Table
II). Correct placement of the guidewire beyond the stricture is
crucial for safe SEMS insertion. In our study, the TTS approach was
accomplished with the assistance of a thin endoscope. This
small-caliber endoscope (GIF XP260; Olympus) proved to be useful
for transverse severe strictures and, hence, allowed placement of
the guidewire without fluoroscopy. Only in 1 case with near
complete obstruction of the descending colon, stent placement was
performed under radiographic image monitoring and endoscopic
guidance (Fig. 3). The procedure was
performed by a skilled endoscopist with therapeutic ERCP experience
(264 procedures per year). It has been well-established that
CO2 as a contrast agent is safe and efficient for
guiding stent placement (12).
CO2 insufflation was applied at the time of the
procedure and no complications were observed post-procedure. Our
experience may also highlight the importance of the skills that
therapeutic ERCP endoscopists have attained in traversing complex
strictures, understanding radiographs and deploying stents
(7).
Of note, the placement of SEMS has additional risks
to be considered in order to achieving maximal safety, such as the
diameter and the length of the stent, which may affect technical
success and complication rates (12). There are reports that stents <25
mm in diameter are associated with increased migration and those
>25 mm with higher perforation rates (8). A stent 20 mm in diameter was selected,
which fits through the working channel of a thin endoscope. The
length of SEMSs used was 6, 8 and 10 cm. It is crucial to measure
the tumor size while passing a guidewire. Subsequently, according
to the length of the tumor, a stent length of at least 2 cm longer
compared with that of the stricture was selected. In addition, the
TTS approach allows for accurate SEMS positioning under direct
vision, aligning the upper end of the stent beyond the tumor margin
for ~1 cm. In this manner, no migration or perforation was observed
in any of the cases.
The retrospective analysis of the data indicates
certain limitations, including different operators with variable
experience and, most importantly, the follow-up was not recorded
for those patients with SEMS placement followed by surgery.
However, in our opinion, urgent colonoscopy as a minimally invasive
approach has its own advantages in managing acute colorectal
obstruction. Furthermore, active discussion should be fostered
among the emergency, surgery/trauma and endoscopy departments to
determine the optimal option for individual patients.
Acknowledgements
The authors would like to thank all the staff at the
Endoscopy Unit of Tongji Hospital for their contributions. We would
especially like to thank Mrs. Ji-Feng Hu, Mrs. Ming Zhang and Mrs.
Qing Zhou for collecting the clinical data for this manuscript.
This study was supported by the National Natural Science Foundation
of China (grant no. 81471612).
References
|
1
|
ASGE Standards of Practice Committee, ;
Harrison ME, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T,
Cash BD, Fanelli RD, Fisher L, Fukami N, et al: The role of
endoscopy in the management of patients with known and suspected
colonic obstruction and pseudo-obstruction. Gastrointest Endosc.
71:669–679. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Olmi S, Scaini A, Cesana G, Dinelli M,
Lomazzi A and Croce E: Acute colonic obstruction: Endoscopic
stenting and laparoscopic resection. Surg Endosc. 21:2100–2104.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Muller KE, Arató A, Lakatos PL, Papp M and
Veres G: Foreign body impaction in the sigmoid colon: A twenty euro
bet. World J Gastroenterol. 19:3892–3894. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Singaporewalla RM, Tan DE and Tan TK: Use
of endoscopic snare to extract a large rectosigmoid foreign body
with review of literature. Surg Laparosc Endosc Percutan Tech.
17:145–148. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Araghizadeh F: Fecal impaction. Clin Colon
Rectal Surg. 18:116–119. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cetinkaya E, Dogrul AB and Tirnaksiz MB:
Role of self expandable stents in management of colorectal cancers.
World J Gastrointest Oncol. 8:113–120. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
van Hooft JE, van Halsema EE, Vanbiervliet
G, Beets-Tan RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones
RG, Hassan C, Jimenez-Perez J, et al: Self-expandable metal stents
for obstructing colonic and extracolonic cancer: European Society
of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy.
46:990–1053. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Geraghty J, Sarkar S, Cox T, Lal S,
Willert R, Ramesh J, Bodger K and Carlson GL: Management of large
bowel obstruction with self-expanding metal stents. A multicentre
retrospective study of factors determining outcome. Colorectal Dis.
16:476–483. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Williams D, Law R and Pullyblank AM:
Colorectal stenting in malignant large bowel obstruction: The
learning curve. Int J Surg Oncol. 2011:9178482011.PubMed/NCBI
|
|
10
|
Repici A, Adler DG, Gibbs CM, Malesci A,
Preatoni P and Baron TH: Stenting of the proximal colon in patients
with malignant large bowel obstruction: Techniques and outcomes.
Gastrointest Endosc. 66:940–944. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Keswani RN, Azar RR, Edmundowicz SA, Zhang
Q, Ammar T, Banerjee B, Early DS and Jonnalagadda SS: Stenting for
malignant colonic obstruction: A comparison of efficacy and
complications in colonic versus extracolonic malignancy.
Gastrointest Endosc. 69:675–680. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Baron TH, Kee Song LM Wong and Repici A:
Role of self-expandable stents for patients with colon cancer (with
videos). Gastrointest Endosc. 75:653–662. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Di Giorgio P, De Luca L, Rivellini G,
Sorrentino E, D'amore E and De Luca B: Endoscopic dilation of
benign colorectal anastomotic stricture after low anterior
resection: A prospective comparison study of two balloon types.
Gastrointest Endosc. 60:347–350. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ferlitsch A, Reinisch W, Püspök A, Dejaco
C, Schillinger M, Schöfl R, Pötzi R, Gangl A and Vogelsang H:
Safety and efficacy of endoscopic balloon dilation for treatment of
Crohn's disease strictures. Endoscopy. 38:483–487. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Adler DG: Colonic strictures: Dilation and
stents. Gastrointest Endosc Clin N Am. 25:359–371. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bravi I, Ravizza D, Fiori G, Tamayo D,
Trovato C, De Roberto G, Genco C and Crosta C: Endoscopic
electrocautery dilation of benign anastomotic colonic strictures: A
single-center experience. Surg Endosc. 30:229–232. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Brandimarte G, Tursi A and Gasbarrini G:
Endoscopic treatment of benign anastomotic colorectal stenosis with
electrocautery. Endoscopy. 32:461–463. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shin SJ, Kim TI, Kim BC, Lee YC, Song SY
and Kim WH: Clinical application of self-expandable metallic stent
for treatment of colorectal obstruction caused by extrinsic
invasive tumors. Dis Colon Rectum. 51:578–583. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ng KC, Law WL, Lee YM, Choi HK, Seto CL
and Ho JW: Self-expanding metallic stent as a bridge to surgery
versus emergency resection for obstructing left-sided colorectal
cancer: A case-matched study. J Gastrointest Surg. 10:798–803.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang X, Lv B, Zhang S and Meng L:
Preoperative colonic stents versus emergency surgery for acute
left-sided malignant colonic obstruction: A meta-analysis. J
Gastrointest Surg. 18:584–591. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tan CJ, Dasari BV and Gardiner K:
Systematic review and meta-analysis of randomized clinical trials
of self-expanding metallic stents as a bridge to surgery versus
emergency surgery for malignant left-sided large bowel obstruction.
Br J Surg. 99:469–476. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Occhionorelli S, Tartarini D, Cappellari
L, Stano R and Vasquez G: Colonic stent placement as a bridge to
surgery in patients with left-sided malignant large bowel
obstruction. An observational study. G Chir. 35:283–289.
2014.PubMed/NCBI
|
|
23
|
Sagar J: Role of colonic stents in the
management of colorectal cancers. World J Gastrointest Endosc.
8:198–204. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Katsanos KH, Maliouki M, Tatsioni A,
Ignatiadou E, Christodoulou DK, Fatouros M and Tsianos EV: The role
of colonoscopy in the management of intestinal obstruction: A
20-year retrospective study. BMC Gastroenterol. 10:1302010.
View Article : Google Scholar : PubMed/NCBI
|