Introduction
Curculiginis orchioides (C.
orchioides) is the dried rhizome of the plant of Curculigo
orchioides Gaertn., belonging to the Amaryllidaceae
family (1). C. orchioides
is predominantly found in the Sichuan, Guizhou, Yunnan and Guangxi
provinces of China, and is a well-known traditional Chinese
medicinal herb (2). It has long
been used for the treatment of kidney disease, pain in the lumbar
spine, frequent urination, arthralgia and myalgia (2). It has been reported that C.
orchioides exhibits various pharmacological activities,
including antioxidant, immunoenhancement and anti-osteoporotic
effects, as well as promoting estrogen expression (3,4). In
addition, it has been reported that C. orchioides contains a
large number of chemical constituents, such as saponin, phenols and
glycosides (2). Curculigoside
(Fig. 1) is the main saponin in
C. orchioides, and its content in C. orchioides
varies from 0.11–0.35% (5).
Numerous investigations have shown that curculigoside exerts
significant antioxidant, anti-osteoporosis, antidepressant and
neuroprotection effects (6).
However, to the best of our knowledge, no studies have yet
investigated the effects of curculigoside in rheumatoid arthritis
(RA).
RA is an autoimmune disease which results in chronic
proliferative synovitis and inflammatory cell infiltration into the
joint synovial tissue (7–9). Chronic inflammation in RA causes
permanent joint destruction and deformity (10). Currently, RA treatment primarily
includes a combination of patient education, rest and exercise,
joint protection, medication and occasionally surgery (11). Medication for RA includes
nonsteroidal anti-inflammatory and disease modifying antirheumatic
drugs, as well as T-cell activation inhibitors, B-cell depleters,
tumor necrosis factor (TNF)-α inhibitors, interleukin (IL)-6
inhibitors and Janus kinase (JAK) inhibitors.
Therefore, the present study was designed to
systematically investigate the anti-inflammatory effects of
curculigoside on rats with type II collagen-induced arthritis
(CIA), and its antiproliferative effects against RA-derived
fibroblast-like synoviocyte MH7A cells. Furthermore, its potential
molecular effect mechanisms were explored, which may have
significant value for further identifying useful agents from the
plant of C. orchioides to treat diseases. Results from the
present study may provide an important scientific basis for future
studies on therapeutic applications.
Materials and methods
Chemicals and reagents
Bovine type II collagen (CII) was purchased from the
Chondrex, Inc. (Redmond, WA, USA), while Complete Freund's Adjuvant
(CFA) and Incomplete Freund's Adjuvant (IFA) were purchased from
Sigma-Aldrich; Merck KGaA (Darmstadt, Germany). Interleukin
(IL)-1β, interleukin-6 (IL-6), IL-10, IL-12 and IL-17A ELISA kits
were purchased from Invitrogen; Thermo Fisher Scientific, Inc.
(Waltham, MA, USA). RPMI-1640 medium and fetal bovine serum (FBS)
and trypsinase were obtained from Gibco (Thermo Fisher Scientific,
Inc.). A Cell Counting kit-8 kit, BCA protein assay reagent and
horseradish-peroxidase (HRP)-conjugated secondary antibodies (cat.
no. A0208) were purchased from Beyotime Institute of Biotechnology
(Haimen, China). Tumor necrosis factor (TNF)-α (cat. no. RAB0477),
dimethyl sulfoxide (DMSO) and IκB (cat. no. SAB1305978) were
purchased from Sigma-Aldrich; Merck KGaA. JAK1 (cat. no. ab133666),
JAK3 (cat. no. ab203611), STAT3 (cat. no. ab119352), nuclear factor
(NF)-κB p65 (Cytosolic; cat. no. ab19870), and β-actin (cat. no.
ab8226) antibodies were purchased from Abcam (Cambridge, MA, USA).
All other reagents used were of analytical grade.
Animals
Male Wistar rats (5–6 weeks old, 170–180 g; n=40)
were purchased from the Experimental Animal Center of Kunming
Medical University (Kunming, China). Animals were housed at 21±1°C
and 30–70% humidity under a 12 h light/dark cycle with free access
to standard pellet food and water. All animal experiments in the
present study were performed in accordance with the National
Institute of Health Guide for the Care and Use of Laboratory
Animals (12), and the
experimental protocols were approved by the Animal Care and Use
Committee of the First Affiliated Hospital of Kunming Medical
University (approval no. KMUH-2016023).
Cell culture
The RA-derived fibroblast-like synoviocyte MH7A cell
line was obtained from the Type Culture Collection of the Chinese
Academy of Sciences (Shanghai, China). MH7A cells were cultured in
RPMI-1640 medium with 10% FBS, 1% penicillin and 1% streptomycin in
a 5% CO2 humidified atmosphere at 37°C.
Curculigoside extraction
Dried rhizomes of C. orchioides were
purchased from Beijing Tongrentang (Beijing, China) and identified
by the department of Traditional Chinese Medicine, The First
Affiliated Hospital of Kunming Medical University (Kunming, China).
According to previously published protocols (13,14),
the rhizome of C. orchioides was powdered and then extracted
using 75% aqueous ethanol by reflux three times. Following this,
the filtrates were concentrated under 50°C in vacuum, and were
partitioned continuously with petroleum ether, ethyl acetate, and
n-butanol. The ethyl acetate fraction mentioned above was
eluted via silica-gel (100–200 mesh) with petroleum ether-acetone
(15:1, 10:1, 5:1, 2:1, 1:1) to obtain five sub-fractions (F1-F5).
By using a series of chromatographic techniques, including silica
gel column chromatography and Sephadex LH-20 chromatography
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany), curculigoside was
extracted from the F3 fraction (13). In addition, curculigoside (Fig. 1) was identified by
1H-nuclear magnetic resonance (NMR), 13C-NMR
and previously reported NMR data according to methods described
previously (13,14).
CIA animal model preparation
To investigate the potential anti-arthritic effects
of curculigoside, a total of 40 rats were divided into the
following four groups (n=10): Normal (not immunized and treated
with 10 ml/kg/day saline), control (immunized and treated with 10
ml/kg/day saline), positive [immunized and treated with
methotrexate (MTX); 1 mg/kg, three times a week] and curculigoside
group (immunized and treated with 50 mg/kg curculigoside).
The CIA rat model was prepared according to
previously reported methods, with minor modifications (15,16).
Briefly, CII was dissolved in 0.1 mM acetic acid to achieve a final
concentration of 4 mg/ml. Then, the CII solution was emulsified
with an equal volume of CFA. Rats were initially immunized by
subcutaneous injection of CII emulsion at the tail root (100
µl/rat). After 7 days, the rats were immunized by CII again,
emulsified by an equal volume of IFA at the same location (100
µl/rat). After approximately 10 days from the initial immunization,
rats evidently exhibited RA symptoms at the toe joint, including
observable inflammatory reactions, erythema and swelling.
At 10 days after the initial immunization with CII,
rats were orally treated with either saline, MTX or curculigoside
(50 mg/kg/day). During the experiment, the rats body weight and paw
volume were measured by using a PV-200 Plethysmometer (Paw Volume)
Meter (Techman Soft, Chengdu, China) every 5 days. In addition, the
arthritis indices of rats were measured every 3 days, using the
following ordinal scale: 0, no obvious signs of arthritis; 1, one
joint affected (swelling and erythema); 2, two joints affected; 3,
three joints affected; 4, three joints affected and maximal
erythema and swelling (17). After
30 days of drug treatment, rat weight was recorded (for the normal
and curculigoside treatment groups, rats weighed 320–340 g; for the
control and MTX groups, rats weighed 280–300 g), then rats were
sacrificed by decapitation under aesthesia with sodium
pentobarbital (35 mg/kg; intraperitoneal injection). Next, blood
was collected from abdominal aorta. The spleen and thymus were
dissected from each mouse to determine the ratio (mg/g) of thymus
or spleen wet weight to body weight.
Determination of serum cytokines
Serum samples were prepared and centrifugation 15
min (1,800 × g) at 4°C, and were stored at −80°C until analysis.
Then, serum TNF-α (cat. no. RAB0477), IL-1β (cat. no. BMS6002),
IL-6 (cat. no. BMS603-2), IL-10 (cat. no. 88-7105-88), IL-12 (cat.
no. BMS616) and IL-17A (cat. no. BMS6001) were detected by using
commercial ELISA kits according to the manufacturer's protocol and
instruction (Invitrogen; Thermo Fisher Scientific, Inc.).
Cell counting kit-8 (CCK-8) assay
Effects of curculigoside on cell viability were
determined by Cell Counting kit-8 according to the manufacturer's
protocol. MH7A cells (5×103 cells/well) were seeded in
96-well plates and incubated with various concentrations of
curculigoside (1, 2, 4, 8, 16, 32 and 64 µg/ml) for 12, 24, 36, 48
or 72 h. CCK-8 solution was added to each well and incubated for
another 1 h at 37°C. Optical density (OD) was measured at 450 nm
using a 96-well plate reader (Bio-Rad Laboratories, Inc., Hercules,
CA, USA). Results were reported as a percentage of DMSO control
cells.
Western blotting
JAK1, JAK3, STAT3, NF-κB p65 (C) and IκB expression
was measured in MH7A cells by western blotting. Following treatment
with various concentrations of curculigoside (4 and 16 µg/ml) or
vehicle (DMSO) in the presence of 10 ng/ml TNF-α for 36 h, Cells
(5×106) were harvested and homogenized with lysis buffer
for 10 min and centrifuged at 4°C for 5 min (10,000 × g). Total
protein was extracted from cells using the cell lysis buffer for
western blotting and IP (cat. no. P0013; Beyotime Institute of
Biotechnology), in addition, the cytoplasmic protein was extracted
by using NE-PER™ Nuclear and Cytoplasmic Extraction Reagents (cat.
no. 78833; Thermo Fisher Scientific, Inc.). The protein
concentration was determined with a bicinchoninic acid protein
assay. Subsequently, 40 µg total proteins in each sample was
separated by 12% SDS-PAGE and blotted onto polyvinylidene
difluoride (PVDF) membranes. Membranes were blocked with 5%
fat-free dry milk in 1X TBST (containing 0.1% Tween-20; Beyotime
Institute of Biotechnology; cat. no. P0233) at room temperature for
2 h. Thereafter, proteins on the PVDF membranes were probed with
JAK1 (dilution 1:1,000), JAK3 (dilution 1:1,000), STAT3 (dilution
1:1,000), NF-κB p65 (C) (dilution 1:1,000), IκB (dilution 1:1,000)
and β-actin (dilution 1:2,000) antibodies at 4°C for 12 h, followed
by incubation with corresponding horseradish peroxidase-conjugated
secondary antibodies (1:1,000; cat. no. A0208) for 2 h at 37°C.
Finally, immunoreactive bands were visualized with enhanced
chemiluminescence detection reagents (Beyotime Institute of
Biotechnology; cat. no. P0018A) and analyzed using the ImageQuant
LAS 4000 Imaging system (GE Healthcare Bio-Sciences, Pittsburgh,
PA, USA). Protein expression was normalized to β-actin.
Statistical analysis
All data are presented as the mean ± standard
deviation of three independent experiments, which were performed in
triplicate. Statistical analyses were performed via one-way ANOVA
followed by Dunnett's test using SPSS 19.0 software package (IBM
Corp., Armonk, NY, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Determination of paw swelling and
arthritis index in CIA rats
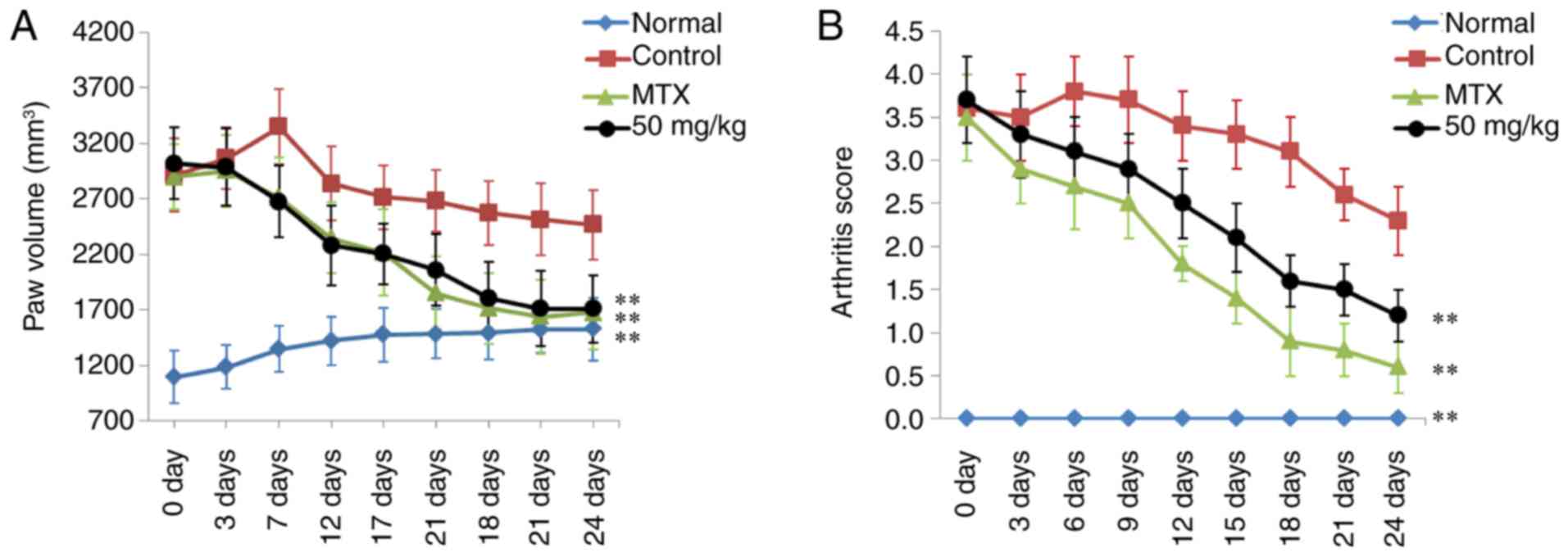
The paw swelling and arthritis score of rats in each
treatment group was determined to evaluate the therapeutic effects
of curculigoside on RA. As shown in Fig. 2, significant RA symptoms were
observed in the control CIA rats when compared to normal rats at 24
days, including paw swelling (P<0.01) and higher arthritis score
(P<0.01). Following treatment with MTX, paw swelling and
arthritis scores were reduced significantly, compared with the
control group (P<0.01). In addition, curculigoside (50 mg/kg)
also markedly decreased paw swelling and arthritis scores of CIA
rats (P<0.01), compared with control rats.
Curculigoside reduces spleen and
thymus indices in CIA rats
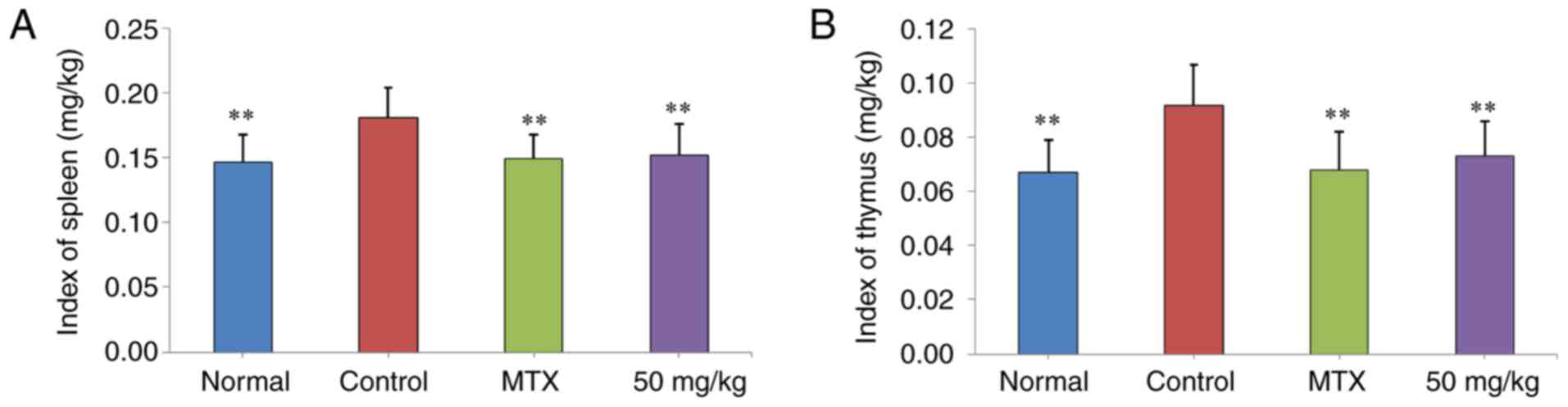
The effects of curculigoside treatment on spleen and
thymus indices in CIA rats were presented in Fig. 3. It was demonstrated that spleen
and thymus indices in the control group were significantly higher
than those of normal rats (P<0.01). Following treatment with
curculigoside (50 mg/kg), spleen and thymus indices were decreased
(P<0.01), compared with the control group.
ELISA assay
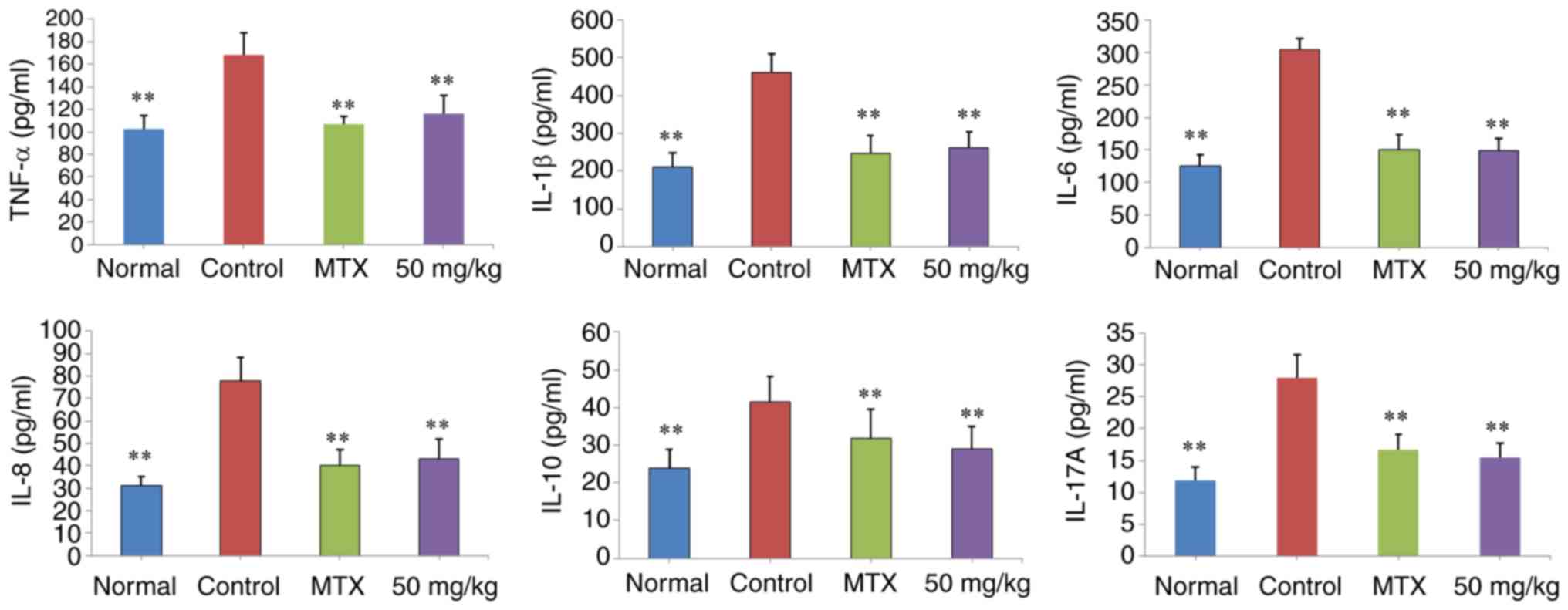
The expression of TNF-α, IL-1β, IL-6, IL-10, IL-12
and IL-17A in serum following treatment were shown in Fig. 4. It was observed that TNF-α, IL-1β,
IL-6, IL-10, IL-12 and IL-17A expression in control rats was
significantly increased when compared to the normal group
(P<0.01). The expression of these proteins in rat serum
decreased significantly following treatment with 50 mg/kg
curculigoside (P<0.01), compared with control CIA rats.
Curculigoside reduces MH7A cell
viability
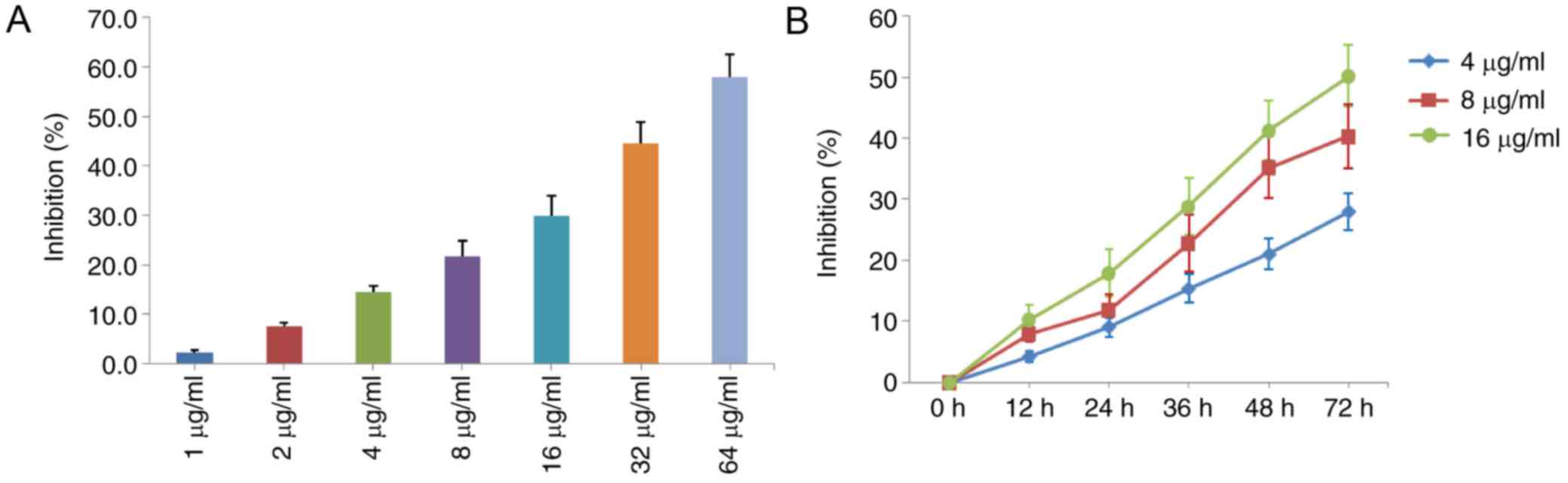
The effect of curculigoside on MH7A cell viability
was detected with CCK-8 assays. As presented in Fig. 5, curculigoside exerted significant
inhibitory effects on MH7A cell viability between 1 and 64 µg/ml.
In addition, our results also showed that curculigoside at the
concentrations of 4, 8 and 16 µg/ml possessed inhibitory effects on
MH7A cell viability within 72 h.
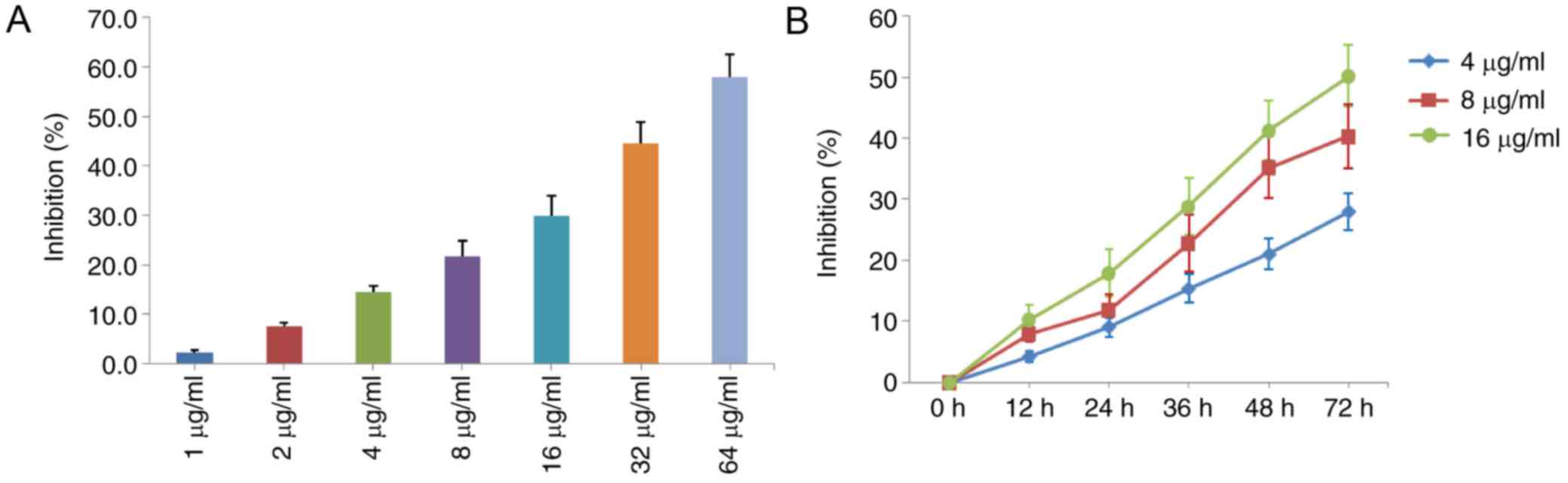 | Figure 5.Inhibitory effects of curculigoside
on the proliferation of MH7A cells. (A) Cells were treated with
curculigoside (1, 2, 4, 8, 16, 32 and 64 µg/ml) for 36 h, and then
a CCK-8 assay was performed to determine the percentage of cell
proliferation inhibition (n=4). (B) Cells were treated with
curculigoside (4, 8 and 16 µg/ml) for 12, 24, 36, 48, and 72 h time
intervals, and then a CCK-8 assay was performed to determine the
percentage of cell proliferation inhibition (%) (n=4). CCK-8, Cell
Counting kit-8. |
Curculigoside decreases JAK1, JAK3 and
STAT3 expression in TNF-α stimulated MH7A cells
Protein expression levels of JAK1, JAK3 and STAT3 in
TNF-α stimulated MH7A cells were measured by western blotting.
Compared to the TNF-α group, the protein expression of JAK1, JAK3
and STAT3 were significantly downregulated in the
curculigoside-treated groups (4 and 6 µg/ml) (P<0.01; Fig. 6).
Curculigoside increases IκB and
cytosolic NF-κB p65 expression in TNF-α stimulated MH7A cells
Furthermore, the effects of curculigoside on NF-κB
p65 (cytosolic) and IκB expression was determined by western
blotting in TNF-α stimulated MH7A cells. As presented in Fig. 7, the expression of NF-κB p65
(cytosolic) and IκB in TNF-α stimulated MH7A cells was
downregulated, compared with normal MH7A cells. Following treatment
with curculigoside (4 and 6 µg/ml) for 24 h, the expression of
NF-κB p65 (Cytosolic) and IκB was significantly upregulated
(P<0.01).
Discussion
Natural constituents isolated from plants or herbs
may have some pharmacological activity, and their discovery will be
useful in the development of novel drugs for treating RA and other
similar diseases (18,19). In the present investigation, the
anti-arthritic effect of curculigoside isolated from the C.
rhizoma was investigated in CIA rats and fibroblast-like
synoviocyte MH7A cells. The results indicated that curculigoside
possessed significant anti-arthritic effects in vivo and
in vitro, and this may be at least partially via regulation
of the JAK/STAT/NF-κB signaling pathway.
It has been reported that RA is an immune-mediated
disease with chronic progressive inflammation (20). Currently, the CIA and
adjuvant-induced arthritis (AIA) models are two commonly used RA
animal models (21). CIA is a
well-known RA animal model, which induces immunological and
pathological features similar to those in the RA in humans
(22,23). In the present study, a CII-induced
arthritis rat model was successfully established, and the
anti-arthritic effects of curculigoside were evaluated. It was
demonstrated that curculigoside decreased paw swelling and
arthritis scores, suggesting that curculigoside may possess
potential therapeutic effects in CIA.
To study the potential pharmacological mechanism,
the effects of curculigoside on the release of TNF-α, IL-1β, IL-6,
IL-10, IL-12 and IL-17A in rat serum were examined.
Pro-inflammatory cytokines have been reported as potential
therapeutic targets for RA, as these cytokines stimulate
inflammatory responses in arthritic joints and synovial tissues
(24–28). TNF-α is known to play a vital role
in the inflammatory and immunological responses in RA progression
and TNF-α is generally recognized as a promising target for anti-RA
drug (15). IL-1β and IL-17A are
other important pro-inflammatory cytokines in the development of RA
(15). Furthermore, IL-6 and IL-12
also serve an important role in RA inflammation via activating
inflammatory reactions (29). By
contrast, IL-10 has been regarded as a potent anti-inflammatory
cytokine through inhibiting the releases of pro-inflammatory
cytokines (30). The results of
the present study demonstrated that curculigoside decreased TNF-α,
IL-1β, IL-6, IL-10, IL-12 and IL-17A release in the serum of CIA
rats.
Synovial cell expansion is one of the main
pathological events in the inflamed synovium of patients with RA
(31). RA-derived fibroblast-like
synoviocytes with tumor-like expansion are the predominant cell
type in the hyperplastic synovium, and result in aggressive
cartilage invasion (32). In the
present study, the anti-proliferative effects of curculigoside on
MH7A cells suggested that it may be useful in RA treatment.
The JAK/STAT signaling pathway is involved in
cytokine signaling regulation. JAK/STAT signaling serves an
important role in the pathogenesis and progression of RA, and JAK
proteins can activate immune cells, induce proinflammatory cytokine
expression and transmit cytokine signaling (33–35).
JAK1 and JAK3 regulate cell signal transduction by binding with
cytokines (36). Additionally,
STAT3 is a key pathogenic factor in RA pathogenesis, and may
inhibit fibroblasts apoptosis, promote angiogenesis and the
expression of matrix metalloproteinase (MMP)-2 and MMP-9 (37). The results of the present study
showed that curculigoside downregulated JAK1, JAK3 and STAT3
expression in TNF-α stimulated MH7A cells, indicating that
curculigoside exerted anti-arthritic effects on MH7A cells,
potentially via the JAK/STAT pathway.
The NF-κB pathway is a prototypical inflammatory and
immune signaling pathway (38).
NF-κB is a key coordinator of innate immunity and inflammation
(39). p65, a NF-κB subunit, is
commonly localized to the cytoplasm by its inhibitor IκB (40). Following stimulation, NF-κB p65
translocates to the nucleus and exerts its function as a
transcription factor when IκB dissociates from NF-κB (41). In the present study, IκB and
cytosolic NF-κB p65 protein expression levels could be upregulated
by curculigoside, indicating that the anti-inflammatory effect of
curculigoside may be associated with inhibition of the NF-κB
signaling pathway.
Collectively, the present study demonstrated that
curculigoside exhibited significant anti-arthritic activity in
vivo and in vitro. This may be mediated by inhibition of
pro-inflammatory cytokine release and downregulation of JAK/STAT
signaling pathway proteins, as well as an increase in NF-κB and IκB
expression. The results of the present study suggested that
curculigoside could be regarded as a potential candidate drug for
RA treatment.
Acknowledgements
Not applicable.
Funding
The present study was supported by Scientific
Research Fund of Yunnan Provincial Education Department of China
(grant no. 2016zzx009), Scientific Research Fund of Yunnan
provincial of China (grant no. 2017FB108), the Fund of Yunnan
Provincial Health Science and Technology Plan (grant nos.
2016NS052, 2016NS051, 2017NS051 and 2017NS052), National Natural
Science Foundation of China (grant nos. 81460256, 81501406 and
81760296), Innovative Research Team of Kunming Medical University
(grant no. CXTD201613), Yunnan Provincial Fund for Preparatory
Young Leaders in Academia and Technology (grant no. 2015HB071), the
Funding of Yunnan Provincial Department of Education (grant no.
2017FE467), Yunnan Applied Basic Research Projects-Union Foundation
[grant no. 2017FE467 (−138)] and National Key R&D
Program-Specialized Research in Precision Medicine (grant no.
2017YFC0907605).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
JX, AL, RC, RB, SLi, WL and GZ performed the
measurements. SJ, SLiu and MZ analyzed and interpreted data. ST, JX
and WW made substantial contributions to conception and design, and
were involved in drafting, revising the manuscript and interpreting
all data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All animal experiments in the present study were
performed in accordance with the National Institute of Health Guide
for the Care and Use of Laboratory Animals, and the experimental
protocols were approved by the Animal Care and Use Committee of the
First Affiliated Hospital of Kunming Medical University (approval
no. KMUH-2016023).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chinese Pharmacopoeia Commission:
Pharmacopoeia of the People's Republic of China Part I. People's
Medical Publishing House. (Beijing). 1022015.
|
|
2
|
Huang YL: Research progress of
Curculiginis orchioides. J Chin Med Mater. 26:225–229.
2003.(In Chinese).
|
|
3
|
Zhang XJ, Sun YH and Wang HoY: Chemical
constituents from Curculigo orchioids. Chin Tradit Pat Med.
29:1869–1872. 2017.(In Chinese).
|
|
4
|
Fan PT, Zhang LM, Heng M, Liu BC, Xie X,
Ning ZS and Xu H: Effects of curculigoside on expressions of
Caspase-3, PARP-1 and estrogen receptor in hippocampus of model
rats with vascular dementia. Chin J Neuroanat. 33:453–458. 2017.(In
Chinese).
|
|
5
|
Lu HW, Zhu BH and Liang YK: Determination
of curculigoside in crude medicine curculigo orchioides by HPLC.
Zhongguo Zhong Yao Za Zhi. 27:192–194. 2002.(In Chinese).
PubMed/NCBI
|
|
6
|
Ooi J, Azmi NH, Imam MU, Alitheen NB and
Ismail M: Curculigoside and polyphenol-rich ethyl acetate fraction
of Molineria latifolia rhizome improved glucose uptake via
potential mTOR/AKT activated GLUT4 translocation. J Food Drug Anal.
26:1253–1264. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pu J, Fang FF, Li XQ, Shu ZH, Jiang YP,
Han T, Peng W and Zheng CJ: Matrine exerts a strong anti-arthritic
effect on type II collagen-induced arthritis in rats by inhibiting
inflammatory responses. Int J Mol Sci. 17(pii): E14102016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Okada Y, Wu D, Trynka G, Raj T, Terao C,
Ikari K, Kochi Y, Ohmura K, Suzuki A, Yoshida S, et al: Genetics of
rheumatoid arthritis contributes to biology and drug discovery.
Nature. 506:376–381. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang Q, Wang L, Wu L, Zhang M, Hu S, Wang
R, Han Y, Wu Y, Zhang L, Wang X, et al: Paroxetine alleviates T
lymphocyte activation and infiltration to joints of
collagen-induced arthritis. Sci Rep. 7:453642017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Firestein GS and McInnes IB:
Immunopathogenesis of rheumatoid arthritis. Immunity. 46:183–196.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xie QC and Yang YP: Anti-proliferative of
physcion 8-O-β-glucopyranoside isolated from Rumex japonicus Houtt.
on A549 cell lines via inducing apoptosis and cell cycle arrest.
BMC Complement Alter Med. 14:3772014. View Article : Google Scholar
|
|
12
|
National Institute of Health, USA. Public
health service policy on humane care and use of laboratory animals.
2002.
|
|
13
|
Wu XY, Li JZ, Guo JZ and Hou BY:
Ameliorative effects of curculigoside from Curculigo orchioides
Gaertn on learning and memory in aged rats. Molecules.
17:10108–10118. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fu DX, Lei GQ, Cheng XW, Chen JK and Zhou
TS: Curculigoside C, a new phenolic glucoside from rhizomes of
curculigo orchioides. Acta Bot Sin. 46:621–624. 2004.
|
|
15
|
Peng W, Wang L, Qiu X, Jiang Y, Han T, Pan
L, Jia X, Qin L and Zheng C: Therapeutic effects of Caragana
pruinosa Kom. roots extract on type II collagen-induced arthritis
in rats. J Ethnopharmacol. 191:1–8. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang F, Qiao YH, Niu HM and Zhao H:
Anti-arthritic effect of total anthraquinone from Polygonum
cuspidatum on type II collagen-induced arthritis in rats. Trop J
Pharm Res. 16:2453–2459. 2017.
|
|
17
|
Zheng CJ, Zhao XX, Ai HW, Lin B, Han T,
Jiang YP, Xing X and Qin LP: Therapeutic effects of standardized
Vitex negundo seeds extract on complete Freund's adjuvant induced
arthritis in rats. Phytomedicine. 21:838–846. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang Q, Kuang H, Su Y, Sun Y, Feng J, Guo
R and Chan K: Naturally derived anti-inflammatory compounds from
Chinese medicinal plants. J Ethnopharmacol. 146:9–39. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Peng W, Shen H, Lin B, Han P, Li CH, Zhang
QY, Ye BZ, Rahman K, Xin HL, Qin LP and Han T: Docking study and
antiosteoporosis effects of a dibenzylbutane lignan isolated from
Litsea cubeba targeting Cathepsin K and MEK1. Med Chem Res.
27:2062–2070. 2018. View Article : Google Scholar
|
|
20
|
Majithia V and Geraci SA: Rheumatoid
arthritis: Diagnosis and management. Am J Med. 120:936–939. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
McNamee K, Williams R and Seed M: Animal
models of rheumatoid arthritis: How informative are they? Eur J
Pharmacol. 759:278–286. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Luo Y, Liu M, Xia Y, Dai Y, Chou G and
Wang Z: Therapeutic effect of norisoboldine, an alkaloid isolated
from Radix Linderae, on collagen-induced arthritis in mice.
Phytomedicine. 17:726–731. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Trentham DE, McCune WJ, Susman P and David
JR: Autoimmunity to collagen in adjuvant arthritis of rats. J Clin
Investig. 66:1109–1117. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Imboden JB: The immunopathogenesis of
rheumatoid arthritis. Annu Rev Pathol Mech Dis. 4:417–434. 2009.
View Article : Google Scholar
|
|
25
|
Sennikov SV, Alshevskaya AA, Shkaruba NS,
Chumasova OA, Sizikov AE and Lopatnikova JA: Expression of TNFα
membrane-bound receptors in the peripheral blood mononuclear cells
(PMBC) in rheumatoid arthritis patients. Cytokine. 73:288–294.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kalden JR: Emerging role of anti-tumor
necrosis factor therapy in rheumatic diseases. Arthritis Res. 4
Suppl 2:S34–S40. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mariaselvam CM, Aoki M, Salah S, Boukouaci
W, Moins-Teisserenc H, Charron D, Krishnamoorthy R, Tamouza R and
Negi VS: Cytokine expression and cytokine-based T cell profiling in
South Indian rheumatoid arthritis. Immunobiology. 219:772–777.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Roeleveld DM and Koenders MI: The role of
the Th17 cytokines IL-17 and IL-22 in rheumatoid arthritis
pathogenesis and developments in cytokine immunotherapy. Cytokine.
74:101–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rossi D, Modena V, Sciascia S and
Roccatello D: Rheumatoid arthritis: Biological therapy other than
anti-TNF. Int Immunopharmacol. 27:185–188. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Conti P, Kempuraj D, Kandere K, Di
Gioacchino M, Barbacane RC, Castellani ML, Felaco M, Boucher W,
Letourneau R and Theoharides TC: IL-10, an inflammatory/inhibitory
cytokine, but not always. Immunol Lett. 86:123–129. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tran CN, Lundy SK and Fox DA: Synovial
biology and T cells in rheumatoid arthritis. Pathophysiology.
12:183–189. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Xia Y, Li X, Ou-Yang Z and Chen JW:
Selective modulation of MAPKs contribute to the anti-proliferative
and anti-inflammatory activities of
1,7-dihydroxy-3,4-dimethoxyxanthone in rheumatoid arthritis-derived
fibroblast-like synoviocyte MH7A cells. J Ethnopharmacol.
168:248–254. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
O'Shea JJ and Murray PJ: Cytokine
signaling modules in inflammatory response. Immunity. 28:477–487.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
O'Shea JJ and Plenge R: JAK and STAT
signaling molecules in immunoregulation and immune-mediated
disease. Immunity. 36:542–550. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Migita K, Izumi Y, Torigoshi T, Satomura
K, Izumi M, Nishino Y, Jiuchi Y, Nakamura M, Kozuru H, Nonaka F, et
al: Inhibition of Janus kinase/signal transducer and activator of
transcription (JAK/STAT) signalling pathway in rheumatoid synovial
fibroblasts using small molecule compounds. Clin Exp Immunol.
174:356–363. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sweeney SE and Firestein GS: Signal
transduction in rheumatoid arthritis. Curr Opin Rheumatol.
16:231–237. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Dutzmann J, Daniel JM, Bauersachs J,
Hilfiker-Kleiner D and Sedding DG: Emerging translational
approaches to target STAT3 signalling and its impact on vascular
dsease. Cardiovasc Res. 106:365–374. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Baker RG, Hayden MS and Ghosh S: NF-κB,
inflammation, and metabolic disease. Cell Metab. 13:11–22. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Vallabhapurapu S and Karin M: Regulation
and function of NF-kappaB transcription factors in the immune
system. Annu Rev Immunol. 27:693–733. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Beg AA and Baldwin AS Jr: The I kappa B
proteins: Multifunctional regulators of Rel/NF-kappa B
transcription factors. Genes Dev. 7:2064–2070. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lyss G, Knorre A, Schmidt TJ, Pahl HL and
Merfort I: The anti-inflammatory sesquiterpene lactone helenalin
inhibits the transcription factor NF-kappaB by directly targeting
p65. J Biol Chem. 273:33508–33516. 1998. View Article : Google Scholar : PubMed/NCBI
|