The health risk assessment of environmental
selenium, concerning both abnormally low and high intakes, and the
related regulatory guidelines are generally based on ‘old’
evidence, since they have generally been unable to take into
consideration the most recent epidemiologic and biochemical
evidence, and particularly the recent results of large and
well-designed randomized controlled trials (RCTs) (1–3). The
results of these trials, in connection with biochemical and
toxicological studies, have shed new light on this relevant public
health issue. This has happened with reference to both the upper
and the lower limits of selenium intake, which have been so far
based in all the assessment on observational studies carried out in
seleniferous Chinese areas during the 1980s (4,5). The
availability of the experimental studies (the trials) is of
particular importance, since they allowed to rule out the key issue
of (unmeasured) confounding, typically affecting most of
observational studies with the possible only exception of the so
called ‘natural experiments’ (6).
In addition, the recent observational and experimental studies made
it possible to investigate different populations with reference to
age, genetic background and life-style factors, also allowing to
test the health effect of selective exposure to specific selenium
compounds, such as inorganic haxavalent selenium (selenate) and an
organic form, selenomethionine. This is particularly important
since there is growing evidence of the key importance of the
specific selenium forms in influencing the biological activity of
this element, with reference to both its toxicological and
nutritional effects (7–11).
A very large number of epidemiologic studies
assessed the relation between chronic exposure to environmental
selenium and human health. The studies on this issue frequently
investigated the effect on human health of unusually low or high
environmental exposures to selenium, due to an abnormal selenium
content in soil, locally produced foods and drinking water, or
following combustion of coal with high selenium content (5,12,13).
In addition, the scientific literature encompasses a large number
of nutritional epidemiology studies on the long-term health effects
of selenium carried out in populations living in non-seleniferous
regions and countries. These studies include experimental
investigations (randomized controlled trials) and observational
studies, the latter characterized by case-control, cohort,
cross-sectional and ecologic design and being characterized by a
far weaker ability compared with trials in addressing the selenium
and health relation (1,14,15).
While the entire review of this huge literature goes beyond the
possibility of this report, we aim at briefly updating the evidence
generated by the most recent environmental and nutritional studies
on the human health effects of selenium, the biological
plausibility of this relation, an overview of the challenges that
these studies and their interpretation pose, and finally their
implications on the adequacy of current environmental selenium
standards. Our update of this issue starts from the comprehensive
assessments of selenium exposure carried out by the US Institute of
Medicine in 2000 (4) and by a
World Health Organization (WHO) working group in 2004 (16).
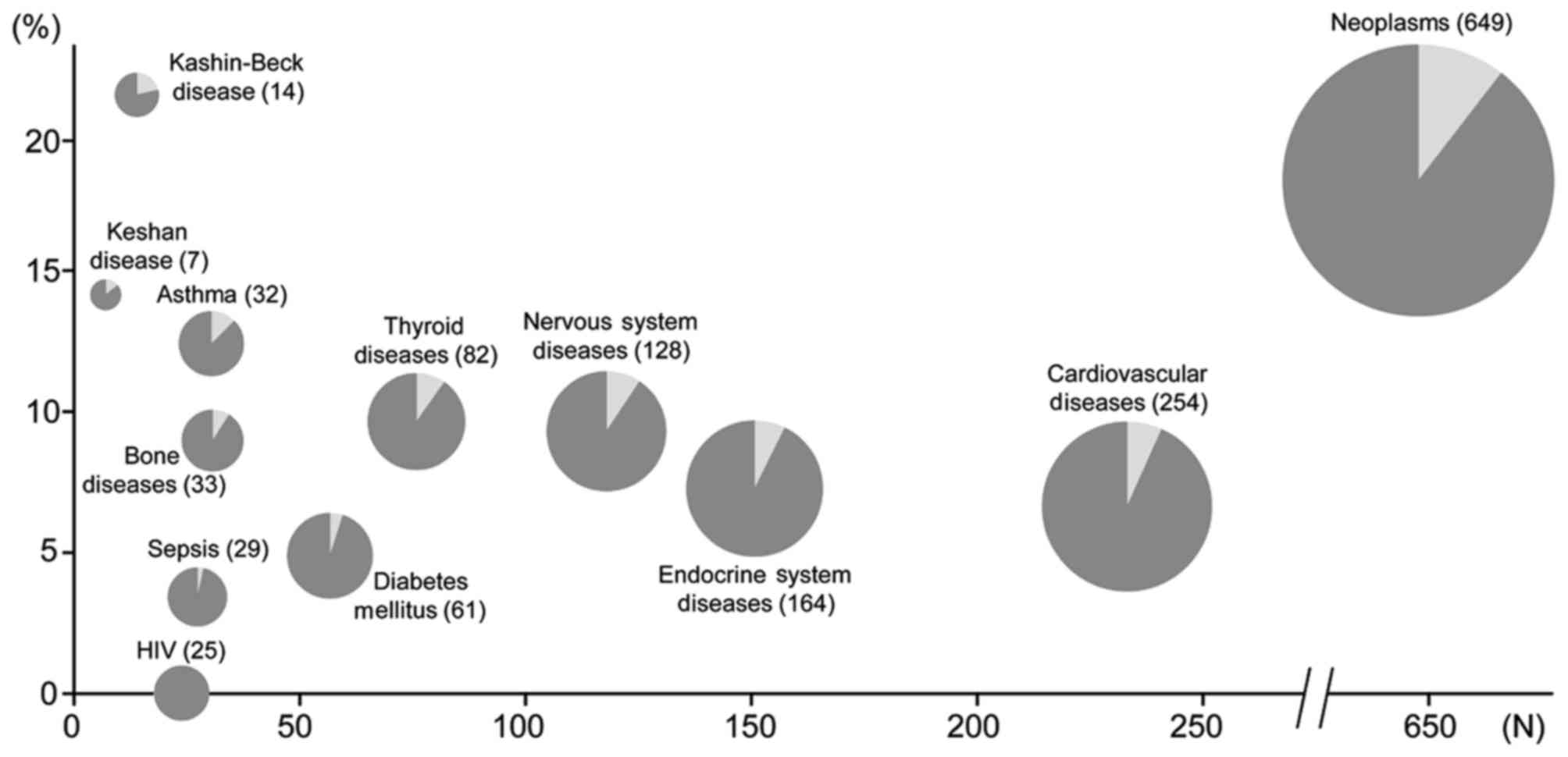
A large number of environmental studies which
investigated the health effects of unusually high or low selenium
areas have been published, as summarized in Table I. These studies have also
substantially contributed to the PubMed-indexed papers on the
epidemiology of selenium and human health in addition to the
previous papers (Fig. 1), adding
relevant data to our understanding of the health effects of
selenium in humans. Some of these studies have been published after
the 2000 Institute of Medicine selenium assessment (4), considerably extending the limited
evidence previously available on the basis of a few ‘old’ Chinese
studies. This literature includes the investigation of health
effects of high-selenium environment in South and North America,
India, China, and Italy. The high content of selenium in these
areas, in most cases of geological origin, has induced unusually
high levels of selenium in locally grown foodstuffs and
occasionally in outdoor air and in drinking water, thus increasing
human exposure to the element. However, systematic investigations
of the health effects of such exposures are unfortunately limited,
and in most cases they came from cross-sectional studies, and very
rarely from studies with a more adequate design, such as
case-control and particularly cohort studies. In addition, the
observational design of these studies induces in most cases a major
concern, the potential bias arising from unmeasured (dietary and
life-style) confounding, in addition to the potential issue of
exposure misclassification. Moreover, health endpoints were
generally different in these studies, thus not allowing their
systematic analysis (and meta-analysis) in the different
populations. Finally, in several cases the small number of exposed
subjects made it impossible to compute statistically stable
estimates, and this lack of precision hampered the detection of
potential health effects of such abnormally low and high exposures
to environmental selenium.
Overall, these studies have yielded an indication
that the extremely low selenium intake, in the order of <10-15
µg/day, may increase the risk of a severe cardiomyopathy named
‘Keshan disease’ (17–20), while high selenium intake may have
unfavorable effects on the endocrine system and particularly on the
thyroid status (21), and increase
the risk of type 2 diabetes (3,22,23),
some specific cancers such as melanoma and lymphoid cancers
(24–26), and nervous system disturbances
including alterations in visual evoked potentials (27) and excess risk of amyotrophic
lateral sclerosis (26,28).
Studies in populations with ‘intermediate’ selenium
status. Several studies have investigated the effects on human
health of even limited changes in exposure to environmental
selenium, which occurs through different environmental sources
(primarily diet, but also air pollution, occupational environment,
smoking and drinking water), in populations characterized by
exposure levels not considered a priori to be unusually
‘low’ or ‘high’ (14). These
studies, generally carried out in Western populations, have
investigated a broad number of health outcomes, but in the majority
of cases they focused on cancer risk (14,15).
However, most of these studies had an observational design, thus
suffering from the potential severe bias due to unmeasured
confounding and exposure misclassification even in prospective
cohort studies, in addition to the other biases typically effecting
studies with case-control, cross-sectional and clearly ecologic
design (1,14,29).
In addition, their results have frequently been conflicting even
for the same cancer type, as shown for instance for liver cancer
(30,31), lung cancer (32–34)
or breast cancer (35–38), though in most cases they supported
the occurrence of an inverse relation between selenium status and
cancer risk (1). Luckily and
rather unexpectedly for a nutrient with also was known to exert a
powerful toxicity, the nutritional interest in this metalloid as
well as the extremely ‘attractive’ preliminary results of the first
selenium trial carried out in Western countries, the Nutrition
Prevention of Cancer (NPC) trial (39), a large number of randomized
controlled trials have been conducted during the last two decades.
The aim of these studies has been to investigate the effects on
cancer risk of an increased intake of this element (1,40).
Overall, all the recent trials have consistently
shown that selenium does not modify risk of overall cancer,
prostate cancer and other specific cancers (2,3,23,43–45),
while it may even increase risk of cancers such as advanced
(46,47) or overall prostate cancer (48), non-melanoma skin cancer (49,50)
and possibly breast cancer in high-risk women (51). These results strongly and
unexpectedly differ from the results reported in the earliest
trial, the NPC (49,52), which however was small and more
importantly was later found to be affected by a detection bias
(53). As previously mentioned,
these trials have also been of fundamental (and unforeseen)
importance in identifying the early signs, symptoms and diseases
associated with chronic or subchronic selenium toxicity. In fact,
they have shown that already at amount of selenium exposure
(baseline dietary intake plus supplementation) of around 250–300
µg/day there is an increased risk of type-2 diabetes. Such excess
diabetes risk linked to selenium overexposure was first discovered
in trial carried out in a population with a ‘low’ baseline selenium
status (15,22) and later confirmed in large trials
(3,23). Finally, the largest of the selenium
RCTs, SELECT (23), whose overall
selenium intake in the supplemented group averaged 300 µg/day
(15), has shown that such amount
of exposure induces ‘minor’ adverse effects such as dermatitis and
alopecia [a long-recognized sign of selenium toxicity (12)]. These effects indicate that the
selenium lower-observed-adverse-effect-level (LOAEL) is much lower
than previously considered by regulatory agencies (5,54),
which could base their assessment on the scarce data yielded by a
few old Chinese environmental studies (55), calling for an update of the risk
assessment of this element (5,15,56,57).
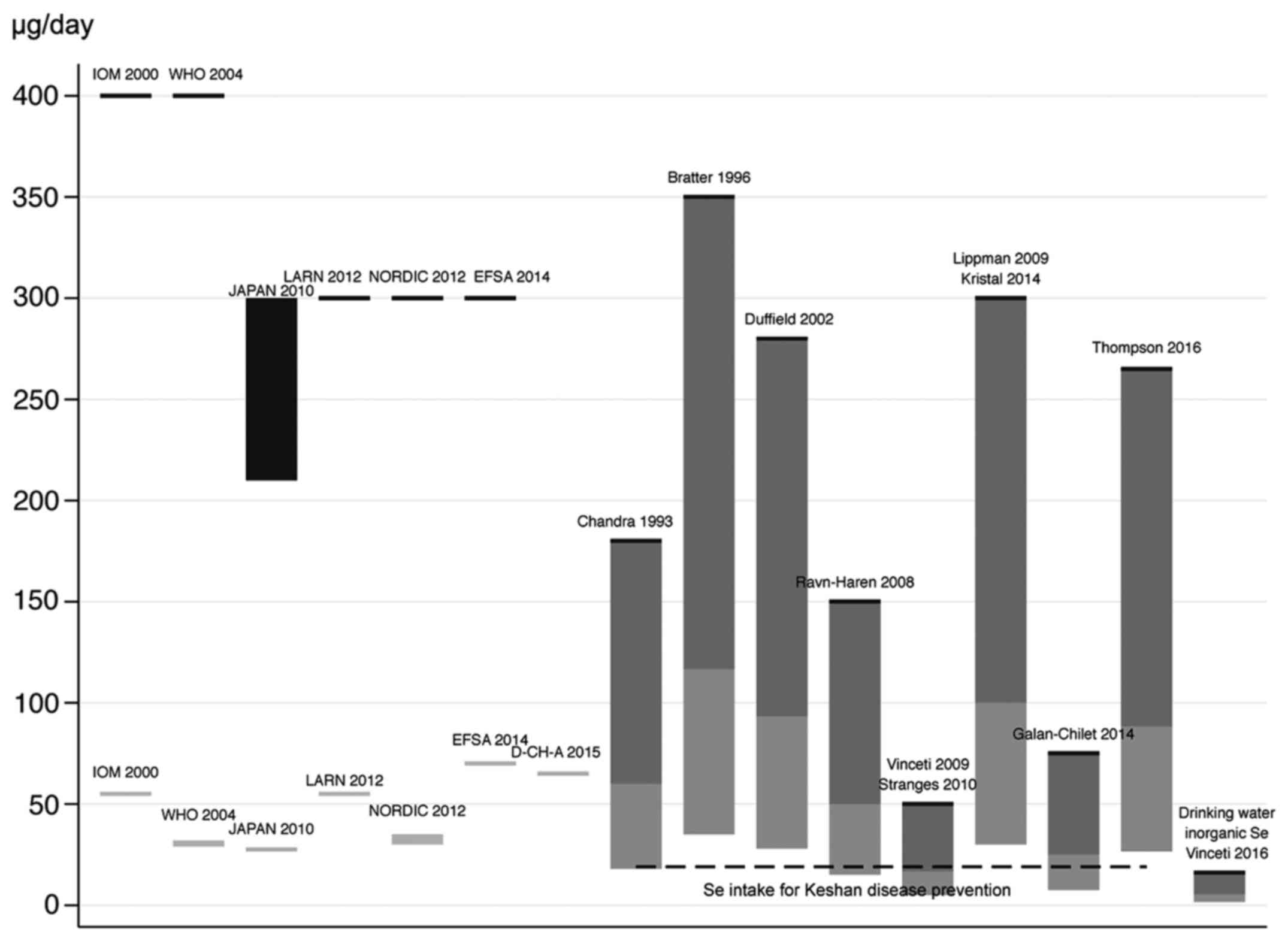
An issue therefore arises about the adequacy of
current standards for environmental risk assessment of selenium in
the human, for both abnormally low and high exposures. These
standards have been defined by a number of agencies since 2000 to
2014, and as summarized in Fig. 2
they encompass minimal recommended values ranging from 30 to 70
µg/day, and upper doses ranging from 300 to 400 µg/day (in adults)
for overall selenium exposure (4,16,58–61).
On the contrary, specific guidelines for single selenium species
have not been unfortunately set, despite the clear evidence that
the various chemical forms of selenium have different biological
properties, i.e. nutritional and toxicological activities (7,9,10,62).
So far, the adequacy of the selenium standards has
been mainly based on biochemical endpoints (for the lowest
recommended intake) and on the occurrence of adverse health
outcomes (for the upper level), as identified in old studies
carried out in seleniferous areas from China. However, the newly
available data from the clinical trials indicate the need of a
substantial reassessment of the dose of selenium toxicity, though
they unfortunately do not allow to clearly identify a NOAEL and
probably also a reliable LOAEL, since only one supplemental dose
(200 µg/selenium/day) have been used in these trials and
dose-response data are lacking. However, using an uncertainty
factor as little as 3, i.e. lower that the uncertainty factors
usually adopted in risk assessment (10 or more) also in light of
the peculiar nature of this element and its nutritional relevance,
selenium intake should not exceed 90 µg/day taking into account the
signs of toxicity yielded by the NPC trial (an excess diabetes and
skin cancer risk) and by the SELECT trial (an excess incidence of
diabetes, advanced prostate cancer, dermatitis and alopecia)
(1), as shown in Fig. 2. However, this estimate may be
still inadequate to protect human health from chronic selenium
toxicity, and in addition it appears to apply only to organic
selenium, and to selenomethionine in particular [whose toxicity has
bene recently much better elucidated (63–65)].
For inorganic selenium, typically selenate such as
those found in underground and drinking waters, the epidemiologic
evidence points to a much higher toxicity compared with organic
selenium and exactly as expected on the basis of experimental
studies (10), therefore
suggesting much lower acceptable environmental standards (57), tentatively 1 µg/l for drinking
water (5). New standards should
also be considered for occupational exposure to selenium, given the
limited data available and the potential for toxicity of this
source of exposure (12,13,66,67).
Finally, air selenium might represent a so far overlooked risk
factor for chronic diseases, taking into account that its outdoor
air concentrations have been positively associated with
cardiovascular mortality (68) and
with childhood leukemia risk (69), though more evidence is clearly
required to confirm such possible associations mainly due to the
inherent risk of unmeasured confounding in these observational
studies.
The lowest acceptable amount of selenium exposure is
instead much more controversial and uncertain. Two approaches have
been used to define such lowest safe level of exposure: the
proteomic change induced by the trace element, and the avoidance of
adverse health effects. Concerning the latter point (health
issues), still limited and inconclusive evidence is available on
the large number of diseases tentatively ascribed to a deficiency
of environmental selenium (4,70),
such as the chronic degenerative osteoarthropathy with unclear
etiology named ‘Kashin-Beck’ disease (71,72)
and an increased susceptibility to viral infections (73,74).
In addition, the hypothesis of an effect of ‘low’
environmental selenium exposure in increasing cancer risk may now
be ruled out, thanks to the consistent evidence yielded by the
recent large and well-conducted randomized trials, which ruled out
any preventive effect of selenium on cancer risk. On the converse,
evidence exists on the involvement of selenium deficiency on the
etiology of a rare but severe cardiomyopathy named Keshan disease
and endemic in some Chinese areas (17,18,20,75–77),
and this observation has played a key role in the identification of
the minimal amount of selenium which appears to be required in
humans (4,78). Such involvement has been suggested
mainly on the basis of observational evidence, i.e. a lower
selenium status in the populations more affected by this disease,
and following the beneficial effects of a selenium supplementation
trial on disease incidence.
However, some epidemiologic features of the disease
have since the discovery of the disease suggested alternative
etiologic hypotheses (79),
particularly a cardiotropic infectious agent such as a Coxsackie
virus, selenium deficiency possibly being a cofactor in disease
etiology or simply an innocent bystander (19,20,54,77).
Under this perspective, the beneficial effect of selenium
supplementation in a Chinese trial might be interpreted as an
indication of antiviral effects of the selenium compound used
(inorganic tetravalent selenium, i.e. selenite), as suggested by
laboratory studies (40,80). In any case, while still
investigating the cause of Keshan disease and the possible
involvement of selenium status, it is prudent to avoid a too low
intake of selenium under the hypothesis of a role in Keshan disease
etiology, and therefore average population intake must be higher
than that shown to be required to avoid disease incidence, i.e.
13.3 µg/day in females and 19.1 in males (16). Finally, recent evidence has
suggested adverse health effects of mutations affecting Sec
insertion sequence-binding protein 2 or the selenoprotein N1 gene
(81–83), though such abnormalities might not
be strictly related to a ‘selenium deficiency’ neither were they
corrected by its supplementation (84), thus being of limited interest in
the setting of minimal dietary selenium requirements.
Alternatively, to the use of health endpoints, and
considerably more frequently, the amount of the selenium needed to
induce the maximization of selenoprotein synthesis (particularly
glutathione-peroxidase and plasma selenoprotein P) has been
proposed to set the minimal requirement of selenium in the human.
This approach has been based on the assumption that achievement of
this biochemical endpoint, i.e. upregulation (frequently defined as
‘optimization’) of selenoprotein synthesis indicates the
achievement of an adequate supply of this trace element to the
human (40,85). This would point to adequate dietary
intake (considering this as only source of selenium exposure) of
amount in the order of 70 µg/day (85), thus reaching or even exceeding the
upper limit definable on the basis of the SELECT trial results
using an uncertainty factor of 3 and clearly even more, of course,
when using an uncertainty factor of 10 (Fig. 2). In addition, this ‘biochemical’
approach does not take into account that selenoprotein maximization
which follows selenium species administration may derive not just
from the ‘correction’ of a nutritional deficiency of the trace
element, but as a compensatory response of these proteins (all
characterized by antioxidant properties) to the pro-oxidant
activity of selenium species (40,54,86–94).
There is also little evidence showing that
selenoprotein activity, and particularly its maximization, are
beneficial to human health, and therefore (as more generally levels
for antioxidant enzymes) this should not be regarded as an
objective unless more evidence in humans are provided (40,54).
This approach is further strengthened when taking into account that
these enzymes are physiologically induced and inducible by
oxidative stress (for selenoproteins, even in the absence of any
change in selenium supply) (40,54),
as long recognized since the discovery of the selenium-containing
antioxidant enzyme glutathione-peroxidase (95–97).
Overall, it seems therefore prudent to avoid a maximal expression
of selenoproteins (54,98), setting as standard a lower amount
of their activity, such as proposed by WHO when suggesting a
‘nutritionally adequate’ target (‘recommended nutrient intake’) the
achievement of two thirds of the maximal selenoprotein activity,
corresponding to a daily selenium intake of 25–34 µg in adults
(Fig. 2). However, more research
is clearly required to set reliable lower and upper safe selenium
levels, though the current standards need to be quickly updated
with reference to the upper levels taking into account the
above-mentioned recent results of the epidemiologic studies, i.e.
the high-quality RCTs and the environmental studies, and also
considering the opportunity to set species-specific standards for
this element.
|
1
|
Vinceti M, Dennert G, Crespi CM, Zwahlen
M, Brinkman M, Zeegers MP, Horneber M, D'Amico R and Del Giovane C:
Selenium for preventing cancer. Cochrane Database Syst Rev.
3:CD0051952014.
|
|
2
|
Lance P, Alberts DS, Thompson PA, Fales L,
Wang F, Jose San J, Jacobs ET, Goodman PJ, Darke AK, Yee M, et al:
Colorectal adenomas in participants of the SELECT randomized trial
of selenium and vitamin E for prostate cancer prevention. Cancer
Prev Res (Phila). 10:45–54. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Thompson PA, Ashbeck EL, Roe DJ, Fales L,
Buckmeier J, Wang F, Bhattacharyya A, Hsu CH, Chow HH, Ahnen DJ, et
al: Selenium supplementation for prevention of colorectal adenomas
and risk of associated type 2 diabetes. J Natl Cancer Inst.
108:pii: djw152. 2016. View Article : Google Scholar
|
|
4
|
Institute of Medicine Food and Nutrition
Board: Dietary references intakes for vitamin C, vitamin E,
selenium, and carotenoids. National Academy Press; Washington, DC:
2000
|
|
5
|
Vinceti M, Crespi CM, Bonvicini F,
Malagoli C, Ferrante M, Marmiroli S and Stranges S: The need for a
reassessment of the safe upper limit of selenium in drinking water.
Sci Total Environ. 443:633–642. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rothman KJ, Greenland S and Lash TL:
Modern Epidemiology. Lippincott Williams & Wilkins;
Philadelphia: 2012, View Article : Google Scholar
|
|
7
|
Michalke B, Halbach S and Nischwitz V: JEM
spotlight: Metal speciation related to neurotoxicity in humans. J
Environ Monit. 11:939–954. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gammelgaard B, Jackson MI and Gabel-Jensen
C: Surveying selenium speciation from soil to cell--forms and
transformations. Anal Bioanal Chem. 399:1743–1763. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Weekley CM and Harris HH: Which form is
that? The importance of selenium speciation and metabolism in the
prevention and treatment of disease. Chem Soc Rev. 42:8870–8894.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vinceti M, Solovyev N, Mandrioli J, Crespi
CM, Bonvicini F, Arcolin E, Georgoulopoulou E and Michalke B:
Cerebrospinal fluid of newly diagnosed amyotrophic lateral
sclerosis patients exhibits abnormal levels of selenium species
including elevated selenite. Neurotoxicology. 38:25–32. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vinceti M, Grill P, Malagoli C, Filippini
T, Storani S, Malavolti M and Michalke B: Selenium speciation in
human serum and its implications for epidemiologic research: A
cross-sectional study. J Trace Elem Med Biol. 31:1–10. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vinceti M, Wei ET, Malagoli C, Bergomi M
and Vivoli G: Adverse health effects of selenium in humans. Rev
Environ Health. 16:233–251. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vinceti M, Mandrioli J, Borella P,
Michalke B, Tsatsakis A and Finkelstein Y: Selenium neurotoxicity
in humans: Bridging laboratory and epidemiologic studies. Toxicol
Lett. 230:295–303. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vinceti M, Crespi CM, Malagoli C, Del
Giovane C and Krogh V: Friend or foe? The current epidemiologic
evidence on selenium and human cancer risk. J Environ Sci Health C
Environ Carcinog Ecotoxicol Rev. 31:305–341. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vinceti M, Burlingame B, Fillippini T,
Naska A, Bargellini A and Borella P: The epidemiology of selenium
and human healthSelenium: Its Molecular Biology and Role in Human
Health. Hatfield D, Schweizer U and Gladyshev VN: 4th. Springer
Science Business Media; New York: pp. 365–376. 2016, View Article : Google Scholar
|
|
16
|
Joint FAO/WHO Expert Consultation on Human
Vitamin and Mineral Requirements: Vitamin and mineral requirements
in human nutrition. 2nd. World Health Organization and Food and
Agriculture Organization of the United Nations; Geneva: 2004
|
|
17
|
Keshan Disease Research Group of the
Chinese Academy of Medical Sciences: Epidemiologic studies on the
etiologic relationship of selenium and Keshan disease. Chin Med J
(Engl). 92:477–482. 1979.PubMed/NCBI
|
|
18
|
Keshan Disease Research Group of the
Chinese Academy of Medical Sciences: Observations on effect of
sodium selenite in prevention of Keshan disease. Chin Med J (Engl).
92:471–476. 1979.PubMed/NCBI
|
|
19
|
Wang T and Li Q: Interpretation of
selenium deficiency and Keshan disease with causal inference of
modern epidemiologyThe 5th International Selenium Seminar.
Organizing Committee of the International Selenium Seminar; Moscow:
pp. 34–35. 2015
|
|
20
|
Lei C, Niu X, Ma X and Wei J: Is selenium
deficiency really the cause of Keshan disease? Environ Geochem
Health. 33:183–188. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Winther KH, Bonnema SJ, Cold F, Debrabant
B, Nybo M, Cold S and Hegedüs L: Does selenium supplementation
affect thyroid function? Results from a randomized, controlled,
double-blinded trial in a Danish population. Eur J Endocrinol.
172:657–667. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Stranges S, Marshall JR, Natarajan R,
Donahue RP, Trevisan M, Combs GF, Cappuccio FP, Ceriello A and Reid
ME: Effects of long-term selenium supplementation on the incidence
of type 2 diabetes: A randomized trial. Ann Intern Med.
147:217–223. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lippman SM, Klein EA, Goodman PJ, Lucia
MS, Thompson IM, Ford LG, Parnes HL, Minasian LM, Gaziano JM,
Hartline JA, et al: Effect of selenium and vitamin E on risk of
prostate cancer and other cancers: The Selenium and Vitamin E
Cancer Prevention Trial (SELECT). JAMA. 301:39–51. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vinceti M, Rovesti S, Gabrielli C,
Marchesi C, Bergomi M, Martini M and Vivoli G: Cancer mortality in
a residential cohort exposed to environmental selenium through
drinking water. J Clin Epidemiol. 48:1091–1097. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Vinceti M, Rothman KJ, Bergomi M, Borciani
N, Serra L and Vivoli G: Excess melanoma incidence in a cohort
exposed to high levels of environmental selenium. Cancer Epidemiol
Biomarkers Prev. 7:853–856. 1998.PubMed/NCBI
|
|
26
|
Vinceti M, Ballotari P, Steinmaus C,
Malagoli C, Luberto F, Malavolti M and Rossi Giorgi P: Long-term
mortality patterns in a residential cohort exposed to inorganic
selenium in drinking water. Environ Res. 150:348–356. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Saint-Amour D, Roy MS, Bastien C, Ayotte
P, Dewailly E, Després C, Gingras S and Muckle G: Alterations of
visual evoked potentials in preschool Inuit children exposed to
methylmercury and polychlorinated biphenyls from a marine diet.
Neurotoxicology. 27:567–578. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vinceti M, Bonvicini F, Rothman KJ,
Vescovi L and Wang F: The relation between amyotrophic lateral
sclerosis and inorganic selenium in drinking water: A
population-based case-control study. Environ Health. 9:772010.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Vinceti M and Rothman KJ: More results but
no clear conclusion on selenium and cancer. Am J Clin Nutr.
104:245–246. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hughes DJ, Duarte-Salles T, Hybsier S,
Trichopoulou A, Stepien M, Aleksandrova K, Overvad K, Tjønneland A,
Olsen A, Affret A, et al: Prediagnostic selenium status and
hepatobiliary cancer risk in the European Prospective Investigation
into Cancer and Nutrition cohort. Am J Clin Nutr. 104:406–414.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ma X, Yang Y, Li HL, Zheng W, Gao J, Zhang
W, Yang G, Shu XO and Xiang YB: Dietary trace element intake and
liver cancer risk: Results from two population-based cohorts in
China. Int J Cancer. 140:1050–1059. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Knekt P, Marniemi J, Teppo L, Heliövaara M
and Aromaa A: Is low selenium status a risk factor for lung cancer?
Am J Epidemiol. 148:975–982. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
van den Brandt PA, Goldbohm RA, van't Veer
P, Bode P, Dorant E, Hermus RJ and Sturmans F: A prospective cohort
study on selenium status and the risk of lung cancer. Cancer Res.
53:4860–4865. 1993.PubMed/NCBI
|
|
34
|
Suadicani P, Hein HO and Gyntelberg F:
Serum selenium level and risk of lung cancer mortality: A 16-year
follow-up of the Copenhagen Male Study. Eur Respir J. 39:1443–1448.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Menkes MS, Comstock GW, Vuilleumier JP,
Helsing KJ, Rider AA and Brookmeyer R: Serum beta-carotene,
vitamins A and E, selenium, and the risk of lung cancer. N Engl J
Med. 315:1250–1254. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
van Noord PA, Maas MJ, van der Tweel I and
Collette C: Selenium and the risk of postmenopausal breast cancer
in the DOM cohort. Breast Cancer Res Treat. 25:11–19. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
van den Brandt PA, Goldbohm RA, van't Veer
P, Bode P, Dorant E, Hermus RJ and Sturmans F: Toenail selenium
levels and the risk of breast cancer. Am J Epidemiol. 140:20–26.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Garland M, Morris JS, Stampfer MJ, Colditz
GA, Spate VL, Baskett CK, Rosner B, Speizer FE, Willett WC and
Hunter DJ: Prospective study of toenail selenium levels and cancer
among women. J Natl Cancer Inst. 87:497–505. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Clark LC, Combs GFJ Jr, Turnbull BW, Slate
EH, Chalker DK, Chow J, Davis LS, Glover RA, Graham GF, Gross EG,
et al: Nutritional Prevention of Cancer Study Group: Effects of
selenium supplementation for cancer prevention in patients with
carcinoma of the skin. A randomized controlled trial. JAMA.
276:1957–1963. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jablonska E and Vinceti M: Selenium and
Human Health: Witnessing a Copernican Revolution? J Environ Sci
Health C Environ Carcinog Ecotoxicol Rev. 33:328–368. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Higgins JP: A revised tool to assess risk
of bias in randomized trials. (RoB 2.0). 2016.
|
|
42
|
Rees K, Hartley L, Day C, Flowers N,
Clarke A and Stranges S: Selenium supplementation for the primary
prevention of cardiovascular disease. Cochrane Database Syst Rev.
1:CD0096712013.
|
|
43
|
Stratton MS, Reid ME, Schwartzberg G,
Minter FE, Monroe BK, Alberts DS, Marshall JR and Ahmann FR:
Selenium and prevention of prostate cancer in high-risk men: The
Negative Biopsy Study. Anticancer Drugs. 14:589–594. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Algotar AM, Stratton MS, Ahmann FR,
Ranger-Moore J, Nagle RB, Thompson PA, Slate E, Hsu CH, Dalkin BL,
Sindhwani P, et al: Phase 3 clinical trial investigating the effect
of selenium supplementation in men at high-risk for prostate
cancer. Prostate. 73:328–335. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Karp DD, Lee SJ, Keller SM, Wright GS,
Aisner S, Belinsky SA, Johnson DH, Johnston MR, Goodman G, Clamon
G, et al: Randomized, double-blind, placebo-controlled, phase III
chemoprevention trial of selenium supplementation in patients with
resected stage I non-small-cell lung cancer: ECOG 5597. J Clin
Oncol. 31:4179–4187. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kristal AR, Darke AK, Morris JS, Tangen
CM, Goodman PJ, Thompson IM, Meyskens FL Jr, Goodman GE, Minasian
LM, Parnes HL, et al: Baseline selenium status and effects of
selenium and vitamin e supplementation on prostate cancer risk. J
Natl Cancer Inst. 106:djt4562014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Albanes D, Till C, Klein EA, Goodman PJ,
Mondul AM, Weinstein SJ, Taylor PR, Parnes HL, Gaziano JM, Song X,
et al: Plasma tocopherols and risk of prostate cancer in the
Selenium and Vitamin E Cancer Prevention Trial (SELECT). Cancer
Prev Res (Phila). 7:886–895. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Martinez EE, Darke AK, Tangen CM, Goodman
PJ, Fowke JH, Klein EA and Abdulkadir SA: A functional variant in
NKX3.1 associated with prostate cancer risk in the Selenium and
Vitamin E Cancer Prevention Trial (SELECT). Cancer Prev Res
(Phila). 7:950–957. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Duffield-Lillico AJ, Slate EH, Reid ME,
Turnbull BW, Wilkins PA, Combs GF Jr, Park HK, Gross EG, Graham GF,
Stratton MS, et al: Nutritional Prevention of Cancer Study Group:
Selenium supplementation and secondary prevention of nonmelanoma
skin cancer in a randomized trial. J Natl Cancer Inst.
95:1477–1481. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Dréno B, Euvrard S, Frances C, Moyse D and
Nandeuil A: Effect of selenium intake on the prevention of
cutaneous epithelial lesions in organ transplant recipients. Eur J
Dermatol. 17:140–145. 2007.PubMed/NCBI
|
|
51
|
Lubinski J, Jaworska K, Durda K,
Jakubowska A, Huzarski T, Byrski T, Stawicka M, Gronwald J, Górski
B, Wasowicz W, et al: Selenium and the risk of cancer in BRCA1
carriers. Hered Cancer Clin Pract. 9:(Suppl 2). A52011. View Article : Google Scholar :
|
|
52
|
Duffield-Lillico AJ, Reid ME, Turnbull BW,
Combs GFJ Jr, Slate EH, Fischbach LA, Marshall JR and Clark LC:
Baseline characteristics and the effect of selenium supplementation
on cancer incidence in a randomized clinical trial: A summary
report of the Nutritional Prevention of Cancer Trial. Cancer
Epidemiol Biomarkers Prev. 11:630–639. 2002.PubMed/NCBI
|
|
53
|
Duffield-Lillico AJ, Dalkin BL, Reid ME,
Turnbull BW, Slate EH, Jacobs ET, Marshall JR and Clark LC:
Nutritional Prevention of Cancer Study Group: Selenium
supplementation, baseline plasma selenium status and incidence of
prostate cancer: An analysis of the complete treatment period of
the Nutritional Prevention of Cancer Trial. BJU Int. 91:608–612.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Vinceti M, Maraldi T, Bergomi M and
Malagoli C: Risk of chronic low-dose selenium overexposure in
humans: Insights from epidemiology and biochemistry. Rev Environ
Health. 24:231–248. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yang GQ, Wang SZ, Zhou RH and Sun SZ:
Endemic selenium intoxication of humans in China. Am J Clin Nutr.
37:872–881. 1983.PubMed/NCBI
|
|
56
|
Barron E, Migeot V, Rabouan S,
Potin-Gautier M, Séby F, Hartemann P, Lévi Y and Legube B: The case
for re-evaluating the upper limit value for selenium in drinking
water in Europe. J Water Health. 7:630–641. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Frisbie SH, Mitchell EJ and Sarkar B:
Urgent need to reevaluate the latest World Health Organization
guidelines for toxic inorganic substances in drinking water.
Environ Health. 14:632015. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Scientific Committee on Food: Opinion of
the Scientific Committee on Food on the Tolerable Upper Intake
Level of SeleniumEuropean Commission. Brussels: 2000, https://ec.europa.eu/food/sites/food/files/safety/docs/sci-com_scf_out80g_en.pdf
|
|
59
|
Tsubota-Utsugi M, Imai E, Nakade M,
Tsuboyama-Kasaoka N, Morita A and Tokudome S: Dietary Reference
Intakes for Japanese - 2010. The summary report from the Scientific
Committee of ‘Dietary Reference intakes for Japanese’National
Institute of Health and Nutrition. Japan: 2012
|
|
60
|
Nordic Nutrition Recommendations 2012.
5th. Nordic Council of Ministers; Copenhagen: 2014, doi:
org/10.6027/Nord2014-002.
|
|
61
|
Società Italiana di Nutrizione Umana: LARN
- Livelli di assunzione di riferimento di nutrienti e energia per
la popolazione italiana - IV revisioneSICS. Milan: 2014, (In
Italian).
|
|
62
|
Marschall TA, Bornhorst J, Kuehnelt D and
Schwerdtle T: Differing cytotoxicity and bioavailability of
selenite, methylselenocysteine, selenomethionine, selenosugar 1 and
trimethylselenonium ion and their underlying metabolic
transformations in human cells. Mol Nutr Food Res. 60:2622–2632.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Lazard M, Dauplais M, Blanquet S and
Plateau P: Trans-sulfuration pathway seleno-amino acids are
mediators of selenomethionine toxicity in Saccharomyces cerevisiae.
J Biol Chem. 290:10741–10750. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Raine JC, Lallemand L, Pettem CM and Janz
DM: Effects of chronic dietary selenomethionine exposure on the
visual system of adult and F1 generation zebrafish (Danio rerio).
Bull Environ Contam Toxicol. 97:331–336. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Dolgova NV, Hackett MJ, MacDonald TC,
Nehzati S, James AK, Krone PH, George GN and Pickering IJ:
Distribution of selenium in zebrafish larvae after exposure to
organic and inorganic selenium forms. Metallomics. 8:305–312. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Göen T, Schaller B, Jäger T, Bräu-Dümler
Ch, Schaller KH and Drexler H: Biological monitoring of exposure
and effects in workers employed in a selenium-processing plant. Int
Arch Occup Environ Health. 88:623–630. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Jäger T, Drexler H and Göen T: Human
metabolism and renal excretion of selenium compounds after oral
ingestion of sodium selenate dependent on trimethylselenium ion
(TMSe) status. Arch Toxicol. 90:149–158. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Ito K, Mathes R, Ross Z, Nádas A, Thurston
G and Matte T: Fine particulate matter constituents associated with
cardiovascular hospitalizations and mortality in New York City.
Environ Health Perspect. 119:467–473. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Heck JE, Park AS, Qiu J, Cockburn M and
Ritz B: Risk of leukemia in relation to exposure to ambient air
toxics in pregnancy and early childhood. Int J Hyg Environ Health.
217:662–668. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Burk RF Jr: Selenium deficiency in search
of a disease. Hepatology. 8:421–423. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Yu FF, Liu H and Guo X: Integrative
multivariate logistic regression analysis of risk factors for
Kashin-Beck disease. Biol Trace Elem Res. 174:274–279. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yu FF, Zhang YX, Zhang LH, Li WR, Guo X
and Lammi MJ: Identified molecular mechanism of interaction between
environmental risk factors and differential expression genes in
cartilage of Kashin-Beck disease. Medicine (Baltimore).
95:e56692016. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Beck MA, Levander OA and Handy J: Selenium
deficiency and viral infection. J Nutr. 133:(Suppl 1). 1463S–1467S.
2003.PubMed/NCBI
|
|
74
|
Sheridan PA, Zhong N, Carlson BA, Perella
CM, Hatfield DL and Beck MA: Decreased selenoprotein expression
alters the immune response during influenza virus infection in
mice. J Nutr. 137:1466–1471. 2007.PubMed/NCBI
|
|
75
|
Gu BQ: Pathology of Keshan disease. A
comprehensive review. Chin Med J (Engl). 96:251–261.
1983.PubMed/NCBI
|
|
76
|
Levander OA and Beck MA: Interacting
nutritional and infectious etiologies of Keshan disease. Insights
from coxsackie virus B-induced myocarditis in mice deficient in
selenium or vitamin E. Biol Trace Elem Res. 56:5–21. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Xu GL, Wang SC, Gu BQ, Yang YX, Song HB,
Xue WL, Liang WS and Zhang PY: Further investigation on the role of
selenium deficiency in the aetiology and pathogenesis of Keshan
disease. Biomed Environ Sci. 10:316–326. 1997.PubMed/NCBI
|
|
78
|
Chen J: An original discovery: Selenium
deficiency and Keshan disease (an endemic heart disease). Asia Pac
J Clin Nutr. 21:320–326. 2012.PubMed/NCBI
|
|
79
|
Guanqing H: On the etiology of Keshan
disease: Two hypotheses. Chin Med J (Engl). 92:416–422.
1979.PubMed/NCBI
|
|
80
|
Cermelli C, Vinceti M, Scaltriti E,
Bazzani E, Beretti F, Vivoli G and Portolani M: Selenite inhibition
of Coxsackie virus B5 replication: Implications on the etiology of
Keshan disease. J Trace Elem Med Biol. 16:41–46. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Schoenmakers E, Agostini M, Mitchell C,
Schoenmakers N, Papp L, Rajanayagam O, Padidela R, Ceron-Gutierrez
L, Doffinger R, Prevosto C, et al: Mutations in the selenocysteine
insertion sequence-binding protein 2 gene lead to a multisystem
selenoprotein deficiency disorder in humans. J Clin Invest.
120:4220–4235. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Scoto M, Cirak S, Mein R, Feng L, Manzur
AY, Robb S, Childs AM, Quinlivan RM, Roper H, Jones DH, et al:
SEPN1-related myopathies: Clinical course in a large cohort of
patients. Neurology. 76:2073–2078. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Ardissone A, Bragato C, Blasevich F,
Maccagnano E, Salerno F, Gandioli C, Morandi L, Mora M and Moroni
I: SEPN1-related myopathy in three patients: Novel mutations and
diagnostic clues. Eur J Pediatr. 175:1113–1118. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Schomburg L, Dumitrescu AM, Liao XH,
Bin-Abbas B, Hoeflich J, Köhrle J and Refetoff S: Selenium
supplementation fails to correct the selenoprotein synthesis defect
in subjects with SBP2 gene mutations. Thyroid. 19:277–281. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
EFSA NDA Panel: Scientific opinion on
dietary reference values for selenium. EFSA J. 12:38462014.
View Article : Google Scholar
|
|
86
|
Ge KY, Wang SQ, Bai J, Xue AN, Deng XJ, Su
CQ and Wu SQ: The protective effect of selenium against viral
myocarditis in miceSelenium in biology and medicine. Part B, Combs
GF, Spallholz JE, Levander OA and Oldfield JE: Avi Book, Van
Nostrand Reinhold Co.; New York: pp. 761–768. 1987
|
|
87
|
Spallholz JE: Free radical generation by
selenium compounds and their prooxidant toxicity. Biomed Environ
Sci. 10:260–270. 1997.PubMed/NCBI
|
|
88
|
Stewart MS, Spallholz JE, Neldner KH and
Pence BC: Selenium compounds have disparate abilities to impose
oxidative stress and induce apoptosis. Free Radic Biol Med.
26:42–48. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Letavayová L, Vlasáková D, Spallholz JE,
Brozmanová J and Chovanec M: Toxicity and mutagenicity of selenium
compounds in Saccharomyces cerevisiae. Mutat Res. 638:1–10. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Misra S, Boylan M, Selvam A, Spallholz JE
and Björnstedt M: Redox-active selenium compounds - from toxicity
and cell death to cancer treatment. Nutrients. 7:3536–3556. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Lee KH and Jeong D: Bimodal actions of
selenium essential for antioxidant and toxic pro-oxidant
activities: The selenium paradox (Review). Mol Med Rep. 5:299–304.
2012.PubMed/NCBI
|
|
92
|
Brozmanová J, Mániková D, Vlčková V and
Chovanec M: Selenium: A double-edged sword for defense and offence
in cancer. Arch Toxicol. 84:919–938. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Schiar VP, Dos Santos DB, Paixão MW,
Nogueira CW, Rocha JB and Zeni G: Human erythrocyte hemolysis
induced by selenium and tellurium compounds increased by GSH or
glucose: A possible involvement of reactive oxygen species. Chem
Biol Interact. 177:28–33. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Guo CH, Hsia S, Hsiung DY and Chen PC:
Supplementation with selenium yeast on the prooxidant-antioxidant
activities and anti-tumor effects in breast tumor xenograft-bearing
mice. J Nutr Biochem. 26:1568–1579. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Hafeman DG, Sunde RA and Hoekstra WG:
Effect of dietary selenium on erythrocyte and liver glutathione
peroxidase in the rat. J Nutr. 104:580–587. 1974.PubMed/NCBI
|
|
96
|
Oh SH, Sunde RA, Pope AL and Hoekstra WG:
Glutathione peroxidase response to selenium intake in lambs fed a
Torula yeast-based, artificial milk. J Anim Sci. 42:977–983. 1976.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Kramer GF and Ames BN: Mechanisms of
mutagenicity and toxicity of sodium selenite
(Na2SeO3) in Salmonella typhimurium. Mutat
Res. 201:169–180. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Macallan DC and Sedgwick P: Selenium
supplementation and selenoenzyme activity. Clin Sci (Lond).
99:579–581. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Tsongas TA and Ferguson SW: Selenium
concentrations in human urine and drinking waterProceedings of
‘Trace Elements in Man and Animal-3’. Kirchgessner N: Institute for
Nursing Physiology Technical University Munchen; Freising: pp.
320–321. 1978
|
|
100
|
Tsongas TA and Ferguson SW: Human health
effects of selenium in a rural Colorado drinking water supply. In:
Proceedings of ‘Trace substances in environmental health-XIA
symposium’. Hemphill DD: University of Missouri; Columbia: pp.
30–35. 1977
|
|
101
|
Valentine JL: Environmental occurrence of
selenium in waters and related health significance. Biomed Environ
Sci. 10:292–299. 1997.PubMed/NCBI
|
|
102
|
Valentine JL, Kang HK, Dang PM and
Schluchter M: Selenium concentrations and glutathione peroxidase
activities in a population exposed to selenium via drinking water.
J Toxicol Environ Health. 6:731–736. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Valentine JL, Faraji B and Kang HK: Human
glutathione peroxidase activity in cases of high selenium
exposures. Environ Res. 45:16–27. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Valentine JL, Reisbord LS, Kang HK and
Schluchter M: Effects on human health of exposure to selenium in
drinking waterProceedings of ‘Selenium in Biology and Medicine -
Part B’. Combs GF, Levander OA, Spallholz JE and Oldfield JE: Van
Nostrand Reihold Co.; New York: pp. 675–687. 1987
|
|
105
|
Longnecker MP, Taylor PR, Levander OA,
Howe M, Veillon C, McAdam PA, Patterson KY, Holden JM, Stampfer MJ,
Morris JS, et al: Selenium in diet, blood, and toenails in relation
to human health in a seleniferous area. Am J Clin Nutr.
53:1288–1294. 1991.PubMed/NCBI
|
|
106
|
Brätter P and de Negretti Brätter VE:
Influence of high dietary selenium intake on the thyroid hormone
level in human serum. J Trace Elem Med Biol. 10:163–166. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Fordyce FM, Zhan G, Green K and Liu X:
Soil, grain and water chemistry in relation to human
selenium-responsive diseases in Enshi District, China. Applied
Geochemistry. 15:117–132. 2000.doi: 10.1016/S0883-2927(99)00035-9.
View Article : Google Scholar
|
|
108
|
Zhu J, Wang N, Li S, Li L, Su H and Liu C:
Distribution and transport of selenium in Yutangba, China: Impact
of human activities. Sci Total Environ. 392:252–261. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Hira CK, Partal K and Dhillon KS: Dietary
selenium intake by men and women in high and low selenium areas of
Punjab. Public Health Nutr. 7:39–43. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Lemire M, Fillion M, Frenette B, Passos
CJ, Guimarães JR, Barbosa F Jr and Mergler D: Selenium from dietary
sources and motor functions in the Brazilian Amazon.
Neurotoxicology. 32:944–953. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Lemire M, Philibert A, Fillion M, Passos
CJ, Guimarães JR, Barbosa F Jr and Mergler D: No evidence of
selenosis from a selenium-rich diet in the Brazilian Amazon.
Environ Int. 40:128–136. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Qin HB, Zhu JM, Liang L, Wang MS and Su H:
The bioavailability of selenium and risk assessment for human
selenium poisoning in high-Se areas, China. Environ Int. 52:66–74.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Martens IB, Cardoso BR, Hare DJ,
Niedzwiecki MM, Lajolo FM, Martens A and Cozzolino SM: Selenium
status in preschool children receiving a Brazil nut-enriched diet.
Nutrition. 31:1339–1343. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Chawla R, Loomba R, Chaudhary RJ, Singh S
and Dhillon KS: Impact of high selenium exposure on organ function
and biochemical profile of the rural population living in
seleniferous soils in Punjab, IndiaGlobal advance in selenium
research from theory to application. CRC Press; Sao Paulo: pp.
93–94. 2015, View Article : Google Scholar
|
|
115
|
Yu SY, Zhu YJ and Li WG: Protective role
of selenium against hepatitis B virus and primary liver cancer in
Qidong. Biol Trace Elem Res. 56:117–124. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Yu SY, Zhu YJ, Li WG, Huang QS, Huang CZ,
Zhang QN and Hou C: A preliminary report on the intervention trials
of primary liver cancer in high-risk populations with nutritional
supplementation of selenium in China. Biol Trace Elem Res.
29:289–294. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Li WG: Preliminary observations on effect
of selenium yeast on high risk populations with primary liver
cancer. Zhonghua Yu Fang Yi Xue Za Zhi. 26:268–271. 1992.(In
Chinese). PubMed/NCBI
|
|
118
|
Li W, Zhu Y, Yan X, Zhang Q, Li X, Ni Z,
Shen Z, Yao H and Zhu J: The prevention of primary liver cancer by
selenium in high risk populations. Zhonghua Yu Fang Yi Xue Za Zhi.
34:336–338. 2000.(In Chinese). PubMed/NCBI
|
|
119
|
Lotan Y, Goodman PJ, Youssef RF, Svatek
RS, Shariat SF, Tangen CM, Thompson IM Jr and Klein EA: Evaluation
of vitamin E and selenium supplementation for the prevention of
bladder cancer in SWOG coordinated SELECT. J Urol. 187:2005–2010.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Klein EA, Thompson IM Jr, Tangen CM,
Crowley JJ, Lucia MS, Goodman PJ, Minasian LM, Ford LG, Parnes HL,
Gaziano JM, et al: Vitamin E and the risk of prostate cancer: The
Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA.
306:1549–1556. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Marshall JR, Tangen CM, Sakr WA, Wood DP
Jr, Berry DL, Klein EA, Lippman SM, Parnes HL, Alberts DS, Jarrard
DF, et al: Phase III trial of selenium to prevent prostate cancer
in men with high-grade prostatic intraepithelial neoplasia: SWOG
S9917. Cancer Prev Res (Phila). 4:1761–1769. 2011. View Article : Google Scholar : PubMed/NCBI
|