Introduction
Cotyledonoid dissecting leiomyoma (CDL) (1), also termed Sternberg tumor (2), is a rare variant of the uterine
leiomyoma. At present, ~43 cases of CDL have been reported in the
English literature (3). An accurate
diagnosis of CDL is challenging prior to surgery, as the
distinctive grapelike (4) gross
appearance of an exophytic mass resembles placental tissue and is
almost always misdiagnosed clinically as an ovarian tumor or
uterine sarcoma (5–8). The majority of patients with CDL are
diagnosed during an exploratory laparotomy (1,9–11), and a frozen section is recommended to
be used for the diagnosis of CDL (7,9). In the
literature, to preserve fertility, the recommended treatment is
resection of intrauterine tumors by myomectomy and extrauterine
tumors by excision (1,5,12,13). In women of postmenopausal stage, total
abdominal hysterectomy and bilateral salpingo-oophorectomy are
recommended with removal of parametrically extended tumors
(6,14–16). No
standard treatment for CDL has been identified; however, the
prognosis of CDL is favorable. In a previous study, follow-up
information was available for 25 of the 41 reported patients (61%),
none of which experienced tumor recurrence or metastases during the
follow-up period (17). The present
study reports the cases of 4 patients that were treated at the
Second Hospital of Jilin University (Changchun, Jilin, China)
between January 2009 and December 2011, in order to improve the
current understanding of the disease and to avoid misdiagnosis and
overtreatment. The study was approved by the Second Hospital of
Jilin Unviersity Ethics Committee (approval no. 2016-006).
Case report
Case 1
A 55-year-old woman, who had experienced menopause
for 7 years, presented to the Second Hospital of Jilin University
in January 2009 with a 3-month history of a palpable pelvic mass. A
pelvic examination revealed a solid mass, which measured 2×3 cm in
size and was attached to the posterior wall of the uterus, and an
irregularly contoured solid mass, which did not result in
tenderness and measured 7×5 cm in size, in the right adnexal
region. The transvaginal ultrasound scan demonstrated a regular
solid heterogenic low-echo mass that measured 6.9×4.5 cm in size in
the right adnexal region. A blood flow signal was detected around
the mass. A low-echo mass measuring 2.3×2.6 cm was identified
protruding from the lower posterior uterine wall. Magnetic
resonance imaging (MRI) examination confirmed the presence of an
irregular, lobulated, slightly enhanced mass signal that measured
10.0×8.0 cm in size, lying alongside the right lateral uterine
margin. A diagnosis of fibroma ovarii was suggested, and potential
serosal myometrial fibroids were not excluded. The cancer antigen
125 (CA125) level was 9 units/ml (normal range, 0–35 units/ml). A
diagnosis of ovarian tumor and uterine fibroid was made. The
patient underwent an exploratory laparotomy. During the surgery,
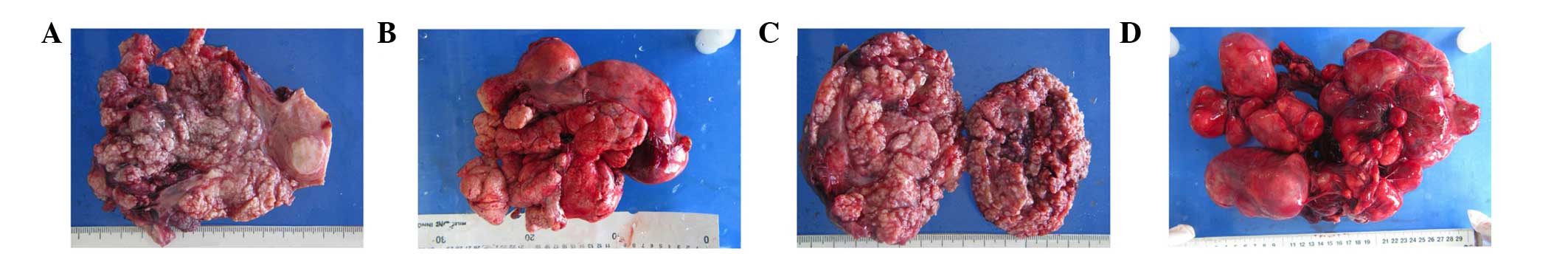
the uterus was detected to be irregularly enlarged (Fig. 1A). Multiple myomas were identified in
the posterior and right wall of the uterus and in the right broad
ligament. The diameter of the myomas ranged between 2 and 6 cm. The
myomas had merged into a large mass that resembled a cluster of
grapes, and extended into the broad ligament. An intraoperative
frozen section was obtained, and a diagnosis of CDL of the uterus
was made. A total abdominal hysterectomy was performed. The
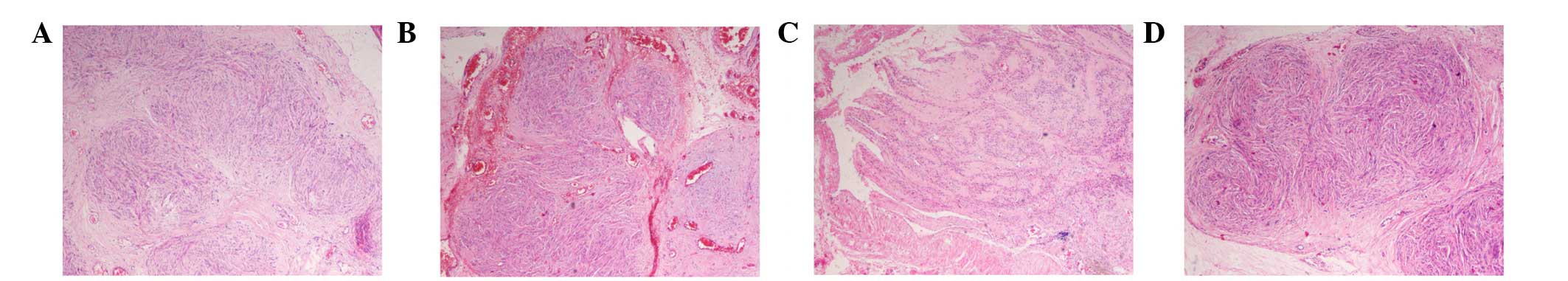
post-operative pathology confirmed that the lesion was CDL
(Fig. 2A). The patient was well and
showed no evidence of the disease subsequent to 48 months of
follow-up.
Case 2
A 43-year-old woman presented to the Second Hospital
of Jilin University in November 2009 with a 1-year history of a
palpable pelvic mass that had increased in size for 3 months. A
pelvic examination revealed a solid fixed mass that measured
~30×20×20 cm in size. A transvaginal ultrasound scan demonstrated
an irregularly contoured heterogenic mass that measured 30×30 cm in
size surrounding the uterus. Blood flow signals were detected
inside the mass, and the boundary of the mass was not clear. The
CA125 level was 13 units/ml (normal range, 0–35 units/ml). A
diagnosis of abdominal-pelvic mass was made. The patient underwent
an exploratory laparotomy. During the surgery, a slightly enlarged
uterus was observed, measuring ~8×8×7 cm in size, and multiple
heterogeneous myomas were distributed similar to a cluster of
grapes around the uterus (Fig. 1B).
The surface of the myomas was smooth. An intraoperative frozen
section was requested, and a diagnosis of CDL of the uterus was
made. A total abdominal hysterectomy and right
salpingo-oophorectomy were performed. The post-operative pathology
determined that the lesion was CDL with intravascular growth
(Fig. 2B). The patient was well and
showed no evidence of disease subsequent to 26 months of
follow-up.
Case 3
A 37-year-old woman presented to the Second Hospital
of Jilin University in May 2010 with a 1-month history of a
palpable pelvic mass. A pelvic examination revealed a solid mass
that measured 20×10×10 cm in size. The mass was not easy to move
when palpitated, indicating the involvement of surrounding tissues.
A transvaginal ultrasound scan demonstrated a mass that measured
30×22×7.1 cm in size surrounding the uterus, which was not observed
separately from the uterus. The echo of the mass resembled the echo
of the uterus, and blood flow signals were detected in the mass.
The CA125 level was 14 units/ml (normal range, 0–35 units/ml). A
diagnosis of pelvic mass and uterine fibroid was made. The patient
underwent an exploratory laparotomy. During the surgery, a solid
tumor that measured 25 cm in diameter, with a soft consistency,
rich vascularity and smooth surface was identified in the left
broad ligament. Multiple coralline-like tumor masses protruded from
the surface of the uterus (Fig. 1C).
An intraoperative frozen section was obtained, and a diagnosis of
CDL of the uterus was made. A subtotal abdominal hysterectomy and
bilateral salpingectomy were performed. The post-operative
pathology determined that the lesion was CDL of the uterus
(Fig. 2C). The patient was well and
showed no evidence of disease subsequent to 27 months of
follow-up.
Case 4
A 48-year-old woman presented to the Second Hospital
of Jilin University in December 2011 with a 3-month history of
fullness felt in the lower abdominal region, and a pelvic mass was
detected 1 day prior to admission to the hospital. A pelvic
examination revealed a solid mass that measured 14×14 cm in size
attached to the right wall of the uterus. The mass was easy to move
when palpitated, therefore the tumor was not adhered to adjacent
tissue, and the mass resulted in no tenderness. The transvaginal
ultrasound scan revealed an enlarged uterus that measured
11.5×6.7×4.8 cm in size, and detected numerous echo-poor regions in
the wall of the uterus. The largest echo-poor region, measuring
6.7×4.8 cm in size, was located in the right wall of the uterus.
The CA125 level was 15 units/ml (normal range, 0–35 units/ml). A
diagnosis of multiple uterine fibroids was made. The patient
underwent an exploratory laparotomy. During the surgery, the uterus
was 15.0×14.0×10.0 cm in size (Fig.
1D). A lobulated tumor mass with soft consistency that extended
from the right uterine wall to the surface of the posterior
peritoneum was detected. The uterine cervix, right fallopian tube,
retroperitoneal space, parametrium, posterior leaf of the left
broad ligament and the bladder posterior wall were involved. The
specimen was excised carefully. Macroscopically, the mass was
lobulated and resembled clusters of grapes. An intraoperative
frozen section was requested, and a diagnosis of CDL of the uterus
was made. A total abdominal hysterectomy and right-salpingectomy
were performed, including a removal of a retroperitoneal fibroid
extension. The post-operative pathology determined that the lesion
of the right broad ligament and the uterus was CDL (Fig. 2D). The patient was well and showed no
evidence of disease subsequent to 32 months of follow-up.
Discussion
CDL was first reported and named by Roth et
al (1) in 1966. As the study was
dedicated to the late Dr William H. Sternberg (2), who had originally studied the tumor as
‘a red seaweed lesion’, CDL was also termed the Sternberg tumor.
CDL is an atypical leiomyoma with an exophytic appearance and
variant growth pattern that was introduced to the WHO
Classification of Tumours of Female Reproductive Organs in 2003
(18). CDLs may be present in women
of reproductive or postmenopausal age, and CDL has a wide age range
of 23–65 years old (mean, 40.3 years) (19). According to the presentation of the
intramural dissection or extrauterine extension, CDL is also
classified as dissecting leiomyoma, cotyledonoid dissecting
leiomyoma or cotyledonoid leiomyoma (1). Due to the lack of typical clinical
symptoms, the majority of patients are admitted to hospital with
palpable masses and abnormal uterine bleeding. Only a few patients
present with no symptoms and identify the disease during physical
examinations. Gynecological examinations reveal a palpable pelvic
mass that may be detected by ultrasound scan in the uterus corpus
or the adnexal region. However, no specific symptoms or tumor
markers may be identified in clinical evaluations (17,20). All 4
patients in the present study presented with a pelvic mass that was
detected during a physical examination, and demonstrated no evident
clinical symptoms or menstruation change, including levels of the
CA125 tumor marker that were within the normal range. Ovarian tumor
was the most common preoperative diagnosis. Therefore, a lack of
specific clinical symptoms and tumor markers contributes to the
misdiagnosis of the disease.
Due to the distinctive gross appearance, the
diagnosis of the majority of CDLs is challenging prior to surgery.
Compared with common uterine fibroids, CDL has its own pathological
characteristics (20).
Macroscopically, the myometrium of the lateral side of the uterus
and the cornua is thinner and weaker compared with the normal
myometrium, which enables the tumor to protrude into the pelvic
cavity from the uterus. The tumor grows in a dissecting pattern in
the intrauterine component, and extends infiltratively from the
myometrium into the pelvic cavity (1,21). The
extrauterine component exhibits the gross features that resemble
cotyledons of the placenta, nodules or clubbed-finger. The cases in
the present study also presented with myomas protruding from the
lateral uterine myometrium that extended into the broad ligament.
In the majority of cases, the extrauterine component of the CDL
presents with increased vascularity and attachment to the lateral
uterine myometrium or cornua with a narrow fundus or soft fibrous
vascular pedicle (22). On electron
microscopy, nuclear atypia, mitotic activity and coagulative tumor
necrosis are absent (9). The cells
are disorganized or swirly in a fascicular or island formation, and
exhibit increased vascularity and significant hydropic stroma.
A differential diagnosis is necessary in order to
carefully distinguish CDL from other leiomyomas that share
similarities with CDL (17).
Endometrial stromal sarcoma is a similar leiomyoma where the smooth
muscle of the uterus is dissected by the tumor and, occasionally,
extends into one lateral ligament. The tumor tissues present with
vascular and lymphovascular invasion and a cancerous embolus.
Microscopically, deeply stained nuclei, nuclear atypia and mitotic
activity may be detected. Intravenous leimyomatosis (IVL) is rarely
reported leiomyoma that is characterized by an intravenous
component and embolus (23). The
typical gross appearance of IVL is multiple nodules protruding into
the broad ligament. Occasionally, the tumor mass may also be
multinodular and present with an irregular diffusion growth
pattern. Mucinous leiomyoma is a leiomyoma that presents with an
infiltrative growth pattern, has the appearance of mucinous
degeneration and contributes to the empty cysts in various sizes of
the mass (24). A degenerated region,
which has the appearance of cotton fibres, may be observed at the
cut surface, including mucinous cysts filled with transparent
mucus. Mucin histochemical staining is conductive to the
differential diagnosis of mucinous leiomyoma. Bizarre leiomyoma
(4) is a leiomyoma in which the
macroscopic features resemble those of conventional leiomyomas.
Microscopically, the mass consists of bizarre cells, pleomorphic
cells, multinucleated giant cell and enlarged hyperchromatic
nuclei. Mitotic figures are rarely observed.
Surgery is the best treatment for CDL. However, due
to the sarcomatoid operative appearance of the lesion,
overtreatment is almost always performed in clinical practice. In
2002, Kim et al (9) first
suggested that a frozen section may be obtained during the surgery.
In the case that the frozen section indicates a benign tumor, a
myomectomy may be considered for young women, particularly for
patients that want to preserve fertility. According to the age of
the patients, the requirement to bear children and the involvement
of the disease, the following surgical methods are always
considered, at present (1,5,6,12–16). For
older patients that do not express the desire to bear children, a
total hysterectomy may be the most appropriate treatment, as
demonstrated by the third and fourth cases in the present study.
For patients that do not express the desire to bear children, but
one of the adnexa is involved, a total hysterectomy and
salpingo-oophorectomy is an alternative. For older patients, a
total abdominal hysterectomy and bilateral salpingo-oophorectomy
may be considered, as demonstrated by the second case in the
present study. For older patients of postmenopausal age, a total
abdominal hysterectomy and bilateral salpingo-oophorectomy is the
best alternative, as demonstrated by the first case in the present
study. For patients of a reproductive age that may or may not
desire children, a myomectomy is appropriate (3). Saeki et al (3) reported the successful delivery of a baby
following a myomectomy for CDL. All patients that were admitted to
the Second Hospital of Jilin University underwent exploratory
laparotomy. The final surgical method was decided according to the
intraoperative findings.
In conclusion, CDL is a rare disease with a good
prognosis. However, the diagnosis of CDL prior to surgery is
challenging. Macroscopically, CDL may resemble malignant tumors,
which poses a significant challenge for the diagnosis and
management of the disease. Microscopically, the determination of a
differential diagnosis may be problematic, so the analysis of a
frozen section is recommended in order to avoid misdiagnosis and
overtreatment. An awareness of leiomyoma variants is required by
gynecological surgeons and pathologists for successful differential
diagnosis.
Acknowledgements
The present study was supported by grants from the
National Natural Science Foundation of China (grant nos. 81272875
and 81302242), the Jilin Science and Technology Fund (grant nos.
20110755, 20130102094JC and 20140204022YY), the Basic Science
Research Fund of Jilin University (grant no. 20142116), the
Teaching Reform Project of Jilin University (grant nos. 2013163 and
2014ZH26), Education Science and Planning Issues of Jilin Province
(grant no. ZZ1301) and the Doctoral Degree courses of Jilin
University (grant no. 2014ZT10).
References
|
1
|
Roth LM, Reed RJ and Sternberg WH:
Cotyledonoid dissecting leiomyoma of the uterus. The Sternberg
tumor. Am J Surg Pathol. 20:1455–1461. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sternberg WH: Proliferating pelvic
angioleiomyomatosis (red seaweed lesion). Proceedings of the 9th
George Papanicolaou Memorial. Seminar in Gynecologic Pathology.
(Las Vegas, NV). 1979.
|
|
3
|
Saeki H, Suzuki C, Yamasaki S, Hashizume
A, Izumi H, Suzuki F, Ishi K, Nojima M and Hino O: Cotyledonoid
dissecting leiomyoma of the uterus: Report of two cases. Arch
Gynecol Obstet. 291:357–361. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
David MP, Homonnai TZ, Deligdish L and
Loewenthal M: Grape-like leiomyomas of the uterus. Int Surg.
60:238–239. 1975.PubMed/NCBI
|
|
5
|
Tanaka H, Toriyabe K, Senda T, Sakakura Y,
Yoshida K, Asakura T, Taniguchi H and Nagao K: Cotyledonoid
dissecting leiomyoma treated by laparoscopic surgery: A case
report. Asian J Endosc Surg. 6:122–125. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim NR, Park CY and Cho HY: Cotyledonoid
dissecting leiomyoma of the uterus with intravascular luminal
growth: A case study. Korean J Pathol. 47:477–480. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Saeed AS, Hanaa B, Faisal AS and Najla AM:
Cotyledonoid dissecting leiomyoma of the uterus: A case report of a
benign uterine tumor with sarcomalike gross appearance and review
of literature. Int J Gynecol Pathol. 25:262–267. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Onu DO, Fiorentino LM and Bunting MW:
Cotyledonoid dissecting leiomyoma as a possible cause of chronic
lower back pain. BMJ Case Rep. 11:20132013.
|
|
9
|
Kim MJ, Park YK and Cho JH: Cotyledonoid
dissecting leiomyoma of the uterus: A case report and review of the
literature. J Korean Med Sci. 17:840–844. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Driss M, Zhioua F, Doqhri R, Mrad K,
Dhouib R and Romdhane KB: Cotyledonoid dissecting leiomyoma of the
uterus associated with endosalpingiosis. Arch Gynecol Obstet.
280:1063–1065. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Blake EA, Cheng G, Post MD and Guntupalli
S: Cotyledonoid dissecting leiomyoma with adipocytic
differentiation: A case report. Gynecol Oncol Rep. 11:7–9. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chávez Martínez S, Arias González ML,
Silva López RM and Villagrán Uribe JA: Cotyledonoid dissecting
leiomyoma of the uterus. A malignant-looking benign tumor. Ginecol
Obstet Mex. 80:528–533. 2012.(In Spanish). PubMed/NCBI
|
|
13
|
Raga F, Sanz-Cortés M, Casañ EM, Burgues O
and Bonilla-Musoles F: Cotyledonoid dissecting leiomyoma of the
uterus. Fertil Steril. 91:1269–1270. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gezginç K, Yazici F, Selimoğlu R and Tavli
L: Cotyledonoid dissecting leiomyoma of the uterus with
intravascular growth in postmenopausal woman: A case presentation.
Int J Clin Oncol. 16:701–704. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Majd Soleymani H, Ismail L, Desai SA and
Reginald PW: Epithelioid cotyledonoid dissecting leiomyoma: A case
report and review of the literature. Arch Gynecol ObstetArch.
283:771–774. 2011. View Article : Google Scholar
|
|
16
|
Weissferdt A, Maheshwari MB and Downey GP:
Cotyledonoid dissecting leiomyoma of the uterus: A case report.
Diagn Pathol. 2:182007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Smith CC, Gold MA, Wile G and Fadare O:
Cotyledonoid dissecting leiomyoma of the uterus: A review of
clinical, pathological, and radiological features. Int J Surg
Pathol. 20:330–341. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tavassoli F and Devilee P: World Health
Organization Classification of Tumours. Pathology and Genetics of
Tumours of the Breacst and Female Genital Organs. IARC Press.
(Lyon). 2412003.
|
|
19
|
Ersöz S, Turgutalp H, Mungan S, Güvendı G
and Güven S: Cotyledonoid leiomyoma of uterus: A case report. Turk
Patoloji Derg. 27:257–260. 2011.PubMed/NCBI
|
|
20
|
Makharoblidze E, Goishvili N,
Mchedlishvili M, Khakhutaishvili I and Jangavadze M: Unusual types
of smooth muscle tumors of uterine corpus: Case reports and
literature review. Georgian Med News. 216:7–11. 2013.PubMed/NCBI
|
|
21
|
Mathew M, Gowri V, Al Hamdani A, Machado
L, Rao K and Shabnam S: Cotyledonoid leiomyoma in pregnancy. Obstet
Gynecol. 109(Suppl): 509–511. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Majd Soleymani H, Ismail L, Desai SA and
Reginald PW: Epithelioid cotyledonoid dissecting leiomyoma: A case
report and review of the literature. Arch Gynecol Obstet.
283:771–774. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jordan LB, Al-Nafussi A and Beattie G:
Cotyledonoid hydropic intravenous leiomyomatosis: A new variant
leiomyoma. Histopathology. 40:245–252. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Radojković M, Stojanović M, Gligorijevioć
J, Stanojević G, Kovarevios P, Petković TR, Pecić V and Rancić Z:
Giant primary retroperitoneal myxoid leiomyoma: A case report.
Vojnosanit Pregl. 70:522–525. 2013. View Article : Google Scholar : PubMed/NCBI
|