Introduction
The activation of microglia, the primary immune
cells of the central nervous system (CNS), occurs in almost all
neurological disorders (1).
Activated microglia undergo marked morphological changes and
secrete various proinflammatory and neurotoxic factors, including
interleukin (IL)-1β and tumor necrosis factor (TNF)-α, which
contribute to neurodegeneration (2,3).
Excessive microglial activation is toxic not only to neurons
however also to other glial cells, such as oligodendrocytes (OL).
Differentiation of oligodendrocyte precursor cells (OPCs) into OL
is a crucial step in the formation of myelin in the CNS (4). Reactive microglia are present in
lesions of myelin-associated white matter disorders, such as
periventricular leukomalacia and multiple sclerosis, resulting in
injuries to OPCs and leading to myelin defects via excessive
production of oxidative stress and cytokines (5). Due to the importance of microglial
activation in demyelination, the mechanism by which activated
microglia affect the survival of OPCs was examined in the present
study.
Heat shock protein 60 (HSP60) is a stress chaperone
protein. HSP60 has dual functions in cell apoptosis: Under
physiological conditions, HSP60 protects cells from apoptosis,
whereas under stress conditions, HSP60 translocates to the plasma
membrane, is released extracellularly and becomes toxic by
targeting self-reactive T cells (6). The role of HSP60 in the myocardium
has been previously reported (7–12),
however, the role of HSP60 in the CNS remains to be fully
elucidated. Previous studies have demonstrated that HSP60 is
involved in the neuroprotection properties of Lycium
barbarum polysaccharides (13), naloxone (14) and dextromorphan (15) by activation of Toll like receptor
(TLR) 4 on microglia, for which HSP60 is a ligand (16). Notably, OPCs have been reported to
express functional TLR4 (17,18).
In the present study, the hypothesis that
extracellular HSP60, released by LPS-activated microglia, may bind
to TLR4 on OPCs and induce OPC apoptosis was examined. The results
demonstrated that OPC apoptosis was decreased by treatment with a
TLR4 blocking antibody. These observations indicate that HSP60,
released during microglia activation, may display a paracrine
effect on neighboring OPCs leading to OPC cell death. The present
study is, to the best of our knowledge, the first report of HSP60
exhibiting a toxic effect on OPCs. The current study may provide a
potential target for treatment of myelin-associated
neurodegenerative diseases that are accompanied by microglia
activation.
Materials and methods
Chemicals
LPS was purchased from Sigma-Aldrich (Merck
Millipore, Darmstadt, Germany). Antibodies against GAPDH (cat no.
ab181602; 1:2,000) and nuclear factor κB (NFκB; cat no. ab31481;
1:1,000) were from Abcam (Cambridge, MA, USA). Recombinant human
(rh) HSP60 (cat no. ESP540), anti-HSP60 antibody (cat no.
API-SPA-901; 1:1,000) and the HSP60 ELISA kit (cat no. ESK-600)
were obtained from Stressgen Biotechnologies Co. (San Diego, CA,
USA). Caspase-3 (cat. no. 9665; 1:2,000), TLR4 (cat. no. 2219;
1:1,000), myeloid differentiation primary response 88 (MyD88; cat.
no. 4283, 1:1,000) antibodies were from Cell Signaling
Technologies, Inc. (Danvers, MA, USA). Anti-O4 antibody was
obtained from Merck Millipore (Darmstadt, Germany; cat no. MAB345;
1:200) The Live/Dead Assay kit was from Invitrogen (Thermo Fisher
Scientific, Inc., Waltham, MA, USA). The proteinase inhibitor
cocktails were from Merck & Co., Inc. (Whitehouse Station,
USA). IL-6 (cat. no. 85-BMS625), IL-1β (cat no. 85-BMS6002) and
TNF-α ELISA kits (cat. no. 85-BMS622) were from eBioscience, Inc.
(San Diego, CA, USA). Caspase 3 activity assay kit was from Promega
Corporation (Madison, WI, USA; cat. no. G809). The cell death assay
(CDD) kit was from Roche Applied Science (Pleasanton, CA, USA; cat
no. 11684795910). Bicinchoninic acid (BCA) and enhanced
chemiluminescence (ECL) kits were from Pierce (Thermo Fisher
Scientific, Inc.). Dulbecco's modified Eagle's medium (DMEM),
ProLong Gold Antifade reagent with DAPI (cat. no. P36931), and
fetal bovine serum (FBS) were from Gibco (Thermo Fisher Scientific,
Inc.). Alexa Fluor 647 Protein Labeling kit (cat no. A20173),
neurobasal medium (cat no. 10888022) and B27 (cat no. 17504044)
were from Thermo Fisher Scientific, Inc. Recombinant
platelet-derived growth factor (PDGF)-AA (cat no. AF-100-13A) and
TNF-α (cat no. 315-01A) were bought from PeproTech, Inc. (Rocky
Hill, NJ, USA). All other chemicals were purchased from ZSGB-BIO
(Shanghai, China), unless otherwise stated.
Primary culture of microglia and
OPCs
Purified microglia and OPCs were isolated as
previously described with some modifications (19). Mixed cortical glia cell cultures
were generated from 10 newborn P1 (weight, 5–7 g) male Sprague
Dawley rats (Animal Center of Ningxia Medical University, Yinchuan,
China) and maintained in DMEM with 20% FBS for 10 days in 75
cm2 flasks at 37°C and 95% O2/5%
CO2. The experiments were approved by the Ethics
Committee of Ningxia Medical University and reviewed by the
Institutional Review Board of Ningxia Medical University. The
culture medium was replaced every 3 days. For OPC collection,
cultures were first shaken for 1–2 h at 200 rpm. The microglia
cells were detached away from the attached cells and the suspension
cells were collected, cultured in fresh flasks with 10% FBS in
DMEM. The previous flasks were incubated in fresh medium in 95%
O2/5% CO2 at 37°C for 4 h, and then shaken at
260 rpm at 37°C for 16–18 h. The detached cell suspension was
seeded and allowed to adhere in uncoated Petri dishes for 1 h at
37°C with 95% O2/5% CO2, which allowed the
microglia and astrocytes to become firmly attached, whereas OPCs
were loosely attached and could be collected by gently shaking the
dishes. Collected OPCs in the medium were then replated at
5,000–50,000 cells/cm2 onto poly-D-lysine-coated plates,
dishes or coverslips. OPCs were grown in Neurobasal medium
supplemented with 2% B27. To expand the OPCs and to keep them
undifferentiated, the culture medium was supplemented with PDGF-AA
(10 nM). Microglia cells were cultured in DMEM supplemented with
10% FBS, penicillin (100 U/ml) and streptomycin (100 g/ml).
Cultures were maintained at 37°C in a humidified incubator gassed
with 95% O2 and 5% CO2.
Coculture of microglia and OPCs
For coculture experiments, microglia cells were
seeded at density 1,000–50,000 cells/cm2 onto Transwell
inserts (Millipore; Merck KGaA), and OPCs were also seeded at a
density 1,000–50,000 cells/cm2 on coverslips in a dish
separately for 24 h. Then microglia cells were treated with 1 µg/ml
LPS for 4 h and no LPS treatment group as control. The medium was
discarded and the Transwell with the microglia was moved on top of
the dish, thus sharing medium (DMEM/10% FBS) with the OPCs for 16
h. The Transwell was then removed and OPCs were fixed with 4%
paraformaldehyde in PBS for 15 min, washed 3 times with PBS, and
permeabilized with 0.5% Triton X-100 in PBS for 20 min. Cells were
washed 3 times again with PBS and blocked with 5% BSA for 1 h at
37°C. Cells were then incubated with anti-O4 mouse antibody in PBS
overnight at 4°C. Following washing with PBS, cells were incubated
with fluorescein isothiocyanate (FITC)-conjugated secondary
antibody (cat no. GTX77318; dilution, 1:1,000; GeneTex, Inc.,
Irvine, CA, USA) for 1 h at 37°C, washed with PBS and mounted using
ProLong Gold Antifade reagent with DAPI. Cells were visualized
using an Eclipse 660 fluorescent microscope (Nikon Corporation,
Tokyo, Japan). The images were analyzed using 5 randomly selected
fields of view and quantified using ImageJ version 1.48u
(imagej.nih.gov/ij/).
Binding assay
rhHSP60 was labeled with Alexa Fluor 647 using a
protein labeling kit (Thermo Fisher Scientific, Inc.), according to
the manufacturer's instructions. For live staining, OPCs were
incubated with Alexa 647-conjugated rhHSP60 at 4°C for 30 min.
Cells were visualized using an Eclipse 660 fluorescent microscope
and a Spot cooled CCD (both obtained from Nikon Corporation, Tokyo,
Japan).
Apoptosis
OPCs were treated with 5 µg/ml rhHSP60 or 10 ng/ml
TNF-α for 16 h at 37°C. Caspase 3 activity was measured using a
kit. DNA fragmentation was measured using the CDD assay, as per the
manufacturer's instructions.
Blocking antibody
Following 30 min of pre-incubation with the TLR4
blocking antibody (20 µg/ml), cells were treated with rhHSP60,
TNF-α or LPS for 16 h, prior to experiments.
ELISA
The levels of IL-6, IL-1β, HSP60 and TNF-α in
culture medium were quantified with commercial ELISA kits,
according to the manufacturer's directions. Absorbance was
determined at 450 nm using a microplate reader.
Western blotting
Cells were washed with PBS 3 times and lysed for 15
min at 4°C with radioimmunoprecipitation assay buffer containing 1%
NP40, 150 mM NaCl, 50 mM Tris-HCl, a protease inhibitor mixture, 50
mM NaF and 1 mM Na3VO4 for phosphatase
inhibition. Then the cell lysates were centrifuged at 1,200 × g for
10 min at 4°C and used for western blotting. The protein
concentration was determined by BCA kit, according to the
manufacturer's instructions. Equal quantities of protein (10 µg per
well) were loaded and ran on a 10% SDS-polyacrylamide gels and then
transferred to a polyvinylidene fluoride membrane. Membranes were
blocked with 5% nonfat dry milk in 0.1% Tween-20-Tris buffered
saline (TBST; pH 7.4) overnight at 4°C and incubated with primary
antibodies in TBS/0.1% Tween-20 (TBST) overnight at 4°C. Following
washing in milk-TBST, blots were incubated with horseradish
peroxidase-conjugated secondary antibodies goat anti-rabbit (cat.
no. ZB-2301; 1:5,000) and anti-mouse IgG (cat. no. ZB-2305;
1:5,000; ZSGB-BIO, Beijing, China). The target proteins were
detected by enhanced chemiluminescence (ECL) detection system and
X-ray films.
Statistical analysis
Statistical differences were determined using
one-way analysis of variance followed by a Holm-Sidak test. Data in
the text and figures are presented as the mean ± standard error.
Experiments were repeated 3 to 6 times. P<0.05 was considered to
indicate a statistically significant difference.
Results
Coculture of activated microglia with
OPCs results in OPC death
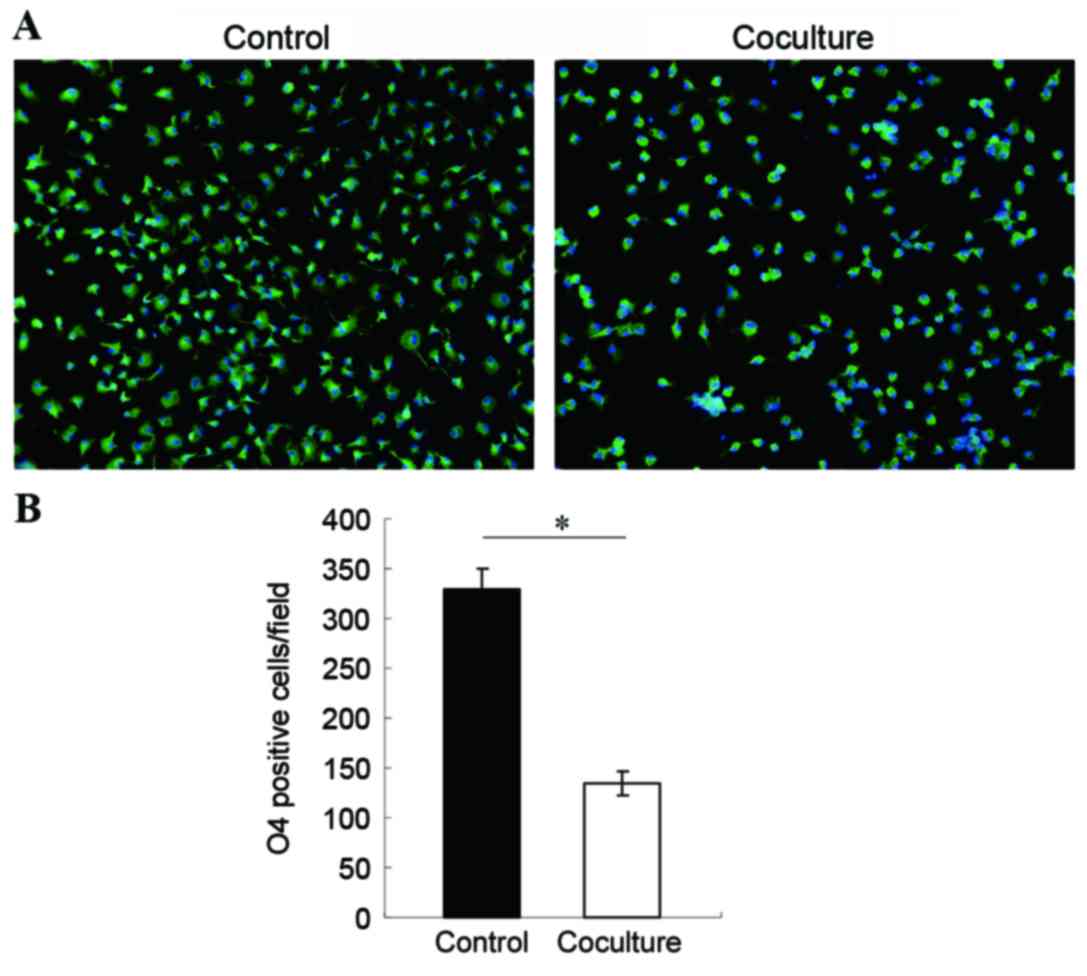
In order to observe the effects of activated
microglia on OPCs, the two cell types were cocultured. Microglia
were activated with 1 µg/ml LPS for 4 h in a transwell, then the
transwell was moved on top of a dish where OPCs were cultured, so
that the two cell types shared medium. Following 16 h of coculture,
OPCs were stained for expression of the O4 oligodendrocyte-specific
marker, visualized by a FITC-conjugated secondary antibody and
observed under a fluorescent microscope. The results demonstrated
that the number of live OPCs decreased significantly following
coculture with activated microglia compared with co-culture control
with non LPS-activated microglia (Fig.
1), indicating that activated microglia were toxic to
neighboring OPCs. Based on this result, the molecular mechanism of
microglia-induced OPC cell death was explored.
Expression and release of HSP60 in
activated microglia
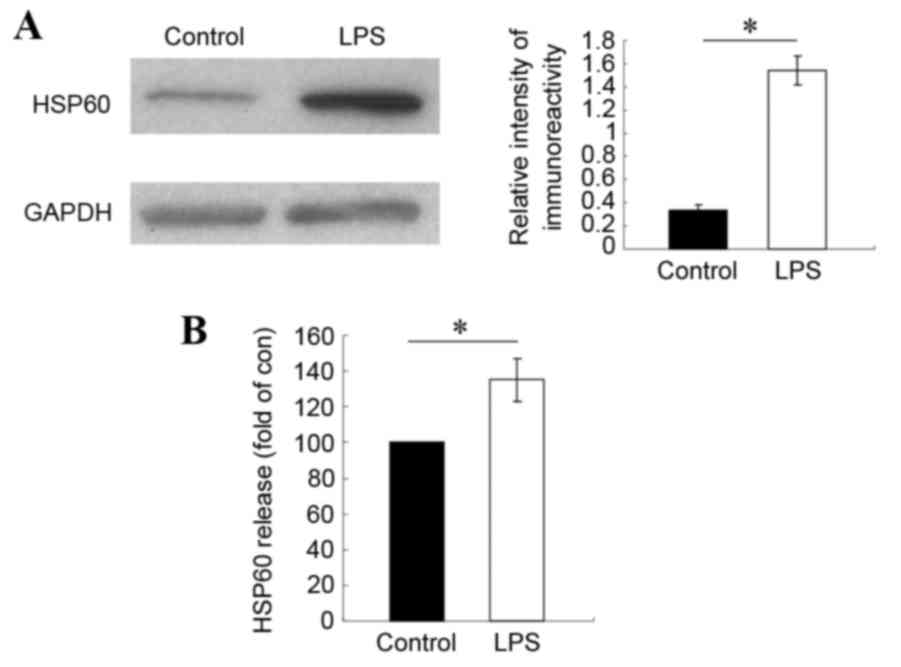
To test the hypothesis that HSP60 may be important
in microglia-mediated OPC death, HSP60 expression levels in
activated microglia were examined. Microglia cells were treated
with 1 µg/ml LPS for 4 h, then the protein lysate was analyzed by
western blotting for HSP60 expression levels. Compared with
untreated control cells, HSP60 protein expression levels increased
significantly in LPS-treated microglia (Fig. 1A). In order to examine the levels
of secreted extracellular HSP60, ELISA assay was performed in
samples of the culture media from LPS-treated and untreated
microglia cells. The results demonstrated that HSP60 levels in the
culture medium also significantly increased in LPS-treated
microglia, compared with untreated control cells (Fig. 2B). These results indicated that
HSP60 was highly expressed by activated microglia and was released
extracellularly. Therefore, HSP60 might be the toxic factor
released by microglia that caused the OPC death.
Extracellular rhHSP60 binding to OPCs
leads to OPC apoptosis
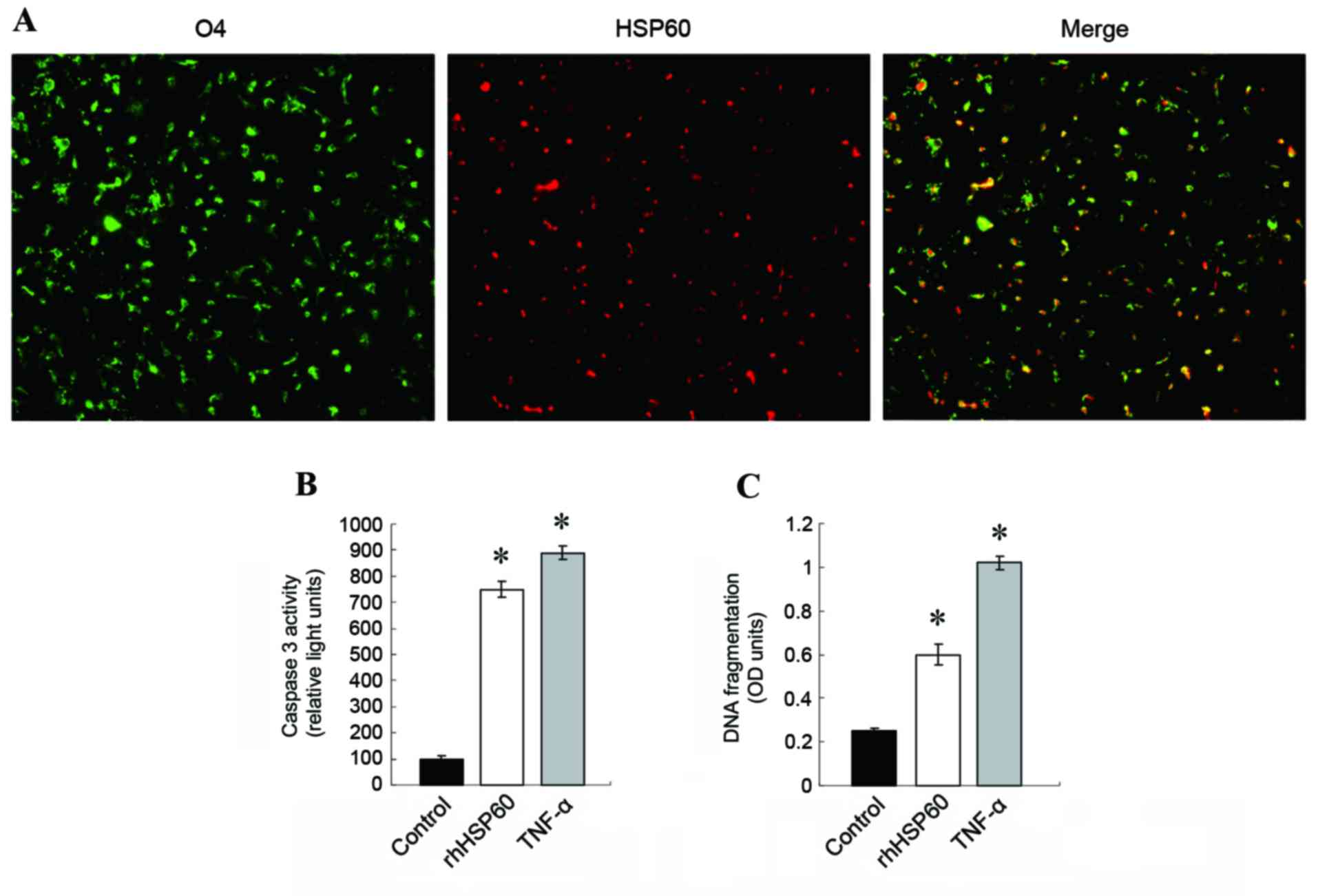
To examine further the effect of HSP60 on OPCs, OPCs
were incubated with fluorescently-labeled rhHSP60. As demonstrated
in Fig. 3A, Alexa 647-rhHSP60
bound on the surface of OPCs. Extracellular HSP60 (exHSP60) has
been reported to be a ligand of TLR4 (20). Therefore, exHSP60 binding on TLR4
in OPCs might lead to OPC apoptosis. Apoptosis was examined by
caspase 3 activity and DNA fragmentation assays following OPCs
treatment with rhHSP60 for 16 and 20 h, respectively. TNF-α
treatment (10 ng/ml), which causes apoptosis in OPCs, was used as a
positive control. Both rhHSP60 and TNF-α treatments resulted in a
similar increase of caspase 3 activity in OPCs, compared with
untreated cells (Fig. 3B). The CDD
assay confirmed this result, with both rhHSP60 and TNF-α
significantly triggering increased DNA fragmentation in OPCs,
compared with untreated cells (Fig.
3C).
TLR4 blocking antibody inhibits
rhHSP60-mediated caspase-3 expression
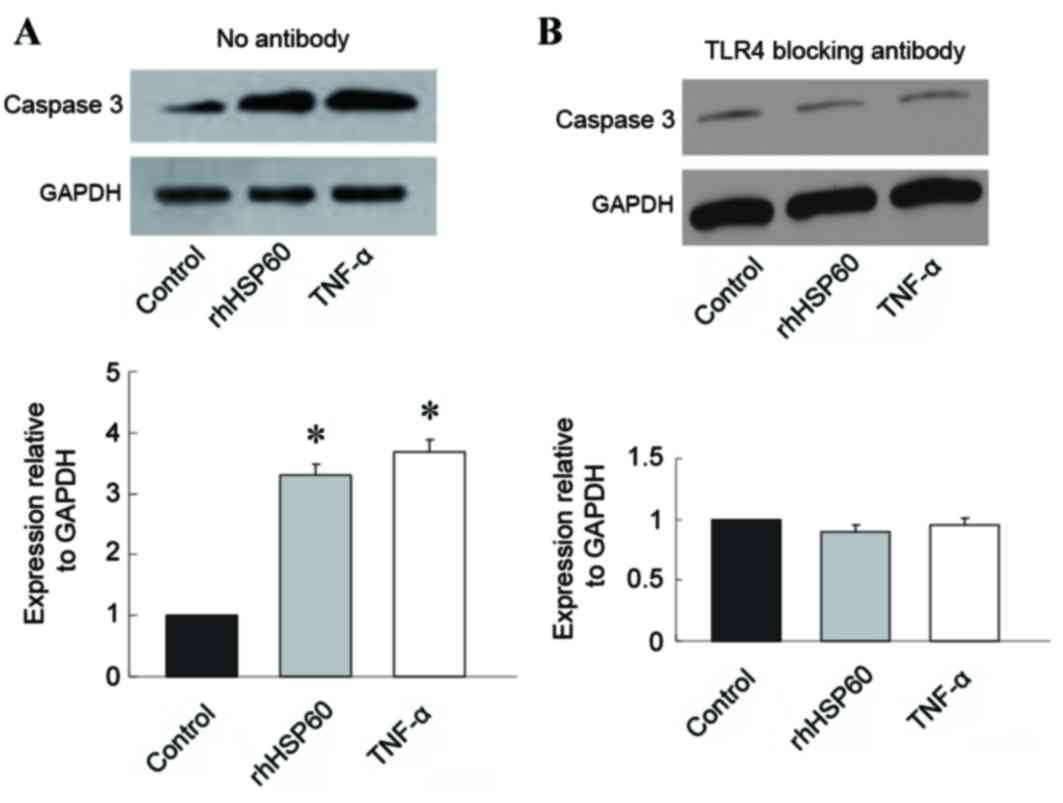
Since HSP60 has been proposed to be a ligand for
TLR4, the role of TLR4 in HSP60-mediated OPC apoptosis was
examined, by pretreating OPCs with a TLR4 blocking antibody.
Without the blocking antibody, rhHSP60 and TNF-α treatment
triggered a significant increase in caspase 3 expression in OPCs
compared with control untreated cells (Fig. 4A). However, pretreatment with 20
µg/ml anti-TLR4 blocking antibody for 30 min prevented the increase
in caspase 3 expression mediated by rhHSP60 or TNF-α; no
significant difference in caspase 3 expression was observed
following treatment with rhHSP60 or TNF-α compared with control
untreated cells (Fig. 4B).
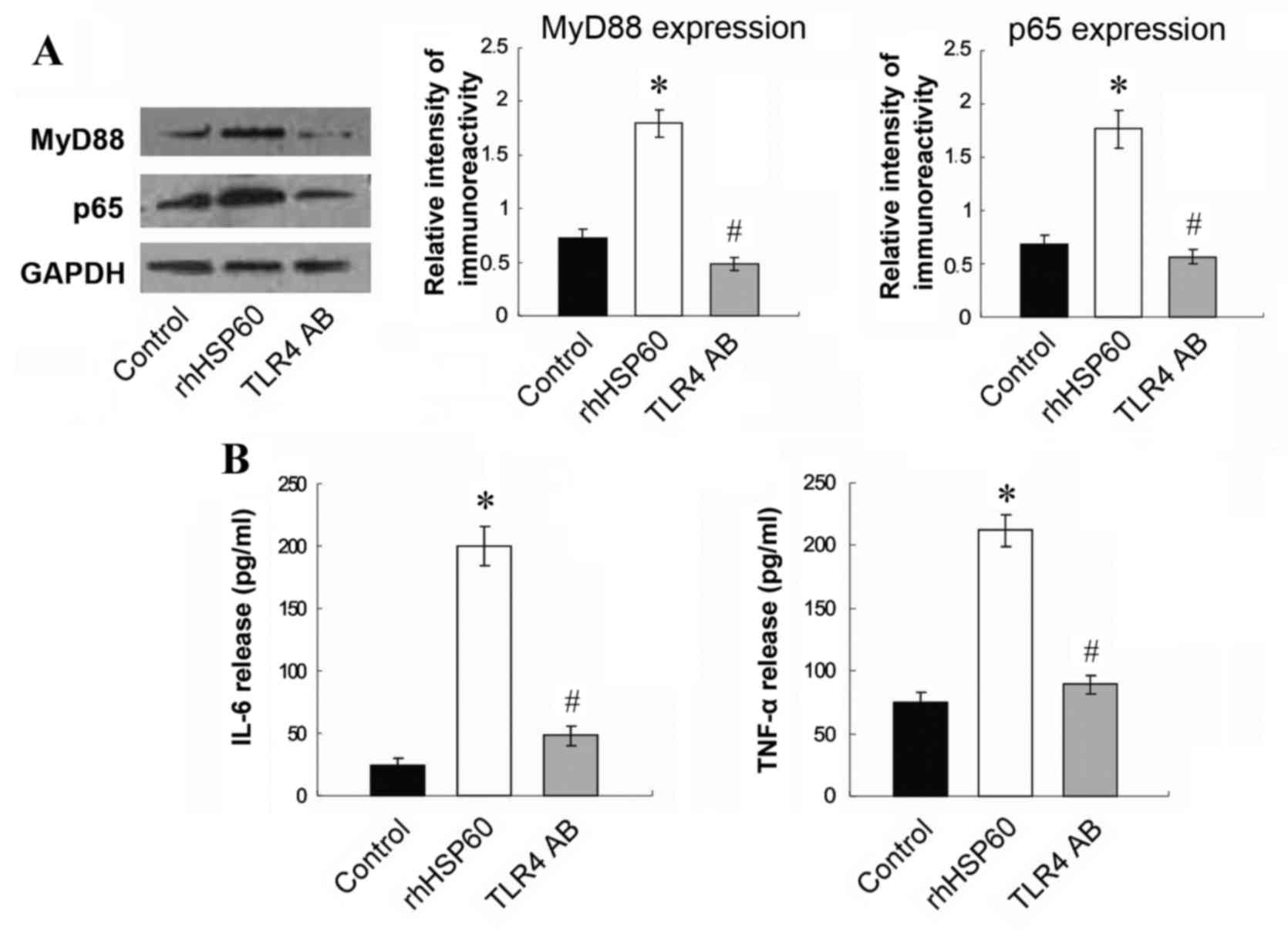
TLR4 blocking antibody reverses rhHSP60-mediated
MyD88, NFκ B and cytokine overexpression in OPCs. To
further investigate the signaling pathway leading to
rhHSP60-mediated apoptosis, the expression of downstream signaling
factors MyD88 and NFκB was examined by western blotting. Protein
expression levels of MyD88 and the NFκB subunit p65 significantly
increased by rhHSP60 treatment for 16 h in OPCs, compared with
untreated control cells (Fig. 5A).
This effect was, however, significantly reduced by pretreatment
with the TLR4 blocking antibody (Fig.
5A). In addition, release in the medium of the proinflammatory
cytokines IL-6 and TNF-α was significantly stimulated by rhHSP60
treatment in OPCs compared with untreated control cells (Fig. 5B), however this effect was also
suppressed by pretreatment with the TLR4 blocking antibody
(Fig. 5B). These results indicated
that HSP60 may act on OPCs through the TLR4-MyD88-NFκB signaling
pathway.
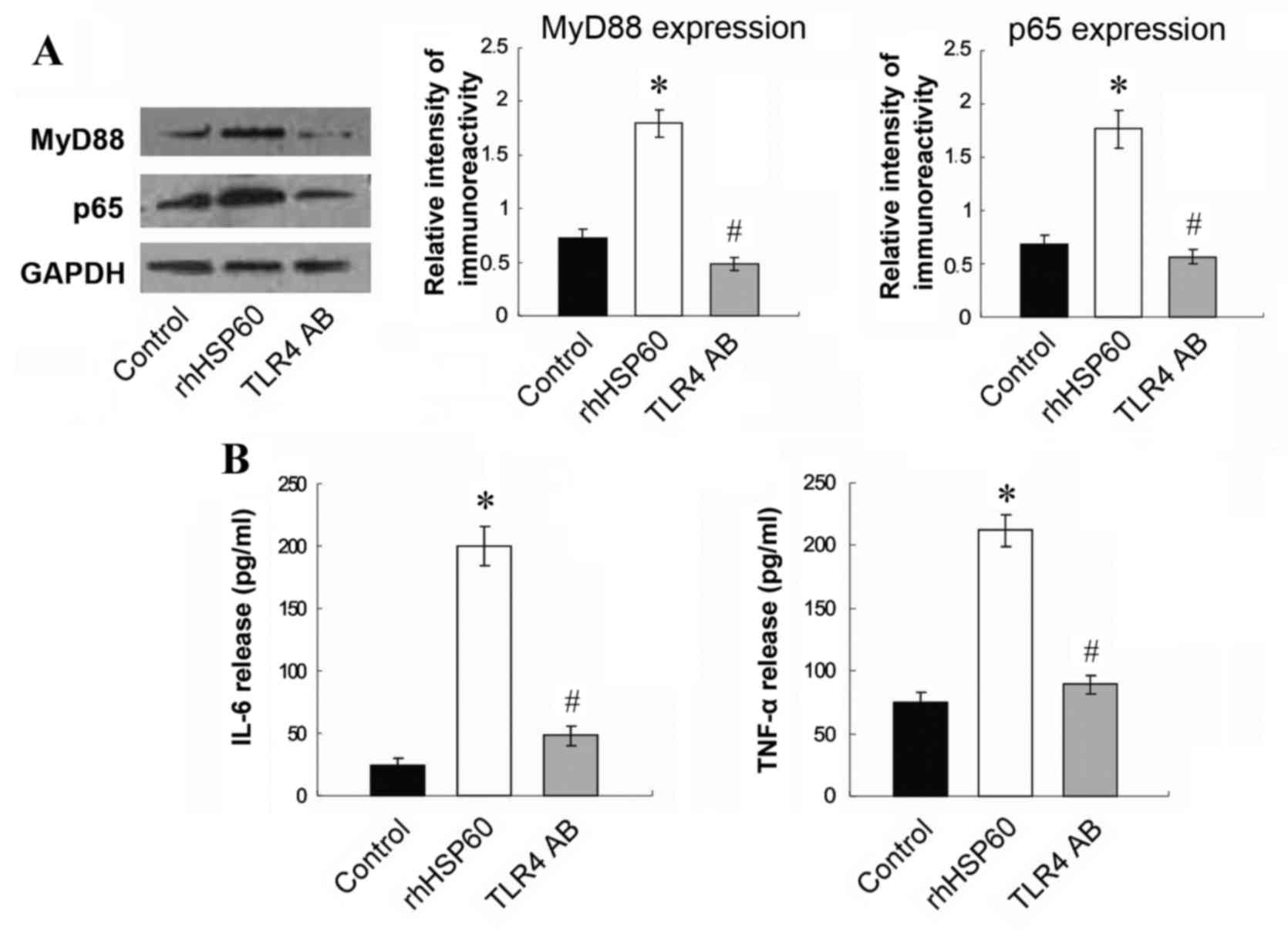 | Figure 5.TLR4 blocking antibody inhibits the
rhHSP60-mediated MyD88 and NFκB overexpression and cytokine
production. Following 30 min of preincubation with a TLR4 blocking
antibody, OPCs were treated with rhHSP60 for 16 h. (A) Protein
expression levels for MyD88 and the NFκB subunit p65 were measured
by western blotting in untreated cells (control), cells treated
with rhHSP60 and cells treated with hHSP60 + TLR4 blocking antibody
(TLR4 AB). Representative images and quantification are presented
relative to the GAPDH loading control. (B) Proinflammatory
cytokines IL-6 and TNF-α levels were measured by ELISA in the media
of untreated cells (control), cells treated with rhHSP60 and cells
treated with hHSP60 + TLR4 blocking antibody (TLR4 AB). *P<0.05
vs. control untreated cells; #P<0.05 vs. rhHSP60.
TLR4, toll-like receptor 4; rhHSP60, recombinant human heat shock
protein 60; MyD88, myeloid differentiation primary response 88;
NFκB, nuclear factor κB; OPCs, oligodendrocyte progenitor cells;
IL-6, interleukin 6; TNF-α, tumor necrosis factor α. |
Discussion
The present study demonstrated that activated
microglia released HSP60. ExHSP60 then bound to OPCs, which
resulted in caspase 3 activation and increased DNA cleavage in
OPCs, both markers of induction of apoptosis. TRL4 signaling was
demonstrated to be essential for the HSP60-mediated caspase 3
activation and release of proinflammatory cytokines. Finally, HSP60
was demonstrated to upregulate the MyD88-NFκB signaling pathway,
through TLR4. Thus, the present study suggested that activated
microglia released HSP60 resulting in OPC apoptosis, presumably
through the TLR4-MyD88-NFκB signaling pathway.
A number of studies have established that activated
microglia influence the survival of neurons (21). Studies examining the effect of
microglia on OPC survival have yielded conflicting results.
Filipovic and Zecevic (22)
reported that activated microglia are beneficial for OPC
proliferation, while Miller et al (23) reported that activated microglia
have divergent effects on OPCs and mature oligodendrocytes,
reducing OPC survival and increasing mature oligodendrocyte
survival. Additional studies have reported that microglia are toxic
to OPC in vivo and in vitro (18,24,25),
which is consistent with the current findings. In the present
study, it was demonstrated that the number of live OPCs decreased
significantly following coculture with LPS-activated microglia.
Activated microglia release various factors that are
important in microglia-induced OPC apoptosis (26). HSP60 is primarily a mitochondrial
protein, however it has been demonstrated that, upon stress or
injury in the heart, HSP60 translocates to the plasma membrane and
gets released extracellularly (12). A previous study from our group also
demonstrated that HSP60 is highly expressed and released by
microglia (13). ExHSP60 has been
demonstrated to be a ligand for TLR4 in the immune system (16), however this remains unclear for
other cell types. Tian et al (8) reported that extracellular HSP60
induces inflammation through upregulation and activation of TLRs in
cardiomyocytes. Taylor et al (17) demonstrated that active TLR4 is
present on OPCs. Therefore, in order to examine whether HSP60 can
be bound by OPCs, a binding experiment was performed by labeling
HSP60 with Alexa Fluor 647 and incubating OPCs with the
Alexa647-rhHSP60. The results demonstrated that exHSP60 bound on
the surface of OPCs, leading to caspase 3 activation and increased
DNA fragmentation compared with untreated cells.
Lehnardt et al (18) demonstrated that HSP60 alone had no
effect on neuronal survival. By contrast, when purified microglia
were added to neuronal cultures, severe loss of neurons was
observed in the presence of HSP60 (18). As a control, the addition of
purified microglia from mice with a tlr4 loss-of-function
mutation to wild-type neurons had no effect on neuronal survival
following HSP60 treatment, confirming the requirement for intact
TLR4 signaling (18). Within the
TLR4 signaling pathway, the adapter protein MyD88 is an important
activator of NFκB. Activation of NFкB is important in the
inflammatory response initiated by microglia, as transcription of
many proinflammatory genes is mediated by NFкB (27). NFκB has also been reported to
initiate transcription of the HSP60 stress protein gene, which
elicits a potent proinflammatory response in innate immune cells
(11). To determine whether HSP60
affects the TLR4-MyD88-NFκB pathway in OPCs, expression levels of
MyD88 and NFκB in OPCs were analyzed following HSP60 treatment. As
expected, MyD88 and NFκB subunit p65 protein expression levels in
OPCs increased significantly following HSP60 treatment, compared
with untreated cells. Activation of TLR4 was necessary for the
HSP60-mediated effects on OPCs; pretreatment with a TLR4 blocking
antibody, significantly inhibited the rhHSP60-mediated caspase 3
activation, in addition to attenuating the expression of MyD88 and
NFκB and the release of the proinflammatory cytokines IL-6 and
TNF-α. These observations suggest that HSP60 acts on OPCs through
the TLR4-MyD88-NFκB signaling pathway.
Acknowledgements
The present study was supported by grants from
Ningxia Natural Science Foundation (grant no. NZ14057), National
Natural Science Foundation of China (grant nos. 81460182, 31460257,
81571098 and 31260243), and Ningixa 13th Plan of five-year Major
Scientific Program (grant no. 2016BZ 07).
References
|
1
|
Hanisch UK and Kettenmann H: Microglia:
Active sensor and versatile effector cells in the normal and
pathologic brain. Nat Neurosci. 10:1387–1394. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
McGuire SO, Ling ZD, Lipton JW, Sortwell
CE, Collier TJ and Carvey PM: Tumor necrosis factor alpha is toxic
to embryonic mesencephalic dopamine neurons. Exp Neurol.
169:219–230. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chao CC, Hu S, Ehrlich L and Peterson PK:
Interleukin-1 and tumor necrosis factor-alpha synergistically
mediate neurotoxicity: Involvement of nitric oxide and of
N-methyl-D-aspartate receptors. Brain Behav Immun. 9:355–365. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pfeiffer SE, Warrington AE and Bansal R:
The oligodendrocyte and its many cellular processes. Trends Cell
Biol. 3:191–197. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Block ML, Zecca L and Hong JS:
Microglia-mediated neurotoxicity: Uncovering the molecular
mechanisms. Nat Rev Neurosci. 8:57–69. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim SC, Stice JP, Chen L, Jung JS, Gupta
S, Wang Y, Baumgarten G, Trial J and Knowlton AA: Extracellular
heat shock protein 60, cardiac myocytes, and apoptosis. Circ Res.
105:1186–1195. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gupta S and Knowlton AA: HSP60, Bax,
apoptosis and the heart. J Cell Mol Med. 9:51–58. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tian J, Guo X, Liu XM, Liu L, Weng QF,
Dong SJ, Knowlton AA, Yuan WJ and Lin L: Extracellular HSP60
induces inflammation through activating and up-regulating TLRs in
cardiomyocytes. Cardiovasc Res. 98:391–401. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Knowlton AA and Gupta S: HSP60, Bax, and
cardiac apoptosis. Cardiovasc Toxicol. 3:263–268. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kirchhoff SR, Gupta S and Knowlton AA:
Cytosolic heat shock protein 60, apoptosis, and myocardial injury.
Circulation. 105:2899–2904. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang Y, Chen L, Hagiwara N and Knowlton
AA: Regulation of heat shock protein 60 and 72 expression in the
failing heart. J Mol Cell Cardiol. 48:360–366. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lin L, Kim SC, Wang Y, Gupta S, Davis B,
Simon SI, Torre-Amione G and Knowlton AA: HSP60 in heart failure:
Abnormal distribution and role in cardiac myocyte apoptosis. Am J
Physiol Heart Circ Physiol. 293:H2238–H2247. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Teng P, Li Y, Cheng W, Zhou L, Shen Y and
Wang Y: Neuroprotective effects of Lycium barbarum polysaccharides
in lipopolysaccharide-induced BV2 microglia cells. Mol Med Rep.
7:1977–1981. 2013.PubMed/NCBI
|
|
14
|
Cheng W, Hou X, Zhang N, Ma J, Ding F, Li
F, Miao Z, Zhang Y, Qi Q, Li G, et al: HSP60 is involved in the
neuroprotective effects of naloxone. Mol Med Rep. 10:2172–2176.
2014.PubMed/NCBI
|
|
15
|
Cheng W, Li Y, Hou X, Bai B, Li F, Ding F,
Ma J, Zhang N, Shen Y and Wang Y: Determining the neuroprotective
effects of dextromethorphan in lipopolysaccharide-stimulated BV2
microglia. Mol Med Rep. 11:1132–1138. 2015.PubMed/NCBI
|
|
16
|
Ohashi K, Burkart V, Flohé S and Kolb H:
Cutting edge: Heat shock protein 60 is a putative endogenous ligand
of the toll-like receptor-4 complex. J Immunol. 164:558–561. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taylor DL, Pirianov G, Holland S,
McGinnity CJ, Norman AL, Reali C, Diemel LT, Gveric D, Yeung D and
Mehmet H: Attenuation of proliferation in oligodendrocyte precursor
cells by activated microglia. J Neurosci Res. 88:1632–1644.
2010.PubMed/NCBI
|
|
18
|
Lehnardt S, Lachance C, Patrizi S,
Lefebvre S, Follett PL, Jensen FE, Rosenberg PA, Volpe JJ and
Vartanian T: The toll-like receptor TLR4 is necessary for
lipopolysaccharide-induced oligodendrocyte injury in the CNS. J
Neurosci. 22:2478–2486. 2002.PubMed/NCBI
|
|
19
|
Yang Z, Watanabe M and Nishiyama A:
Optimization of oligodendrocyte progenitor cell culture method for
enhanced survival. J Neurosci Methods. 149:50–56. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rosenberger K, Dembny P, Derkow K, Engel
O, Krüger C, Wolf SA, Kettenmann H, Schott E, Meisel A and Lehnardt
S: Intrathecal heat shock protein 60 mediates neurodegeneration and
demyelination in the CNS through a TLR4- and MyD88-dependent
pathway. Mol Neurodegener. 10:52015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chao CC, Hu S, Molitor TW, Shaskan EG and
Peterson PK: Activated microglia mediate neuronal cell injury via a
nitric oxide mechanism. J Immunol. 149:2736–2741. 1992.PubMed/NCBI
|
|
22
|
Filipović R and Zecević N: 2005.
Interaction between microglia and oligodendrocyte cell progenitors
involves Golli proteins. Ann N Y Acad Sci. 1048:166–174. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Miller BA, Crum JM, Tovar CA, Ferguson AR,
Bresnahan JC and Beattie MS: Developmental stage of
oligodendrocytes determines their response to activated microglia
in vitro. J Neuroinflamm. 4:282007. View Article : Google Scholar
|
|
24
|
Pang Y, Cai Z and Rhodes PG: Effects of
lipopolysaccharide on oligodendrocyte progenitor cells are mediated
by astrocytes and microglia. J Neurosci Res. 62:510–520. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu X, Fan XL, Zhao Y, Luo GR, Li XP, Li R
and Le WD: Estrogen provides neuroprotection against activated
microglia-induced dopaminergic neuronal injury through both
estrogen receptor-alpha and estrogen receptor-beta in microglia. J
Neurosci Res. 81:653–665. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Butovsky O, Landa G, Kunis G, Ziv Y,
Avidan H, Greenberg N, Schwartz A, Smirnov I, Pollack A, Jung S and
Schwartz M: Induction and blockage of oligodendrogenesis by
differently activated microglia in an animal model of multiple
sclerosis. J Clin Invest. 116:905–915. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Khasnavis S, Jana A, Roy A, Mazumder M,
Bhushan B, Wood T, Ghosh S, Watson R and Pahan K: Suppression of
nuclear factor-κB activation and inflammation in microglia by
physically modified saline. J Biol Chem. 287:29529–29542. 2012.
View Article : Google Scholar : PubMed/NCBI
|