Introduction
Xerostomia in head and neck (H&N) cancer
patients following radiation treatment (RT) is caused by
locoregional and permanent damage to the salivary glands in the RT
field (1). Xerostomia is a common
complaint, significantly affecting the quality of life (QoL) of the
patients. The prevalence of xerostomia has been reported to range
between 73.5 and 93% (2,3). Unfortunately, precise evaluation of
radiation-induced xerostomia requires morphological and functional
assessment methods, such as histological evaluation, computed
tomography, magnetic resonance (MR) imaging and ultrasonography, MR
sialography and scintigraphy. As these methods are technically
complex and practically non-applicable in the clinical setting, and
xerostomia is primarily a subjective symptom, its assessment mainly
relies on patient self-reports. Longitudinal studies in H&N
cancer patients support the hypothesis that the feeling of
xerostomia increases and QoL decreases during and directly after
treatment and is restored to pretreatment levels at least after 12
months, despite any remaining functional disability (4). Despite extensive research in this
field, only a limited number of studies have simultaneously
investigated the association between QoL, the general subjective
feeling of xerostomia, and the amount of saliva during and after
RT, whereas it remains uncertain whether and to what extent
objective signs are in accordance with subjective symptoms
(5,6). Modern RT techniques, such as
intensity-modulated RT (IMRT), which are able to spare a large
volume of the salivary glands, have been developed (2). However, a significant number of
patients cannot benefit from these techniques, mainly due to
financial restraints, with the most representative example being
the current state of the public hospitals in Greece. The financial
crisis Greece has been experiencing over the last decade has
adversely affected the availability of medical resources and
services. New RT techniques are currently not available in Greece
due to the lack of expertise and the fact that there are no
available funds for the replacement of the existing linear
accelerators with new ones and for training the medical staff in
the new technology. However, QoL and xerostomia must be assessed
with widely accepted and adequately validated tools for valid and
reliable data to be obtained. In that context, the aim of the
present study was to investigate the associations among these three
variables (QoL, xerostomia and quantity of saliva) in a sample of
Greek H&N cancer patients who were treated with conventional
RT.
Materials and methods
Patients
The present study was conducted at the outpatient
clinics of the Department of Radiation Therapy of the University
Hospital of Larissa (Larissa, Greece), the ‘Theagenio’ Cancer
Hospital (Thessaloniki, Greece) and the ‘AHEPA’ University Hospital
of Thessaloniki (Thessaloniki, Greece) between 2014 and 2015.
Patients with H&N cancer comprised the study population. The
exclusion criteria were as follows according to the literature: i)
Salivary gland cancer, ii) psychiatric morbidity, iii) distant
metastases, iv) past RT for H&N irrelevant to the present
disease, v) Sjögren syndrome and other autoimmune diseases, such as
systemic lupus erythematosus and rheumatoid arthritis, vi) diabetes
mellitus, vii) use of antihistamines and anticholinergic drugs or
antipsychotics and viii) use of pilocarpine. Due to the limited
resources, 60 patients were randomly selected from the eligible
subjects to participate in the study.
The patients completed the questionnaires in a
private clinic room in the presence of the primary researcher. All
the patients were adults (aged >18 years), capable of fluent
communication in Greek, with histologically confirmed H&N
cancer and an Eastern Cooperative Oncology Group performance status
of 0–2.
The Radiation Therapy Oncology Group (RTOG)/
European Organisation for Research and Treatment of Cancer (EORTC)
late xerostomia grading was determined during follow-up visits at
the clinic by 3 physicians at each visit. Each of the observers
assigned the score independently and was blinded to the scores
assigned by the others. The scores ranged from 0 to 3 (0, none; 1,
slight dryness of the mouth, good response on stimulation; 2,
moderate dryness, poor response on stimulation; and 3, complete
dryness, no response on stimulation). A mean RTOG/EORTC score was
calculated from the scores provided by the 3 observers and was used
for correlations with the patient reported scores.
Questionnaires
The patients answered three questionnaires at the
same time: The Greek version of the XQ Instrument (7,8) the
EORTC Quality of Life Questionnaire-Core 30 (QLQ-C30) and the
Quality of Life Questionnaire Head and Neck Module (QLQ-H&N35)
(9) from the EORTC group. All the
questionnaires have been validated in the Greek population. The
QLQ-C30 encompasses 30 questions grouped into five functional
scales, nine scales associated with symptoms and a global scale.
The QLQ-H&N35 includes 35 questions, 30 of which are grouped in
13 scales and 5 are simple-answer. This questionnaire addresses
symptoms associated with specific tumor location, side effects
associated with the treatment provided and additional QoL aspects
affected by the disease or its treatment. The answers were
converted into a linear scoring scale, with values between 0 and
100, as per advocated by EORTC (9,10). The
results were expressed as mean values with confidence intervals. A
high score in the questions associated with the symptoms reflects
more prominent symptoms, while a high score in the questions
associated with function reflects a better condition of the
patient. The XQ provides a measure of the severity of
radiation-induced xerostomia that affects the patients' QoL. This
questionnaire consists of 8 questions, 4 of which are associated
with patient-reported dryness while eating or chewing and the
remaining 4 are associated with dryness in the absence of eating or
chewing. The XQ is a self-administered tool and patients are asked
to rate each symptom on an 11-point ordinal Likert scale of 0–10,
with higher scores indicating more severe dryness or discomfort due
to dryness. Each item score is added, and the sum is linearly
transformed to produce the final summary score ranging from 0 to
100, with higher scores representing higher levels of xerostomia.
The results of this questionnaire are correlated with more global
QoL parameters (7,8). The XQ has recently been validated in
the Greek population by the research team conducting the present
study, in an attempt to yield a reliable xerostomia tool for Greek
patients. The Greek version of XQ exhibited excellent validity and
reliability, as well as high correlation with the observers'
estimation of the salivary output (11).
Assessment of unstimulated salivary
flow rate
The unstimulated salivary flow rate was assessed
using the spitting method. Patients were instructed to collect
their saliva for 5 min in a graded tube. The volume of the saliva
was then determined and divided by 5 to obtain a flow reading per
minute. Stimulated salivary flow was determined in the same manner.
Saliva secretion was stimulated by chewing a piece of parafilm, to
avoid chewing gum containing mannitol or other substances that may
interfere with saliva production.
All measurements but QoL ones were conducted at 6
timepoints: i) Initiation of RT, ii) during RT, iii) at the end of
RT, iv) 3 months after RT completion, v) 6 months after RT
completion and vi) 1 year after RT completion.
pH measurement
For pH measurement, commercial kit strips (Simplex
Health, Wollaston, UK) were used. The manufacturers' instructions
for sample preparation were strictly followed: The measurement was
conducted at least 2 h after eating, drinking or brushing teeth.
The patients were instructed not to rinse their mouth and strictly
avoid any beverages/coffee to avoid altering the pH. The patients
spat saliva on a spoon. The pH strip was dipped into the fluid for
~3 sec until both pads on the test strip were sufficiently covered
with liquid. After 15 sec, the color change was compared with the
color chart. The test was repeated three times to obtain an average
reading.
Ethics
All the procedures were conducted in accordance with
the ethical standards of the University Hospital and National
Committees on human experimentation, and with the principles of the
Helsinki Declaration of 1975, as revised in 2000.
Statistical analysis
The distribution and normality of the collected data
were tested using the Shapiro-Wilk test and the Kolmogorov-Smirnov
test. Item analysis was performed using the mean and standard
deviation data of the items. Pearson's and Spearman's correlations
were used as appropriate. The Friedman's test was performed for
repeated measures analysis. Statistical significance was set at
P<0.05. SPSS 22.0 software (IBM Corp., Armonk, NY, USA) was used
to analyze data. SigmaPlot 12.5 and Microsoft Excel 2007 (version
12.00) were used for graph construction.
Therefore, clinicians should be confident with
well-validated instruments in the assessment of xerostomia and
adjust therapeutic regimens as appropriate.
Results
Patient characteristics
The socio-demographic and clinical characteristics
of the participants are summarized in Table I. The mean age of the patients was
61.08 years [standard deviation (SD), 10.07 years] and 80% (48/60)
were men. Half of the patients had laryngeal/hypopharyngeal cancer
and 78.3% had undergone chemotherapy (Table I).
 | Table I.Socio-demographic and clinical
characteristics of the study subjects (n=100). |
Table I.
Socio-demographic and clinical
characteristics of the study subjects (n=100).
| Variables | Values |
|---|
| Gender, n |
|
| Male | 48 |
|
Female | 12 |
| Age, years |
|
| Mean | 61.08 |
| Standard
deviation | 10.07 |
| Tumor location,
n |
|
|
Oropharynx | 9 |
|
Nasopharynx | 9 |
|
Larynx | 28 |
|
Hypopharynx | 2 |
|
Tongue | 12 |
| Chemotherapy |
|
| Yes | 47 |
| No | 13 |
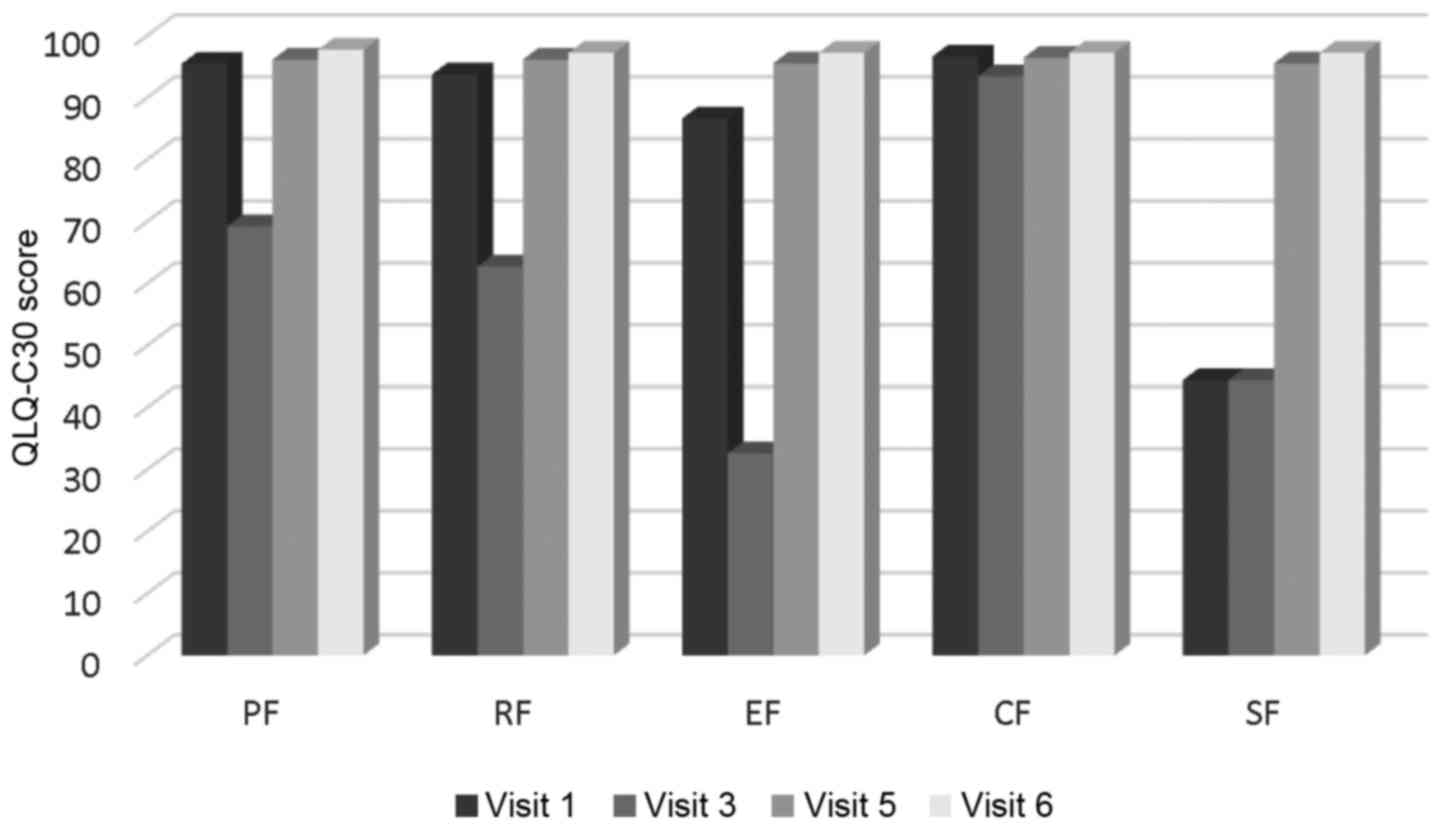
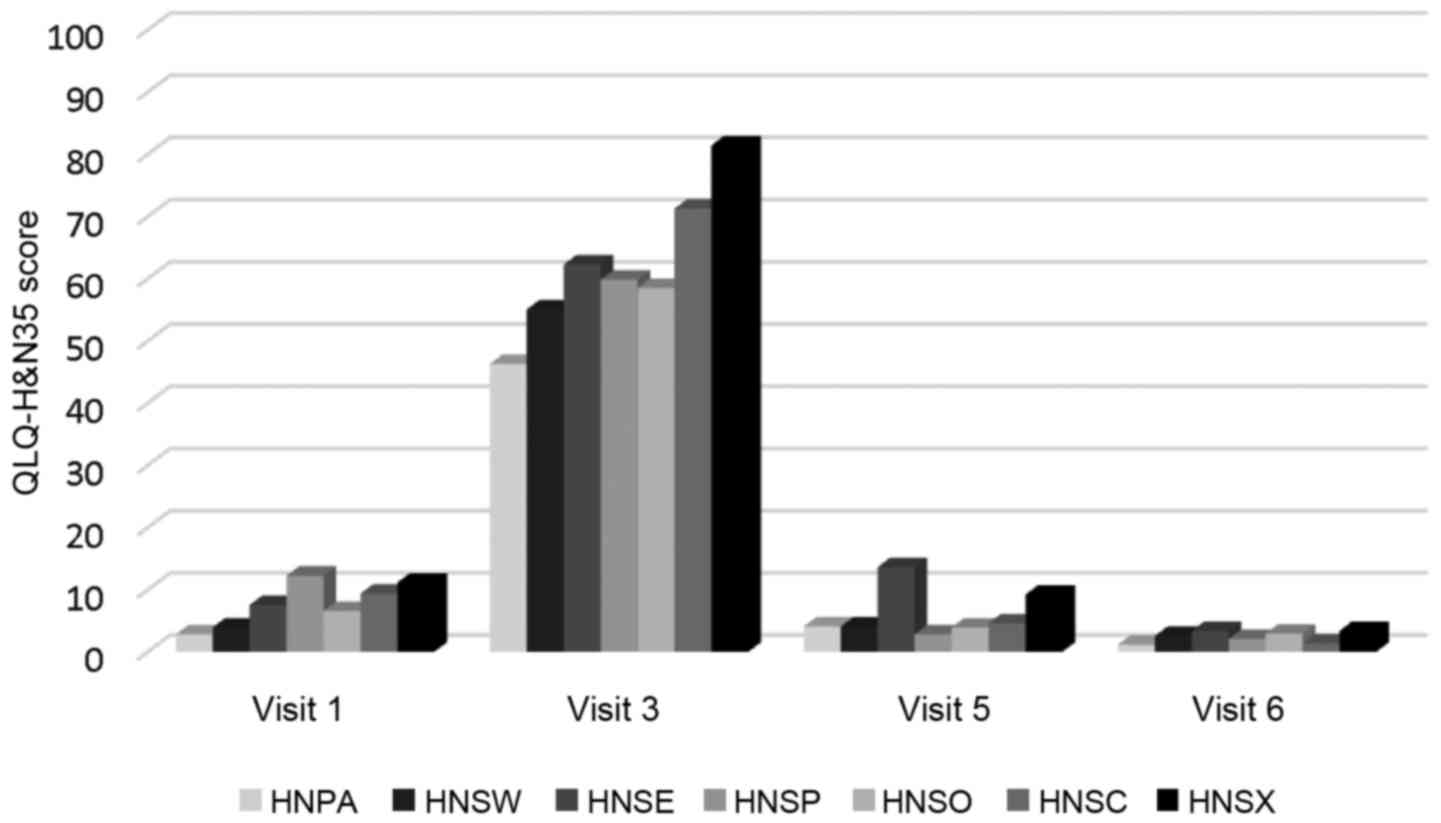
Changes in functional and symptom scales over time.
All functional scales and symptom scales, apart from cognitive
functioning in QLQ-C30 and feeding tube in H&N35, exhibited an
abrupt deterioration at timepoint 3 and were gradually restored
over time. The difference was statistically significant
(P<0.001). The mean XQ values at timepoint 2 were 47.27 (SD,
18.26) indicating a low-to-medium grade of xerostomia (Figs. 1 and 2). XQ scores at different timepoints
exhibited a statistically significant negative correlation with
salivary flow rates, while the difference in XQ score between the
start and endpoint of the study was significantly correlated only
with the corresponding difference in stimulated salivary flow
(r=0.333, P=0.009).
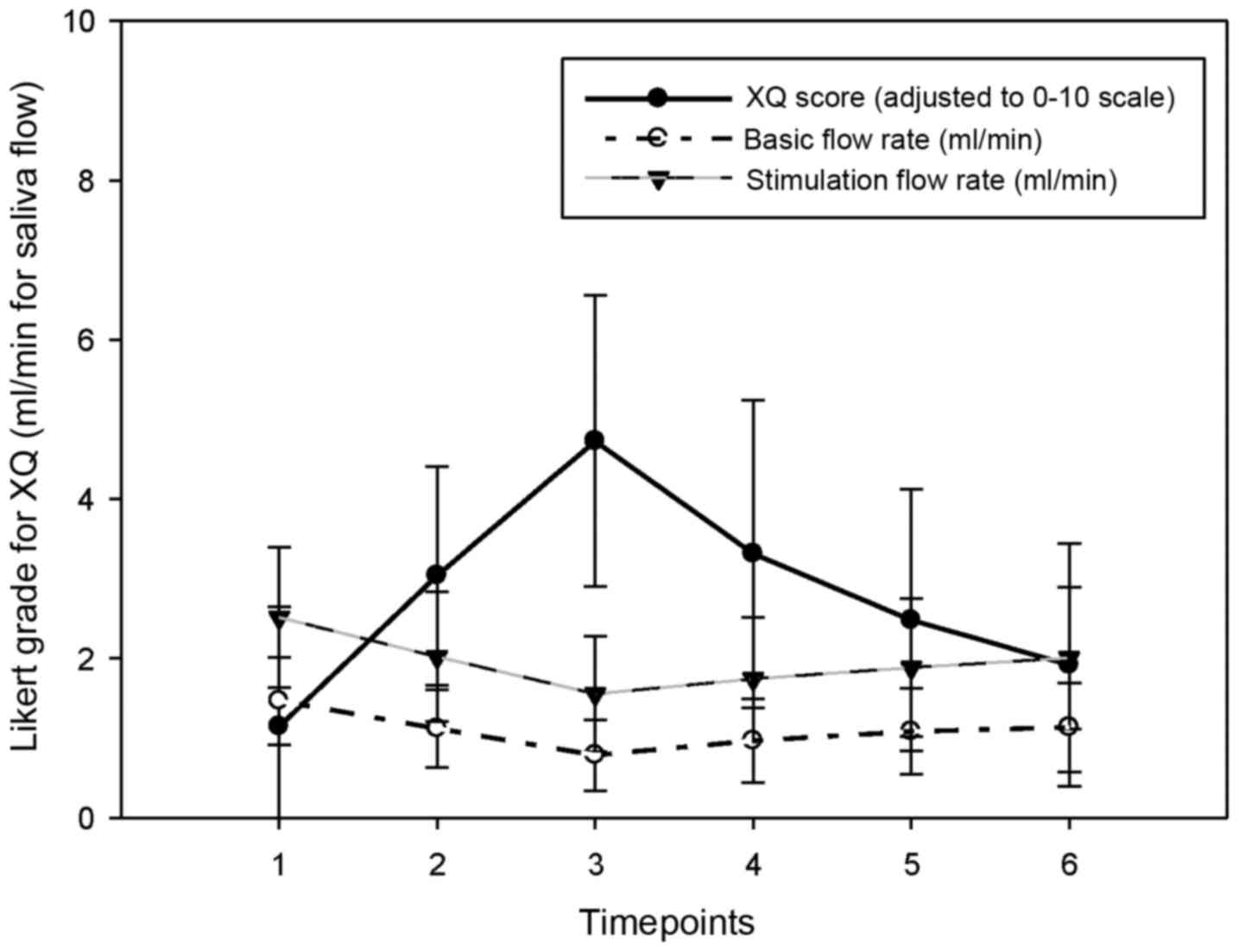
Changes in biochemical indices over time. Salivary
flow rate and XQ scores almost parallelled one another (Fig. 3). The peak in XQ and dip in the flow
rate both occured at timepoint 3. The unstimulated mean flow rate
was at its minimum at timepoint 2 [immediately after RT: 1,12 (SD,
0.49)], while the minimum stimulated flow rate was 2.02 (SD, 0.55)
at the same time. The values gradually recovered to a level of 20%
below baseline values by the end of the follow-up period (Table II).
 | Table II.Changes in biochemical indices over
time. |
Table II.
Changes in biochemical indices over
time.
|
|
Timepointsa |
|---|
|
|
|
|---|
| Indices | 1 | 3 | 5 | 6 | P-value |
|---|
| Unstimulated saliva
volume, ml | 7.33 | 3.93 | 5.42 | 5.68 | <0.001 |
| Stimulated saliva
volume, ml | 12.57 | 7.77 | 9.42 | 10.03 | <0.001 |
| pH | 6.35 | 6.52 | 6.39 | 6.45 | <0.001 |
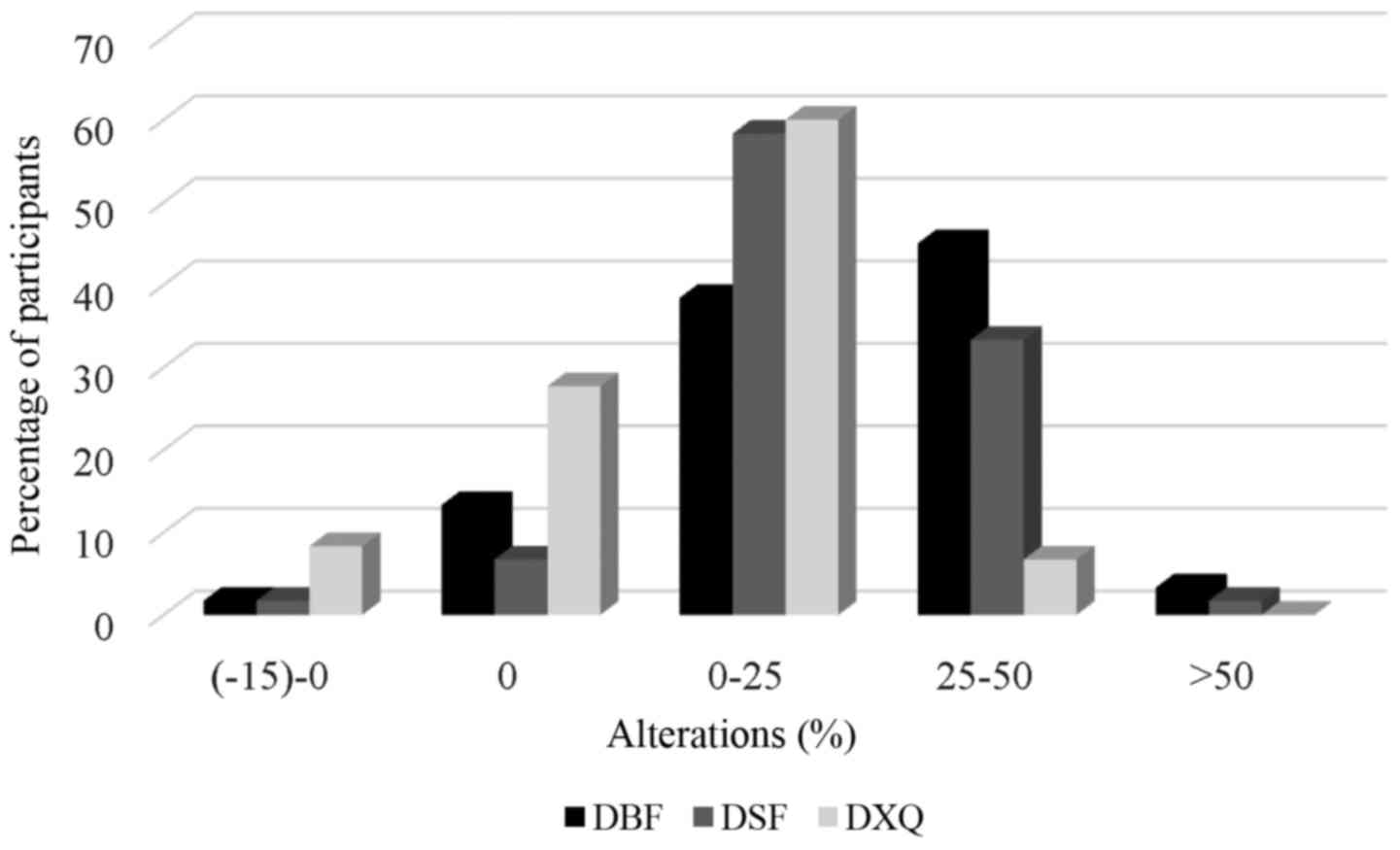
A total of 8.4 and 15% of the patients exhibited a
completely restored or even increased stimulated and unstimulated
salivary flow rate, respectively, while 3.3 and 1.7% of the
participants exhibited >50% loss of unstimulated and stimulated
saliva production, respectively (Fig.
4).
Discussion
The findings of the present study strongly support
the hypothesis that the subjective feeling of xerostomia, as
measured by certain instruments (XQ in this study), may be
well-parallelled with physiological indices, such as salivary flow.
Furthermore, QoL may be particularly compromised following RT,
gradually improving over time and to a significant extent within
the first year after treatment initiation. Data allow some optimism
regarding patients' recovery, as salivary flow after stimulation
shows a significant improvement over time and the functional scales
suggest an almost full recovery of the patients' daily activities.
To the best of our knowledge, this is the first study in Greece to
investigate the associations of QoL with the general subjective
feeling of xerostomia, and the amount of saliva production prior to
and following RT.
There is no consensus on the extent of the
association between the subjective feeling of xerostomia and
objective measures and, despite the validated tools used to
evaluate the salivary gland function, xerostomia is only a
subjective symptom (12). Patients
complaining of xerostomia do not always suffer from hyposalivation
(13), while qualitative changes in
saliva may well affect the feeling of xerostomia, despite adequate
saliva production (14). Moreover,
methodological issues, such as sample selection bias, may affect
the conclusions. The inclusion of patients with advanced disease or
comorbidities may negatively affect the results, while salivary
flow stimulation with not purely mechanical methods may
overestimate saliva production. In the present study, a purely
mechanical method was used for salivary flow stimulation, in order
to avoid misinterpretations. In that context, our results are
likely more representative of the patients' daily symptoms, best
reflecting their basic saliva production. Examining mean cohort
levels of xerostomia may also be misleading, as patients who have a
flow ratio below the critical cut-off (<25%) appeared to
complain the most of a dry mouth (14,15). In
the present study, hyposalivation was not prominent (minimum
baseline salivary flow rate >0.1 ml/min following RT) and, due
to the exclusion criteria, patients with severe comorbidities or
metastatic disease were excluded, whereas no deaths were reported
during the follow-up period. Therefore, terminally ill patients
were not included in the present study.
It is estimated that at least 1 year of follow-up is
required to determine the effect of RT on QoL (12,16).
Thus, the follow-up period in the present study may be considered
as sufficient to provide adequate information in terms of QoL
following RT. Of note, when estimating xerostomia and QoL,
psychological issues should also be taken into consideration. The
psychological shock early in the treatment course may contribute to
the subjective feeling of xerostomia, even in the absence of a
considerable decrease of the amount of saliva, although in the
majority of the patients salivary production decreases
significantly after RT. However, long-term follow-up (>6 months)
indicates that QoL improves over time, although xerostomia may not
be directly associated with QoL. Furthermore, all QoL aspects may
not improve, at least not to the same extent. In the study of Filho
et al, despite some symptom scale deterioration, functional
scale scores remained high throughout the 3-month follow-up,
without significant changes over time, and the overall QoL did not
exhibit any significant changes (17); however, the authors commented on
significant symptom variability. Melo Filho et al (18) reported loss of physical, social and
emotional function and role performance, while Braam et al
(16) observed that, compared to
baseline, patients reported better emotional functioning and worse
social functioning at 12 months, while a better overall health
status was reported at 24 months. The authors of that study
emphasized the contribution of the patients' own beliefs regarding
their illness in terms of QoL prediction after 2 years. When the
patients believed their own behaviour did not affect their outcome,
it predicted better functioning and better overall health and vice
versa.
In the present study, salivary flow rate, QoL and
subjective feeling of xerostomia, as measured by XQ, were almost
parallel. XQ has been previously validated in a Greek H&N
cancer population by the same research team and yielded excellent
psychometric properties (11); its
association with salivary flow rate allows clinicians to reliably
estimate xerostomia and patients' perspective during the follow-up
period, without resorting to laboratory methods.
In the present study, all the functional and symptom
scales declined following RT and significantly improved after the
third timepoint, while salivary flow rates approached or even
surpassed baseline levels in a considerable number of patients. The
sample homogeneity (mostly laryngeal and nasopharyngeal cancer
patients) and the exclusion of terminally ill patients may partly
account for these results. However, financial restraints did not
allow for a larger study sample and the patients, although randomly
selected, may not be representative of all H&N patients
attending public hospitals. Despite receiving conventional
radiation therapy (not IMRT), the participants exhibited a
considerable preservation of salivary gland function after 12
months, allowing for some optimism regarding the course of
xerostomia in selected patients.
References
|
1
|
Guobis Z, Baseviciene N, Paipaliene P,
Sabalys G and Kubilius R: Xerostomia: Clinic, etiology, diagnosis
and treatment. Medicina (Kaunas). 42:171–179. 2006.(In Lithuanian).
PubMed/NCBI
|
|
2
|
Pow EH, Kwong DL, McMillan AS, Wong MC,
Sham JS, Leung LH and Leung WK: Xerostomia and quality of life
after intensity-modulated radiotherapy vs. conventional
radiotherapy for early-stage nasopharyngeal carcinoma: Initial
report on a randomized controlled clinical trial. Int J Radiat
Oncol Biol Phys. 66:981–991. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liu XK, Zeng ZY, Hong MH, Zhang AL, Cui NJ
and Chen FJ: [Clinical analysis of xerostomia in patients with
nasopharyngeal carcinoma after radiation therapy]. Ai Zheng.
23:593–596. 2004.PubMed/NCBI
|
|
4
|
Ledeboer QC, Velden LA, Boer MF, Feenstra
L and Pruyn JF: Physical and psychosocial correlates of head and
neck cancer: An update of the literature and challenges for the
future (1996–2003). Clin Otolaryngol. 30:303–319. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Heutte N, Plisson L, Lange M, Prevost V
and Babin E: Quality of life tools in head and neck oncology. Eur
Ann Otorhinolaryngol Head Neck Dis. 131:33–47. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Meirovitz A, Murdoch-Kinch CA, Schipper M,
Pan C and Eisbruch A: Grading xerostomia by physicians or by
patients after intensity-modulated radiotherapy of head-and-neck
cancer. Int J Radiat Oncol Biol Phys. 66:445–453. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pacholke HD, Amdur RJ, Morris CG, Li JG,
Dempsey JF, Hinerman RW and Mendenhall WM: Late xerostomia after
intensity-modulated radiation therapy versus conventional
radiotherapy. Am J Clin Oncol. 28:351–358. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jabbari S, Kim HM, Feng M, Lin A, Tsien C,
Elshaikh M, Terrel JE, Murdoch-Kinch C and Eisbruch A: Matched
case-control study of quality of life and xerostomia after
intensity-modulated radiotherapy or standard radiotherapy for
head-and-neck cancer: Initial report. Int J Radiat Oncol Biol Phys.
63:725–731. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bjordal K, Hammerlid E, Ahlner-Elmqvist M,
de Graeff A, Boysen M, Evensen JF, Biörklund A, de Leeuw JR, Fayers
PM, Jannert M, et al: Quality of life in head and neck cancer
patients: Validation of the European Organization for Research and
Treatment of Cancer Quality of Life Questionnaire-H&N35. J Clin
Oncol. 17:1008–1019. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Aaronson NK, Ahmedzai S, Bergman B,
Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman
SB, de Haes JC, et al: The European Organization for Research and
Treatment of Cancer QLQ-C30: A quality-of-life instrument for use
in international clinical trials in oncology. J Natl Cancer Inst.
85:365–376. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Memtsa PT, Tolia M, Tzitzikas I, et al:
Validity and reliability of the Greek version of the xerostomia
questionnaire in head and neck cancer patients. Supportive care in
cancer: official journal of the Multinational Association of
Supportive Care in Cancer. 2016.(In press). PubMed/NCBI
|
|
12
|
Kakoei S, Haghdoost AA, Rad M,
Mohammadalizadeh S, Pourdamghan N, Nakhaei M and Bahador M:
Xerostomia after radiotherapy and its effect on quality of life in
head and neck cancer patients. Arch Iran Med. 15:214–218.
2012.PubMed/NCBI
|
|
13
|
Shahdad SA, Taylor C, Barclay SC, Steen IN
and Preshaw PM: A double-blind, crossover study of Biotène
Oralbalance and BioXtra systems as salivary substitutes in patients
with post-radiotherapy xerostomia. Eur J Cancer Care (Engl).
14:319–326. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pinna R, Campus G, Cumbo E, Mura I and
Milia E: Xerostomia induced by radiotherapy: An overview of the
physiopathology, clinical evidence, and management of the oral
damage. Ther Clin Risk Manag. 11:171–188. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Roesink JM, Schipper M, Busschers W,
Raaijmakers CP and Terhaard CH: A comparison of mean parotid gland
dose with measures of parotid gland function after radiotherapy for
head-and-neck cancer: Implications for future trials. Int J Radiat
Oncol Biol Phys. 63:1006–1009. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Braam PM, Roesink JM, Moerland MA,
Raaijmakers CP, Schipper M and Terhaard CH: Long-term parotid gland
function after radiotherapy. Int J Radiat Oncol Biol Phys.
62:659–664. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Scharloo M, de Baatenburg Jong RJ,
Langeveld TP, van Velzen-Verkaik E, den Doorn-Op Akker MM and
Kaptein AA: Illness cognitions in head and neck squamous cell
carcinoma: Predicting quality of life outcome. Support Care Cancer.
18:1137–1145. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Filho Melo MR, Rocha BA, Pires MB, Fonseca
ES, Freitas EM, Junior Martelli H and Santos FB: Quality of life of
patients with head and neck cancer. Braz J Otorhinolaryngol.
79:82–88. 2013. View Article : Google Scholar : PubMed/NCBI
|