Introduction
Lung cancer is the leading cause of cancer-related
mortality worldwide (1).
Approximately 85% of lung cancers are classified as non-small cell
lung cancer (NSCLC) (2), and the
majority of patients present with unresectable advanced disease.
Despite the advances over the past decades in terms of cancer
treatments, the overall five-year survival rate for NSCLC patients
remains less than 15% (3). Late
diagnosis of NSCLC is one of the significant contributing factors
to the poor clinical outcome, since the tumor has often spread to
distant organs at the time of diagnosis. The five-year survival
rate following surgical resection is ~80% for early-stage NSCLC,
but that rate drops to just 30% in patients with advanced stages
(4). Thus, earlier detection of NSCLC
would greatly facilitate more effective management of the
disease.
Currently, histological examination is still the
gold standard for the diagnosis of NSCLC. However, in this approach
it is necessary to obtain tissues or cells from patients, and
invasive examination methods are required, including bronchoscopy,
lung puncture, endobronchial ultrasound or thoracotomy. Although
chest X-ray and computed tomography examinations are capable of
detecting early-stage NSCLC, certain studies have demonstrated that
50% of pulmonary nodules detected by these approaches are benign
(5), and that these methods have
limited function in reducing lung cancer mortality (6). Moreover, the limited sensitivity and
specificity of previously known lung cancer biomarkers, including
cytokeratin fragment 21-1, tumor polysaccharides and
carcinoembryonic antigen, hampered their further application and
development (7). Therefore, a
biomarker with non-invasiveness, high sensitivity and high
specificity for the early diagnosis of lung cancer is required.
microRNAs (miRNAs) are a class of highly conserved
non-coding small RNAs, consisting of 20–24 nt and existing widely
in eukaryotic cells. The first miRNA was identified in the mutant
of Caenorhabditis elegans by Lee et al in 1993
(8). Following that, a large number
of miRNAs were identified in Drosophila, Arabidopsis, zebra
fish, rice and human cells. According to the latest version of the
miRBase (http://www.mirbase.org/), there are more
than 2600 miRNAs in humans, and ~60% of human genes are regulated
by miRNAs. Previous studies have demonstrated that there are a
large number of miRNAs existing in plasma (9), where they have different expression
profiles between lung cancer patients and normal healthy controls
(10). Other studies have
demonstrated that the abnormally expressed miRNAs may be used as
diagnostic markers for NSCLC (7,11).
However, studies using the abnormal expression of miRNAs in plasma
for early diagnosis of NSCLC are still lacking. In this study,
following a large number of relevant studies which have reported
the diagnostic value of miRNAs for NSCLC (7,11–14), we investigated the plasma levels of 10
miRNAs in the early stage of NSCLC patients using reverse
transcription-quantitative polymerase chain reaction (RT-qPCR). The
valuable diagnostic miRNAs were identified by receiver operating
characteristics (ROC) curve analysis, and are likely to improve the
diagnostic ability in early-stage NSCLC patients.
Materials and methods
Patients and ethics
All 232 participants were recruited from Shanghai
Chest Hospital, China, between July 2012 and May 2014. In the
training set, we selected 20 early-stage NSCLC patients and 20 age-
and gender-matched healthy controls to compare the expression
profile of candidate plasma miRNAs between NSCLC patients and
healthy controls. In the validation set, 109 early-stage NSCLC
patients and 63 healthy controls were recruited. To increase the
number of samples for validation, we merged the 40 cases of samples
in the screening stage with those in the validation stage. To
investigate whether the altered expression of the valuable
diagnostic miRNAs in plasma was of tumor origin, their expression
levels were measured in an independent set of 20 cases with
early-stage NSCLC. The inclusion criteria for NSCLC patients
included: i) no previous history of cancer-related diseases; ii)
did not receive radiotherapy or chemotherapy prior to surgery; iii)
diagnosed as NSCLC pathologically following surgery; iv) I and II
stages of NSCLC according to the tumor-node-metastasis (TNM)
staging guidelines of the American Joint Committee on Cancer (7th
version) (15). The inclusion
criterion for the healthy control group was that the individuals
were without tumor-associated lesions confirmed by chest CT, blood
test and other full body examinations. Samples were collected two
days after admission and 7 to 9 days after surgery. The collection
of samples was approved by the Medical Ethics Committee of Shanghai
Chest Hospital, Shanghai Jiaotong University. All patients and
healthy controls signed an informed consent form.
Sample processing and RNA
isolation
Whole blood (4 ml) was added to an ethylenediamine
tetraacetic acid (EDTA)-treated anticoagulant tube, and then plasma
was isolated by centrifugation at 1,200 rpm for 10 min and
subsequently at 12,000 rpm for 10 min at 4°C. A total of 400 µl
plasma was added to an equal volume of TRIzol. After putting on ice
for 5 min, 800 µl chloroform was added and incubated on ice for 5
min. Following centrifugation at 1,200 rpm for 10 min at 4°C, the
supernatant was collected. In order to obtain a suitable internal
control following the isolation of miRNAs, we added cel-miR-39
(Takara Biological Engineering Co., Ltd., Dalian, China) to the
supernatant as reported previously (9,12). The
synthetic sequences were from the miRBase database. Total RNA was
isolated using the mirVana PARIS kit following the manufacturer's
instructions (Ambion Life Technologies, Carlsbad, CA, USA). Total
RNA (100 µl) was collected from the filter by washing with
enzyme-free water (Shanghai Biological Engineering Co., Ltd.,
Shanghai, China), and then RNA concentration and purity were
measured using a NanoDrop ND-1000 (NanoDrop Technologies,
Wilmington, DE, USA).
Evaluation of internal controls for
quantification of plasma miRNAs
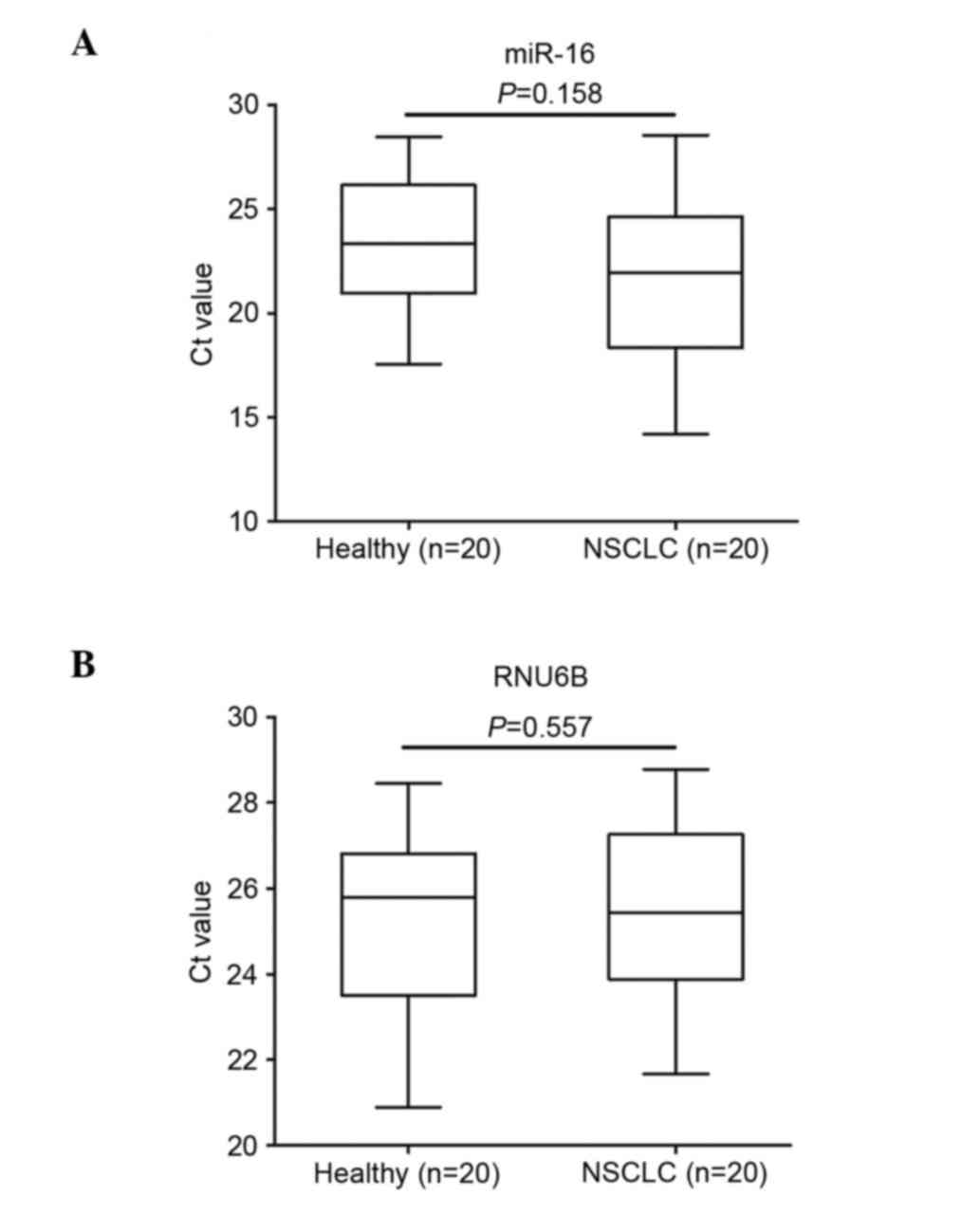
To select an appropriate internal control, we
examined the expression levels of miR-16 and RNU6B in the plasma of
20 cases of NSCLC patients and 20 age- and gender-matched healthy
individuals, as described previously (16–20). Using
the fixed volume approach, we added cel-miR-39 to each sample as a
control. In order to investigate the stability of the two potential
internal controls at room temperature, we randomly selected three
copies of plasma samples, and each one was divided into four parts.
These sample aliquots were maintained at room temperature for 0, 2,
4 and 8 h in nuclease-free tubes before being processed for RNA
isolation. Following quantification by RT-qPCR, PCR products were
randomly selected to analyze the sequence integrity by
electrophoresis.
RT-qPCR for miRNAs
Reverse transcription was performed using a TaqMan
microRNA reverse transcription kit (Ambion Life Technologies), and
qPCR was performed using a Brilliant III Ultra-Fast SYBR-Green qPCR
master mix kit (Ambion Life Technologies). RT-PCR was performed as
described previously by Kroh et al (18). PCR primers with a stem-loop structure
of each miRNA were designed based on the miRNA sequences obtained
from the miRBase database. The primers were synthesized by Shanghai
Biological Engineering Co., Ltd. (Table
I). We used the fixed volume approach for detection in the
reaction systems of reverse transcription and qPCR since the total
RNA concentration detected by the microspectrophotometer was very
low (~10 ng/µl). A total of 1.5 µl 10X RT-PCR buffer, 0.15 µl 100X
dNTP mixture, 1 µl 50 U/µl Multiscribe RT enzyme, 0.19 µl 20 U/µl
RNase inhibitor, 1 µl 10 µmol/l primer and 10 µl total RNA were
added to the reverse transcription system and made up to 15 µl
volume with diethylpyrocarbonate. The reaction conditions for
reverse transcription were 16°C for 30 min, 42°C for 30 min, 85°C
for 5 min and terminated at 4°C. The qPCR system (20 l) included
TaqMan 2X 10 µl Universal PCR master mix, 1 µl primers (final
concentration 200 nM) and 9 µl cDNA. The reaction was performed in
an ABI 7500 Real-Time PCR system (Ambion Life Technologies), and
the reaction conditions for qPCR were 95°C for 10 min, 40 cycles of
95°C for 15 sec and 60°C for 1 min. Three parallel samples and a
negative control were set. To check the integrity of the
amplification product, we used 3% agarose gel electrophoresis to
analyze and verify the specificity of the PCR product. Relative
expression levels were calculated using the 2−ΔΔCq
method (21), and miR-16 was used as
an internal control.
 | Table I.miRNA-specific primers. |
Table I.
miRNA-specific primers.
| Primer | Sequences
(5′-3′) |
|---|
| Cel-miR-39 |
TCACCGGGTGTAAATCAG |
| miR-30d |
CGCTGTAAACATCCCCGAC |
| miR-383 |
CGCAGATCAGAAGGTGATT |
| miR-16 |
GTAGCAGCACGTAAATATTGG |
| miR-20a |
CGCTAAAGTGCTTATAGTGC |
| miR-145 |
TGAACTTCGCAACTACCGTTTG |
| miR-21 |
CGCTAGCTTATCAGACTGA |
| miR-221 |
CGAGCTACATTGTCTGCTGGGT |
| miR-126 |
CGCTCGTACCGTGAGTAAT |
| miR-223 |
GCGGGTGTCAGTTTGTCAAATA |
| miR-25 |
CATTGCACTTGTCTCGGTCTG |
| miR-210 |
CGCAGCCCCTGCCCACCGC |
| RNU6B |
ACGCAAATTCGTGAAGCGTT |
Selection and validation of plasma
microRNA
In accordance with previous studies, we selected 10
miRNAs (miR-30d, miR-383, miR-20a, miR-145, miR-221, miR-25,
miR-223, miR-21, miR126 and miR-210) (7,11–14) and examined their expression using
RT-qPCR in a small set of plasma samples (20 NSCLC patients and 20
gender- and age-matched healthy controls). The upregulated markers
in NSCLC plasma were further validated in an independent
large-scale set of plasma from 109 NSCLC patients and 63 healthy
controls using RT-qPCR. The inclusion criteria were as mentioned
above. The effect of miRNAs in the early diagnosis of NSCLC was
analyzed by ROC curve. In order to observe whether the abnormally
expressed miRNAs are derived from tumor tissues, we collected the
plasma from 20 cases of early-stage NSCLC before and after surgery,
then examined the expression of miRNAs using RT-PCR.
Statistical analysis
Differences in miRNA levels between cases and
controls were assessed by the Mann-Whitney U test or the
Kruskall-Wallis test. The Chi-square test and one-way analysis of
variance were used to assess the difference in clinicopathological
characteristics and association between miRNA levels and
clinicopathological characteristics between cases and controls. The
multivariate logistic regression model was used to establish the
optimum regression equation and calculate the odds ratio and 95%
confidence interval for each variable. An ROC curve was established
to interpret the ability of miRNA in discriminating patients from
healthy controls. The area under the curve (AUC), sensitivity and
specificity at the optimal cut-off were computed in order to
validate the diagnostic application of these effective miRNAs as
cancer biomarkers. All P-values were shown bilaterally, and a value
less than 0.05 was considered to indicate a statistically
significant difference. Statistical analysis of the data was
performed using SPSS 18.0 software (SPSS Inc., Chicago, IL, USA)
and graphs were generated using GraphPad Prism 6.0 (GraphPad
Software, Inc., La Jolla, CA, USA).
Results
Clinical characteristics of study
population
There were 149 NSCLC patients and 83 healthy
controls (Table II). In the training
set, there were 20 patients in the NSCLC group and 20 healthy
individuals in the control group (gender and age were matched in
the two groups). At the verification stage, there were 109 NSCLC
patients and 63 healthy controls. There were no significant
differences in the mean age, gender and smoking history between the
two groups (P>0.05). The peripheral blood was collected from 20
early-stage NSCLC patients and the expression levels of miRNAs were
investigated before and after surgery (Table II).
 | Table II.Clinical characteristics of NSCLC
patients and healthy controls (cases, %). |
Table II.
Clinical characteristics of NSCLC
patients and healthy controls (cases, %).
|
| Training set | Validation set |
|
|---|
|
|
|
|
|
|---|
| Category | Control (n=20) | NSCLC (n=20) | P | Control (n=63) | NSCLC (n=109) | P | Pre- and
post-surgery (n=20) |
|---|
| Gender |
|
| 1 |
|
| 0.525 |
|
|
Male | 12 (60) | 12 (60) |
| 36 (57.1) | 69 (63.3) |
| 13 (65) |
|
Female | 8
(40) | 8
(40) |
| 27 (42.9) | 40 (36.7) |
| 7 (45) |
| Age (year) |
|
| 1 |
|
| 0.539 |
|
|
<60 | 9
(45) | 9
(45) |
| 31 (49.2) | 47 (43.1) |
| 8 (40) |
|
>60 | 11 (55) | 11 (55) |
| 32 (40.8) | 62 (56.9) |
| 12 (60) |
| Mean age
(year) | 61.7+8.8 | 61.0+8.1 | 0.749 | 59.7+8.0 | 59.3+9.0 | 0.783 | 61.4+8.3 |
| Smoking
statusa |
|
| 0.747 |
|
| 0.064 |
|
|
Yes | 11 (55) | 13 (65) |
| 27 (42.9) | 64 (58.7) |
| 13 (65) |
| No | 9
(45) | 7
(35) |
| 36 (57.1) | 45 (41.3) |
| 7 (45) |
| TNM stage |
|
|
|
|
|
|
|
| I |
| 7
(35) |
|
| 48 (44.0) |
| 6 (30) |
| II |
| 13 (65) |
|
| 61 (56.0) |
| 14 (70) |
| Pathological
type |
|
|
|
|
|
|
|
|
Adenocarcinoma |
| 9
(45) |
|
| 49 (45.0) |
| 11 (55) |
|
Squamous cell carcinoma |
| 11 (55) |
|
| 42 (38.5) |
| 9 (45) |
|
Other |
|
|
|
| 18 (16.5) |
|
|
Evaluation of potential internal
control for quantification of plasma miRNA
To identify an internal control that is capable of
reliably quantifying the expression of the target miRNAs in plasma,
we examined the levels of miR-16 and RNU6B using RT-qPCR in plasma
samples of 20 NSCLC patients and 20 healthy controls. To normalize
the difference in extraction efficiency and reverse transcription
efficiency among the different samples, the plasma levels of miR-16
and RNU6B were compared with spiked-in cel-miR-39. No significant
difference was observed in the levels of miR-16 (P=0.158) and RNU6B
(P=0.557) between the NSCLC patients and healthy controls (Fig. 1). To examine the stability of the two
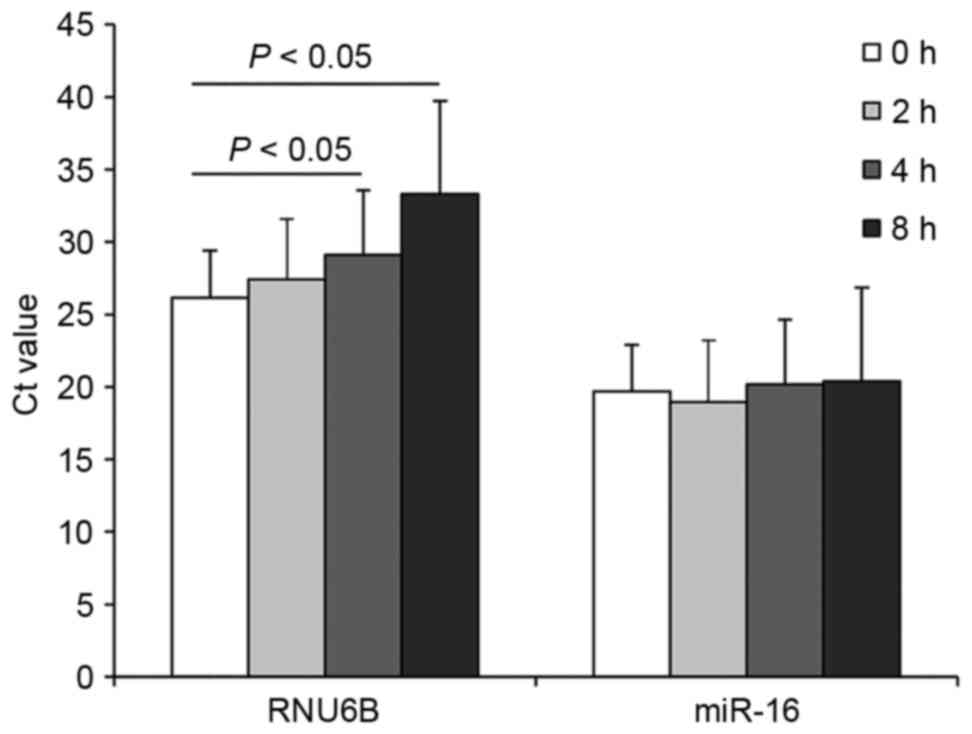
internal controls, we measured the levels in the samples prepared
at various time points. We randomly selected three copies of plasma
from the 20 NSCLC cases and 20 controls (each was divided into four
parts). Total RNA was isolated and quantified after the samples had
been kept at room temperature for 0, 2, 4 and 8 h. We observed that
miR-16 was relatively stable at room temperature, and there were no
significant differences in the expression of miR-16 among the
samples kept at room temperature for 0, 2, 4 and 8 h (P>0.05,
Fig. 2). However, the expression
levels of RNU6B were significantly different when the samples were
kept at room temperature for 4 and 8 h (P<0.05, Fig. 2). Together, the observations indicated
that miR-16 exhibited higher stability and abundance than RNU6B in
plasma. Therefore, we selected miR-16 as the normalization control
to determine the expression of the 10 miRNAs in the present
study.
Evaluation of 10 candidate miRNAs as
biomarkers for NSCLC screening in training set
To screen the potential upregulated miRNAs, we first
examined the expression levels of 10 candidate miRNAs (miR-30d,
miR-383, miR-20a, miR-145, miR-221, miR-25, miR-223, miR-21,
miR-126 and miR-210) based on previous studies (7,11–14) using RT-qPCR in 40 plasma samples (20
NSCLC cases and 20 controls). We observed that the expression of
four miRNAs in the plasma of NSCLC patients was more than two-fold
higher than that in the healthy control group (Table III, P<0.05). miRNA-383 was not
detectable in the plasma (Ct value>35). There were no
significant differences in the expression of miR-221, miR-25 and
miR-30d in the plasma of NSCLC patients and healthy controls
(P>0.05). The expression levels of miR-126 and miR-210 were
slightly decreased in the plasma of NSCLC patients, but there was
no significant difference between the cases and controls
(P>0.05).
 | Table III.Expression levels of 10 plasma miRNAs
between 20 NSCLC patients and 20 healthy controls (mean ± SD). |
Table III.
Expression levels of 10 plasma miRNAs
between 20 NSCLC patients and 20 healthy controls (mean ± SD).
| miRNAs | Expression | NSCLC/healthy
(fold) | P-value |
|---|
| miR-145 | ↑ | 21.67+0.89 |
2.04×10−4 |
| miR-20a | ↑ | 13.39+1.02 |
9.22×10−5 |
| miR-21 | ↑ | 6.15+0.49 |
3.72×10−4 |
| miR-223 | ↑ | 2.64+0.39 |
1.48×10−3 |
| miR-221 | ↑ | 1.37+0.31 | 0.0612 |
| miR-25 | ↑ | 1.23+0.28 | 0.7510 |
| miR-30d | ↑ | 1.13+0.29 | 0.3326 |
| miR-126 | ↓ | 0.93+0.27 | 0.3942 |
| miR-210 | ↓ | 0.62+0.16 | 0.1195 |
| miR-383 | / | / | / |
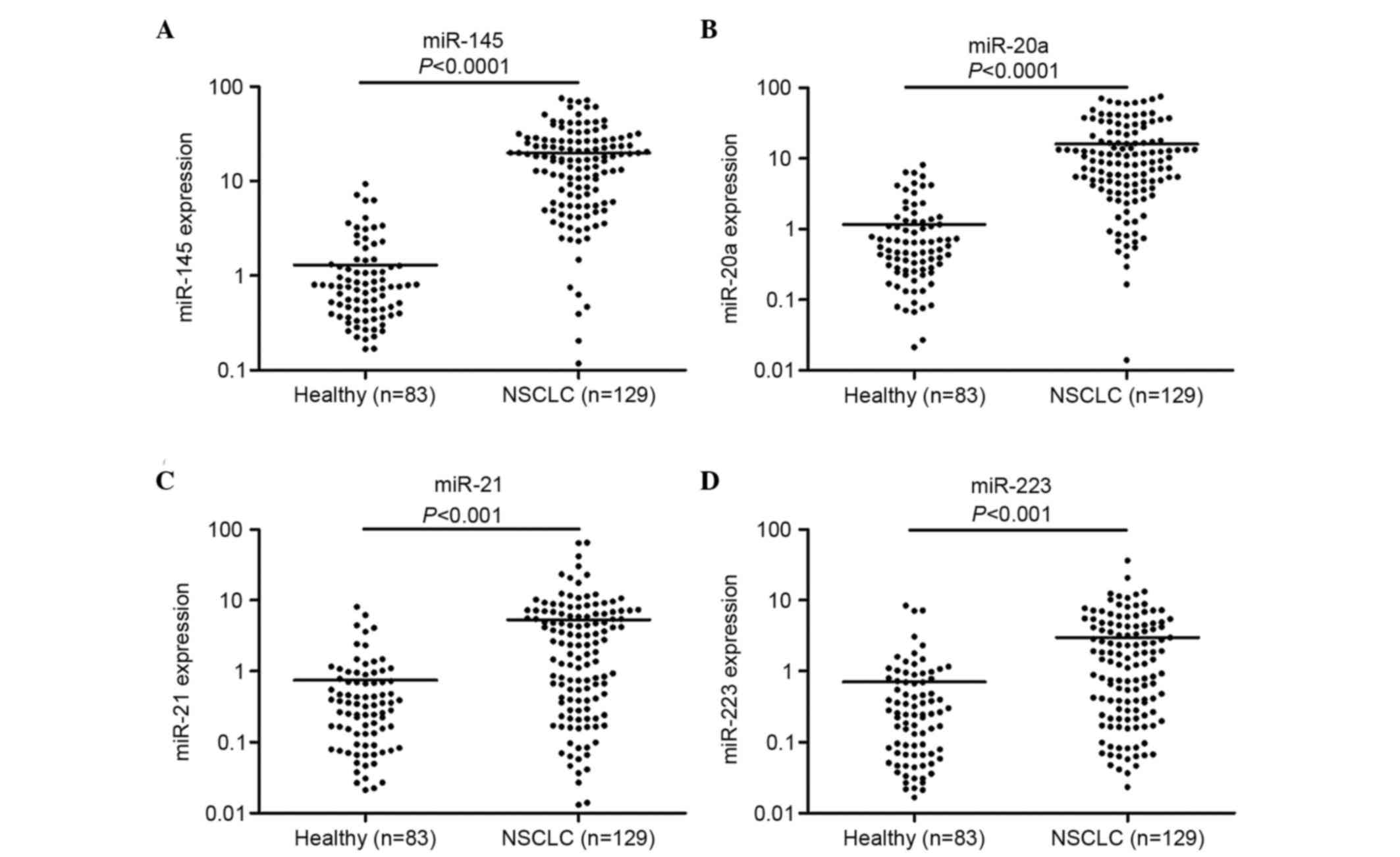
miRNA validation and ROC curve
analysis
In order to increase the number of samples for
validation, we merged the 40 cases of samples in the screening
stage with those in the validation stage, making 129 cases of NSCLC
patients and 83 healthy individuals. Following detection by RT-PCT,
we observed that the expression of miR-145, miR-20a, miR-21 and
miR-223 in the plasma of NSCLC patients was significantly enhanced
compared with that of the healthy controls (Fig. 3). ROC curve analysis revealed that
these four miRNAs distinguished NSCLC patients from healthy
individuals (Fig. 4). The AUCs of
miR-145, miR-20a, miR-21 and miR-223 were 0.886 (95% CI,
0.835–0.925), 0.889 (95% CI, 0.839–0.928), 0.838 (95% CI,
0.782–0.885) and 0.809 (95% CI, 0.749–0.860), respectively. Their
optimum cut-off point was 4.086, 2.428, 1.101 and 1.020,
respectively, and the sensitivity and specificity at this cut-off
point were 80.6 and 89.2%; 79.8 and 88.0%; 77.5 and 85.5%; and 69.8
and 84.3%, respectively. Multivariate logistic regression analyses
on variables including gender, age, smoking history and plasma
miRNAs revealed that plasma miR-145, miR-20a, miR-21 and miR-223
were potential biomarkers for early-stage NSCLC diagnosis. The odds
ratios of miR-145, miR-20a, miR-21 and miR-223 were 18.5 (95% CI,
7.410–45.649), 16.0 (95% CI, 6.516–43.810), 13.0 (95% CI,
5.570–36.219) and 11.0 (95% xCI, 4.516–30.629), respectively. The
panel of miR-145, miR-20a, miR-21 and miR-223 had the highest
predictive accuracy in early-stage NSCLC screening (Fig. 5). The AUC, optimum cut-off point,
sensitivity and specificity of this combination were 0.897 (95% CI,
0.875–0.917), 1.485, 81.8 and 90.1%, respectively.
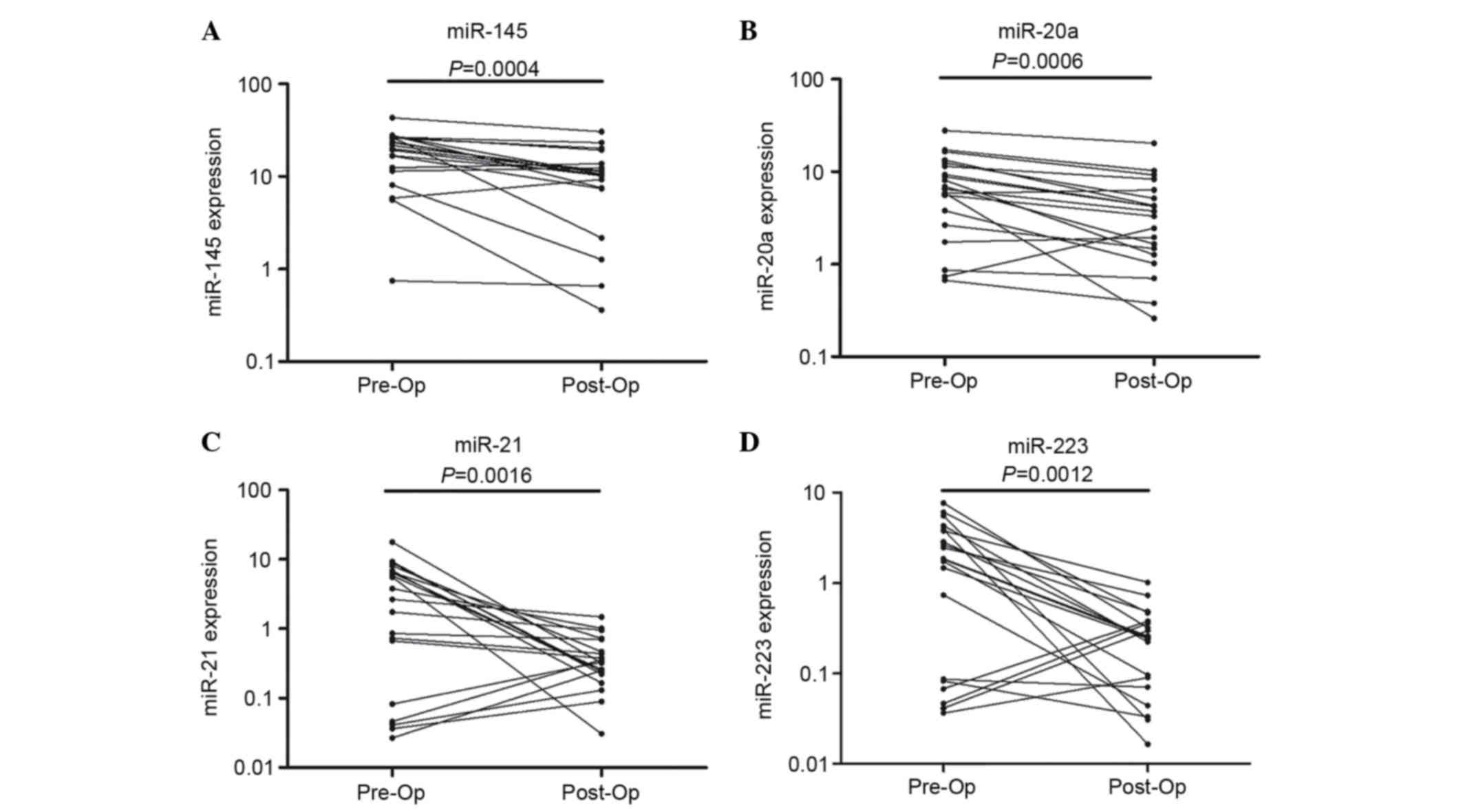
Expression levels of plasma miRNAs
before and after surgery
To investigate whether the plasma miR-145, miR-20a,
miR-21 and miR-223 were of tumor origin, we collected plasma
samples from an independent set of 20 early-stage NSCLC patients,
and then examined the plasma expression levels of these four miRNAs
before and after surgery with RT-qPCR. We observed that the
expression of these four miRNAs was significantly decreased in the
post-operative patients compared with the pre-operative patients
(Fig. 6).
Discussion
Lung cancer is a major global health problem. Due to
the high level of incidence and low therapeutic efficacy, it has
become the leading cause of malignancy-related mortality in
numerous countries (22). Late
diagnosis of lung cancer is one of the significant contributing
factors to the high mortality of this disease since the tumor has
often spread to distant organs at the time of diagnosis (23). Conventional diagnostic methods,
including CT, positron emission tomography and X-ray, have several
limitations. CT screening has a relatively high false positive
rate, and benign lung nodules may be misdiagnosed as malignant
tumors (24). Several protein
biomarkers have been identified as non-invasive and cost-effective
diagnostic tools for early-stage NSCLC, which have limited
sensitivity and specificity, including cytokeratin fragment 21-1
(sensitivity≈0.5, specificity≈0.95), tissue polypeptide-specific
antigen (sensitivity≈0.34, specificity≈0.95) and carcinoembryonic
antigen (sensitivity≈0.53, specificity≈0.95) (25,26).
Therefore, developing novel non-invasive biomarkers by taking
advantage of recent developments in molecular genetics for the
screening of early-stage NSCLC is of clinical significance.
Accumulating studies suggest that circulating miRNAs
may be used as potential molecular biomarkers for several disease
conditions, including human malignancies (27–29). Chen
et al reported that the expression profiles of plasma miRNAs
in lung cancer, colorectal cancer and diabetic patients are
different from those of healthy individuals, and proposed that
miR-25 and miR-223 may be used as diagnostic markers for NSCLC
(12). In 2011, Chen et al
further studied the function of plasma miRNAs as diagnostic markers
for NSCLC, and identified that 10 miRNAs may potentially be used as
diagnostic markers, with the sensitivity and specificity of the
combined use of these 10 miRNAs reaching 93 and 90%, respectively
(7). Shen et al revealed that
miR-21, miR-126, miR-210 and miR-486-5p may be used as diagnostic
markers for stage I NSCLC, and the sensitivity and specificity of
the combined use of these four miRNAs were 73.33 and 96.55%,
respectively (11). Foss et al
demonstrated that plasma miR-1254 and miR-574-5p serve as
non-invasive screening tools in the early detection of NSCLC with
relatively high accuracy (30).
Subsequently, an increasing number of studies have investigated the
diagnostic value of miRNAs for early-stage lung cancer (7). Compared with these previous studies, the
present study has several advantages. Firstly, we concentrated on
the detection of early-stage NSCLC by using miRNAs as biomarkers,
and observed that plasma miR-145, miR-20a, miR-21 and miR-223 may
be used as biomarkers for the early detection of NSCLC with
relatively high sensitivity and specificity. Secondly,
normalization is a key step for the accurate quantification of RNA
levels with RT-qPCR. Our results revealed that RNU6B is unstable at
room temperature. miR-16 exhibited a higher stability and abundance
than RNU6B in plasma. Finally, we demonstrated that the expression
of plasma miR-145, miR-20a, miR-21 and miR-223 was significantly
decreased in the postoperative plasma samples when compared with
the preoperative samples. To our knowledge, the present study is
the first to evaluate the expression levels of plasma miRNAs before
and after surgery.
In the present study, we observed that miR-145,
miR-20a, miR-21 and miR-223 were significantly dysregulated in
NSCLC patients compared with healthy controls. The data from our
study demonstrated that each single miRNA presents high sensitivity
and specificity in the detection process. Despite the different
expression levels, all four of these miRNAs were validated to have
the potential to discriminate early-stage NSCLC patients from
healthy controls. The panel of four candidate miRNAs demonstrated
the highest predictive accuracy in NSCLC detection (AUC=0.897). We
also analyzed the expression levels of plasma miRNAs before and
after surgery, and observed that the levels of the four candidate
miRNAs decreased rapidly following surgical removal of the tumors.
Collectively, miR-145, miR-20a, miR-21 and miR-223 presented great
clinical value in NSCLC preliminary screening, and further studies
in a large population are required to validate the feasibility of
these miRNAs as novel non-invasive biomarkers.
Upregulation of miR-21 has been observed in numerous
human cancers (31). Capodanno et
al previously revealed that miR-21 expression was significantly
increased in NSCLC tissues, and may be used to distinguish NSCLC
from non-cancerous lung tissues (32). Furthermore, high expression of miR-21
predicts recurrence and unfavorable survival in non-small cell lung
cancer (33). The data produced from
the present study imply that plasma miR-21 may serve as a biomarker
for the diagnosis of lung cancer. miR-20a inhibits E2F1, which is a
transcription factor associated with lung cancer cell growth, and
it serves as a non-invasive screening tool for early detection of
lung cancer (34). miR-145 inhibits
proliferation of NSCLC cells by targeting c-Myc (35) and plays an inhibitory role in tumor
angiogenesis, cell growth and invasion and tumor growth through
post-transcriptional regulation through N-RAS and vascular
endothelial growth factor-A in breast cancer (36). However, conclusions from several
studies which focused on the serum expression of miR-145 were
inconsistent. These included studies in breast cancer (37,38). As
for miR-223, scientists have proven that miR-223 functions as a
tumor suppressor in lung cancer cells at multiple steps of
tumorigenesis and progression (39,40), which
serves as reasonable explanation for the function of miR-223 as an
NSCLC biomarker.
In our study, we also noted that the expression
levels of these four miRNAs were significantly different before and
7–10 days after the surgery in early-stage NSCLC patients. However,
it is not known what causes this change, and additional studies are
required to clarify this.
In this study, we have demonstrated that these four
miRNAs in plasma had dysregulated expression in NSCLC, suggesting
that they may serve as biomarkers in precise clinical diagnosis of
early-stage NSCLC. However, certain limitations in our tests need
to be addressed. In the training set, there were only 10 miRNAs
included in our study. Further studies are required to expand the
investigation number of miRNAs. Secondly, the changes in the miRNA
expression level before and after surgery need to be verified using
a larger sample. The selection of reference gene is a crucial step
for accurate quantification by RT-PCR. However, there is still no
well-recognized reference gene for miRNA quantification in plasma.
In this study, we selected miR-16 and RNU6B as candidate reference
genes and observed no significant difference between them in
early-stage NSCLC patients and healthy individuals. However, RNU6B
was not stable at room temperature; therefore, we selected miR-16
as the internal reference, and this was also supported by previous
studies (16,19,41,42).
Further studies are still required to identify and validate more
suitable reference genes to study circulating miRNAs in early-stage
NSCLC patients, and thus provide more accurate results for
RT-PCR.
In summary, miR-145, miR-20a, miR-21 and miR-223
appear to be novel biomarkers for early detection of early-stage
NSCLC. However, other miRNAs that could function as biomarkers for
the early diagnosis of NSCLC may also exist in plasma, therefore
further studies are required to screen more suitable miRNAs, and
thus improve the diagnostic ability for early-stage NSCLC
patients.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ettinger DS, Akerley W, Bepler G, Blum MG,
Chang A, Cheney RT, Chirieac LR, D'Amico TA, Demmy TL, Ganti AK, et
al: Non-small cell lung cancer. J Natl Compr Canc Netw. 8:740–801.
2010.PubMed/NCBI
|
|
3
|
Crinò L, Weder W, van Meerbeeck J and
Felip E: ESMO Guidelines Working Group: Early stage and locally
advanced (non-metastatic) non-small-cell lung cancer: ESMO Clinical
Practice Guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 21:(Suppl 5). v103–v115. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Swensen SJ, Jett JR, Hartman TE, Midthun
DE, Mandrekar SJ, Hillman SL, Sykes AM, Aughenbaugh GL, Bungum AO
and Allen KL: CT screening for lung cancer: five-year prospective
experience. Radiology. 235:259–265. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Boeri M, Verri C, Conte D, Roz L, Modena
P, Facchinetti F, Calabrò E, Croce CM, Pastorino U and Sozzi G:
MicroRNA signatures in tissues and plasma predict development and
prognosis of computed tomography detected lung cancer. Proc Natl
Acad Sci USA. 108:3713–3718. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen X, Hu Z, Wang W, Ba Y, Ma L, Zhang C,
Wang C, Ren Z, Zhao Y, Wu S, et al: Identification of ten serum
microRNAs from a genome-wide serum microRNA expression profile as
novel non-invasive biomarkers for nonsmall cell lung cancer
diagnosis. Int J Cancer. 130:1620–1628. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee RC, Feinbaum RL and Ambros V: The C.
elegans heterochronic gene lin-4 encodes small RNAs with antisense
complementarity to lin-14. Cell. 75:843–854. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mitchell PS, Parkin RK, Kroh EM, Fritz BR,
Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O'Briant
KC, Allen A, et al: Circulating microRNAs as stable blood-based
markers for cancer detection. Proc Natl Acad Sci USA.
105:10513–10518. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Keller A, Leidinger P, Gislefoss R, Haugen
A, Langseth H, Staehler P, Lenhof HP and Meese E: Stable serum
miRNA profiles as potential tool for non-invasive lung cancer
diagnosis. RNA Biol. 8:506–516. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shen J, Todd NW, Zhang H, Yu L, Lingxiao
X, Mei Y, Guarnera M, Liao J, Chou A, Lu CL, et al: Plasma
microRNAs as potential biomarkers for non-small-cell lung cancer.
Lab Invest. 91:579–587. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K,
Guo J, Zhang Y, Chen J, Guo X, et al: Characterization of microRNAs
in serum: a novel class of biomarkers for diagnosis of cancer and
other diseases. Cell Res. 18:997–1006. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Boeri M, Verri C, Conte D, Roz L, Modena
P, Facchinetti F, Calabrò E, Croce CM, Pastorino U and Sozzi G:
MicroRNA signatures in tissues and plasma predict development and
prognosis of computed tomography detected lung cancer. Proc Natl
Acad Sci USA. 108:3713–3718. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Silva J, Garcia V, Zaballos Á, Provencio
M, Lombardía L, Almonacid L, García JM, Domínguez G, Peña C, Diaz
R, et al: Vesicle-related microRNAs in plasma of nonsmall cell lung
cancer patients and correlation with survival. Eur Respir J.
37:617–623. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tsim S, O'Dowd CA, Milroy R and Davidson
S: Staging of non-small cell lung cancer (NSCLC): a review. Respir
Med. 104:1767–1774. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wong TS, Liu XB, Wong BY, Ng RW, Yuen AP
and Wei WI: Mature miR-184 as potential oncogenic microRNA of
squamous cell carcinoma of tongue. Clin Cancer Res. 14:2588–2592.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang Z, Huang D, Ni S, Peng Z, Sheng W
and Du X: Plasma microRNAs are promising novel biomarkers for early
detection of colorectal cancer. Int J Cancer. 127:118–126. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kroh EM, Parkin RK, Mitchell PS and Tewari
M: Analysis of circulating microRNA biomarkers in plasma and serum
using quantitative reverse transcription-PCR (qRT-PCR). Methods.
50:298–301. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu CJ, Kao SY, Tu HF, Tsai MM, Chang KW
and Lin SC: Increase of microRNA miR-31 level in plasma could be a
potential marker of oral cancer. Oral Dis. 16:360–364. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tsujiura M, Ichikawa D, Komatsu S,
Shiozaki A, Takeshita H, Kosuga T, Konishi H, Morimura R, Deguchi
K, Fujiwara H, et al: Circulating microRNAs in plasma of patients
with gastric cancers. Br J Cancer. 102:1174–1179. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Russ R and Slack FJ:
Cigarette-smoke-induced dysregulation of MicroRNA expression and
its role in lung carcinogenesis. Pulm Med. 2012:7912342012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wu X, Piper-Hunter MG, Crawford M, Nuovo
GJ, Marsh CB, Otterson GA and Nana-Sinkam SP: MicroRNAs in the
pathogenesis of lung cancer. J Thorac Oncol. 4:1028–1034. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Swensen SJ, Jett JR, Sloan JA, Midthun DE,
Hartman TE, Sykes AM, Aughenbaugh GL, Zink FE, Hillman SL, Noetzel
GR, et al: Screening for lung cancer with low-dose spiral computed
tomography. Am J Respir Crit Care Med. 165:508–513. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wieskopf B, Demangeat C, Purohit A,
Stenger R, Gries P, Kreisman H and Quoix E: Cyfra 21-1 as a
biologic marker of non-small cell lung cancer. Evaluation of
sensitivity, specificity, and prognostic role. Chest. 108:163–169.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nisman B, Lafair J, Heching N, Lyass O,
Baras M, Peretz T and Barak V: Evaluation of tissue polypeptide
specific antigen, CYFRA 21-1, and carcinoembryonic antigen in
nonsmall cell lung carcinoma: does the combined use of cytokeratin
markers give any additional information? Cancer. 82:1850–1859.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Andersen M, Grauslund M, Ravn J, Sørensen
JB, Andersen CB and Santoni-Rugiu E: Diagnostic potential of
miR-126, miR-143, miR-145, and miR-652 in malignant pleural
mesothelioma. J Mol Diagn. 16:418–430. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zheng H, Zhang L, Zhao Y, Yang D, Song F,
Wen Y, Hao Q, Hu Z, Zhang W and Chen K: Plasma miRNAs as diagnostic
and prognostic biomarkers for ovarian cancer. PLoS One.
8:e778532013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang RJ, Zheng YH, Wang P and Zhang JZ:
Serum miR-125a-5p, miR-145 and miR-146a as diagnostic biomarkers in
non-small cell lung cancer. Int J Clin Exp Pathol. 8:765–771.
2015.PubMed/NCBI
|
|
30
|
Foss KM, Sima C, Ugolini D, Neri M, Allen
KE and Weiss GJ: miR-1254 and miR-574-5p: serum-based microRNA
biomarkers for early-stage non-small cell lung cancer. J Thorac
Oncol. 6:482–488. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Volinia S, Calin GA, Liu CG, Ambs S,
Cimmino A, Petrocca F, Visone R, Iorio M, Roldo C, Ferracin M, et
al: A microRNA expression signature of human solid tumors defines
cancer gene targets. Proc Natl Acad Sci USA. 103:2257–2261. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Capodanno A, Boldrini L, Proietti A, Alì
G, Pelliccioni S, Niccoli C, D'Incecco A, Cappuzzo F, Chella A,
Lucchi M, et al: Let-7g and miR-21 expression in non-small cell
lung cancer: correlation with clinicopathological and molecular
features. Int J Oncol. 43:765–774. 2013.PubMed/NCBI
|
|
33
|
Yang M, Shen H, Qiu C, Ni Y, Wang L, Dong
W, Liao Y and Du J: High expression of miR-21 and miR-155 predicts
recurrence and unfavourable survival in non-small cell lung cancer.
Eur J Cancer. 49:604–615. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
O'Donnell KA, Wentzel EA, Zeller KI, Dang
CV and Mendell JT: c-Myc-regulated microRNAs modulate E2F1
expression. Nature. 435:839–843. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chen Z, Zeng H, Guo Y, Liu P, Pan H, Deng
A and Hu J: miRNA-145 inhibits non-small cell lung cancer cell
proliferation by targeting c-Myc. J Exp Clin Cancer Res.
29:1512010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zou C, Xu Q, Mao F, Li D, Bian C, Liu LZ,
Jiang Y, Chen X, Qi Y, Zhang X, et al: MiR-145 inhibits tumor
angiogenesis and growth by N-RAS and VEGF. Cell Cycle.
11:2137–2145. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
37
|
Mar-Aguilar F, Mendoza-Ramirez JA,
Malagón-Santiago I, Espino-Silva PK, Santuario-Facio SK,
Ruiz-Flores P, Rodríguez-Padilla C and Reséndez-Pérez D: Serum
circulating microRNA profiling for identification of potential
breast cancer biomarkers. Dis Markers. 34:163–169. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ng EK, Li R, Shin VY, Jin HC, Leung CP, Ma
ES, Pang R, Chua D, Chu KM, Law WL, et al: Circulating microRNAs as
specific biomarkers for breast cancer detection. PLoS One.
8:e531412013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Haneklaus M, Gerlic M, O'Neill LA and
Masters SL: miR-223: infection, inflammation and cancer. J Intern
Med. 274:215–226. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Nian W, Ao X, Wu Y, Huang Y, Shao J, Wang
Y, Chen Z, Chen F and Wang D: miR-223 functions as a potent tumor
suppressor of the Lewis lung carcinoma cell line by targeting
insulin-like growth factor-1 receptor and cyclin-dependent kinase
2. Oncol Lett. 6:359–366. 2013.PubMed/NCBI
|
|
41
|
Lawrie CH, Gal S, Dunlop HM, Pushkaran B,
Liggins AP, Pulford K, Banham AH, Pezzella F, Boultwood J,
Wainscoat JS, et al: Detection of elevated levels of
tumour-associated microRNAs in serum of patients with diffuse large
B-cell lymphoma. Br J Haematol. 141:672–675. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Heneghan HM, Miller N, Lowery AJ, Sweeney
KJ, Newell J and Kerin MJ: Circulating microRNAs as novel minimally
invasive biomarkers for breast cancer. Ann Surg. 251:499–505. 2010.
View Article : Google Scholar : PubMed/NCBI
|