Introduction
Patients with lung cancer have an increased danger
of developing a second tumor in the lung. Synchronous multiple
primary lung cancer (SMPLC) is characterized by the presence of the
second tumor concurrently. The incidence of SMPLC has been variably
reported as being between 1 and 16% (1). However, the exact incidence is not
easily evaluated due to the difficulty in distinguishing SMPLC from
a single pulmonary neoplasm with intrapulmonary metastases or
pulmonary metastases originating from primary cancers in different
organs.
The diagnostic criteria of SMPLC proposed by Martini
and Melamed is as follows (2): i)
lesions occur in different lobes or in different segments of the
same lobe, ii) lesions originate respectively from different kinds
of carcinoma in situ and show different histological types,
and iii) no metastasis is detected in the lymphatic systems and
other organs. Nevertheless, not all patients can be stratified in
accordance to the above standards.
To date, there is no universal agreement regarding
which methods should be followed in the diagnosis of SMPLC cases.
Therefore, the aim of the present study was to identify useful
clues used for the diagnosis or prognosis of SMPLC through the
retrospective study of 10 cases with SMPLC.
Patients and methods
Between January 2000 and December 2010, out of 2,991
patients diagnosed with lung cancer in our clinic (Chinese PLA
General Hospital), 10 patients were diagnosed as having SMPLC with
different histological categories by three radiologists. The
diagnosis of SMPLC was based on the combination of clinical
presentations, radiological findings and biopsy following pulmonary
lobectomy, bronchoscopy or percutaneous puncture.
The ethics board in our hospital made the decision
that there was no need to gain informed consent from the patients
since this was a retrospective investigation.
The patients underwent chest radioscopy and
abdominal ultrasonography. A total of 8 patients underwent brain
magnetic resonance imaging (MRI) and radionuclide bone scanning.
Two patients underwent systemic positron emission computed
tomography/computed tomography (PET/CT) scan. We retrospectively
analyzed these cases through reviewing the patient medical records,
radiological findings, pathological changes, treatment strategy and
survival time following diagnosis.
Results
The patients included in this study were 8 males and
2 females. Their mean age was 64.3 (range, 48–78 years). A total of
8 male patients were smokers, whose average smoking history was 44
years [4 pack-years (range, 15–80 pack-years)]. The detailed
information is listed in Table
I.
 | Table IClinical characteristics of 10
patients with SMPLC. |
Table I
Clinical characteristics of 10
patients with SMPLC.
| No. | Age/ gender | Smoking
(pack-years) | Number of
lesions | Tumor size (cm) | Primary TNM
stage | Pathology | Revised TNM
stage | Location of
lesions | Treatment plans | Survival
(months) |
|---|
| 1 | 73/M | 50 | 2 | 4.5×4.5×3 | T4N0M0 | SQ | T2aN0M0 | Rt upper lobe | Lobectomy +
segmentectomy + chemoradiation | 19 |
| 0.5×0.5×0.3 | LA | T1aN0M0 | Rt middle lobe | 50 |
| 2 | 48/M | 40 | 2 | 4×3×3 | T4N0M0 | LA | T2aN0M0 | Lt lower lobe | Pneumonectomy +
chemo-radiation | 50 |
| 1.4×1.3×1 | AD | T1aN0M0 | Lt upper lobe |
| 3 | 67/M | 60 | 2 | 5×4×3 | T3N0M0 | SM | LD | Rt upper lobe | Pneumonectomy +
chemo-radiation | 45 |
| 3×3×2 | SQ | T1bN0M0 | Rt upper lobe |
| 4 | 76/M | 40 | 2 | 4.5×3.2×2 | T2aN0M1a | SQ | T2aN0M0 | Lt upper lobe | Chemoradiation | 14 |
| 2×1.5×1 | SM | LD | Rt lower lobe |
| 5 | 58/M | 15 | 2 | 3.5×2×2 | T2aN0M1a | SQ | T2aN1M0 | Rt upper lobe | Chemoradiation | 4 |
| 2×1.3×1 | SM | LD | Lt upper lobe |
| 6 | 55/F | 0 | 2 | 2.8×2×2 | T4N0M0 | AD | T1bN0M0 | Lt upper lobe | Lobectomy +
segmentectomy | 64 |
| 1.6×1.6×1.5 | BAC | T1aN0M0 | Lt lower lobe |
| 7 | 59/M | 80 | 2 | 2.3×2.1×1.5 | T1aN0M1a | AD | T1aN0M0 | Rt lower lobe | Lobectomy +
lobectomy | 6 |
| 1.6×1.5×1.5 | BAC | T1aN0M0 | Lt lower lobe |
| 8 | 65/M | 40 | 2 | 3×2×2 | T4N0M0 | AD | T1aN0M0 | Rt lower lobe | Lobectomy +
segmentectomy | 26 |
| 1.5×1.4×1.4 | BAC | T1aN0M0 | Rt upper lobe |
| 9 | 78/M | 30 | 2 | 3.5×2.5×2 | T4N0M0 | AD | T1bN0M0 | Rt upper lobe | Chemoradiation | 17 |
| 2.8×1.9×1.2 | BAC | T1aN0M0 | Rt lower lobe |
| 10 | 64/F | 0 | 2 | 12×8.5×3 | T4N0M0 | BAC | T3N0M0 | Lt upper lobe | Pneumonectomy +
chemo-radiation | 14 |
| 3×3×2 | AD | T1bN0M0 | Lt lower lobe |
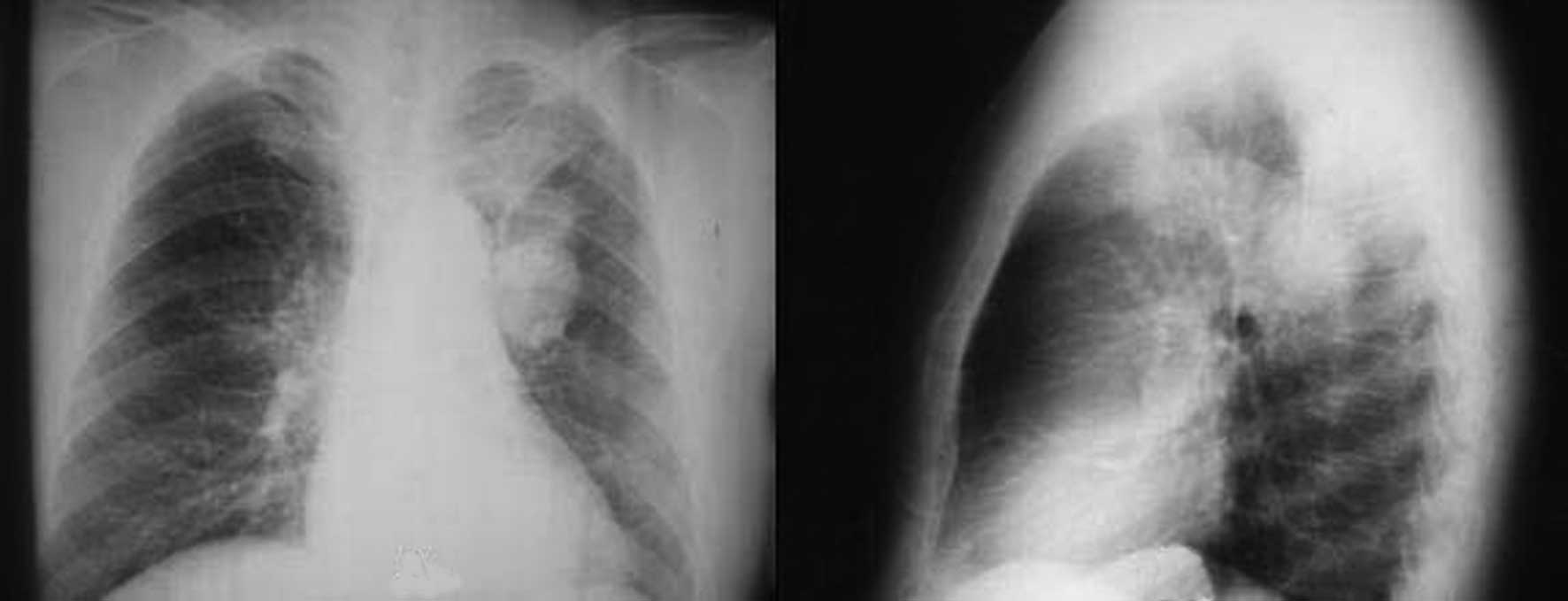
Chest CT findings demonstrated two pulmonary lesions
arising in different sites in patients. The two pulmonary lesions
occurred in the bilateral lung in 3 patients, in different lobes of
the unilateral lung in 6 patients, as well as the same lobe of the
unilateral lung in 1 patient. The sizes of lesions were similar in
7 cases. All these lesions displayed malignant characteristics of
primary lung cancer, including an irregular margin, spicule
formation, abnormal lung lobulation, irregular cavity, signs of
bronchiole inflation and signs of pleural indentation. In addition,
chest CT findings revealed no lymphadenectasis other than for 1
patient. Admission chest radiograph demonstrated that 2 similar
tumor masses were located in 2 segments of the left upper lobe of
patient 3 (Fig. 1). One mass (3×3×2
cm) in the anterior segment of the left upper lobe displayed
malignant characteristics, such as spicule formation and pleural
indentation, and the other mass (5×4×3 cm) in the posterior segment
of the left upper lobe displayed malignant characteristics, such as
spicule formation and bronchiole inflation. Chest CT showed no
lymphadenectasis in the hilum of the lung and the mediastinum. In
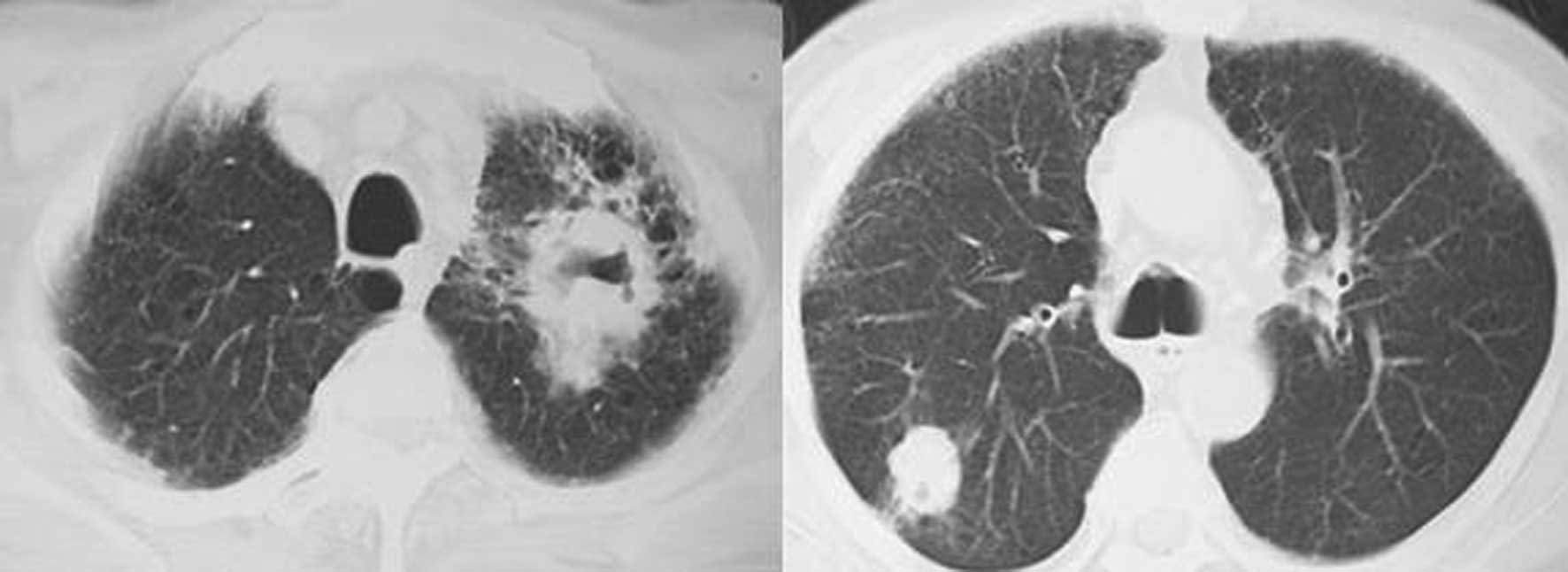
case 4, one mass (4.5×3.2×2 cm) was located in the left upper lobe
with an irregular cavity, and honeycomb-like changes were found
surrounding the mass. The other mass (2×1.5×1 cm), located in the
right upper lobe, displayed signs of pleural indentation (Fig. 2). There was no lymphadenectasis
observed in the chest CT.
The levels of a number of tumor markers increased in
2 patients. In patient 5, the levels of the tumor markers were as
follows: neuron-specific enolase (NSE) 79.26 ng/ml, cytokeratin
fragment 21-1 (CYFRA21-1) 7.98 ng/ml and squamous cell carcinoma
(SCC) 4.3 ng/ml. In patient 4, the results were as follows:
carcinoembryonic antigen (CEA) 13.04 ng/ml, NSE 51.02 ng/ml and SCC
12.80 ng/ml.
The combined results obtained from abdominal
ultrasonography, brain MRI, radionuclide bone scanning and PET/CT
scanning showed no metastatic lesions in these patients.
Pathological examination on the biopsy specimens from bronchoscopy,
percutaneous puncture or pneumonectomy confirmed that 2 lesions
showed different histological properties. On the basis of the
pathological changes, chest CT findings and the results of the
tumor marker test, their preliminary clinical diagnoses of primary
lung cancer staged IIIB or IV with intrapulmonary metastasis were
revised as SMPLC staged I, II and IIIA. According to the revised
clinical stage, a reasonable treatment strategy was drawn. A total
of 7 patients were treated with pulmonary resection, regional and
mediastinal lymphadenectomy. Following the treatment, 6 patients
lived longer than 1 year, out of which 3 patients lived longer than
3 years. Another patient remains alive. The remaining 3 patients
did not undergo surgery owing to poor heart and pulmonary
functions, and instead were treated with chemoradiation. Following
the chemoradiation treatment, 2 patients lived longer than 1 year,
while the other lived less than 1 year.
Discussion
When 2 or more primary tumors are contemporaneously
detected in different pulmonary sites, they are termed as SMPLC.
According to the results from the present study, SMPLC presents
apparent preponderance in smokers. These results are consistent
with those from a previous report that the intensity and duration
of smoking was associated with the occurrence of SMPLC (3). The incidence of SMPLC has been
reported to range from 0.7 to 20% in all patients with lung cancer
in previous studies (4–10), and to increase with the progression
of diagnostic techniques in recent years. A possible cause for this
variability is that the discrimination of multiple primary lung
cancers from intrapulmonary metastasis is very difficult. In this
study, out of 2,991 patients diagnosed with lung cancer, only 10
were diagnosed as SMPLC. This incidence was lower than other
reported data, which suggested that SMPLC patients might be
overlooked. Thus, a high index of awareness of this disease is
required for early diagnosis.
Iconography findings of all 10 patients in this
study shared some common characteristics: i) two pulmonary lesions
arised in different sites of lung, ii) the sizes of lesions were
similar, iii) the lesions displayed malignant characteristics of
primary lung cancer without signs of lymphadenectasis in the hilum
of the lung and the mediastinum, and iv) no extensive metastatic
lesions were detected. All the above characteristics are considered
to be potential clues for the early diagnosis of SMPLC.
Tumor markers have been extensively investigated in
lung cancer. The most extensively studied tumor markers for
non-small cell lung cancer are CEA, SCC and cytokeratins [CYFRA,
tissue polypeptide antigen (TPA) and tissue polypeptide-specific
antigen (TPS)]. NSE was considered to be the representative tumor
marker for small cell lung cancer (SCLC). None of these markers are
ideal (11–18). In this study, the levels of these
tumor markers simultaneously increased in 2 patients, which
indicates poor performance of these tumor markers in the diagnosis
of SMPLC.
The staging of lung cancer is crucial for the
evaluation and prognosis of the disease, exchanging information
among clinicians and researchers, and providing a guidance for the
most appropriate treatment strategy (19–22).
In the present study, the 2 tumors in SMPLC patients were
separately staged. Based on the different stages of the 2 tumors,
corresponding surgery was thus performed, which proved to be more
beneficial for the patients. Thus, separate biopsies for different
pulmonary masses should be performed as soon as possible in
suspected SMPLC patients.
In conclusion, the diagnosis of SMPLC might be
delayed or mistaken as lung cancer with intrapulmonary metastasis.
A high index of awareness is required for the early diagnosis of
this disease. The malignant characteristics of primary lung cancer
in different lesions might be valuable clues for the diagnosis of
SMPLC. Alterations in the levels of tumor markers may be a poor
diagnostic tool for the detection of SMPLC. A separate staging of
different tumors in SMPLC patients should be beneficial. Therefore,
separate biopsies for various pulmonary masses should be performed
for clinical staging as soon as possible, and reasonable treatments
based on this staging should also be selected.
References
|
1
|
Ferguson MK, DeMeester TR, DesLauriers J,
et al: Diagnosis and management of synchronous lung cancer. J
Thorac Cardiovasc Surg. 89:378–385. 1985.
|
|
2
|
Martini N and Melamed MR: Multiple primary
lung cancers. J Thorac Cardiovasc Surg. 70:606–612. 1975.
|
|
3
|
Wang X, Christiani DC, Mark EJ, et al:
Carcinogen exposure, p53 alteration, and K-ras mutation in
synchronous multiple primary lung carcinoma. Cancer. 85:1734–1739.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Miura H, Nakajima N, Ikeda N, et al:
Therapeutic strategy for secondary lung cancer. Kyobu Geka.
63:956–961. 2010.PubMed/NCBI
|
|
5
|
Van Rens MTM, Zanen P, de la Riviere AB,
et al: Survival in synchronous versus single lung cancer: upstaging
better reflects prognosis. Chest. 118:952–958. 2000.PubMed/NCBI
|
|
6
|
Lam S, MacAulay C and Palcic B: Detection
and localization of early lung cancer by imaging techniques. Chest.
103:S12–S14. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Woolner LB, Fontana RS, Cortese DA, et al:
Roentgenographically occult lung cancer: pathologic findings and
frequency of multicentricity during a 10-year period. Mayo Clin
Proc. 59:453–466. 1984.PubMed/NCBI
|
|
8
|
Morita T: Incidence, contents and change
of autopsied multiple primary cancers of the lung based on the
annual of the autopsy cases in Japan between 1958 and 1992. Haigan.
37:283–294. 1997. View Article : Google Scholar
|
|
9
|
Saito Y, Fujimura S, Sato M, et al: Recent
advances in diagnosis and treatment of multiple primary lung
cancers. Nippon Kyobu Rinsho. 52:95–101. 1993.
|
|
10
|
Matsuge S, Hosokawa Y, Sato K, et al:
Surgical treatment for bilateral multiple lung cancers. Kyobu Geka.
53:89–94. 2000.
|
|
11
|
Niho S, Nishiwaki Y, Goto K, et al:
Significance of serum pro-gastrin-releasing peptide as a predictor
of relapse of small cell lung cancer: comparative evaluation with
neuron-specific enolase and carcinoembryonic antigen. Lung Cancer.
27:159–167. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shibayama T, Ueoka H, Nishii K, et al:
Complementary roles of pro-gastrin-releasing peptide (ProGRP) and
neuron specific enolase (NSE) in diagnosis and prognosis of small
cell lung cancer (SCLC). Lung Cancer. 32:61–69. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jorgensen LGM, Osterlind K, Genolla J, et
al: Serum neuron-specific enolase (S-NSE) and the prognosis in
small-cell lung cancer (SCLC): a combined multivariable analysis on
data from nine centres. Br J Cancer. 74:463–467. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Molina R, Filella X and Auge JM: ProGRP: a
new biomarker for small cell lung cancer. Clin Biochem. 37:505–511.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Stieber P, Dienemann H, Schalhorn A, et
al: Pro-gastrin-releasing peptide (ProGRP) - a useful marker in
small cell lung carcinomas. Anticancer Res. 19:2673–2678.
1999.PubMed/NCBI
|
|
16
|
Lamy PJ, Grenier J and Pujol JL:
Pro-gastrin-releasing peptide, neuron specific enolase and
chromogranin A as serum markers of small cell lung cancer. Lung
Cancer. 29:197–203. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Goto K, Kodama T, Hojo F, et al:
Clinicopathologic characteristics of patients with nonsmall cell
lung carcinoma with elevated serum progastrin-releasing peptide
levels. Cancer. 82:1056–1061. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Molina R, Auge JM, Bosch X, et al:
Usefulness of serum tumor markers, including progastrin-releasing
peptide, in patients with lung cancer: correlation with histology.
Tumor Biol. 30:121–129. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Van Rens MTM, de la Riviere AB, Elbers
HRJ, et al: Prognostic assessment of 2,361 patients who underwent
pulmonary resection for non-small cell lung cancer stage I, II and
IIIA. Chest. 117:374–379. 2000.PubMed/NCBI
|
|
20
|
Chang YL, Wu CT and Lee YC: Surgical
treatment of synchronous multiple primary lung cancers: experience
of 92 patients. J Thorac Cardiovasc Surg. 134:630–637. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Adebonojo SA, Moritz DM and Danby CA: The
results of modern surgical therapy for multiple primary lung
cancers. Chest. 112:693–701. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tsunezuka Y, Matsumoto I, Tamura M, et al:
The results of therapy for bilateral multiple primary lung cancers:
30 years experience in a single centre. Eur J Surg Oncol.
30:781–785. 2004.PubMed/NCBI
|