Introduction
Lung cancer is one of the most malignant tumors that
are frequently seen in clinical practice. It is associated with an
extremely high morbidity rate and mortality rate. Lung cancer ranks
first among general malignant tumors, which can severely threaten
the physical health of human beings (1). Lung cancer can be categorized into small
cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
NSCLC composes almost 80% of the lung cancer cases (2). Various treatment methods have been
developed for NSCLC, including surgeries, chemotherapy and
radiotherapy, in which surgeries have been considered as the
preferred choice for treatment of NSCLC in the early stage. After
surgeries, 50–80% patients experience a 5-year survival period
(3,4).
With an advancement of medical techniques and instruments,
thoracoscope-assisted segmental resection of lungs have become the
major method in the surgical treatment of lung cancer, and shows
excellent efficacy, particularly for the elderly patients or
patients with poor cardiac or pulmonary functions (5). In this study, we performed
thoracoscope-assisted segmental resection of lung for patients with
NSCLC at the early stage, and observed the short- and long-term
efficacy to provide a reference for the surgical treatment of NSCLC
at the early stage.
Materials and methods
Sample selection
We selected a total of 86 patients with NSCLC that
were admitted to The First People's Hospital of Xuzhou for
treatment between December 2010 and December 2011. Using a random
number table, we divided them in to the control group (n=43) and
the observation group (n=43). The inclusion criteria included: a)
Patients that were diagnosed with NSCLC at the early stage
according to results of computed tomography (CT) and pathological
examinations, b) patients with the peripheral nodule diameters ≤2
cm, c) patients without any history of surgery, chemotherapy or
radiotherapy, and d) patients who signed the informed consent form.
Exclusion criteria included, a) patients with abnormal coagulation
function, b) patients with NSCLC above stage III A, c) patients
with a history of thoracic surgeries, or with lymph node metastasis
in hilum of lung and mediastinum or distant metastasis. Comparison
of the baseline characteristics of patients between the two groups
showed no statistically significant differences (P>0.05;
Table I). The study was approved by
the Ethics Committee of The First People's Hospital of Xuzhou.
 | Table I.Comparison of general materials of
patients between the two groups. |
Table I.
Comparison of general materials of
patients between the two groups.
| Characteristics | Control group
(n=47) | Observation group
(n=47) |
t-value/χ2 | P-value |
|---|
| Sex
(male/female) | 29/18 | 27/20 | 0.044 | 0.836 |
| Age (years) | 40–75 | 40–78 |
|
|
| Average age
(years) | 57.69±7.69 | 58.24±7.53 | 0.350 | 0.727 |
| Smoking (n, %) |
|
|
|
|
| Cigarette
amount ≥5 | 19 (40.43) | 16 (34.04) | 0.325 | 0.850 |
| Cigarette
amount <5 | 9
(19.15) | 10 (21.28) |
|
|
| No
smoking | 19 (40.43) | 21 (44.68) |
|
|
Pre-surgery preparation
Routine examinations were carried out before surgery
for patients to exclude surgical contradiction and ascertain the
optimal surgical time. At 2 weeks before surgery, patients were
required to quit smoking. Food and water was withdrawn at 8 h
before surgery.
Treatment
All patients received general intravenous anesthesia
with trachea cannula in the lateral position. During surgery, the
arterial blood gases, arterial blood pressure, pulse and
electrocardiography were monitored. Patients in the control group
received conventional thoracic surgery in following procedures.
After the sterile drape was covered on the surgical site, the
lateral approach was prepared for opening the chest layer by layer.
The mediastinal lymph nodes were resected followed by a routine
resection of lobes of the lung. Warm saline was used to rinse the
thoracic cavity after the surgery, and the air leakage was examined
in the lung. The residual bronchial ends with the drainage tube
being detained into the chest. The incision was closed through
suturing.
In the observation group, patients received the
thoracoscope-assisted segmental resection of lung through 3 ports:
The observation port was prepared in the 7th and 8th intercostal
space along the midline of the lateral axillary, which is
approximately 1 cm. The main operation port was located in the
intercostal space between the 4th and 5th rib along the anterior
axillary line, which is approximately 3 cm. The auxiliary operation
port in the 8th intercostal space along the infrascapular line,
which is approximately 1 cm. Under the view of video, the resection
of different pulmonary segments was performed with the lymph nodes
being resected. After surgery, surgeons examined the dilation of
residual lung, air leakage in lung or the residual bronchial end.
The drainage tube was inserted into the thoracic cavity followed by
suture of incision.
Indicators of detection
Before surgery and at 1 week after surgery, we
collected 5 ml of fasting peripheral venous blood from the patients
in both groups, and the samples were used for enzyme-linked
immunosorbent assay ELISA to determine levels of interleukin 6
(IL-6), interleukin 8 (IL-8) and tumor necrosis factor-α (TNF-α).
The appropriate kits were purchased from Beijing Biolab Science and
Technology Co. Ltd. (Beijing, China) and the procedures were
conducted in strict accordance with the manufacturer's
instructions. The levels of IL-6, IL-8 and TNF-α were calculated
using optical density (OD) values at a wavelength of 450 nm,
detected by a microplate reader (Jiangsu Potebio Biotechnology Co.,
Ltd., Jiangsu, China). With kits purchased from Zhejiang Ikon
Biotechnology Co., Ltd. (Zhejiang, China), immunoturbidimetry was
conducted to detect levels of IgG, IgA and IgM in serum of patients
in strict accordance with the instructions of the kit. The
turbidity of the reaction solution was used to detect the content
of IgG, IgA and IgM in samples with the standard substance as a
reference. In the samples, CD3+, CD4+ and
CD8+ antibodies were added, respectively, and then
incubated for 30 min in the dark at 4°C. Flow cytometer (BD, USA)
was used to detect levels of T lymphocyte subgroups
(CD3+, CD4+ and CD8+).
Evaluation indicators
We compared the surgical efficacy of patients
between the groups, including the intraoperative bleeding volume
and the number of resected lymph nodes. After surgery, pain was
evaluated using a visual analogue scale (VAS) within the range of
scores between 0 and 10 points (0 point for no pain, and 10 points
for intolerable acute pain). The comparison of postoperative
complications was also conducted through recording the incidence
rates of hyperthermia, persistent air leakage, cardiac arrhythmia,
and pulmonary atelectasis.
Before surgery and at 1 week after surgery, 5 ml of
fasting venous blood was drawn from patients in the morning who had
been fasting for 8 h. The samples were used for detecting the
levels of IL-6, IL-8 and TNF-α in serum of patients through ELISA.
Immunoturbidimetry was conducted to measure the levels of IgG, IgA
and IgM, and the levels of T lymphocyte subgroups (CD3+,
CD4+, CD8+ and
CD4+/CD8+) were detected using flow
cytometry. Before surgery and at 3 months post-surgery, we examined
the cardiac and pulmonary functions of patients, including the
following indicators: heart rate (HR), forced expiratory volume in
one second (FEV1), maximal voluntary ventilation (MVV) and carbon
monoxide-diffusing capacity (DLCO).
During the 5-year follow-up, we collected statistics
of recurrence rate, disease-free survival (DFS) and 5-year survival
rate, in which the DFS was defined from the 1st day after surgery
to the day of first onset of recurrence or metastasis, and 5-year
survival was defined as the patients had no recurrence or
metastasis within the 5-year follow-up.
Statistical analysis
SPSS 19.0 (SPSS Inc., Chicago, IL, USA) was used to
perform data processing. Measurement data are presented as mean ±
standard deviation, and t-test was performed for intergroup
comparison. The count data were presented as a rate, and a
Chi-square test was performed for comparison of countable data. The
Kaplan-Meier curve was applied in the survival analysis. P<0.05
was considered to indicate a statistically significant
difference.
Results
Comparison of surgical efficacy of
patients between the groups
In the observation group, the intraoperative
bleeding volume of patients was significantly less than that in the
control group. In addition, the surgical duration was respectively
short and the postoperative pain was alleviated compared to the
control group (P<0.05). There were no statistically significant
differences in comparison of the number of resected lymph nodes of
patients between the groups (P>0.05; Table II).
 | Table II.Comparison of surgical condition of
patients between the two groups. |
Table II.
Comparison of surgical condition of
patients between the two groups.
| Group | Case | Surgical duration
(min) | Intraoperative
bleeding amount (ml) | Number of resected
lymph nodes (n) | Score of
postoperative pain (point) |
|---|
| Observation
group | 47 | 124.73±8.05 | 216.43±11.63 | 7.23±1.56 | 2.58±1.57 |
| Control group | 47 | 165.24±8.37 | 325.86±18.78 | 7.56±2.47 | 5.56±1.48 |
| t-value |
| 23.951 | 33.936 | 0.774 | 9.469 |
| P-value |
| <0.001 | <0.001 | 0.441 | <0.001 |
Comparison of incidence rates of
postoperative complications of patients between the two groups
In the observation group, the rate of complications,
including hyperthermia, persistent air leakage (>1 week),
cardiac arrhythmia and pulmonary atelectasis, was 6.98%, while the
rate of complications in the control group was 30.23%, suggesting
that the rate in the observation group was significantly lower than
that in the control group (P<0.05; Table III).
 | Table III.Comparison of the incidence rate of
postoperative complications of patients between the two groups (n,
%). |
Table III.
Comparison of the incidence rate of
postoperative complications of patients between the two groups (n,
%).
| Group | Case | Hyperthermia | Persistent air
leakage | Cardiac
arrhythmia | Pulmonary
atelectasis |
|---|
| Observation
group | 47 | 0 (0.00) | 0 (0.00) | 1 (2.13) | 1 (2.13) |
| Control group | 47 | 4 (8.51) | 3 (6.38) | 2 (4.26) | 4 (8.51) |
| χ2 |
|
| 7.932 |
|
| P-value |
|
| 0.005 |
|
Comparison of the levels of
inflammatory cytokines of patients between the groups
At 1 week after surgery, the levels of TNF-α, IL-6
and IL-8 of patients in both groups were remarkably elevated, and
the elevation in the control group was more significant than that
in the observation group (P<0.05; Table IV).
 | Table IV.Comparison of the levels of
inflammatory cytokines of patients between the two groups
(ng/l). |
Table IV.
Comparison of the levels of
inflammatory cytokines of patients between the two groups
(ng/l).
| Group | Time | Case | TNF-α | IL-6 | IL-8 |
|---|
| Observation
group | Before surgery | 47 | 62.64±6.28 | 56.36±4.27 | 73.52±3.16 |
|
| After surgery | 47 |
106.56±6.63a,b |
95.47±6.36a,b |
117.56±8.74a,b |
| Control group | Before surgery | 47 | 62.83±3.57 | 56.74±4.52 | 73.85±3.47 |
|
| After surgery | 47 |
123.39±8.24a |
116.56±9.53a |
135.62±9.83a |
Comparison of the cardiac and
pulmonary functions of patients at 3 months after surgery between
the two groups
There was significant improvement seen in the
cardiac and pulmonary function of these two groups, and the
improvement in the observation group was superior to that of the
control group (P<0.05; Table
V).
 | Table V.Comparison of the cardiac and
pulmonary functions of patients between the two groups. |
Table V.
Comparison of the cardiac and
pulmonary functions of patients between the two groups.
| Group | Time | Case | HR (bpm) | FEV1 (%) | MVV (%) | DLCO (%) |
|---|
| Observation
group | Before surgery | 47 | 69.87±6.54 | 1.96±0.36 | 68.63±3.73 | 77.57±3.26 |
|
| After surgery | 47 |
82.76±6.75a,b |
1.67±0.32a,b |
74.59±3.84a,b |
67.74±3.04a,b |
| Control group | Before surgery | 47 | 70.32±6.18 | 1.93±0.27 | 69.54±3.56 | 78.13±3.47 |
|
| After surgery | 47 |
96.53±7.43a |
1.44±0.25a |
61.57±3.14a |
71.25±3.16a |
Comparison of immunoglobulin levels of
patients between the groups
At 1 week after surgery, the levels of IgG, IgA and
IgM of patients of both groups were decreased, and the decrease in
the control group was more significant than that in the observation
group (P<0.05; Table VI).
 | Table VI.Comparison of immunoglobulin levels
of patients between the two groups. |
Table VI.
Comparison of immunoglobulin levels
of patients between the two groups.
| Group | Time | Case | IgG | IgA | IgM |
|---|
| Observation
group | Before surgery | 47 | 14.64±3.28 | 2.16±0.27 | 1.27±0.16 |
|
| After surgery | 47 |
12.58±2.73a,b |
1.87±0.18a,b |
1.06±0.12a,b |
| Control group | Before surgery | 47 | 14.58±3.14 | 2.13±0.23 | 1.25±0.14 |
|
| After surgery | 47 |
9.57±2.15a |
1.46±0.15a |
0.97±0.08a |
Comparison of levels of T lymphocyte
subgroups in serum of patients between the two groups
In these two groups, the levels of CD3+,
CD4+, CD8+ and
CD4+/CD8+ were decreased, and the decrease in
the control group was more significant than that in the observation
group (P<0.05; Table VII).
 | Table VII.Comparison of levels of T lymphocyte
subgroups in serum of patients between the two groups. |
Table VII.
Comparison of levels of T lymphocyte
subgroups in serum of patients between the two groups.
| Group | Time | Case |
CD3+ |
CD4+ |
CD8+ |
CD4+/CD8+ |
|---|
| Observation
group | Before surgery | 47 | 62.25±3.78 | 36.85±2.27 | 28.53±2.16 | 1.82±0.26 |
|
| After surgery | 47 |
53.56±3.13a,b |
31.43±2.16a,b |
23.16±2.04a,b |
1.52±0.14a,b |
| Control group | Before surgery | 47 | 63.84±3.46 | 37.13±2.24 | 28.67±2.16 | 1.85±0.27 |
|
| After surgery | 47 |
46.23±3.16a |
25.38±2.06a |
19.54±1.89a |
1.37±0.13a |
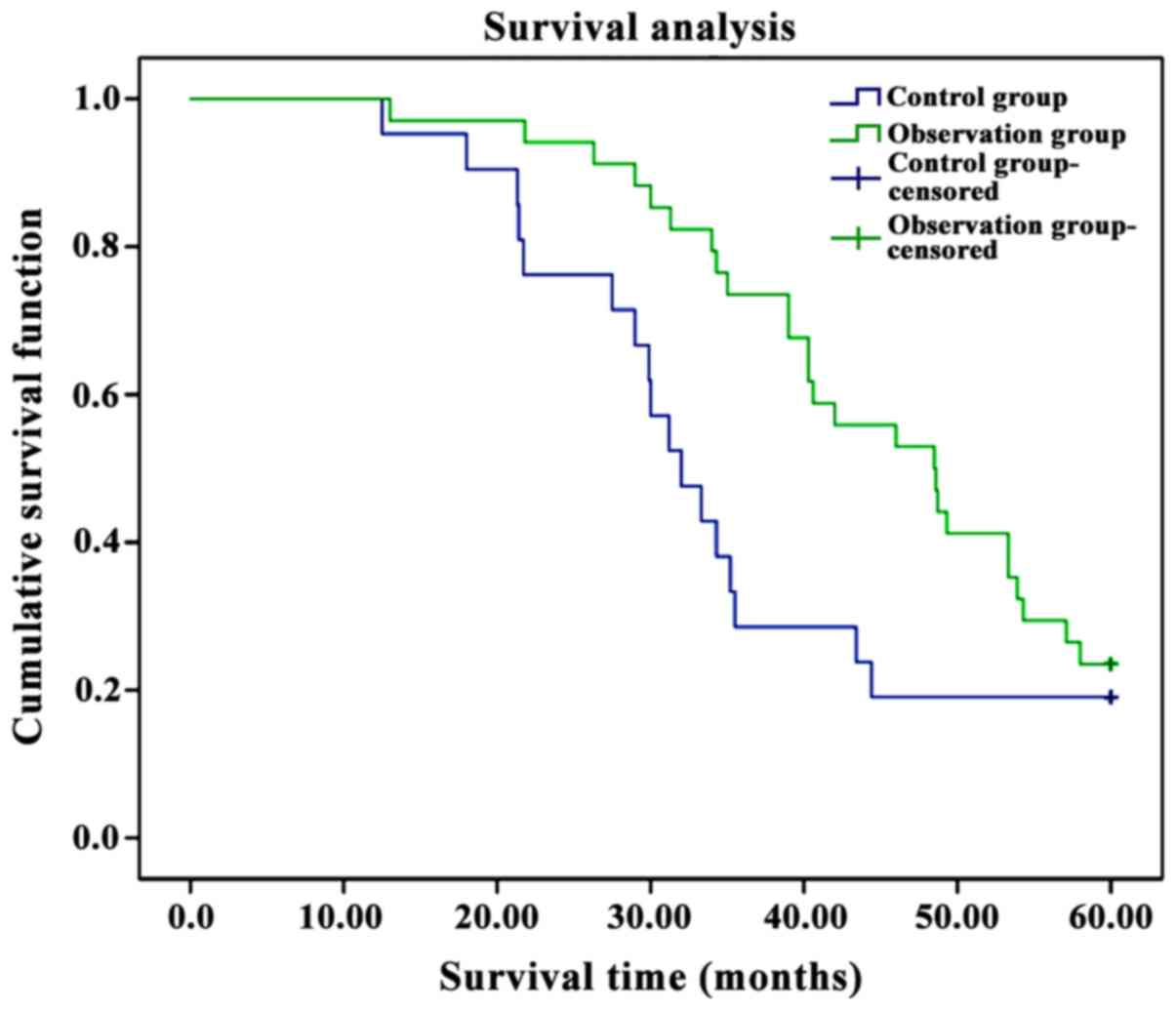
Comparison of the recurrence rate and
survival of patients between the groups
In the observation group, the average survival
duration of patients was significantly longer than that in the
control group, the recurrence rate was significantly lower than
that in the control group, and the 5-year survival rate after
surgery was significantly higher than that in the control group
(P<0.05; Table VIII and
Fig. 1).
 | Table VIII.Comparison of the condition of
patients in a five-year follow-up between the two groups. |
Table VIII.
Comparison of the condition of
patients in a five-year follow-up between the two groups.
| Group | Case | Five-year survival
(n, %) | Recurrence rate (n,
%) | Average survival
duration (month) |
|---|
| Observation
group | 47 | 33 (70.21) | 2 (4.26) | 49.76±7.75 |
| Control group | 47 | 22 (46.81) | 13 (27.65) | 40.83±7.68 |
|
χ2/t-value |
| 4.382 | 7.932 | 5.611 |
| P-value |
| 0.036 | 0.005 | <0.001 |
Discussion
Lung cancer is the most clinically common primary
malignant tumor of the lung; it is also known as bronchial lung
cancer for its origins in the bronchial epithelium (6). Various factors can contribute to the
onset of NSCLC, including smoking, occupational carcinogens, air
pollution, ionized radiation, diet, nutrition and variations in
genes and heritability (7).
Currently, the pathogenesis of NSCLC remains unclear yet, it is
believed to be caused by the malignant proliferation of mutated
cells due to an adverse microenvironment in local parts (8). Affected by various factors and the
invasion of exogenous carcinogens into the lung, the body initiates
a routine immune mechanism to minimize damage to the pulmonary
tissues and functions by limitation, neutralization, elimination
and eradication. Simultaneously, seal-repair is also conducted in
pulmonary tissues and functions. Once the factors that contribute
to the damage cannot be eradicated thoroughly in the body, a small
number of factors will be stagnated in local parts of the lung.
Although this may not cause acute stress response and extensive
damage to the lung, it can result in persistent inflammation of
local parts, which, together with the continuous repair of the
micro-damage through the repair mechanism, can lead to significant
difference between affected regions and the surrounding tissues in
normal metabolism. With extension of time, these parts will evolve
into adverse microenvironment in the local parts, whereas cells in
normal pulmonary tissues would not be able to adapt to the adverse
environment, and go into a differentiation phase, which can weaken
the repair capability, and facilitate loss of control, thereby
forming malignant proliferation and generation of NSCLC tumors
(9,10).
With a continuous increase in the healthcare
awareness of people and the development of modern medical imaging
techniques, NSCLC is apt to be discovered at an early stage, which
has brought opportunities for patients to receive the early-stage
treatment, and made surgical treatment into a preferred treatment
method (11). Segmental bronchi,
together with a bronchial tree and surrounding pulmonary tissues,
constitutes the bronchopulmonary segments, also known as pulmonary
segments. There are 8 segments in the left lung, and ten in right
lung with the tip in the radix pulmonis and the root on the surface
of lung (12). The independent
artery, bronchi and the vein share with adjacent pulmonary segment,
which consists of the independent bronchial tree and the relatively
independent blood-supply circulation system into each pulmonary
segment, which endows segmental resection with clinical
availability (13). With a continuous
development in the micro-invasive technique, thoracoscope-assisted
segmental resection has become increasingly popular among elderly
patients that are more susceptible to various diseases and have
difficulties in conventional thoracic surgeries (14). In this study, results show that in
comparison of surgical efficacy between the two groups, the
intraoperative bleeding amount, surgical duration and the
postoperative pain in the observation group is significantly
reduced, shortened and alleviated, respectively, and the incidence
rate of postoperative complications in the observation group is
significantly lower than that in the control group (P<0.05). In
addition, there was no significant difference in the comparison of
the number of resected lymph nodes between the groups (P>0.05).
The results suggest that thoracoscope-assisted surgery can
maximally shorten the surgical duration, reduce intraoperative
bleeding amount for its small surgical incision and alleviate
postoperative pain. Particularly for elderly patients, this
surgical method results in fewer injuries and a lower incidence
rate of postoperative complications.
The results of this study show that at 1 month
post-surgery, the cardiac and pulmonary function in both groups
were significantly improved, and the improvement in the observation
group was more significant than in the control group (P<0.05).
This may be due to thoracoscope-assisted segmental resection, which
on the premise of guaranteeing the surgical efficacy, maximally
retains the function of residual lung of patients, and is superior
to conventional thoracic surgery in terms of FEV1. Moreover, small
surgical parts can be magnified on the video screen, alleviate the
damage to the lung and effectively protect the pulmonary function
of patients, which is more conducive to the postoperative recovery
of patients (15).
Most NSCLC patients suffer from poor cellular immune
function, and, moreover, the stress responses caused by anesthesia
and surgeries will further inhibit immune functions, resulting in
disorders of immune function with inflammatory reactions, and
postoperative infection of patients (16). The results of this study reveal that
the levels of TNF-α, IL-6 and IL-8 at 1 week post-surgery in both
groups were significantly increased, and the increase in the
control group was more significant than those in the observation
group. At 1 week post-surgery, the levels of IgG, IgA and IgM of
the patients in two groups were reduced, and the decreases in the
control group was more significant than those in the observation
group. In addition, the levels of CD3+, CD4+,
CD8+ and CD4+/CD8+ were reduced in
the two groups, and the reductions in the control group were more
significant than those in the observation group (P<0.05). This
is due to the fact that thoracoscope-assisted segmental resection
results in fewer traumas, slighter stress responses and less
activation to the reactions in the immune system. Consequently, the
secretion of inflammatory factors, including TNF-α, IL-6 and IL-8,
is reduced. In addition, with features such as precision and
micro-invasion, thoracoscope-assisted segmental resection brings
less injury to normal immune functions, and scarcely affects normal
postoperative levels of IgG, IgA and IgM of patients (17). In the body, CD3+ assists to
identify the receptor of antibodies in T cells (18), CD4+ T cells, with the
regulatory function in the immune system, participates in the
activation of CD8+ T cells as an assistant role
(19), and the activated
CD8+ T cells eliminates cells infected by virus and
tumor cells (20).
Thoracoscope-assisted segmental resection poses lower injury on the
immune functions of patients, thereby resulting in a less
significant decrease in the capability of an immune response to
tumors.
The results of this study show that when comparing
the recurrence rate and survival of patients between the groups,
the average survival duration of patients in the observation group
was significantly longer than that in the control group, and the
recurrence rate was significantly lower than that in the control
group. The 5-year survival rate after surgery was higher than that
in the control group (P<0.05). This is due to the slight trauma
caused by thoracoscope-assisted segmental resection, which causes
relatively mild inflammatory responses, little influence on immune
functions, and significant short- and long-term efficacy, which
remarkably augments the postoperative survival rate and prolongs
survival duration of patients. In addition, the long-term efficacy
of thoracoscope-assisted segmental resection is more evident than
that of conventional thoracic surgery.
In conclusion, for the treatment of NSCLC,
thoracoscope-assisted segmental resection has a more evident short-
and long term efficacy and higher security. Thus, it is worthy of
being promoted in clinical practice.
References
|
1
|
Borghaei H, Paz-Ares L, Horn L, Spigel DR,
Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, et al:
Nivolumab versus docetaxel in advanced nonsquamous non-small-cell
lung cancer. N Engl J Med. 373:1627–1639. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
D'Addario G, Früh M, Reck M, Baumann P,
Klepetko W and Felip E: ESMO Guidelines Working Group: Metastatic
non-small-cell lung cancer: ESMO Clinical Practice Guidelines for
diagnosis, treatment and follow-up. Ann Oncol. 21 Suppl
5:v116–v119. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Garon EB, Rizvi NA, Hui R, Leighl N,
Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L,
et al: KEYNOTE-001 Investigators: Pembrolizumab for the treatment
of non-small-cell lung cancer. N Engl J Med. 372:2018–2028. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sprung J, Scavonetto F, Yeoh TY, Kramer
JM, Karnes RJ, Eisenach JH, Schroeder DR and Weingarten TN:
Outcomes after radical prostatectomy for cancer: a comparison
between general anesthesia and epidural anesthesia with fentanyl
analgesia: a matched cohort study. Anesth Analg. 119:859–866. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Klapper J and D'Amico TA: VATS versus open
surgery for lung cancer resection: Moving toward a minimally
invasive approach. J Natl Compr Canc Netw. 13:162–164. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Masters GA, Temin S, Azzoli CG, Giaccone
G, Baker S Jr, Brahmer JR, Ellis PM, Gajra A, Rackear N, Schiller
JH, et al: American Society of Clinical Oncology Clinical Practice:
Systemic Therapy for Stage IV Non-Small-Cell Lung Cancer: American
Society of Clinical Oncology Clinical Practice Guideline Update. J
Clin Oncol. 33:3488–3515. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Travis WD, Travis LB and Devesa SS: Lung
cancer. Cancer. 75 Suppl:191–202. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Thomas A, Liu SV, Subramaniam DS and
Giaccone G: Refining the treatment of NSCLC according to
histological and molecular subtypes. Nat Rev Clin Oncol.
12:511–526. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Grimminger PP, Maus MK, Schneider PM,
Metzger R, Hölscher AH, Sugita H, Danenberg PV, Alakus H and
Brabender J: Glutathione S-transferase PI (GST-PI) mRNA expression
and DNA methylation is involved in the pathogenesis and prognosis
of NSCLC. Lung Cancer. 78:87–91. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Black RC and Khurshid H: NSCLC: An update
of driver mutations, their role in pathogenesis and clinical
significance. R I Med J (2013). 98:25–28. 2015.PubMed/NCBI
|
|
11
|
Van Der Steen N, Rolfo C, Giovannetti E,
Reclusa P, Peters GJ and Pauwels P: P2.09: cMET in NSCLC:
Expression, amplification and mutations: track: biology and
pathogenesis. J Thorac Oncol. 11:S221–S222. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Seok Y, Cho S, Lee JY, Yang HC, Kim K and
Jheon S: The effect of postoperative change in bronchial angle on
postoperative pulmonary function after upper lobectomy in lung
cancer patients. Interact Cardiovasc Thorac Surg. 18:183–188. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cheng YD, Duan CJ, Dong S, Zhang H, Zhang
SK, Wang SQ and Zhang CF: Clinical controlled comparison between
lobectomy and segmental resection for patients over 70 years of age
with clinical stage I non-small cell lung cancer. Eur J Surg Oncol.
38:1149–1155. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Laursen LØ, Petersen RH, Hansen HJ, Jensen
TK, Ravn J and Konge L: Video-assisted thoracoscopic surgery
lobectomy for lung cancer is associated with a lower 30-day
morbidity compared with lobectomy by thoracotomy. Eur J
Cardiothorac Surg. 49:870–875. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goto T, Kadota Y, Mori T, Yamashita S,
Horio H, Nagayasu T and Iwasaki A: Video-assisted thoracic surgery
for pneumothorax: Republication of a systematic review and a
proposal by the guideline committee of the Japanese association for
chest surgery 2014. Gen Thorac Cardiovasc Surg. 63:8–13. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hong Y and Rurong W: Systemic and alveolar
inflammatory response in the dependent and nondependent lung in
patients undergoing lung resection surgery. Eur J Anaesthesiol.
33:63–64. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang J, Wang X, Zhang Y, Wu J and Zhou N:
Leucine-rich repeats and immunoglobulin-like domains protein 1 and
fascin actin-bundling protein 1 expression in nonsmall cell lung
cancer. J Cancer Res Ther. 12 Suppl:C248–C251. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feng Q, Wei H, Morihara J, Stern J, Yu M,
Kiviat N, Hellstrom I and Hellstrom KE: Th2 type inflammation
promotes the gradual progression of HPV-infected cervical cells to
cervical carcinoma. Gynecol Oncol. 127:412–419. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kayhan Erdogan G, Gul M, Kayhan B, Gedik
E, Ozgul U, Kurtoglu EL, Durmus M and Ersoy MÖ: Dexmedetomidine
ameliorates TNBS-induced colitis by inducing immunomodulator
effect. J Surg Res. 183:733–741. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jackute J, Zemaitis M, Pranys D,
Sitkauskiene B, Miliauskas S, Bajoriunas V, Lavinskiene S and
Sakalauskas R: The prognostic influence of tumor infiltrating
Foxp3(+)CD4(+), CD4(+) and CD8(+) T cells in resected non-small
cell lung cancer. J Inflamm (Lond). 12:632015. View Article : Google Scholar : PubMed/NCBI
|