Introduction
Gastric diverticulum (GD) is a rare condition, with
a prevalence of 0.04 and 0.02% in upper gastrointestinal and
autopsy studies, respectively (1). GD
is characterized by the presence of a pouch protruding from the
gastric wall (1,2), however, the majority of GD cases are
asymptomatic and are diagnosed incidentally during routine
examinations (1). GDs are classified
into congenital and acquired types, of which, congenital types are
more common. Congenital GDs, located in the retroperitoneal space,
may be explained by embryogenesis. Acquired GDs are
pseudodiverticula and are typically located in the gastric antrum.
Acquired GDs are usually associated with gastrointestinal diseases,
such as, peptic ulcers, gastric outlet obstruction or other
malignancies (1). Although there is
currently no specific treatment for asymptomatic GD, symptomatic GD
requires appropriate management, which depends on the underlying
pathology and the severity of the presentation. In symptomatic
patients, typical symptoms include upper abdominal and epigastric
pain, anorexia, nausea and dysphagia (3). The first line therapy includes a
comprehensive examination for underlying pathology and medical
treatment, such as protein pump inhibitors, antacids, or
antispasmodics (4). When the
diverticulum is large, has not responded to medical therapy, or is
complicated by bleeding, perforation or other malignancies,
surgical resectioning is recommended (5). With prompt management, GDs may be
treated successfully without further complications.
Computed tomography (CT) imaging may detect the
presence of GDs as thin-walled cystic masses in the left adrenal
area. Conducting scans with the patient in a prone position may
further aid diagnosis, by forcing gastric air into the diverticulum
cavity, leading to the formation of an air-fluid level in the mass
(6). However, sole reliance on CT
imaging has been demonstrated to lead to the misdiagnosis of
gastric diverticula as adrenal tumors (7–15). The
current study reports the case of a 49-year-old male patient whose
initial abdominal CT scan indicated the presence of an adrenal
mass. A systematic literature review was also performed to
investigate the reasons for incorrect interpretation, and how this
may be avoided in future cases. Written informed consent was
obtained from the patient.
Case report
A 49-year-old male was admitted to The First
Affiliated Hospital, Zhejiang University School of Medicine
(Hangzhou, China) for further assessment of a left adrenal lesion
which had been identified incidentally at a routine physical
examination one month previously. The patient underwent an upper
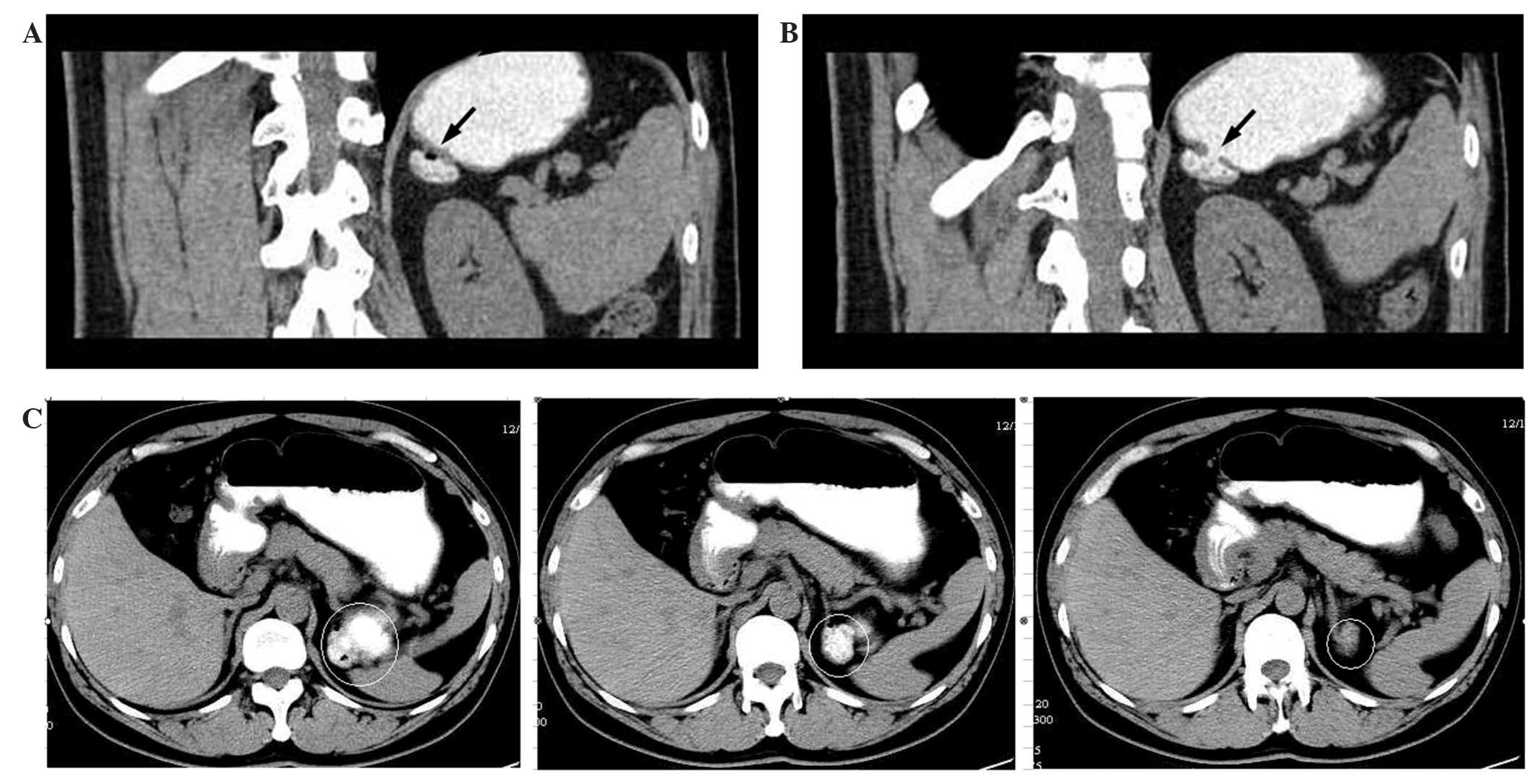
abdominal CT scan with intravenous contrast. A low-density mass
measuring 2.3 cm in diameter was observed in the area of the left
adrenal gland (Fig. 1). However, the
patient did not exhibit any clinical features and symptoms
typically associated with adrenal adenomas, which include
hypertension, hypokalemia and symptoms of hypercortisolism.
Furthermore, laboratory tests revealed that the basal levels of
plasma adrenocorticotropin, cortisol, aldosterone, renin,
testosterone, adrenaline, noradrenaline and dopamine were within
the normal range. A moderate elevation of urinary free cortisol
(345.4 µg/day; normal, 24–268 µg/day) was detected, which decreased
by >50% following treatment with low dose dexamethasone. The
results of all other laboratory examinations were normal.
The patient underwent several ultrasonography
examinations to visualize and evaluate the presumptive adrenal
mass, with negative results. A subsequent thorough review of the
data, including all prior CT images, revealed that the abnormality
was only visible in a small number of the CT imaging slices, and
appeared to be associated with the stomach. Oral contrast was
administered during a repeat abdominal CT scan in order to assess
whether the mass originated from the gastrointestinal tract.
Visualization of the mass was enhanced by the oral contrast
material shortly after staining the stomach and duodenum (Fig. 2). The results showed the presence of a
diverticulum in the fundus of the stomach. No treatment was
administered as the patient was asymptomatic. The patient was
followed up regularly and underwent an annual upper
gastrointestinal (GI) barium study. At the time of writing the
patient had been followed for more than three years and their
condition was stable.
Discussion
In the present case of gastric diverticulum, a
misdiagnosis was initially determined on the basis of a hypodense
component observed in the initial CT images. However, laboratory
findings were normal and ultrasonography examinations did not
detect an adrenal mass. Oral contrast material was administered
during a repeat abdominal CT scan, subsequently revealing the
presence of a diverticulum in the fundus of the stomach.
Reliance on CT scans in the absence of upper
gastrointestinal examinations may lead to misdiagnosis in cases of
GD, as this disorder, in addition to a number of normal structures,
anatomic variations, and lesions of adjacent organs (including
hepatic tumors, fluid-filled colon, splenic lobulation, tortuous or
dilated splenic arteries or veins, exophytic upper pole renal mass,
suprarenal fat, thickening of the diaphragm crura and pancreatic
tail masses) may mimic adrenal tumors. It is important to be
cautious when diagnosing masses in the region of the left adrenal
gland that are visualized on CT images (16).
A search of Pubmed, Medline, Cochrane, EMBASE, and
Google Scholar databases was conducted, identifying a total of 15
studies that described similar cases of misdiagnosed GD. Following
the exclusion of four non-relevant studies and four non-English
articles, a systematic review was conducted on seven studies,
including one article in Chinese (7,9–14) (Table I).
All studies were case reports of male patients with GD that
simulated masses in the left adrenal region. Of the seven studies,
six used an initial CT scan to visualize the lesion in the left
adrenal area. Approximately 5% of GDs are overlooked, even when
upper gastrointestinal tests are conducted (17). These studies emphasize the importance
of careful analysis of clinical data in order to eliminate the
possibility of pseudotumors and reduce unnecessary surgical
procedures. Only one case reported the use of magnetic resonance
imaging for initial diagnosis, based on which the patient was
diagnosed with an adrenal cyst (10).
In this patient, a signal void was observed the region three years
later, and a retrospective study of a previous CT images revealed
the presence of a previously unnoticed GD (10).
 | Table 1.Summary of reviewed articles
describing cases where gastric diverticula were initially
misdiagnosed as adrenal tumors. |
Table 1.
Summary of reviewed articles
describing cases where gastric diverticula were initially
misdiagnosed as adrenal tumors.
| Author (ref) | Age, y/ gender | Medical history | Assessment/ imaging
finding | Initial diagnosis and
treatment | Assessment/ imaging
finding not supporting initial diagnosis | Confirmation of
gastric diverticulum |
|---|
| Nogurea et al
(10) | N/A | N/A | MRI: A small signal
void in ventral area interpreted as ferritin and hemosiderin. | Left adrenal
cyst.
Treatment: N/A | Retrospective viewing
of previous CT: Small bubble of gas in ventral area of diverticulum
(initially overlooked). | CT scan |
| Kodera et al
(9) | 46/M | Four-month history of
hypertension | CT: 2.5 cm tumor
located in left adrenal region, observable with homogeneously low
(15HU) CT density.
MRI: Tumor clearly isolated from other tissues in suprarenal region
and exhibited high-intensity area on T2-weighted image. | Left adrenal cystic
and/or degenerated tumor. Treatment: None | Review of previous
CT: Small bubble shadow was observed in ventral aspect of left
adrenal tumor only in single slice of a CT scan. Consecutive views
of repeated thin-sliced CT scan did not detect air-like inclusion
in the tumor. | CT with oral contrast
gastrografin and upper GI barium study |
| Araki et al
(7) | 47/M | Hypertension/primary
aldosteronism | CT: Two masses in
left upper (3 cm) and lower (1.5 cm) adrenal portion. | Two left adrenal
adenomas. Treatment: Transperitoneal laparoscopic left
adrenalectomy | Laparoscopic surgical
exploration: Surface of 3 cm mass observed to be continuous with
stomach.
Reexamination of previous CT scan: Small bubble at ventral aspect
of 3 cm mass; supplied by a branch of splenic artery. | CT with more
concentrated oral contrast medium |
| Chasse et al
(11) | 42/M | Two-month history of
left lumbar pain, asthenia, and frequent headaches. | CT: 4.5 cm necrotic
mass close to left adrenal gland on upper abdominal CT scan. | Left adrenal
mass.
Treatment: Surgical exploration | Surgical exploration:
No mass identified in vicinity of kidney, adrenal gland or tail of
pancreas.
Repeated CT: Mass adjacent to left adrenal gland containing fluid
and circular hyperdense images consistent with tablets. | Upper GI barium
study |
| Silverman (12) | 46/M | Seven-month history
of hoarseness | CT: Failed intention
for mediastinal mass, discovered soft tissue mass posterior to
gastric fundus. | Left adrenal
mass.
Treatment: N/A | Upper GI barium
study: Gastric diverticulum extending posteriorly from fundus of
stomach. barium study | Selective CT
following upper GI |
| Schwartz et al
(13) | 63/M | Abdominal aortic
aneurysm | CT: Thin-walled
cystic mass with air-fluid level adjacent to left adrenal
gland. | Cystic left adrenal
mass.
Treatment: N/A | Repeat CT in 10 mm
sections with oral contrast: Barium-fluid-air level with mass,
indicating communication with GI tract. | Upper GI barium
study |
| Jing and Huang
(14) | 67/M | Hypertension, CVD,
pulmonary emphysema | CT: 3.4 cm necrotic
mass close to left adrenal gland on upper abdominal CT scan. | Left adrenal tumor
mass
Treatment: N/A | Repeat CT revealed
mass adjacent to left adrenal gland containing bubble.
Upper GI barium study confirmed 3 cm gastric diverticulum extending
posteriorly from fundus of stomach. | Repeat CT following
upper GI barium study |
Following an initial misdiagnosis as an adrenal cyst
or tumor, five of the seven studies used an upper GI barium test,
which confirmed the presence of GD in these patients. In one of
these cases, a left adrenal tumor was incidentally discovered in a
46-year-old male with hypertension who had been subjected to an
abdominal CT scan. Based on the presence of a bubble shadow in the
ventral section of the mass, oral contrast gastrografin was used in
a repeat CT scan to enhance the mass, and an upper GI barium study
was used to determine the diagnosis of GD (9). A 42-year-old male who presented with
left lumbar pain, asthenia and headaches was subjected to an upper
abdominal CT scan which indicated a necrotic mass in the area of
the left adrenal gland. However, surgical exploration revealed no
mass in the kidney, adrenal gland or tail of the pancreas, and the
presence of a GD was determined following an upper GI barium study
(11). Similarly, in a previous case
report in Japan, GD was not confirmed until postoperative X-rays of
the upper GI were evaluated (15).
Only one study exhibited similar characteristics to
the current study in the use of oral contrast material to diagnose
GD without performing an upper GI barium test (7). In this case, reported by Araki et
al (7), the presence of two left
adrenal adenomas in a 47-year-old male was indicated by an initial
CT scan. Laparoscopic left adrenalectomy revealed one adrenal
tumor, while the second mass was located between the spleen and
stomach and was continuous with the stomach. A repeat CT scan using
oral contrast material confirmed that the second mass was a GD.
Thus, in the case reported by Araki et al (7), oral contrast material was used to
diagnose GD without performing an upper GI barium test, which was
consistent with that of the present case.
In conclusion, given the risk of severe
complications in cases of GD, which includes bleeding, perforation,
and potential for malignant transformation, determining the correct
diagnosis is imperative (1). The
current case and data collected from the literature review suggests
that CT imaging enhanced by oral contrast material is an effective
technique which may aid in differentiating GD from an adrenal mass.
With the current advances in imaging technology, several
non-invasive modalities are available, such as CT image
reconstruction. Further investigations are required in order to
evaluate their diagnostic use in GD cases and to establish whether
they could be used to differentiate GDs from adrenal gland
tumors.
References
|
1
|
Rashid F, Aber A and Iftikhar SY: A review
on gastric diverticulum. World J Emerg Surg. 7:12012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen JH, Su WC, Chang CY and Lin H:
Education and imaging. Gastrointestinal: bleeding gastric
diverticulum. J Gastroenterol Hepatol. 23:3362008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
DuBois B, Powell B and Voeller G: Gastric
diverticulum: “a wayside house of ill fame” with a laparoscopic
solution. JSLS. 16:473–477. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Palmer ED: Gastric diverticulosis. Am Fam
Physician. 7:114–117. 1973.PubMed/NCBI
|
|
5
|
Rodeberg DA, Zaheer S, Moir CR and
Ishitani MB: Gastric diverticulum: a series of four pediatric
patients. J Pediatr Gastroenterol Nutr. 34:564–567. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Verbeeck N and De Geeter T: Suprarenal
mass due to a gastric diverticulum. J Belge Radiol. 77:119–120.
1994.PubMed/NCBI
|
|
7
|
Araki A, Shinohara M, Yamakawa J, Tanaka
M, Natsui S and Izumi Y: Gastric diverticulum preoperatively
diagnosed as one of two left adrenal adenomas. Int J Urol.
13:64–66. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Velanovich V: Gastric diverticulum.
Endoscopic and radiologic appearance. Surg Endosc. 8:1338–1339.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kodera R, Otsuka F, Inagaki K, et al:
Gastric diverticulum simulating left adrenal incidentaloma in a
hypertensive patient. Endocr J. 54:969–974. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Noguera JJ, Benito A, HernandezSastre C,
Cano D, Vivas I and Gonzalez-Crespo I: Gastric diverticulum
mimicking cystic lesion in left adrenal gland. Urology. 73:997–998.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chasse E, Buggenhout A, Zalcman M,
Jeanmart J, Gelin M and El Nakadi I: Gastric diverticulum
simulating a left adrenal tumor. Surgery. 133:447–448. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Silverman PM: Gastric diverticulum
mimicking adrenal mass: CT demonstration. J Comput Assist Tomogr.
10:709–710. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schwartz AN, Goiney RC and Graney DO:
Gastric diverticulum simulating an adrenal mass: CT appearance and
embryogenesis. AJR Am J Roentgenol. 146:553–554. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jing SL and Huang GZ: One case of gastric
diverticulum misdiagnosed as tumor in left adrenal gland. Zhongguo
Xian Dai Yi Xue Za Zhi. 17:24322007.(In Chinese).
|
|
15
|
Inaba Y, Maeda H and Umezu K: A case of
gastric diverticulum difficult to differentiate from left adrenal
tumor. Hinyokika Kiyo. 39:553–555. 1993.(In Japanese). PubMed/NCBI
|
|
16
|
Gokan T, Ohgiya Y, Nobusawa H and
Munechika H: Commonly encountered adrenal pseudotumours on CT. Br J
Radiol. 78:170–174. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Meeroff M, Gollán JR and Meeroff JC:
Gastric diverticulum. Am J Gastroenterol. 47:189–203.
1967.PubMed/NCBI
|