Introduction
Primary central nervous system (CNS) lymphomas
originating from the brain, leptomeninges, spinal cord, or eyes are
rare tumors, accounting for <2% of all cerebral neoplasms
(1). Local mass effect may result in
ocular involvement, or focal lesion of the cranial nerve roots. As
the blood-brain barrier may impair drug delivery, the available
treatments for primary natural killer (NK)/T-cell lymphomas are
limited. Early possible diagnostic neuroimaging is therefore
important. Positive cerebrospinal fluid cytology or brain biopsy
results may provide definitive proof of primary NK/T-cell
lymphomas. Modern imaging technology has demonstrated that these
lesions have a characteristic appearance on neuroimaging. Typical
NK/T-cell lymphomas appear as hypointense lesions on long
TR-weighted magnetic resonance imaging (MRI) of the brain. Lesions
exhibiting enhancement on computed tomography (CT) scans following
contrast administration are considered to be deposits of lymphoma
cells (2). In particular, increased
glycose metabolism in areas of the brain on positron emission
tomography (PET)-CT is an important distinguishing characteristic
of these lesions (3).
The majority of extranodal NK/T-cell lymphomas are
pathological entities distinct from B- or T-cell lymphomas. Primary
NK/T-cell lymphomas are more rare and, although generally rare,
they are more commonly encountered in individuals of Asian descent.
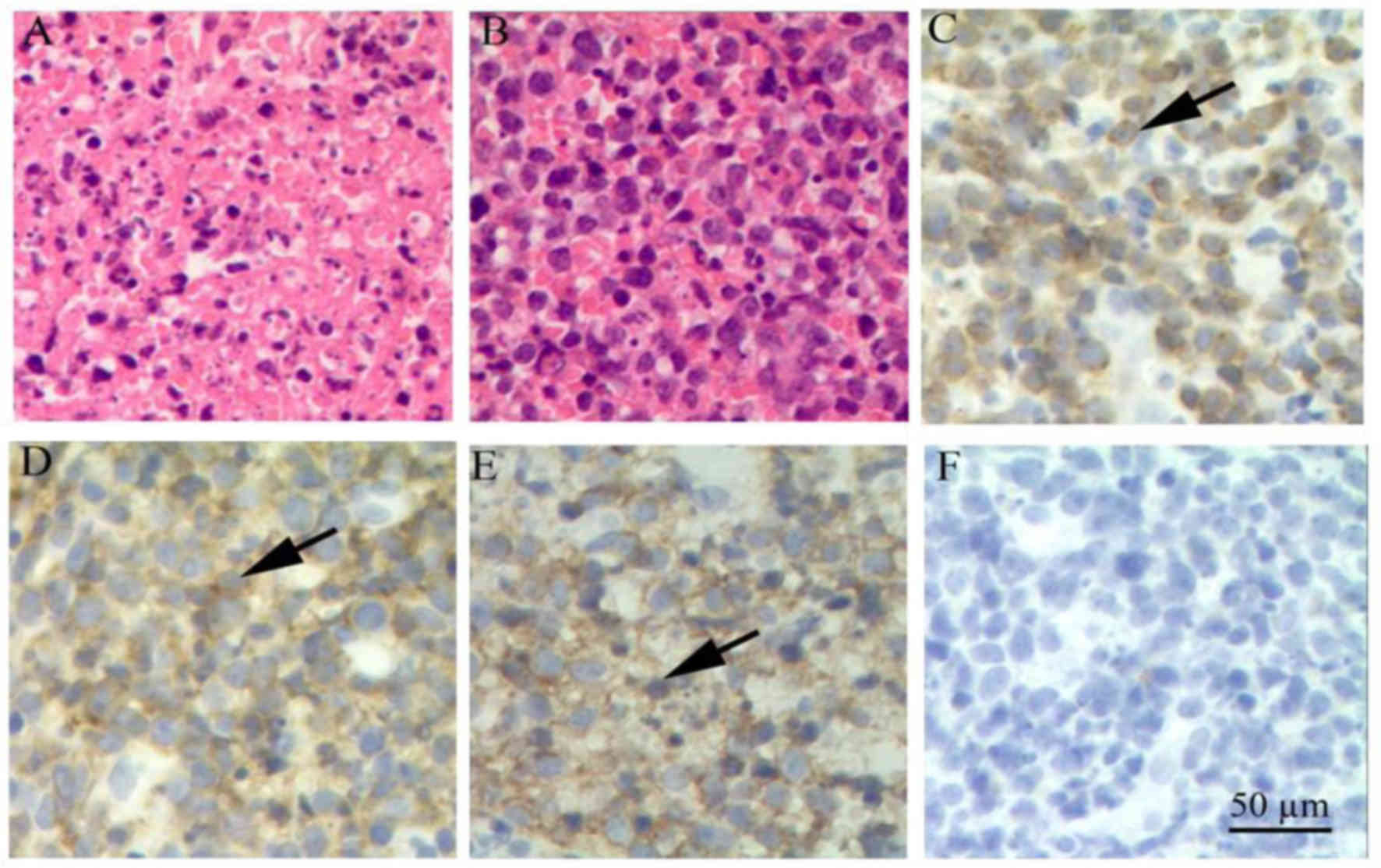
On immunohistochemical examination, lesions of extranodal NK/T-cell
lymphomas often consist of CD2-positive, surface CD3-negative,
cytoplasmic CD3-positive and CD57-positive cells (4,5). As
extranodal NK/T-cell lymphomas often affect the nasal cavity, they
frequently present in midline facial structures accompanied with
nasal obstruction. However, NK/T-cell lymphomas causing cavernous
sinus syndrome via direct destruction of the cavernous sinus and
cranial nerves are rarely reported.
Case report
A 39-year-old man in good general health was first
admitted to The First Affiliated Hospital of Jinan University
(Guangzhou, China) on November 17, 2013. The patient presented with
sudden onset of epistaxis and was admitted to the ENT department
due to diagnosis of nasal polyps by nasal endoscopy. On November 27
(3 days after nasal surgery), the patient developed fever, headache
and diplopia associated with pain in the right orbital region. Due
to worsening of the symptoms, he was referred to the Neurology
Department. On neurological examination, there was paralysis of the
right III and VI cranial nerves, with ptosis and bilateral eyelid
edema. The right pupil measured 4.0 mm and did not constrict to
direct light; the left pupil measured 3 mm and the pupillary light
reflex was normal. A peanut-sized nodule was found in right medial
canthus. Sensation in the area of right trigeminal nerve was lost.
The patient's diplopia was associated with ophthalmoplegia and
third and sixth cranial nerve palsy on the right side. The findings
of the general examination and chest radiograph were normal. The
result of the laboratory examinations were as follows: The
erythrocyte sedimentation rate was 50 mm/h and the high-sensitivity
C-reactive protein was 91.79 mg/l. Diagnostic lumbar spinal
puncture on December 19 revealed a high pressure of 195
mmH20. The nasal secretions culture was positive for
Enterococcus avium and the cerebrospinal fluid culture was
positive for Staphylococcus aureus. A naso-antral CT scan
revealed paranasal sinusitis, which was attributed to inflammation
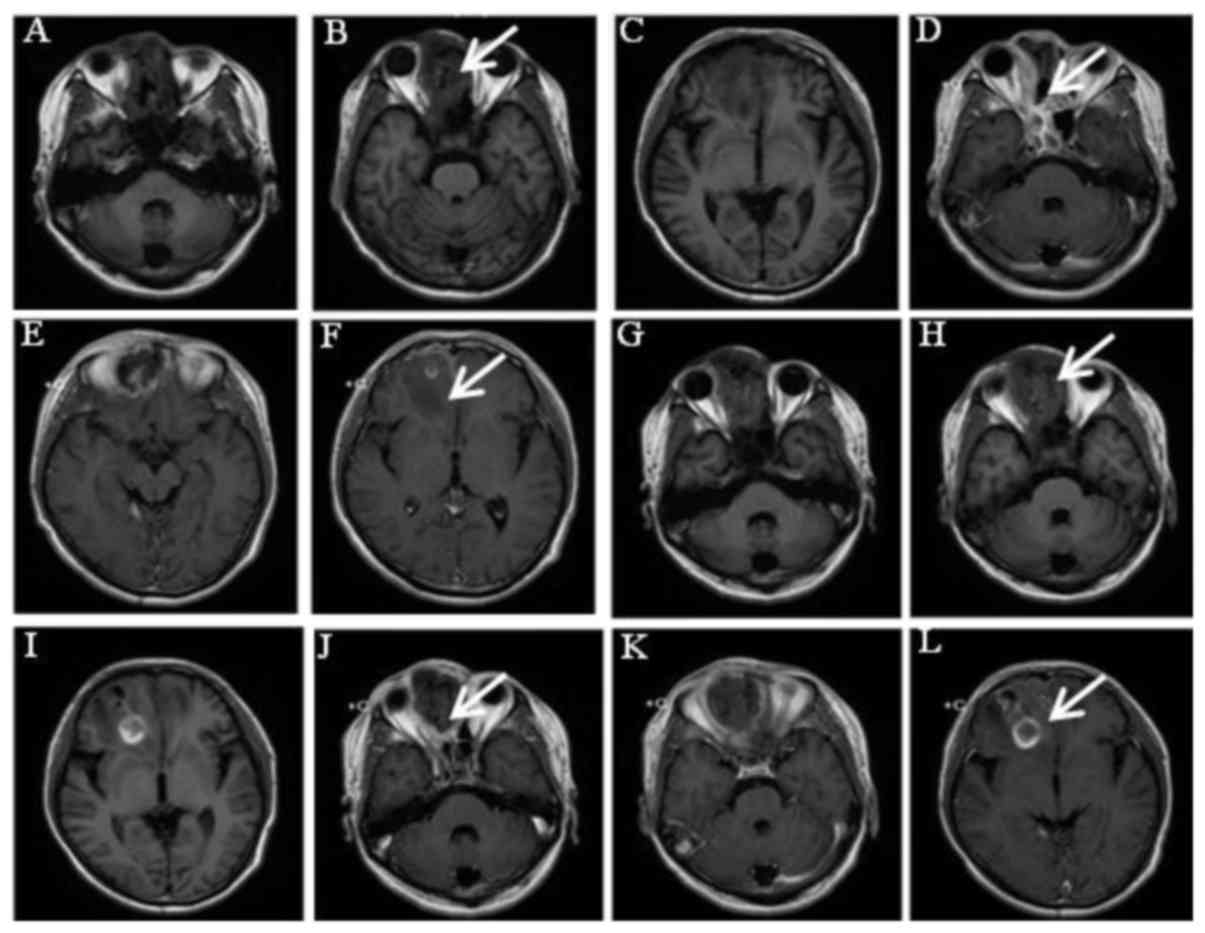
following bilateral nasal polypectomy on December 7. A brain MRI on
December 16 showed an area of abnormal signal in the right frontal
lobe and cranium (Fig. 1). Compared
to the former MRI, moderate annular enhancement of the lesion was
observed, exhibiting T2-weighted hyperintensity and T1-weighted
hypointensity in the right frontal lobe. The maxillary sinus
bilaterally, the sphenoid sinus and the frontal sinus exhibited
long T1 and T2 signal. The mucosa of the sinus wall exhibited an
annular enhancement sign on enhancement scan. Repeat MRI after 1
month showed progression of the lesions in the frontal lobe
(Fig. 1). The patient improved
rapidly within 7 days after the initiation of ceftriaxone sodium
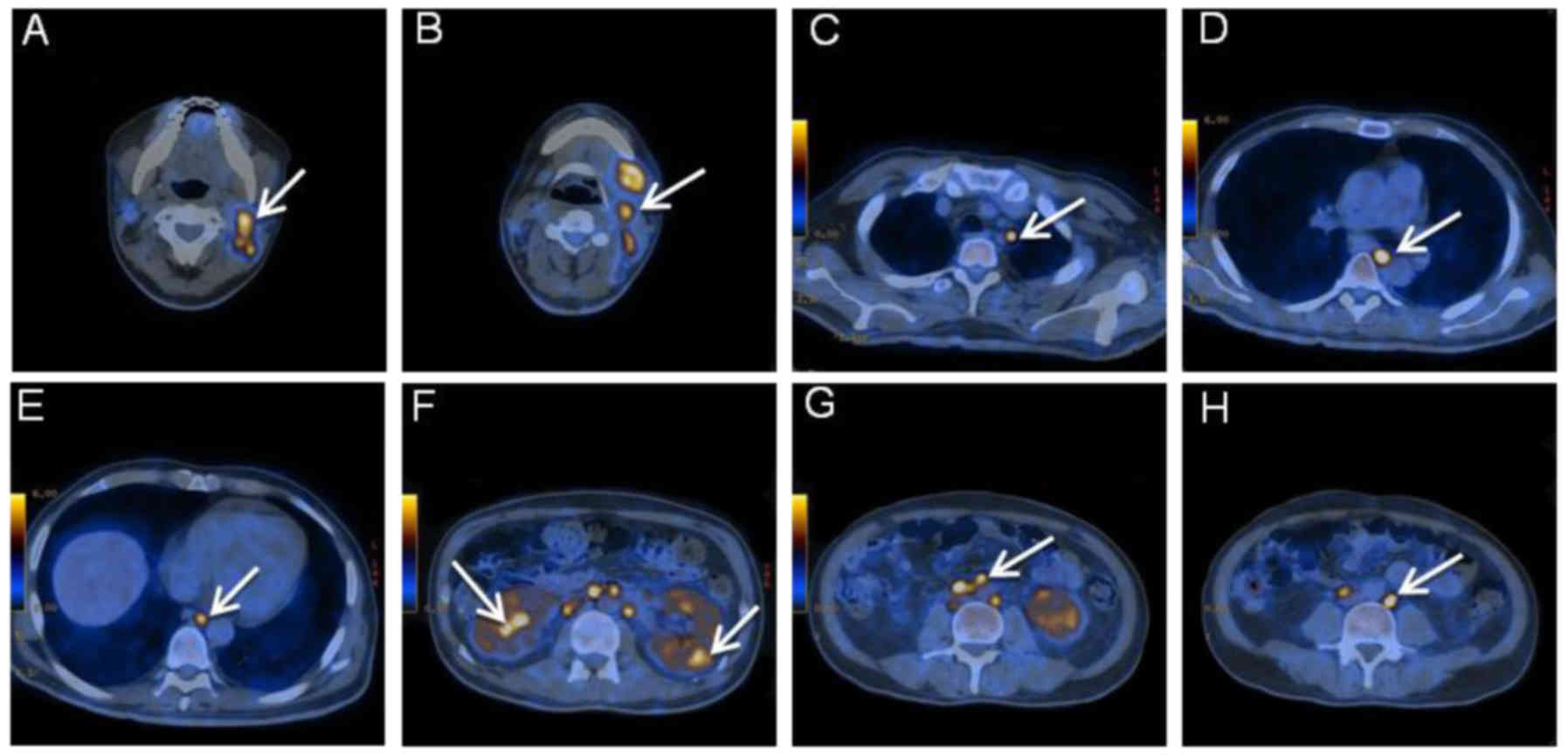
and glucocorticoid treatment. The glycose metabolism was found to
be increased in the right side of the nose, cavernous sinus and
sphenoid sinus on PET-CT examination (Fig. 2). Following pathological examination,
the patient was diagnosed with lymphoma metastatic to the lymph
nodes.
Further investigation identified the mass from the
nasal cavity as extranodal NK/T-cell lymphoma (Fig. 3). Re-examination of the cranial
nerves revealed partial recovery of the III and VI nerves. The
symptoms of fever, headache and diplopia associated with pain in
the right orbital region subsided significantly following
antibiotic and glucocorticoid treatment. However, similar severe
symptoms suddenly developed, accompanied by muscle twitching in the
limbs and coma. The right eye developed severe erythema and edema,
with fever and headache. The patient developed kidney and heart
failure and succumbed to the disease 4 months after the initial
diagnosis.
Discussion
Cavernous sinus syndrome was first described by Foix
in 1921 (also referred to as Foix's syndrome) and is most commonly
caused by vascular disease, tumors and the Tolosa-Hunt syndrome
(6). An investigation of 102
cavernous sinus syndrome patients revealed that 69% of the cases
resulted from tumors, 19% from vascular diseases and 12% from
inflammation. Another etiological study including 151 cavernous
sinus syndrome patients also reported similar results, namely that
the major causative factors are tumors (7). Primary brain tumors, such as
meningiomas, as well as metastatic brain tumors may lead to
cavernous sinus syndrome. Non-Hodgkin lymphoma (NHL) comprises a
group of aggressive lymphoproliferative malignancies originating
from lymphoid tissue that usually invade the CNS (8). However, there is currently a lack of
reports on cavernous sinus syndrome from NHL. Extranodal NK/T-cell
lymphoma presenting with cavernous sinus is more rare in clinical
practice, with very few cases reported to date.
Extranodal NK/T-cell lymphomas are uncommon, highly
aggressive malignant lymphomas, which exhibit a strong association
with episomal Epstein-Barr virus (9)
and have a higher incidence in Asia, Mexico and South America
(10). The nasal cavity is the most
common site of involvement, as was the case in our patient, who
presented with sudden onset of epistaxis; however, other sites were
also affected, including the paranasal sinuses, pharynx and CNS,
where destructive lesions may present with nasal obstruction,
facial pain, or edema. The case reported herein is significant. The
cavernous sinus is a pentahedron that contains cranial nerves b, c,
d and e and the carotid artery. When the cavernous sinus is
affected by traumatic or infectious lesions, vascular or neoplastic
processes, the presenting signs and symptoms may include orbital or
retroorbital pain, diplopia and Horner's syndrome due to the
involvement of one or more related eye muscles and nerves or
branches of the trigeminal nerve.
Histologically, NK/T-cell lymphomas typically
express both T-cell and NK-cell immunophenotypes and NK and T cells
share a common ontogenesis and express cytoplasmic CD3 antigen
(11). In addition, NK cells
consistently express CD56 and CD57, which are considered as
NK-associated antigens (12).
In the present case, the patient was originally
admitted to the hospital with fever of unknown origin and
epistaxis, which may be easily misdiagnosed as a common cold.
However, the typical symptoms or signs of cavernous sinus syndrome,
together with abnormal solid lesions on MRI, should raise concerns
in the attending doctors, as early findings may affect later
diagnostic testing and treatment. PET-CT is useful for staging and
is recommended in the clinical setting when more accurate
evaluation may alter management. PET-CT has a higher sensitivity in
aggressive extranodal NK/T-cell lymphomas when compared with CT
alone and is widely recognized as the most sensitive and specific
imaging for patients with NHL, particularly extranodal NK/T-cell
lymphomas (13). When PET/CT is
unavailable, CT or MRI may be considered.
As extranodal NK/T cell lymphoma is one of the most
difficult subtypes to treat and is associated with a poor
prognosis, current treatment strategies are adopted from
retrospective analyses and have not been clear defined. Reviewing
the treatment strategies, these currently include radiotherapy,
intensive chemotherapy and surgery for patients with early-stage
disease. For remission of early-stage lymphomas, the role of
hematopoietic stem cell transplantation is not indicated for
prospective evaluation. Radiotherapy together with chemotherapy is
the standard approach for localized disease. Systemic chemotherapy
consisting of CNS prophylaxis for this patient remains the mainstay
of treatment (14). The indication
for patients with CNS involvement is early recurrence with rapid
progression, which was the case in our patient. However, no
treatment has been found to be sufficiently effective, and this
malignancy manifests early signs of aggression. It was previously
reported that the median survival time of nasal-type extranodal
NK/T-cell lymphoma is 2 years in patients responding poorly to
standard therapies (15).
Accompanied by systemic progression of this disease, death often
ensues within 1 year of diagnosis.
In summary, we herein present the case of a patient
with cavernous sinus syndrome, in which an autopsy confirmed
extranodal NK/T-cell lymphoma with multiple metastases. MRI and
PET-CT imaging should provide sufficient evidence for the diagnosis
of early-stage extranodal NK/T-cell lymphoma and early treatment of
aggressive disease may significantly improve outcome. Clinicians
should apply the findings from clinical studies to targeted
therapy.
Acknowledgements
The present study was supported by grants from the
National Natural Science Foundation of China (nos. 81171084 and
81671167), the Science and Technology Program of Guangzhou (nos.
155700029 and 1561000289), the Natural Science Foundation of
Guangdong Province (no. 2014A030313384) and the Medical Scientific
Research Foundation of Guangdong Province (no. A2014381), P.R.
China.
References
|
1
|
Liu JK, Sayama C, Chin SS and Couldwell
WT: Extranodal NK/T-cell lymphoma presenting as a pituitary mass.
Case report and review of the literature. J Neurosurg. 107:660–665.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kwong YL: Natural killer-cell
malignancies: Diagnosis and treatment. Leukemia. 19:2186–2194.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Khong PL, Pang CB, Liang R, Kwong YL and
Au WY: Fluorine-18 fluorodeoxyglucose positron emission tomography
in mature T-cell and natural killer cell malignancies. Ann Hematol.
87:613–621. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sitthinamsuwan P, Pongpruttipan T,
Chularojmontri L, Pattanaprichakul P, Khuhapinant A and
Sukpanichnant S: Extranodal NK/T cell lymphoma, nasal type,
presenting with primary cutaneous lesion mimicking granulomatous
panniculitis: A case report and review of literature. J Med Assoc
Thai. 93:1001–1007. 2010.PubMed/NCBI
|
|
5
|
Sun JC and Lanier LL: NK cell development,
homeostasis and function: Parallels with CD8+ T cells. Nat Rev
Immunol. 11:645–657. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen SM, Chang CN, Wei KC, Jung SM and
Chuang CC: Sellar lymphoma mimicking sphenoid infection presenting
with cavernous sinus syndrome. J Clin Neurosci. 15:1148–1151. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Keane JR: Cavernous sinus syndrome.
Analysis of 151 cases. Arch Neurol. 53:967–971. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jahnke K, Thiel E, Martus P, Schwartz S
and Korfel A: Retrospective study of prognostic factors in
non-Hodgkin lymphoma secondarily involving the central nervous
system. Ann Hematol. 85:45–50. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li Z, Xia Y, Feng LN, Chen JR, Li HM, Cui
J, Cai QQ, Sim KS, Nairismägi ML, Laurensia Y, et al: Genetic risk
of extranodal natural killer T-cell lymphoma: A genome-wide
association study. Lancet Oncol. 17:1240–1247. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kwong YL, Kim WS, Lim ST, Kim SJ, Tang T,
Tse E, Leung AY and Chim CS: SMILE for natural killer/T-cell
lymphoma: Analysis of safety and efficacy from the Asia lymphoma
study group. Blood. 120:2973–2980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chan JK, Tsang WY and Ng CS: Clarification
of CD3 immunoreactivity in nasal T/natural killer cell lymphomas:
The neoplastic cells are often CD3 epsilon+. Blood. 87:839–841.
1996.PubMed/NCBI
|
|
12
|
Sabattini E, Bacci F, Sagramoso C and
Pileri SA: WHO classification of tumours of haematopoietic and
lymphoid tissues in 2008 An overview. Pathologica. 102:83–87.
2010.PubMed/NCBI
|
|
13
|
Kasenda B, Haug V, Schorb E, Fritsch K,
Finke J, Mix M, Hader C, Weber WA, Illerhaus G and Meyer PT:
18F-FDG PET is an independent outcome predictor in primary central
nervous system lymphoma. J Nucl Med. 54:184–191. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tse E and Kwong YL: How I treat NK/T-cell
lymphomas. Blood. 121:4997–5005. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee
JH, Lee DH, Huh J, Oh SY, Kwon HC, et al: Extranodal natural killer
T-cell lymphoma, nasal-type: A prognostic model from a
retrospective multicenter study. J Clin Oncol. 24:612–618. 2006.
View Article : Google Scholar : PubMed/NCBI
|